Abstract
Purpose
Chronic kidney disease (CKD) affects over 10% of the global population. Health-related quality of life (HRQoL) has been identified as a reliable indicator for assessing the effectiveness of treatment in chronic patients, and resilience as a predictor of low levels of stress and higher QoL. The aim of this research is to identify the relationship between HRQoL, resilience, perceived stress, and the different sociodemographic and clinical routine variables of advanced chronic kidney disease (ACKD).
Methods
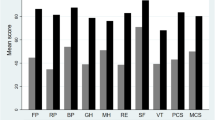
Multicenter, cross-sectional, and correlational study with 155 ACKD patients in the Valencian Community (Spain). The measures for the study included the Kidney Disease Quality of Life 36 (KDQOL-36), the Perceived Stress Scale 10 (PSS10), and the Connors–Davidson Resilience Scale (CD-RISC). To identify the variables with predictive power over the scales and subscales of the KDQOL-36, multiple regression analyses were performed.
Results
Average participants’ age was 67.39, 68.4% were male, 29% diabetic, and 83.2% had undergone arteriovenous vascular access placement with a Charlson Comorbidity Index of 6 (SD = 2.09). The regression models identified that age and resilience explained up to 26.8% of the variance of the KDQOL-36 total score. As for the physical component of QoL, comorbidity with other clinical conditions, resilience, and the presence of diabetes explained 32.1% of its variance.
Conclusions
Resilience was identified as one of the most important predictors of HRQoL. Thus, the development of interventions aiming to improve the level of resilience may have a positive impact over the quality of life of patients with CKD.
Similar content being viewed by others
References
Eckardt, K. U., Coresh, J., Devuyst, O., Johnson, R. J., Köttgen, A., Levey, A. S., et al. (2013). Evolving importance of kidney disease: From subspecialty to global health burden. The Lancet. https://doi.org/10.1016/S0140-6736(13)60439-0.
de Vries, A. M., Schulz, T., Westerhuis, R., Navis, G. J., Niesing, J., Ranchor, A. V., et al. (2017). Goal disturbance changes pre/post-renal transplantation are related to changes in distress. British Journal of Health Psychology,22(3), 524–541. https://doi.org/10.1111/bjhp.12243.
Registro Español de Enfermos Renales. (2018). Informe de diálisis y transplante 2017. Madrid. Retrieved from https://www.registrorenal.es/download/documentacion/Informe_REER_2017.pdf
Tonelli, M., Wiebe, N., Knoll, G., Bello, A., Browne, S., Jadhav, D., et al. (2011). Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. American Journal of Transplantation,11(10), 2093–2109. https://doi.org/10.1111/j.1600-6143.2011.03686.x.
Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney disease. The Lancet,389(10075), 1238–1252. https://doi.org/10.1016/S0140-6736(16)32064-5.
Wang, R., Tang, C., Chen, X., Zhu, C., Feng, W., Li, P., et al. (2016). Poor sleep and reduced quality of life were associated with symptom distress in patients receiving maintenance hemodialysis. Health and Quality of Life Outcomes. https://doi.org/10.1186/s12955-016-0531-6.
Liu, Y. M., Chang, H. J., Wang, R. H., Yang, L. K., Lu, K. C., & Hou, Y. C. (2018). Role of resilience and social support in alleviating depression in patients receiving maintenance hemodialysis. Therapeutics and Clinical Risk Management,14, 441–451. https://doi.org/10.2147/TCRM.S152273.
Finkelstein, F. O., Wuerth, D., & Finkelstein, S. H. (2009). Health related quality of life and the CKD patient: Challenges for the nephrology community. Kidney International,76(9), 946–952. https://doi.org/10.1038/ki.2009.307.
Lowrie, E. G., Curtin, R. B., LePain, N., & Schatell, D. (2003). Medical Outcomes Study Short Form-36: A consistent and powerful predictor of morbidity and mortality in dialysis patients. American Journal of Kidney Diseases,41(6), 1286–1292. https://doi.org/10.1016/S0272-6386(03)00361-5.
