Abstract
Purpose
Although the EQ-5D has a long history of use in a wide range of populations, the newer five-level version (EQ-5D-5L) has not yet had such extensive experience. This systematic review summarizes the available published scientific evidence on the psychometric properties of the EQ-5D-5L.
Methods
Pre-determined key words and exclusion criteria were used to systematically search publications from 2011 to 2019. Information on study characteristics and psychometric properties were extracted: specifically, EQ-5D-5L distribution (including ceiling and floor), missing values, reliability (test–retest), validity (convergent, known-groups, discriminate) and responsiveness (distribution, anchor-based). EQ-5D-5L index value means, ceiling and correlation coefficients (convergent validity) were pooled across the studies using random-effects models.
Results
Of the 889 identified publications, 99 were included for review, representing 32 countries. Musculoskeletal/orthopedic problems and cancer (n = 8 each) were most often studied. Most papers found missing values (17 of 17 papers) and floor effects (43 of 48 papers) to be unproblematic. While the index was found to be reliable (9 of 9 papers), individual dimensions exhibited instability over time. Index values and dimensions demonstrated moderate to strong correlations with global health measures, other multi-attribute utility instruments, physical/functional health, pain, activities of daily living, and clinical/biological measures. The instrument was not correlated with life satisfaction and cognition/communication measures. Responsiveness was addressed by 15 studies, finding moderate effect sizes when confined to studied subgroups with improvements in health.
Conclusions
The EQ-5D-5L exhibits excellent psychometric properties across a broad range of populations, conditions and settings. Rigorous exploration of its responsiveness is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The EQ-5D is a broadly used generic multi-attribute health utility instrument. In addition to a thermometer-like visual analog scale (VAS) anchored by 0 (worst imaginable health) and 100 (best imaginable health), the EQ-5D’s descriptive system comprises five dimensions with one item per dimension: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD) and anxiety/depression (AD). Responses to these items can be converted into a single measure of health utility using preference-based (typically country-specific) weights. Preference weights are derived from preference elicitation studies using hypothetical EQ-5D health profiles [1], typically sampling a general population.
Until 2005, respondents could select from three response levels of function or symptoms for each dimension (the EQ-5D-3L; 3L). However, due to evidence of notable ceiling effects of the EQ-5D-3L in some populations [2,3,4,5] and concerns regarding the instrument’s sensitivity to certain patient-relevant changes [6,7,8,9,10], a five response level version of the instrument was developed by the EuroQol group in 2010 [11, 12]. The five-level version (EQ-5D-5L; 5L) added two response levels: one between “no problems” (level 1) and “moderate/some problems” (level 2 in 3L, level 3 in 5L), and another one between “moderate/some problems” and “severe problems” (level 3 in 3L, level 5 in 5L). The EQ-5D-5L also updated the middle response level with the term “moderate” from the EQ-5D-3L’s “some” for the first three dimensions, while the most severe response level for MO was changed from “confined to bed” to “unable to walk about”. Additionally, the instructions for marking overall health today on the visual analog scale (VAS) were different between the two versions until 2019. The EQ-5D-5L is currently available for more than 130 languages [13] and has been formally tested against the EQ-5D-3L in numerous studies, demonstrating improved psychometric properties over the EQ-5D-3L [14]. An interim scoring strategy that applies existing EQ-5D-3L preference weights to EQ-5D-5L can be used if EQ-5D-5L preference weights for certain populations are not yet available [A4].
Although its use has expanded to a wide range of settings and research purposes, there is no study reporting a comprehensive review of the measurement properties of the EQ-5D-5L. This review will be informative for researchers interested in economic evaluation and preference measurement, decision makers, users of EQ-5D-5L as patient-reported outcome measure for improving health care, and readers who need to interpret the findings from studies incorporating the EQ-5D-5L. The 5L instrument has now enjoyed over a decade of use and this paper aims to summarize the existing evidence on the psychometric properties of the EQ-5D-5L. A second objective of this review is to identify knowledge gaps regarding the psychometric properties of the EQ-5D-5L, and to highlight important areas for future research.
Methods
This literature search and review was guided by the PRISMA guidance on systematic reviews and meta-analyses [15]. This review focuses on the descriptive system of the EQ-5D-5L (the five items) as it was not always clear which version of the EQ-VAS was used in extracted studies.
Literature search
Four online databases—PUBMED (MEDLINE), PsycINFO, Excerpta Medica Database (EMBASE), and the EuroQol website—were searched using pre-determined terms: “EQ-5D,” “EQ-5D-5L,” “5L,” “EuroQol” and “5 Level.” The search included publications up to January 2019. Duplicates were assessed using author names, titles and journals. Exact search strategy and terms can be found in Supplementary Table 1.
Two screening phases were conducted: (1) title and abstract, and (2) full text. Two researchers experienced in psychometric research methods and the EQ-5D instruments (IB and YF) independently screened the publications and reached consensus on any disagreements to determine inclusion. When consensus could not be reached, two senior researchers with extensive experience in psychometric research, health-related quality of life (HRQoL) measurement and the EQ-5D instrument were consulted for a final decision (TK and MFJ).
The a priori exclusion criteria were:
-
1.
does not study humans 18 years or older;
-
2.
publication language is other than German or English;
-
3.
study does not assess the official version of the EQ-5D-5L or an experimental version of the 5L was used;
-
4.
published prior to 2005 (prior to development of the 5L);
-
5.
not a peer-reviewed primary study, literature review or conference paper (conference papers were included but other conference proceedings such as presentations or posters were excluded); and
-
6.
not evaluating the measurement and psychometric properties of the EQ-5D-5L.
Data extraction
Publications selected for inclusion were reviewed and data entered into pre-determined tables by either YF or IB. Sometimes, values needed to be estimated from available information. When information on means and standard deviations were not available, but other sufficient data were reported (such as range or median), the mean and standard deviations were estimated using recommendations from Wan et al. 2014 [16]. When multiple studies use the same underlying dataset, data was extracted only once (e.g., [A20, A26, A31, A36–A38, A49, A53, A77, A79, A96]). General study characteristics including sample size, study design, sample characteristics and version of EQ-5D-5L were extracted, as were information on distributional properties such as means, percent reporting best health (“no problems” on dimensions or ‘11111’ across the health profile), percent reporting worst health (“extreme” or “unable to” on dimensions or ‘55555’ across the health profile) and missing values, for dimensions as well as the health profile. Although no guidance for level of missing values indicate the feasibility of an instrument, ≤ 5% has been found to be acceptable for multiple imputation [17]. Missing values ≤ 5% and floor ≤ 15% are considered acceptable [18].
Reliability is the consistency of an instrument, internally (extent to which subscale items are interrelated) as well as the instrument’s stability across time (whether the instrument produces similar results in stable environments). Internal consistency is not a relevant psychometric property for the EQ-5D instruments and therefore we did not include it in this review. Agreement between two applications of the instrument over a period of time over which it should be stable (test–retest) is usually evaluated using Cohen’s Kappa (κ) for categorical items (EQ-5D-5L items) or ICC for continuous values (EQ-5D-5L index value), with a level of ≥0.8 and ≥0.7 determined as acceptable, respectively [19,20,21]. We relied on the guidance from Cicchetti 1994 [22] to define Kappa and ICC: < 0.40 = poor, 0.40–0.59 = fair, 0.60–0.74 = good, 0.75–1.00 = excellent. Other methods such as area under the receiver operating characteristic curve (AUROC) were also reported [23, 24].
In general, validity refers to the degree to which a measurement tool captures the underlying construct of interest. We extracted all information regarding different forms of validity from included publications, the most commonly investigated being convergent validity (a specific subtype of construct validity), that examines how closely two instruments that are intended to measure the same construct are related. This is most often done by testing the correlation between the EQ-5D-5L and other measures of health or health-related quality of life (including those measuring pain, and mental or physical health or HRQoL). Other validity results extracted include known-groups validity (examining whether the 5L can distinguish between a priori determined groups).