Mandzuk, L. L., & McMillan, D. E. (2005). A concept analysis of quality of life. Journal of Orthopaedic Nursing,9(1), 12–18. https://doi.org/10.1016/j.joon.2004.11.001.
Mapes, D. L., Lopes, A. A., Satayathum, S., McCullough, K. P., Goodkin, D. A., Locatelli, F., et al. (2003). Health-related quality of life as a predictor of mortality and hospitalization: The dialysis outcomes and practice patterns study (DOPPS). Kidney International,64(1), 339–349. https://doi.org/10.1046/j.1523-1755.2003.00072.x.
Rebollo-Rubio, A., Morales-Asencio, J. M., Pons-Raventos, M. E., & Mansilla-Francisco, J. J. (2015). Revisión de estudios sobre calidad de vida relacionada con la salud en la enfermedad renal crónica avanzada en España. Nefrologia,35(1), 92–109. https://doi.org/10.3265/Nefrologia.pre2014.Jul.12133.
Hays, R. D., Kallich, J. D., Mapes, D. L., Coons, S. J., & Carter, W. B. (1994). Development of the Kidney Disease Quality of Life (KDQOLTM) Instrument. Quality of Life Research,3(5), 329–338. https://doi.org/10.1007/BF00451725.
Rand Health Corporation. (n.d.). Kidney Disease Quality of Life Instrument (KDQOL). Rand Corporation Website. Retrieved October 5, 2019, from rand.org/health/%0Asurveys_tools/kdqol.html
Pabón-Varela, Y., Paez-Hernandez, K. S., Rodriguez-Daza, K. D., Medina-Atencia, C. E., López-Tavera, M., & Salcedo-Quintero, L. V. (2015). Calidad de vida del adulto con insuficiencia renal crónica, una mirada bibliográfica. Duazary,12(2), 157. https://doi.org/10.21676/2389783x.1473.
Gonzalez Flores, C. J., Ureña Rodriguez, M. G., & Meda Lara, R. M. (2018). Resiliencia y enfermedad renal crónica: Una Revisión sistemática. Revista Iberoamericana de Psicología,11(2), 79–86. https://doi.org/10.33881/2027-1786.rip.11209.
Bonanno, G. A., Ho, S. M. Y., Chan, J. C. K., Kwong, R. S. Y., Cheung, C. K. Y., Wong, C. P. Y., et al. (2008). Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology,27(5), 659–667. https://doi.org/10.1037/0278-6133.27.5.659.
Stainton, A., Chisholm, K., Kaiser, N., Rosen, M., Upthegrove, R., Ruhrmann, S., et al. (2019). Resilience as a multimodal dynamic process. Early Intervention in Psychiatry,13(4), 725–732. https://doi.org/10.1111/eip.12726.
Bonanno, G. A., & Diminich, E. D. (2013). Annual research review: Positive adjustment to adversity—Trajectories of minimal-impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry and Allied Disciplines,54(4), 378–401. https://doi.org/10.1111/jcpp.12021.
Molina, Y., Yi, J. C., Martinez-Gutierrez, J., Reding, K. W., Yi-Frazier, J. P., & Rosenberg, A. R. (2014). Resilience among patients across the cancer continuum: Diverse perspectives. Clinical Journal of Oncology Nursing,18(1), 93–101. https://doi.org/10.1188/14.CJON.93-101.
Wu, W. W., Tsai, S. Y., Liang, S. Y., Liu, C. Y., Jou, S. T., & Berry, D. L. (2015). The Mediating role of resilience on quality of life and cancer symptom distress in adolescent patients with cancer. Journal of Pediatric Oncology Nursing,32(5), 304–313. https://doi.org/10.1177/1043454214563758.
Temprado, M. D., Agut, S., & Collado, E. (2019). The mediating role of resilience in the relationship between personality and adjustment to disease in patients with a drainage enterostomy. Journal of Health Psychology,24(8), 1110–1124. https://doi.org/10.1177/1359105316689142.
Temprado Albalat, M. D., García Martínez, P., Ballester Arnal, R., & Collado-Boira, E. J. (2018). The relationship between resilience and quality of life in patients with a drainage enterostomy. Journal of Health Psychology. https://doi.org/10.1177/1359105318761555.
Haase, J. E., Kintner, E. K., Monahan, P. O., & Robb, S. L. (2014). The resilience in illness model, Part 1: Exploratory evaluation in adolescents and young adults with cancer. Cancer Nursing. https://doi.org/10.1097/NCC.0b013e31828941bb.
Alonso, J. (n.d.). Kidney Disease Quality of Life Instrument (KDQOL), Spanish Version. Rand Corporation Website. Retrieved October 5, 2019, from https://www.rand.org/health-care/surveys_tools/kdqol.html
Peipert, J. D., Nair, D., Klicko, K., Schatell, D. R., & Hays, R. D. (2019). Kidney disease quality of life 36-item short form survey (KDQOL-36) normative values for the United States dialysis population and new single summary score. Journal of the American Society of Nephrology,30(4), 654–663. https://doi.org/10.1681/ASN.2018100994.
Chavez, K., Duarte, A., & Vega, J. (2013). Adaptación transcultural del cuestionario KDQOL SF 36 para evaluar calidad de vida en pacientes con enfermedad renal crónica en Colombia. Revista Médica,21(2), 12. https://doi.org/10.18359/rmed.1170.
Menezes, V. A., Fernández, B., Hernández, L., Ramos, F., & Contador, I. (2006). Resiliencia y el modelo Burnout-Engagement en cuidadores formales de ancianos. Psicothema,18(4), 791–796.
Ahern, N., Kiehl, E., Lou Sole, M., & Byers, J. (2006). A review of instruments measuring resilience. Comprehensive Child and Adolescent Nursing,29(2), 103–125. https://doi.org/10.1080/01460860600677643.
Bezdjian, S., Schneider, K. G., Burchett, D., Baker, M. T., & Garb, H. N. (2017). Resilience in the united states air force: Psychometric properties of the connor-davidson resilience scale (CD-RISC). Psychological Assessment,29(5), 479–485. https://doi.org/10.1037/pas0000370.
Madewell, A. N., & Ponce-Garcia, E. (2016). Assessing resilience in emerging adulthood: The Resilience Scale (RS), Connor-Davidson Resilience Scale (CD-RISC), and Scale of Protective Factors (SPF). Personality and Individual Differences,97, 249–255. https://doi.org/10.1016/j.paid.2016.03.036.
Remor, E. (2006). Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Spanish Journal of Psychology,9(1), 86–93. https://doi.org/10.1017/S1138741600006004.
Campo-Arias, A., Oviedo, H. C., & Herazo, E. (2014). The psychometric performance of the perceived stress scale-10 on medical students from bucaramanga, Colombia. Revista Facultad de Medicina,62(3), 407–413. https://doi.org/10.15446/revfacmed.v62n3.43735.
Hunsley, J., & Mash, E. J. (2008). A guide to assessments that work. New York: Oxford University Press.
Hair, J. F., Black, W. C., & Babin, B. J. (2010). Multivariate data analysis: A global perspective. Boston: Pearson.
Williams, M. N., Grajales, C. A. G., & Kurkiewicz, D. (2013). Assumptions of multiple regression: Correcting two misconceptions. Practical Assessment, Research and Evaluation,18(9), 1–14.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: L. Erlbaum Associates.
Morales García, A. I., Arenas Jiménez, M. D., Reig-Ferrer, A., Álvarez-Ude, F., Malek, T., Moledous, A., et al. (2011). Optimismo disposicional en pacientes en hemodiálisis y su influencia en el curso de la enfermedad. Nefrologia,31(2), 199–205. https://doi.org/10.3265/Nefrologia.pre2011.Feb.10534.
Alonso, R. P., Sánchez, J. L. C., López, M. R., de Buruaga, A. S. P., Rincón, A. T., Nates, R. A., et al. (2011). Repercusión del acceso vascular sobre la calidad de vida de los pacientes en tratamiento con hemodiálisis. Revista de la Sociedad Espanola de Enfermeria Nefrologica,14(4), 242–249. https://doi.org/10.4321/S1139-13752011000400006.