Responsiveness is the ability of an instrument to capture true changes (e.g., due to a health intervention) in the construct of interest over time. Some argue that responsiveness is a subtype of validity or reliability [25]. Responsiveness is of particular importance for the EQ-5D-5L: one of the reasons the instrument was created was to address criticisms that the EQ-5D-3L was not sufficiently sensitive to change [26]. Responsiveness can be specific to population, context, and depends on the direction of change in the underlying construct [27]. In the case of the EQ-5D-5L, responsiveness addresses the question if the index value or individual items can detect relevant changes in underlying health. Preliminary research conducted on experimental five-level versions of the EQ-5D found its index value to be sensitive to change. Commonly used methods evaluating responsiveness include standardized effect size (SES) and/or standardized response mean (SRM) [25, 27, 28]. Both standardize the difference in means from two measurement points by dividing by standard deviation (of the mean or of the change scores). An SES of 0.2 to 0.3 is considered small, ≈ 0.5 medium and ≥ 0.8 large effect sizes [29]. Some studies examined the EQ-5D-5L’s ability to detect a change as defined by external criteria, or anchor, to estimate minimally important differences (MID) or the smallest change in score that is beneficial or relevant for patients [27, 28, 30]. The external anchor is usually a patient-assessment.
Analysis
Due to the heterogeneity of studies and outcomes included, we were only able to summarize three outcomes across studies: proportion of respondents reporting the best health, mean index values, and EQ-5D-5L’s correlations with other measures (Spearman’s or Pearson’s Rho). When multiple index scores are reported in a study, the most up to date (EQ-5D-5L as opposed to the interim or ‘crosswalk’) or most appropriate (closest to the sampled population) index scores were extracted. The signs of correlation coefficients were changed if authors had not corrected for the directionality of the scales. Subgroup analysis was performed when there were at least three studies representing a relevant subgroup.
Data were pooled by means of random-effects models using inverse variance weight for pooling. Pooling was based on Fisher’s z transformation of correlation coefficients and logit transformation of proportions. Microsoft excel was used for data extraction, while R was used for data analysis [31]. The R package “meta” was used to estimate pooled values [32].
Results
We identified 496 papers during the initial search and additional 397 papers during the updates in 2018 and 2019, of which 99 papers were included for review (Fig. 1; reference list A). These papers included general population (n = 32) and patients (n = 58) from 32 countries (see Table 1). The country where the most numerous studies were conducted was the UK/England (n = 18), while Canada, Germany, Singapore and the USA were the locations with the second most numerous studies (n = 8 each). The patient groups represented by the most studies are musculoskeletal/orthopedic (n = 8), cancer (n = 8) and lung/respiratory diseases (n = 7). The Multi-Instrument Comparison study (MIC) [A20, A26, A31, A36–A38, A49, A53, A77, A79, A96] and the study that developed a method of deriving 5L interim index values from 3L value sets [A4, A6, A83] were represented by 11 and 3 studies, respectively. General characteristics of included studies can be found in Supplementary Table 2.
Distribution properties
Missing values (17 of 17 papers) and most severe health state (43 of 48 papers) were under 5% and 15%, respectively, showing the 5L to be feasible and free from floor effects (Table 1). Studies with greater than 15% reporting the most severe health (in certain dimensions) were those studying patients with stroke [A28, A46], spinal cord injury [A56], women just after giving birth [A84] and patients with chronic illnesses [A83]. These patients were reporting severe health impairments in MO, SC, and/or UA. Enough information was reported by 48 studies to pool proportion reporting the best health state ‘11111,’ which was 23% for patients, ranging from 2% (musculoskeletal diseases) to 36% (cancer; Fig. 2a). Pooled proportion of over 15% at full health was observed for patients with diabetes, cancer, liver diseases, kidney diseases and skin diseases. General and healthy population studies were 48% and 41% reporting full health, respectively (Fig. 2b).
By dimension, proportions reporting “no problems” were smallest across the board for stroke, while SC consistently had large ceilings except for patients with stroke, diseases of the nervous system and diseases of the musculoskeletal system (pooled proportion reporting “no problems” in EQ-5D-5L dimensions can be found in Supplementary Table 3). Konnopka and Koenig (2017) also found SC to be most problematic in terms of percentage at the ceiling, even for those reporting four or more diseases and needing one or more hours of daily care [A61].
Index value means could be pooled from 58 publications, showing they were generally lower for disease groups than healthy populations and lower socio-economic/socio-demographic groups than higher (Fig. 3a, b).
Reliability
Nine papers addressed test–retest reliability, eight found the scale agreement (ICC) excellent and the remaining study finding an ICC of 0.7. However, five studies found fair agreement on the item level (Cohen’s Kappa) for certain dimensions: they tend to be smaller for PD and highest for MO (Table 1).
Validity
Studies examining construct validity typically compared the EQ-5D-5L to the EQ-5D-3L: the focus has been on the response categories as the items themselves were identical. As we did not include studies with experimental versions of the 5L, most of the earlier studies examining the construct validity of various response options of the 5L have not been included. One included study used exploratory factor analysis to examine the structure of the EQ-5D-5L, Satisfaction with Life Scale and MacNew questionnaire [A96]. They found MO, SC, UA, and PD to load onto one factor with other physical health and usual activity items, and AD to load onto a second factor including items addressing mood, depression, and confidence. Of the five included papers addressing content validity, three used qualitative methods. Keeley et al. (2013) sampled research professionals who found the SC item to be too narrowly defined and the UA item to be too broad, while deeming PD and AD as the most relevant dimensions related to health-related quality of life [A7]. Whitehurst et al. (2014) sampled patients with spinal cord injuries, who generally found the 5L to be relevant for their health problems [A21]. However, some found the instrument to lack coverage of specific aspects of spinal cord injury. A more recent qualitative study found the EQ-5D-5L to lack relevancy for asthma patients except for some physical limitations, but also praised the instrument for its generic nature [A92].
Craig et al. (2014) found via regression analysis that the 5L encompasses a slightly larger range of EQ-VAS scores from best to worst health state compared to the 3L [A15]. Janssen et al. 2018 also investigated the distance between the 3L and 5L levels using a direct approach asking patients to place the labels onto a horizontal VAS scale, finding a larger range covered by the 5L [A83].
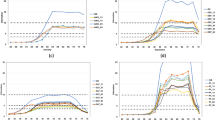
Convergent validity was assessed by the greatest number of papers (n = 33), usually examining correlations of EQ-5D-5L with other measures of health using Pearson’s correlation or Spearman’s Rho rank correlation coefficient. Figure 4a–c illustrates pooled correlations of the EQ-5D-5L index value with other measures of physical health, mental/social/cognitive health and global health. The strongest correlations were observed for multi-attribute utility instruments (pooled rho = 0.756), physical/functional measures (pooled rho = 0.582) and pain/discomfort measures (pooled rho = 0.595). The EQ-5D-5L index value correlated poorly with measures of satisfaction (pooled rho = 0.335) and cognition/communication (pooled rho = 0.259).
a Pooled correlation coefficient for EQ-5D-5L index value with other physical health measures. b Pooled correlation coefficient for EQ-5D-5L index value with other mental, emotional, cognitive and fatigue/vitality health measures. c Pooled correlation coefficient for EQ-5D-5L index value with other global health, clinical and non-health measures
On a dimension level, the strongest correlation was observed for PD and pain measures (pooled rho = 0.636), while all items correlated poorly with measures of cognition/communication and vitality/fatigue/sleep. AD was the only item to show (moderate) correlation with mental (pooled rho = 0.461), emotional and social health items (pooled rho = 0.413). Pooled correlation of EQ-5D-5L dimensions and other measures of health can be found in Supplementary Table 4.
Bhadhuri et al. 2017 examined the EQ-5D-5L’s ability to measure spillover effects and found strong correlations between EQ-5D-5L scores of family of meningitis survivors and survivors’ social lives (Spearman’s Rho = 0.52, 0.45), exercise (rho = 0.55, 0.82), and personal health (rho = 0.88, 0.95) [A57]. Poor correlations were found between carers’ and survivors’ EQ-5D-5L dimensions (rho = 0.07 to 0.24), index (rho = 0.19, 0.26), and EQ-VAS (rho = 0.22, 0.24).
Table 2 includes information from studies, which examined validity other than convergent. Generally, the 5L can distinguish across disease groups, disease severity, symptoms, and related groups, and also across age and education. However, it does not consistently distinguish across groups differing with certain clinical outcomes (e.g., presence of deformities in the spine, frequency of medication use, gender, use of health services, and marital status.
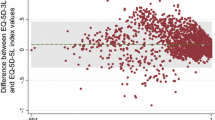
Responsiveness
Fifteen studies examined whether the EQ-5D-5L captures change in health over time. All of these papers included SES and/or SRM. Although not reported, the SES could be calculated for two papers using reported information [A71, A84]. Five assessed results across respondents who improved, remained stable or deteriorated over time based on an anchor measure [A28, A39, A57, A59, A68, A87]. Four papers also reported MID [A46, A50, A71, A85]. Two used retrospective items to define change [A50, A71]. Table 4 summarizes the responsiveness results—when available, the SES and SRM are used for ease of interpretability. The EQ-5D-5L index values typically had moderate effect sizes for improved patients and those expected to improve (over the course of medical or therapeutic intervention). The largest effect sizes were observed for patients days and weeks after giving birth [A84]. Compared to other instruments, the 5L generally performs as well or better. Two additional papers addressed dimension-level changes [A23, A74], both finding the 5L to be more sensitive than the 3L. Crick et al. 2018 examined only the AD dimension and noted that both the 3L and 5L were limited in responsiveness [A74].
Discussion
The EQ-5D is a generic preference-based health status instrument that has enjoyed widespread use since its creation in the 1980s [33]. The psychometric properties of the three-level version have been well established [34,35,36,37,38,39,40]. Any reluctance of using the more recently developed five-level version might come in part from limited experience and evidence for validity, reliability or responsiveness in different populations [41]. This review summarized published evidence on the psychometric properties of the EQ-5D-5L, which has been investigated in a broad array of countries, populations and contexts in the past decade. No studies found missing values to be problematic for the instrument, demonstrating feasibility. Test–retest results show potential problems with stability over time on an item level, but not at the instrument (index score) level. Note that internal consistency is not a relevant psychometric property for the EQ-5D-5L since its index score is based on a completely different measurement framework (as a preference-based measure).
Rather large proportions of respondents reporting the best health profile were observed for general population studies but less so for patient populations. The EQ-5D was conceptualized to measure deviations from full health (or negative health) and is more prone to larger ceilings than instruments that include positive health dimensions (e.g., the SF-6D). Therefore, studies with samples for which impact on the functions covered by the EQ-5D-5L (e.g., recovered cancer patients, liver disease, diabetes) is less relevant, other disease-specific instruments should be used in conjunction. On the item level, most studies, even those with populations in poorer health, reported a substantial ceiling with the dimension “self-care”, although the ceiling for self-care was low for respondents who were expected to have limitations with this function (e.g., patients before hip replacement surgery, patients shortly after cesarean section, patients with spinal cord injury [A21, A24, A84]). These results suggest that while most populations may not report problems in “self-care”, it is relevant for particular patient groups.
Our results overall solidly establish the validity of the EQ-5D-5L as supported by observed trends across subgroups (pooled means, known-group validity) as well as the convergent validity (correlation of items and index to other measures of health-related quality of life). Index values as well as the dimensions show moderate to strong correlations with physical/functional measures, pain, measures of mental and emotional health, activities of daily living and clinical/biological measures as well as with other multi-attribute utility measures. On the other hand, the 5L is not found to be correlated with satisfaction with life and cognition/communication measures. Indeed, current efforts investigating adding dimensions (so-called “bolt-ons”) to the 5L has identified cognition as an important dimension missing from the EQ-5D [42,43,44].
Included studies on responsiveness are heterogeneous in terms of the population, whether and which anchors were used, whether a health intervention was administered, and stratification of results across subgroups. This is not a problem unique to the EQ-5D-5L as, unlike other psychometric properties, there is not a set of recommended analyses to address responsiveness [25, 30]. Therefore, it is difficult to elucidate whether the EQ-5D-5L has problems with sensitivity to change in certain populations or with certain treatments. Despite this limitation, responsiveness is found to be acceptable by all included studies. A previous review found the EQ-5D-5L to be responsive to half of the conditions included, but found mixed evidence for the other half [26]. Responsiveness and sensitivity to changes in health is clearly an area that needs further investigation. Future studies could benefit from defining what a relevant change is for the EQ-5D-5L (MID) and defining appropriate anchor measures that can be used across populations (e.g., a level of change in EQ-VAS scores or a single self-rated health item). Parkin and colleagues (2016) demonstrated the EQ-5D-5L distribution to be affected both by the descriptive system and the value set applied [45]. Although not a focus of this study, the valuation method and applied utility scores are as important as the descriptive system when assessing responsiveness of index values. It has been shown that choice of value set has an impact on utility scores [46,47,48,49] and may change results of cost-utility analyses [48, 50, 51]. Other results show that the effect of value sets on utility scores is relatively small [A37, A83]. Due to the heterogeneity of studies found in this review, we have insufficient information to evaluate how value sets impact responsiveness. Future research will benefit from systematically examining responsiveness of the descriptive system and how choice of value set farther impacts responsiveness.
This review included nearly one hundred studies published in the past decade that investigated the psychometric properties of the EQ-5D-5L, the majority of which sample populations from western Europe, OECD countries and secondarily, from East Asia. This clearly reflects where the EQ-5D-5L is currently used [52]. However, almost a third of new user registrations in 2018 come from countries accounting for less than 1.5% of total registrations, demonstrating widespread as opposed to concentrated use of the instrument [52]. For instance, two reviews report rapid uptake of the instrument in Eastern Europe [53, 54]. Establishing validity in other regions is crucial as the EQ-5D-5L expands in its use. Similarly, as the EQ-5D instrument has expanded in its application, it would also be important to assess how well it performs in particular settings and applications, such as used to inform clinical practice, in health services research or in health surveillance programs.
Study limitations
A limitation of this study is that studies using experimental versions of the EQ-5D-5L were excluded. Early experimental work on the content validity of the instrument [55,56,57,58,59,60,61,62] and investigations of bolt-on items [63] are therefore not captured by this review. Similarly, due to the very large number and range of quality of studies identified, we did not include application studies of the EQ-5D-5L which did not explicitly address psychometric properties, and therefore are missing distributional and perhaps responsiveness information that may have been captured by those publications. As already discussed, choice of value set and valuation methodology are as important as the descriptive system in the case of the EQ-5D. This review does not address valuation methods and therefore does not tackle a crucial component of the instrument and its index value. A previous review of valuation methodology provides valuable information on this topic [64].
Conclusions
The EQ-5D-5L is a reliable and valid generic instrument that describes health status which can be applied to a broad range of populations and settings. The assessment of responsiveness, in particular, needs further and more rigorous exploration. Rather large ceilings persist in general population samples, reflecting the conceptualization of the EQ-5D instrument, which focuses on limitations in function and symptoms, and does not include positive aspects of health such as energy or well-being.