Moura, A., Madureira, J., Alija, P., Fernandes, J. C., Oliveira, J. G., Lopez, M., et al. (2015). Predictors of health-related quality of life perceived by end-stage renal disease patients under online hemodiafiltration. Quality of Life Research,24(6), 1327–1335. https://doi.org/10.1007/s11136-014-0854-x.
Cohen, D. E., Lee, A., Sibbel, S., Benner, D., Brunelli, S. M., & Tentori, F. (2019). Use of the KDQOL-36TM for assessment of health-related quality of life among dialysis patients in the United States. BMC Nephrology. https://doi.org/10.1186/s12882-019-1295-0.
Peipert, J. D., Bentler, P. M., Klicko, K., & Hays, R. D. (2018). Psychometric properties of the kidney disease quality of life 36-item short-form survey (KDQOL-36) in the United States. American Journal of Kidney Diseases,71(4), 461–468. https://doi.org/10.1053/j.ajkd.2017.07.020.
Chen, J. Y., Wan, E. Y. F., Choi, E. P. H., Chan, A. K. C., Chan, K. H. Y., Tsang, J. P. Y., et al. (2017). The health-related quality of life of chinese patients on hemodialysis and peritoneal dialysis. Patient,10(6), 799–808. https://doi.org/10.1007/s40271-017-0256-6.
Tao, X., Chow, S. K. Y., & Wong, F. K. Y. (2014). Determining the validity and reliability of the Chinese version of the Kidney Disease Quality of Life Questionnaire (KDQOL-36TM). BMC Nephrology. https://doi.org/10.1186/1471-2369-15-115.
Yang, F., Luo, N., Lau, T., Yu, Z. L., Foo, M. W. Y., & Griva, K. (2018). Health-related quality of life in patients treated with continuous ambulatory peritoneal dialysis and automated peritoneal dialysis in Singapore. PharmacoEconomics Open,2(2), 203–208. https://doi.org/10.1007/s41669-017-0046-z.
Mateti, U. V., Nagappa, A. N., Attur, R. P., Nagaraju, S. P., Mayya, S. S., & Balkrishnan, R. (2015). Cross-cultural adaptation, validation and reliability of the South Indian (Kannada) version of the Kidney Disease and Quality of Life (KDQOL-36) instrument. Saudi Journal of Kidney Diseases and Transplantation,26(6), 1246–1252. https://doi.org/10.4103/1319-2442.168662.
Noghan, N., Akaberi, A., Pournamdarian, S., Borujerdi, E., & Sadat Hejazi, S. (2018). Resilience and therapeutic regimen compliance in patients undergoing hemodialysis in hospitals of Hamedan, Iran. Electronic Physician,10(5), 6853–6858. https://doi.org/10.19082/6853.
Ricardo, A. C., Hacker, E., Lora, C. M., Ackerson, L., De Salvo, K. B., Go, A., et al. (2013). Validation of the Kidney Disease Quality of Life Short Form 36 (KDQOL-36TM) US Spanish and English versions in a cohort of Hispanics with chronic kidney disease. Ethnicity and Disease,23(2), 202–209.
Chao, S., Yen, M., Lin, T. C., Sung, J. M., Wang, M. C., & Hung, S. Y. (2016). Psychometric properties of the Kidney Disease Quality of Life–36 Questionnaire (KDQOL-36TM). Western Journal of Nursing Research,38(8), 1067–1082. https://doi.org/10.1177/0193945916640765.
Yang, F., Griva, K., Lau, T., Vathsala, A., Lee, E., Ng, H. J., et al. (2015). Health-related quality of life of Asian patients with end-stage renal disease (ESRD) in Singapore. Quality of Life Research,24(9), 2163–2171. https://doi.org/10.1007/s11136-015-0964-0.