Abbreviations
- 15D:
-
15 measure of health-related quality of life
- ADL:
-
Activities of Daily Living
- AQoL-8D:
-
Assessment of Quality of Life (AQoL)-8D Multi-Attribute Utility Instrument
- BMI:
-
Body Mass Index
- BREAST-Q:
-
Breast surgery-specific patient-reported outcome measure
- DASS-21:
-
Depression, Anxiety and Stress Scale-21 Items
- DEMQOL:
-
Dementia Quality Of Life Questionnaire
- GAD:
-
Generalized Anxiety Disorder Scale
- JOABPEQ:
-
Japanese Orthopedic Association (JOA) Back Pain Evaluation Questionnaire
- EORTC:
-
European Organization for Research and Treatment of Cancer
- EQ-VAS:
-
Visual Analog Scale of the European Quality of Life-5 Dimensions (EQ-5D)
- FIM:
-
Functional Independence Measure
- HAL:
-
Hemophilia Activities List
- HUI3:
-
Health Utilities Index Mark 3
- K-BILD:
-
King’s Brief Interstitial Lung Disease Questionnaire
- KDQoL:
-
Kidney Disease Quality of Life Questionnaire
- MBI:
-
Modified Barthel Index
- MDS UPDRS:
-
Movement Disorder Society Unified Parkinson’s Disease Rating Scale (UPDRS)
- MRC:
-
Medical Research Council scales for muscle strength
- mRS:
-
Modified Rankin Scale
- NPI-Q:
-
Neuropsychiatric Inventory Questionnaire
- ODI:
-
Oswestry Disability Index
- PACT-Q2:
-
Perception of Anticoagulant Treatment Questionnaire (PACT-Q) Part 2
- PHQ-9:
-
Patient Health Questionnaire-9 Items
- PEmb-QoL:
-
Pulmonary Embolism Quality Of Life Questionnaire
- PGA:
-
Patient Global Assessment
- QOLIE-31P:
-
Quality of Life in Epilepsy-Patients-Weighted 31p
- PAS-cog:
-
Psychogeriatric Assessment Scale-Cognitive Impairment
- QWB:
-
Quality of Well-Being
- SF-6D:
-
Short Form-6 Dimensions
- SF-12(v2):
-
Short Form-12 Items Health Survey; v2—version 2 (Subscales: BP – Bodily Pain, GH – General Health, MH – Mental Health, PF, RE – Role Emotion, RP – Role Physical, SF – social functioning, VT – Vitality, Summary Scores: MCS – Mental Component Score, PCS – Physical Component Score)
- SF-36(v2):
-
Short Form-36 Items Health Survey; v2—version 2 (Subscales: BP – Bodily Pain, GH – General Health, MH – Mental Health, PF, RE – Role Emotion, RP – Role Physical, SF – social functioning, VT – Vitality, Summary Scores: MCS – Mental Component Score, PCS – Physical Component Score)
- SWLS:
-
Satisfaction with Life Scale
- WHO-5:
-
World Health Organization-5 Well-Being Index
- WHOQoL-BREF:
-
World Health Organization Quality of Life Assessment
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
References
Works Cited
Stolk, E., Ludwig, K., Rand, K., van Hout, B., & Ramos-Goni, J. M. (2019). Overview, update, and lessons learned from the international EQ-5D-5L valuation work: Version 2 of the EQ-5D-5L valuation Protocol. Value in Health, 22(1), 23–30.
Bharmal, M., & Thomas, J. (2006). Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the US general population. Value in Health, 9(4), 262–271.
Luo, N., Johnson, J. A., Shaw, J. W., & Coons, S. J. (2009). Relative efficiency of the EQ-5D, HUI2, and HUI3 index scores in measuring health burden of chronic medical conditions in a population health survey in the United States. Medical Care, 47(1), 53–60.
Palta, M., Chen, H. Y., Kaplan, R. M., Feeny, D., Cherepanov, D., & Fryback, D. G. (2011). Standard error of measurement of 5 health utility indexes across the range of health for use in estimating reliability and responsiveness. Medical Decision Making, 31(2), 260–269.
Tordrup, D., Mossman, J., & Kanavos, P. (2014). Responsiveness of the EQ-5D to clinical change: Is the patient experience adequately represented? International Journal of Technology Assessment in Health Care, 30(1), 10–19.
Brazier, J., Roberts, J., Tsuchiya, A., & Busschbach, J. (2004). A comparison of the EQ-5D and SF-6D across seven patient groups. Health Economics, 13(9), 873–884.
Cunillera, O., Tresserras, R., Rajmil, L., Vilagut, G., Brugulat, P., Herdman, M., et al. (2010). Discriminative capacity of the EQ-5D, SF-6D, and SF-12 as measures of health status in population health survey. Quality of Life Research, 19(6), 853–864.
Ferreira, L. N., Ferreira, P. L., & Pereira, L. N. (2014). Comparing the performance of the SF-6D and the EQ-5D in different patient groups. Acta Medica Portuguesa, 27(2), 236–245.
Kontodimopoulos, N., Pappa, E., Chadjiapostolou, Z., Arvanitaki, E., Papadopoulos, A. A., & Niakas, D. (2012). Comparing the sensitivity of EQ-5D, SF-6D and 15D utilities to the specific effect of diabetic complications. The European Journal of Health Economics, 13(1), 111–120.
Macran, S., Weatherly, H., & Kind, P. (2003). Measuring population health: a comparison of three generic health status measures. Medical Care, 41(2), 218–231.
EuroQol Research Foundation. (2019). EQ-5D-5L User Guide Version 3.0: Basic information on how to use the EQ-5D-5L instrument. https://euroqol.org/publications/user-guides.
Herdman, M., Gudex, C., Lloyd, A., Janssen, M., Kind, P., Parkin, D., et al. (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research, 20(10), 1727–1736.
EQ-5D website: EQ-5D-5L About. (2017). Retrieved 2019, from https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/.
Buchholz, I., Janssen, M. F., Kohlmann, T., & Feng, Y. S. (2018). A systematic review of studies comparing the measurement properties of the three-level and five-level versions of the EQ-5D. Pharmacoeconomics, 36(6), 645–661.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097.
Wan, X., Wang, W., Liu, J., & Tong, T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology, 14, 135.
Schafer, J. L. (1999). Multiple imputation: a primer. Statistical Methods in Medical Research, 8(1), 3–15.
Terwee, C. B., Bot, S. D. M., de Boer, M. R., van der Windt, D. A. W. M., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46.
Fleiss, J. L., & Cohen, J. (1973). The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educational and Psychological Measurement, 33, 613–619.
Shrout, P. E., & Fleiss, J. L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428.
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6(4), 284–290.
Deyo, R. A., & Centor, R. M. (1986). Assessing the responsiveness of functional scales to clinical change: An analogy to diagnostic test performance. Journal of Chronic Diseases, 39(11), 897–906.
Deyo, R. A., Diehr, P., & Patrick, D. L. (1991). Reproducibility and responsiveness of health status measures. Statistics and strategies for evaluation. Controlled Clinical Trials, 12(4 Suppl), 142S–158S.
Terwee, C. B., Dekker, F. W., Wiersinga, W. M., Prummel, M. F., & Bossuyt, P. M. (2003). On assessing responsiveness of health-related quality of life instruments: Guidelines for instrument evaluation. Quality of Life Research, 12(4), 349–362.
Payakachat, N., Ali, M. M., & Tilford, J. M. (2015). Can the EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics, 33(11), 1137–1154.
Revicki, D., Hays, R. D., Cella, D., & Sloan, J. (2008). Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. Journal of Clinical Epidemiology, 61(2), 102–109.
Revicki, D. A., Cella, D., Hays, R. D., Sloan, J. A., Lenderking, W. R., & Aaronson, N. K. (2006). Responsiveness and minimal important differences for patient reported outcomes. Health and Quality of Life Outcomes, 4, 70.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. New York: Routledge Academic.
Norman, G. R., Sridhar, F. G., Guyatt, G. H., & Walter, S. D. (2001). Relation of distribution- and anchor-based approaches in interpretation of changes in health-related quality of life. Medical Care, 39(10), 1039–1047.
R Core Team. (2013). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. http://www.R-project.org/.
Schwarzer, G. (2007). meta: An R package for meta-analysis. R News, 7(3), 40–45.
Devlin, N. J., & Brooks, R. (2017). EQ-5D and the EuroQol group: Past, present and future. Applied Health Economics and Health Policy, 15(2), 127–137.
Finch, A. P., Brazier, J. E., & Mukuria, C. (2018). What is the evidence for the performance of generic preference-based measures? A systematic overview of reviews. The European Journal of Health Economics, 19(4), 557–570.
Dyer, M. T., Goldsmith, K. A., Sharples, L. S., & Buxton, M. J. (2010). A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health and Quality of Life Outcomes, 8, 13.
Finch, A. P., Dritsaki, M., & Jommi, C. (2016). Generic preference-based measures for low back pain: Which of them should be used? Spine (Phila Pa 1976), 41(6), E364–E374.
Grobet, C., Marks, M., Tecklenburg, L., & Audige, L. (2018). Application and measurement properties of EQ-5D to measure quality of life in patients with upper extremity orthopaedic disorders: A systematic literature review. Archives of Orthopaedic and Trauma Surgery, 138(7), 953–961.
Pickard, A. S., Wilke, C. T., Lin, H. W., & Lloyd, A. (2007). Health utilities using the EQ-5D in studies of cancer. Pharmacoeconomics, 25(5), 365–384.
Yang, Y., Brazier, J., & Longworth, L. (2015). EQ-5D in skin conditions: An assessment of validity and responsiveness. The European Journal of Health Economics, 16(9), 927–939.
Janssen, M. F., Lubetkin, E. I., Sekhobo, J. P., & Pickard, A. S. (2011). The use of the EQ-5D preference-based health status measure in adults with Type 2 diabetes mellitus. Diabetic Medicine, 28(4), 395–413.
Round, J. (2018). Once bitten twice Shy: Thinking carefully before adopting the EQ-5D-5L. Pharmacoeconomics, 36(6), 641–643.
Yang, Y., Rowen, D., Brazier, J., Tsuchiya, A., Young, T., & Longworth, L. (2015). An exploratory study to test the impact on three “bolt-on” items to the EQ-5D. Value in Health, 18(1), 52–60.
Geraerds, A. J. L. M., Bonsel, G. J., Janssen, M. F., de Jongh, M. A., Spronk, I., Polinder, S., et al. (2019). The added value of the EQ-5D with a cognition dimension in injury patients with and without traumatic brain injury. Quality of Life Research, 28(7), 1931–1939.
Jelsma, J., & Maart, S. (2015). Should additional domains be added to the EQ-5D health-related quality of life instrument for community-based studies? (p. 13). Population Health Metrics: An analytical descriptive study.
Parkin, D., Devlin, N., & Feng, Y. (2016). What determines the shape of an EQ-5D index distribution? Medical Decision Making, 36(8), 941–951.
Kiadaliri, A. A., Eliasson, B., & Gerdtham, U. G. (2015). Does the choice of EQ-5D tariff matter? A comparison of the Swedish EQ-5D-3L index score with UK, US, Germany and Denmark among type 2 diabetes patients. Health and Quality of Life Outcomes, 13, 145.
Zhao, Y., Li, S. P., Liu, L., Zhang, J. L., & Chen, G. (2017). Does the choice of tariff matter? A comparison of EQ-5D-5L utility scores using Chinese, UK, and Japanese tariffs on patients with psoriasis vulgaris in Central South China. Medicine (Baltimore), 96(34), e7840.
Mulhern, B., Feng, Y., Shah, K., Janssen, M. F., Herdman, M., van Hout, B., et al. (2018). Comparing the UK EQ-5D-3L and English EQ-5D-5L Value Sets (vol 36, pg 699, 2018). Pharmacoeconomics, 36(6), 727–727.
Gerlinger, C., Bamber, L., Leverkus, F., Schwenke, C., Haberland, C., Schmidt, G., et al. (2019). Comparing the EQ-5D-5L utility index based on value sets of different countries: Impact on the interpretation of clinical study results. BMC Research Notes, 12(1), 18.
Yang, F., Devlin, N., & Luo, N. (2019). Cost-utility analysis using EQ-5D-5L data: Does how the utilities are derived matter? Value in Health, 22(1), 45–49.
Lien, K., Tam, V. C., Ko, Y. J., Mittmann, N., Cheung, M. C., & Chan, K. K. W. (2015). Impact of country-specific EQ-5D-3L tariffs on the economic value of systemic therapies used in the treatment of metastatic pancreatic cancer. Current Oncology, 22(6), E443–E452.
EuroQol. (2018). Where is EQ-5D used? Retrieved December 03, 2019, from https://euroqol.org/eq-5d-instruments/how-can-eq-5d-be-used/where-is-eq-5d-used/.
Rencz, F., Gulacsi, L., Drummond, M., Golicki, D., Prevolnik Rupel, V., Simon, J., et al. (2016). EQ-5D in Central and eastern Europe: 2000-2015. Quality of Life Research, 25(11), 2693–2710.
Zrubka, Z., Rencz, F., Zavada, J., Golicki, D., Rupel, V. P., Simon, J., et al. (2017). EQ-5D studies in musculoskeletal and connective tissue diseases in eight Central and Eastern European countries: A systematic literature review and meta-analysis. Rheumatology International, 37(12), 1957–1977.
Luo, N., Li, M., Chevalier, J., Lloyd, A., & Herdman, M. (2013). A comparison of the scaling properties of the English, Spanish, French, and Chinese EQ-5D descriptive systems. Quality of Life Research, 22(8), 2237–2243.
Luo, N., Li, M., & Liu, G. (2009). Investigation of Labels for a 5-level EQ-5D descriptive system in Chinese. EuroQol Proceedings, 26, 77–102.
Luo, N., Li, M., Liu, G. G., Lloyd, A., de Charro, C., & Herdman, M. (2013). Developing the Chinese version of the new 5-level EQ-5D descriptive system: The response scaling approach. Quality of Life Research, 22(4), 885–890.
Luo, N., Wang, Y., How, C. H., Tay, E. G., Thumboo, J., & Herdman, M. (2015). Interpretation and use of the 5-level EQ-5D response labels varied with survey language among Asians in Singapore. Journal of Clinical Epidemiology, 68(10), 1195–1204.
Janssen, M. F., Birnie, E., & Bonsel, G. J. (2008). Quantification of the level descriptors for the standard EQ-5D three-level system and a five-level version according to two methods. Quality of Life Research, 17(3), 463–473.
Pickard, A. S., De Leon, M. C., Kohlmann, T., Cella, D., & Rosenbloom, S. (2007). Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Medical Care, 45(3), 259–263.
Pickard, A. S., Kohlmann, T., Janssen, M. F., Bonsel, G., Rosenbloom, S., & Cella, D. (2007). Evaluating equivalency between response systems: Application of the Rasch model to a 3-level and 5-level EQ-5D. Medical Care, 45(9), 812–819.
Chevalier, J., & De Pouvourville, G. (2008). Testing a new 5 level version of the EQ-5D in France. EuroQol Proceedings, 14, 75–88.
Finch, A. P., Brazier, J. E., Mukuria, C., & Bjorner, J. B. (2017). An exploratory study on using principal-component analysis and confirmatory factor analysis to identify bolt-on dimensions: The EQ-5D case study. Value in Health, 20(10), 1362–1375.
Xie, F., Gaebel, K., Perampaladas, K., Doble, B., & Pullenayegum, E. (2014). Comparing EQ-5D Valuation Studies: A systematic review and methodological reporting checklist. Medical Decision Making, 34(1), 8–20.
References for publications included for review
Scalone, L. (2011). Comparing the standard EQ-5D-3L versus 5L version for the assessment of health of patients with live diseases. EuroQol Proceedings, 16, 213–239.
Kim, S. H., Kim, H. J., Lee, S. I., & Jo, M. W. (2012). Comparing the psychometric properties of the EQ-5D-3L and EQ-5D-5L in cancer patients in Korea. Quality of Life Research, 21(6), 1065–1073.
Tran, B. X., Ohinmaa, A., & Nguyen, L. T. (2012). Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health and Quality of Life Outcomes, 10, 132.
van Hout, B., Janssen, M. F., Feng, Y. S., Kohlmann, T., Busschbach, J., Golicki, D., et al. (2012). Interim scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L value sets. Value. Health, 15(5), 708–715.
Augustovski, F., Rey-Ares, L., Irazola, V., Oppe, M., & Devlin, N. J. (2013). Lead versus lag-time trade-off variants: Does it make any difference? The European Journal of Health Economics, 14(Suppl 1), S25–S31.
Janssen, M. F., Pickard, A. S., Golicki, D., Gudex, C., Niewada, M., Scalone, L., et al. (2013). Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: A multi-country study. Quality of Life Research, 22(7), 1717–1727.
Keeley, T., Al-Janabi, H., Lorgelly, P., & Coast, J. (2013). A qualitative assessment of the content validity of the ICECAP-A and EQ-5D-5L and their appropriateness for use in health research. PLoS ONE, 8(12), e85287.
Kim, T. H., Jo, M. W., Lee, S. I., Kim, S. H., & Chung, S. M. (2013). Psychometric properties of the EQ-5D-5L in the general population of South Korea. Quality of Life Research, 22(8), 2245–2253.
Lee, C. F., Luo, N., Ng, R., Wong, N. S., Yap, Y. S., Lo, S. K., et al. (2013). Comparison of the measurement properties between a short and generic instrument, the 5-level EuroQoL Group’s 5-dimension (EQ-5D-5L) questionnaire, and a longer and disease-specific instrument, the Functional Assessment of Cancer Therapy-Breast (FACT-B), in Asian breast cancer patients. Quality of Life Research, 22(7), 1745–1751.