Harris, B. A., Berger, A. M., Mitchell, S. A., Steinberg, S. M., Baker, K. L., Handel, D. L., et al. (2010). Spiritual well-being in long-term survivors with chronic graft-versus-host disease after hematopoietic stem cell transplantation. Journal of Supportive Oncology,8(3), 119–125. https://doi.org/10.1200/jco.2008.26.15_suppl.18017.
Costanzo, E. S., Ryff, C. D., & Singer, B. H. (2009). Psychosocial adjustment among cancer survivors: Findings from a national survey of health and well-being. Health Psychology,28(2), 147–156. https://doi.org/10.1037/a0013221.
Lee, P. W. H., Kwan, T. T. C., Kwong, D. L. W., Sham, J. S. T., Pow, E. H. N., McMillan, A. S., et al. (2007). A prospective study of the impact of nasopharyngeal cancer and radiotherapy on the psychosocial condition of Chinese patients. Cancer,109(7), 1344–1354. https://doi.org/10.1002/cncr.22539.
Ong, A. D., Bergeman, C. S., & Boker, S. M. (2009). Resilience comes of age: Defining features in later adulthood. Journal of Personality,77(6), 1777–1804. https://doi.org/10.1111/j.1467-6494.2009.00600.x.
Martínez-Castelao, A., Gòrriz, J. L., Garcia-López, F., López-Revuelta, K., De Alvaro, F., Cruzado, J. M., et al. (2004). Perceived health-related quality of life and comorbidity in diabetic patients starting dialysis (CALVIDIA study). Journal of Nephrology,17(4), 544–551.
Chmitorz, A., Kunzler, A., Helmreich, I., Tüscher, O., Kalisch, R., Kubiak, T., et al. (2018). Intervention studies to foster resilience—A systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review,59, 78–100. https://doi.org/10.1016/j.cpr.2017.11.002.
Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan, C. A., Charney, D., & Southwick, S. (2007). Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry,4(5), 35–40.
De Pasquale, C., Conti, D., Pistorio, M. L., Fatuzzo, P., Veroux, M., & Di Nuovo, S. (2017). Comparison of the CBA-H and SF-36 for the screening of the psychological and behavioural variables in chronic dialysis patients. PLoS ONE,12(6), e0180077. https://doi.org/10.1371/journal.pone.0180077.
Bradshaw, B. G., Richardson, G. E., Kumpfer, K., Carlson, J., Stanchfield, J., Overall, J., et al. (2007). Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educator,33(4), 650–659. https://doi.org/10.1177/0145721707303809.
Jeste, D. V., Savla, G. N., Thompson, W. K., Vahia, I. V., Glorioso, D. K., Martin, A. S., et al. (2013). Association between older age and more successful aging: Critical role of resilience and depression. American Journal of Psychiatry,170(2), 188–196. https://doi.org/10.1176/appi.ajp.2012.12030386.
Rutter, M. (2013). Annual research review: Resilience—Clinical implications. Journal of Child Psychology and Psychiatry and Allied Disciplines,54(4), 474–487. https://doi.org/10.1111/j.1469-7610.2012.02615.x.
Stubbs, B., Vancampfort, D., Veronese, N., Schofield, P., Lin, P. Y., Tseng, P. T., et al. (2018). Multimorbidity and perceived stress: a population-based cross-sectional study among older adults across six low- and middle-income countries. Maturitas,107, 84–91. https://doi.org/10.1016/j.maturitas.2017.10.007.
Ahola, A. J., Saraheimo, M., Forsblom, C., Hietala, K., Sintonen, H., & Groop, P. H. (2010). Health-related quality of life in patients with type 1diabetes—Association with diabetic complications (the FinnDiane Study). Nephrology Dialysis Transplantation,25(6), 1903–1908. https://doi.org/10.1093/ndt/gfp709.
Funding
Authors did not received funding for conducting this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Martínez, P., Temprado-Albalat, M.D., Ballester-Arnal, R. et al. Predictive model of variables associated with health-related quality of life in patients with advanced chronic kidney disease receiving hemodialysis. Qual Life Res 29, 1817–1827 (2020). https://doi.org/10.1007/s11136-020-02454-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02454-0