Scalone, L., Ciampichini, R., Fagiuoli, S., Gardini, I., Fusco, F., Gaeta, L., et al. (2013). Comparing the performance of the standard EQ-5D 3L with the new version EQ-5D 5L in patients with chronic hepatic diseases. Quality of Life Research, 22(7), 1707–1716.
Swan, J. S., Hur, C., Lee, P., Motazedi, T., & Donelan, K. (2013). Responsiveness of the testing morbidities index in colonoscopy. Value in Health, 16(6), 1046–1053.
Swinburn, P., Lloyd, A., Boye, K. S., Edson-Heredia, E., Bowman, L., & Janssen, B. (2013). Development of a disease-specific version of the EQ-5D-5L for use in patients suffering from psoriasis: Lessons learned from a feasibility study in the UK. Value. Health, 16(8), 1156–1162.
Agborsangaya, C. B., Lahtinen, M., Cooke, T., & Johnson, J. A. (2014). Comparing the EQ-5D 3L and 5L: Measurement properties and association with chronic conditions and multimorbidity in the general population. Health and Quality of Life Outcomes, 12, 74.
Au, N., & Lorgelly, P. K. (2014). Anchoring vignettes for health comparisons: An analysis of response consistency. Quality of Life Research, 23(6), 1721–1731.
Craig, B. M., Pickard, A. S., & Lubetkin, E. I. (2014). Health problems are more common, but less severe when measured using newer EQ-5D versions. Journal of Clinical Epidemiology, 67(1), 93–99.
Garcia-Gordillo, M., del Pozo-Cruz, B., Adsuar, J. C., Sanchez-Martinez, F. I., & Bellan-Perpinan, J. M. (2014). Validation and comparison of 15-D and EQ-5D-5L instruments in a Spanish Parkinson’s disease population sample. Quality of Life Research, 23(4), 1315–1326.
Hinz, A., Kohlmann, T., Stobel-Richter, Y., Zenger, M., & Brahler, E. (2014). The quality of life questionnaire EQ-5D-5L: Psychometric properties and normative values for the general German population. Quality of Life Research, 23(2), 443–447.
Jia, Y. X., Cui, F. Q., Li, L., Zhang, D. L., Zhang, G. M., Wang, F. Z., et al. (2014). Comparison between the EQ-5D-5L and the EQ-5D-3L in patients with hepatitis B. Quality of Life Research, 23(8), 2355–2363.
Lin, F. J., Pickard, A. S., Krishnan, J. A., Joo, M. J., Au, D. H., Carson, S. S., et al. (2014). Measuring health-related quality of life in chronic obstructive pulmonary disease: Properties of the EQ-5D-5L and PROMIS-43 short form. BMC Medical Research Methodology, 14, 78.
Mihalopoulos, C., Chen, G., Iezzi, A., Khan, M. A., & Richardson, J. (2014). Assessing outcomes for cost-utility analysis in depression: comparison of five multi-attribute utility instruments with two depression-specific outcome measures. British Journal of Psychiatry, 205(5), 390–397.
Whitehurst, D. G., Suryaprakash, N., Engel, L., Mittmann, N., Noonan, V. K., Dvorak, M. F., et al. (2014). Perceptions of individuals living with spinal cord injury toward preference-based quality of life instruments: A qualitative exploration. Health and Quality of Life Outcomes, 12, 50.
Alvarado-Bolanos, A., Cervantes-Arriaga, A., Rodriguez-Violante, M., Llorens-Arenas, R., Calderon-Fajardo, H., Millan-Cepeda, R., et al. (2015). Convergent validation of EQ-5D-5L in patients with Parkinson’s disease. Journal of the Neurological Sciences, 358(1–2), 53–57.
Buchholz, I., Thielker, K., Feng, Y. S., Kupatz, P., & Kohlmann, T. (2015). Measuring changes in health over time using the EQ-5D 3L and 5L: A head-to-head comparison of measurement properties and sensitivity to change in a German inpatient rehabilitation sample. Quality of Life Research, 24(4), 829–835.
Conner-Spady, B. L., Marshall, D. A., Bohm, E., Dunbar, M. J., Loucks, L., Al, K. A., et al. (2015). Reliability and validity of the EQ-5D-5L compared to the EQ-5D-3L in patients with osteoarthritis referred for hip and knee replacement. Quality of Life Research, 24(7), 1775–1784.
Feng, Y., Devlin, N., & Herdman, M. (2015). Assessing the health of the general population in England: How do the three- and five-level versions of EQ-5D compare? Health and Quality of Life Outcomes, 13, 171.
Gamst-Klaussen, T., Chen, G., Lamu, A. N., & Olsen, J. A. (2015). Health state utility instruments compared: inquiring into nonlinearity across EQ-5D-5L, SF-6D, HUI-3 and 15D. Quality of Life Research, 25(7), 1667–1678.
Golicki, D., Niewada, M., Buczek, J., Karlinska, A., Kobayashi, A., Janssen, M. F., et al. (2015). Validity of EQ-5D-5L in stroke. Quality of Life Research, 24(4), 845–850.
Golicki, D., Niewada, M., Karlinska, A., Buczek, J., Kobayashi, A., Janssen, M. F., et al. (2015). Comparing responsiveness of the EQ-5D-5L, EQ-5D-3L and EQ VAS in stroke patients. Quality of Life Research, 24(6), 1555–1563.
Greene, M. E., Rader, K. A., Garellick, G., Malchau, H., Freiberg, A. A., & Rolfson, O. (2015). The EQ-5D-5L improves on the EQ-5D-3L for health-related quality-of-life assessment in patients undergoing total hip arthroplasty. Clinical Orthopaedics and Related Research, 473(11), 3383–3390.
Luo, N., Wang, Y., How, C. H., Wong, K. Y., Shen, L., Tay, E. G., et al. (2015). Cross-cultural measurement equivalence of the EQ-5D-5L items for English-speaking Asians in Singapore. Quality of Life Research, 24(6), 1565–1574.
Mitchell, P. M., Al-Janabi, H., Richardson, J., Iezzi, A., & Coast, J. (2015). The relative impacts of disease on health status and capability wellbeing: A multi-country study. PLoS ONE, 10(12), e0143590.
Mulhern, B., O’Gorman, H., Rotherham, N., & Brazier, J. (2015). Comparing the measurement equivalence of EQ-5D-5L across different modes of administration. Health and Quality of Life Outcomes, 13, 191.
O’Leary, E., Drummond, F. J., Gavin, A., Kinnear, H., & Sharp, L. (2015). Psychometric evaluation of the EORTC QLQ-PR25 questionnaire in assessing health-related quality of life in prostate cancer survivors: A curate’s egg. Quality of Life Research, 24(9), 2219–2230.
Pan, C. W., Sun, H. P., Wang, X., Ma, Q., Xu, Y., Luo, N., et al. (2015). The EQ-5D-5L index score is more discriminative than the EQ-5D-3L index score in diabetes patients. Quality of Life Research, 24(7), 1767–1774.
Pattanaphesaj, J., & Thavorncharoensap, M. (2015). Measurement properties of the EQ-5D-5L compared to EQ-5D-3L in the Thai diabetes patients. Health and Quality of Life Outcomes, 13, 14.
Richardson, J., Chen, G., Khan, M. A., & Iezzi, A. (2015). Can multi-attribute utility instruments adequately account for subjective well-being? Medical Decision Making, 35(3), 292–304.
Richardson, J., Iezzi, A., & Khan, M. A. (2015). Why do multi-attribute utility instruments produce different utilities: The relative importance of the descriptive systems, scale and ‘micro-utility’ effects. Quality of Life Research, 24(8), 2045–2053.
Richardson, J., Khan, M. A., Iezzi, A., & Maxwell, A. (2015). Comparing and explaining differences in the magnitude, content, and sensitivity of utilities predicted by the EQ-5D, SF-6D, HUI 3, 15D, QWB, and AQoL-8D multiattribute utility instruments. Medical Decision Making, 35(3), 276–291.
Sakthong, P., Sonsa-Ardjit, N., Sukarnjanaset, P., & Munpan, W. (2015). Psychometric properties of the EQ-5D-5L in Thai patients with chronic diseases. Quality of Life Research, 24(12), 3015–3022.
Scalone, L., Cortesi, P. A., Ciampichini, R., Cesana, G., & Mantovani, L. G. (2015). Health Related Quality of Life norm data of the general population in Italy: Results using the EQ-5D-3L and EQ-5D-5L instruments. Epidemiology Biostatistics and Public Health, 12(3), e11457.
Shiroiwa, T., Fukuda, T., Ikeda, S., Igarashi, A., Noto, S., Saito, S., et al. (2015). Japanese population norms for preference-based measures: Eq-5d-3 l, Eq-5d-5 l, and Sf-6d. Value. Health, 18(7), A738.
Wang, Y., Tan, N. C., Tay, E. G., Thumboo, J., & Luo, N. (2015). Cross-cultural measurement equivalence of the 5-level EQ-5D (EQ-5D-5L) in patients with type 2 diabetes mellitus in Singapore. Health and Quality of Life Outcomes, 13, 103.
White, J., Withers, K. L., Lencioni, M., Carolan-Rees, G., Wilkes, A. R., Wood, K. A., et al. (2015). Cardiff cardiac ablation patient-reported outcome measure (C-CAP): validation of a new questionnaire set for patients undergoing catheter ablation for cardiac arrhythmias in the UK. Quality of Life Research, 25(6), 1571–1583.
Yang, F., Lau, T., Lee, E., Vathsala, A., Chia, K. S., & Luo, N. (2015). Comparison of the preference-based EQ-5D-5L and SF-6D in patients with end-stage renal disease (ESRD). The European Journal of Health Economics, 16(9), 1019–1026.
Augustovski, F., Rey-Ares, L., Irazola, V., Garay, O. U., Gianneo, O., Fernandez, G., et al. (2016). An EQ-5D-5L value set based on Uruguayan population preferences. Quality of Life Research, 25(2), 323–333.
Chen, P., Lin, K. C., Liing, R. J., Wu, C. Y., Chen, C. L., & Chang, K. C. (2016). Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Quality of Life Research, 25(6), 1585–1596.
Ferreira, L. N., Ferreira, P. L., Pereira, L. N., & Antunes, P. (2016). Comparing Eq-5d-3 l and Eq-5d-5 l in a general population. Value in Health, 19(7), A477.
Garcia-Gordillo, M. A., Collado-Mateo, D., Olivares, P. R., & Adsuar, J. C. (2016). Application of EQ-5D-5L questionnaire in patients suffering from urinary incontinence. Actas Urologicas Espanolas, 40(7), 457–462.
Lamu, A. N., & Olsen, J. A. (2016). The relative importance of health, income and social relations for subjective well-being: An integrative analysis. Social Science and Medicine, 152, 176–185.
McCaffrey, N., Kaambwa, B., Currow, D. C., & Ratcliffe, J. (2016). Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health and Quality of Life Outcomes, 14(1), 133.
Nolan, C. M., Longworth, L., Lord, J., Canavan, J. L., Jones, S. E., Kon, S. S., et al. (2016). The EQ-5D-5L health status questionnaire in COPD: Validity, responsiveness and minimum important difference. Thorax, 71(6), 493–500.
Oremus, M., Xie, F., Pullenayegum, E., & Gaebel, K. (2016). Can the general public use vignettes to discriminate between Alzheimer’s disease health states? BMC Geriatrics, 16, 36.
Richardson, J., Iezzi, A., Khan, M. A., Chen, G., & Maxwell, A. (2016). Measuring the sensitivity and construct validity of 6 utility instruments in 7 disease areas. Medical Decision Making, 36(2), 147–159.
Rogers, K. D., Pilling, M., Davies, L., Belk, R., Nassimi-Green, C., & Young, A. (2016). Translation, validity and reliability of the British Sign Language (BSL) version of the EQ-5D-5L. Quality of Life Research, 25(7), 1825–1834.
Wang, P., Luo, N., Tai, E. S., & Thumboo, J. (2016). The EQ-5D-5L is more discriminative than the EQ-5D-3L in patients with diabetes in Singapore. Value in Health Regional Issues, 9, 57–62.
Whitehurst, D. G., Mittmann, N., Noonan, V. K., Dvorak, M. F., & Bryan, S. (2016). Health state descriptions, valuations and individuals’ capacity to walk: A comparative evaluation of preference-based instruments in the context of spinal cord injury. Quality of Life Research, 25, 2481–2496.
Bhadhuri, A., Jowett, S., Jolly, K., & Al-Janabi, H. (2017). A comparison of the validity and responsiveness of the EQ-5D-5L and SF-6D for measuring health spillovers: A study of the family impact of meningitis. Medical Decision Making, 37(8), 882–893.
Feng, Y., Herdman, M., van Nooten, F., Cleeland, C., Parkin, D., Ikeda, S., et al. (2017). An exploration of differences between Japan and two European countries in the self-reporting and valuation of pain and discomfort on the EQ-5D. Quality of Life Research, 26(8), 2067–2078.
Fermont, J. M., Blazeby, J. M., Rogers, C. A., Wordsworth, S., on behalf of the By-Band-Sleeve Study Management Group. (2017). The EQ-5D-5L is a valid approach to measure health related quality of life in patients undergoing bariatric surgery. PLoS ONE, 12(12), e0189190.
Huber, M. B., Felix, J., Vogelmann, M., & Leidl, R. (2017). Health-related quality of life of the general German population in 2015: Results from the EQ-5D-5L. International Journal of Environmental Research and Public Health, 14(4), 426.
Konnopka, A., & Koenig, H. H. (2017). The “no problems”-problem: An empirical analysis of ceiling effects on the EQ-5D 5L. Quality of Life Research, 26(8), 2079–2084.
Nguyen, L. H., Tran, B. X., Hoang Le, Q. N., Tran, T. T., & Latkin, C. A. (2017). Quality of life profile of general Vietnamese population using EQ-5D-5L. Health and Quality of Life Outcomes, 15(1), 199.
Poor, A. K., Rencz, F., Brodszky, V., Gulacsi, L., Beretzky, Z., Hidvegi, B., et al. (2017). Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L in psoriasis patients. Quality of Life Research, 26(12), 3409–3419.
Yfantopoulos, J., Chantzaras, A., & Kontodimas, S. (2017). Assessment of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in psoriasis. Archives of Dermatological Research, 309(5), 357–370.
Yfantopoulos, J. N., & Chantzaras, A. E. (2017). Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. The European Journal of Health Economics, 18(4), 519–531.
Batt, K., Boggio, L., Neff, A., Buckner, T. W., Wang, M., Quon, D., et al. (2018). Patient-reported outcomes and joint status across subgroups of US adults with hemophilia with varying characteristics: Results from the Pain, Functional Impairment, and Quality of Life (P-FiQ) study. European Journal of Haematology, 100(Suppl 1), 14–24.
Bewick, J., Morris, S., Hopkins, C., Erskine, S., & Philpott, C. M. (2018). Health utility reporting in chronic rhinosinusitis patients. Clinical Otolaryngology, 43(1), 90–95.
Bilbao, A., Garcia-Perez, L., Arenaza, J. C., Garcia, I., Ariza-Cardiel, G., Trujillo-Martin, E., et al. (2018). Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: Reliability, validity and responsiveness. Quality of Life Research, 27(11), 2897–2908.
Buckner, T. W., Sidonio, R., Jr., Guelcher, C., Kessler, C. M., Witkop, M., Clark, D., et al. (2018). Reliability and validity of patient-reported outcome instruments in US adults with hemophilia B and caregivers in the B-HERO-S study. European Journal of Haematology, 101(6), 781–790.
Camacho, E. M., Shields, G., Lovell, K., Coventry, P. A., Morrison, A. P., & Davies, L. M. (2018). A (five-)level playing field for mental health conditions?: Exploratory analysis of EQ-5D-5L-derived utility values. Quality of Life Research, 27(3), 717–724.
Campbell, J. A., Hensher, M., Neil, A., Venn, A., Wilkinson, S., & Palmer, A. J. (2018). An exploratory study of long-term publicly waitlisted bariatric surgery patients’ quality of life before and 1 year after bariatric surgery, and considerations for healthcare planners. Pharmacoeconomics-Open, 2(1), 63–76.
Cheung, P. W. H., Wong, C. K. H., & Cheung, J. P. Y. (2018). Differential psychometric properties of EuroQoL 5-dimension 5-level and short-form 6-dimension utility measures in low back pain. Spine, 44(11), E679–E686.
Conner-Spady, B. L., Marshall, D. A., Bohm, E., Dunbar, M. J., & Noseworthy, T. W. (2018). Comparing the validity and responsiveness of the EQ-5D-5L to the Oxford hip and knee scores and SF-12 in osteoarthritis patients 1 year following total joint replacement. Quality of Life Research, 27(5), 1311–1322.
Crick, K., Al Sayah, F., Ohinmaa, A., & Johnson, J. A. (2018). Responsiveness of the anxiety/depression dimension of the 3- and 5-level versions of the EQ-5D in assessing mental health. Quality of Life Research, 27(6), 1625–1633.
Easton, T., Milte, R., Crotty, M., & Ratcliffe, J. (2018). An empirical comparison of the measurement properties of the EQ-5D-5L, DEMQOL-U and DEMQOL-Proxy-U for older people in residential care. Quality of Life Research, 27(5), 1283–1294.
Efthymiadou, O., Mossman, J., & Kanavos, P. (2018). Differentiation of health-related quality of life outcomes between five disease areas: Results from an international survey of patients. International Journal of Technology Assessment in Health Care, 34(5), 498–506.
Engel, L., Chen, G., Richardson, J., & Mihalopoulos, C. (2018). The impact of depression on health-related quality of life and wellbeing: Identifying important dimensions and assessing their inclusion in multi-attribute utility instruments. Quality of Life Research, 27(11), 2873–2884.
Fan, X., Wang, D., Hellman, B., Janssen, M. F., Bakker, G., Coghlan, R., et al. (2018). Assessment of health-related quality of life between people with Parkinson’s disease and non-Parkinson’s: Using data drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study. International Journal of Environmental Research and Public Health, 15(11), 2538.
Gamst-Klaussen, T., Gudex, C., & Olsen, J. A. (2018). Exploring the causal and effect nature of EQ-5D dimensions: An application of confirmatory tetrad analysis and confirmatory factor analysis. Health and Quality of Life Outcomes, 16(1), 153.
Ge, L., Ong, R., Yap, C. W., & Heng, B. H. (2018). Effects of chronic diseases on health-related quality of life and self-rated health among three adult age groups. Nursing & Health Sciences, 21(2), 214–222.
Hernandez, G., Garin, O., Pardo, Y., Vilagut, G., Pont, A., Suarez, M., et al. (2018). Validity of the EQ-5D-5L and reference norms for the Spanish population. Quality of Life Research, 27(9), 2337–2348.
Huber, M., Vogelmann, M., & Leidl, R. (2018). Valuing health-related quality of life: Systematic variation in health perception. Health and Quality of Life Outcomes, 16(1), 156.
Janssen, M. F., Bonsel, G. J., & Luo, N. (2018). Is EQ-5D-5L better than EQ-5D-3L? A head-to-head comparison of descriptive systems and value sets from seven countries. Pharmacoeconomics, 36(6), 675–697.
Kohler, S., Sidney Annerstedt, K., Diwan, V., Lindholm, L., Randive, B., Vora, K., et al. (2018). Postpartum quality of life in Indian women after vaginal birth and cesarean section: A pilot study using the EQ-5D-5L descriptive system. BMC Pregnancy Childbirth, 18(1), 427.
Lagendijk, M., van Egdom, L. S. E., van Veen, F. E. E., Vos, E. L., Mureau, M. A. M., van Leeuwen, N., et al. (2018). Patient-reported outcome measures may add value in breast cancer surgery. Annals of Surgical Oncology, 25(12), 3563–3571.
Marti-Pastor, M., Pont, A., Avila, M., Garin, O., Vilagut, G., Forero, C. G., et al. (2018). Head-to-head comparison between the EQ-5D-5L and the EQ-5D-3L in general population health surveys. Population Health Metrics, 16(1), 14.
McClure, N. S., Sayah, F. A., Ohinmaa, A., & Johnson, J. A. (2018). Minimally important difference of the EQ-5D-5L index score in adults with type 2 diabetes. Value in Health, 21(9), 1090–1097.
Purba, F. D., Hunfeld, J. A. M., Iskandarsyah, A., Fitriana, T. S., Sadarjoen, S. S., Passchier, J., et al. (2018). Quality of life of the Indonesian general population: Test-retest reliability and population norms of the EQ-5D-5L and WHOQOL-BREF. PLoS ONE, 13(5), e0197098.
Szentes, B. L., Kreuter, M., Bahmer, T., Birring, S. S., Claussen, M., Waelscher, J., et al. (2018). Quality of life assessment in interstitial lung diseases: A comparison of the disease-specific K-BILD with the generic EQ-5D-5L. Respiratory Research, 19(1), 101.
Tamasi, B., Brodszky, V., Pentek, M., Gulacsi, L., Hajdu, K., Sardy, M., et al. (2018). Validity of the EQ-5D in patients with pemphigus vulgaris and pemphigus foliaceus. British Journal of Dermatology, 180(4), 802–809.
Thaweethamcharoen, T., Noparatayaporn, P., Sritippayawan, S., & Aiyasanon, N. (2018). Comparison of EQ-5D-5L, VAS, and SF-6D in Thai patients on peritoneal dialysis. Value in Health Regional Issues, 18, 59–64.
Whalley, D., Globe, G., Crawford, R., Doward, L., Tafesse, E., Brazier, J., et al. (2018). Is the EQ-5D fit for purpose in asthma? Acceptability and content validity from the patient perspective. Health and Quality of Life Outcomes, 16(1), 160.
Wijnen, B. F. M., Mosweu, I., Majoie, M., Ridsdale, L., de Kinderen, R. J. A., Evers, S., et al. (2018). A comparison of the responsiveness of EQ-5D-5L and the QOLIE-31P and mapping of QOLIE-31P to EQ-5D-5L in epilepsy. The European Journal of Health Economics, 19(6), 861–870.
Chuang, L. H., Cohen, A. T., Agnelli, G., Gumbs, P. D., Bauersachs, R., Kroep, S., et al. (2019). Comparison of quality of life measurements: EQ-5D-5L versus disease/treatment-specific measures in pulmonary embolism and deep vein thrombosis. Quality of Life Research, 28(5), 1155–1177.
Gandhi, M., Ang, M., Teo, K., Wong, C. W., Wei, Y. C., Tan, R. L., et al. (2019). EQ-5D-5L is more responsive than EQ-5D-3L to treatment benefit of cataract surgery. Patient, 12(4), 383–392.
Gao, L., Moodie, M., & Chen, G. (2019). Measuring subjective wellbeing in patients with heart disease: Relationship and comparison between health-related quality of life instruments. Quality of Life Research, 28(4), 1017–1028.
Hernandez, G., Garin, O., Dima, A. L., Pont, A., Marti Pastor, M., Alonso, J., et al. (2019). EuroQol (EQ-5D-5L) validity in assessing the quality of life in adults with asthma: Cross-sectional study. Journal of Medical Internet Research, 21(1), e10178.
Kouwenberg, C. A. E., Kranenburg, L. W., Visser, M. S., Busschbach, J. J., & Mureau, M. A. M. (2019). The validity of the EQ-5D-5L in measuring quality of life benefits of breast reconstruction. Journal of Plastic, Reconstructive & Aesthetic Surgery, 72(1), 52–61.
Rencz, F., Lakatos, P. L., Gulacsi, L., Brodszky, V., Kurti, Z., Lovas, S., et al. (2019). Validity of the EQ-5D-5L and EQ-5D-3L in patients with Crohn’s disease. Quality of Life Research, 28(1), 141–152.
Acknowledgements
EuroQol Research Foundation fully funded this project (Grant ID EQ Project 2016170).
Funding
Open Access funding enabled and organized by Projekt DEAL. The submitted manuscript was not censored or directed by the foundation. The views expressed by the authors in the publication do not necessarily reflect the view of the EuroQol Group.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All four authors are members of the EuroQol group. Outside of scientific meetings, group members do not receive any financial support.
Ethical approval
This is a review paper and therefore none of the authors conducted human or animal data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feng, YS., Kohlmann, T., Janssen, M.F. et al. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res 30, 647–673 (2021). https://doi.org/10.1007/s11136-020-02688-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02688-y