Abstract
Purpose
The majority of studies on quality of life (QoL) of women with menstrual disturbances have not taken menstrual cycle phase into account. We aimed to determine the size of changes in QoL score during perimenstrual week compared to those during late follicular phase in women suffering from dysmenorrhea with or without premenstrual syndrome (PMS) and also to compare the two groups.
Methods
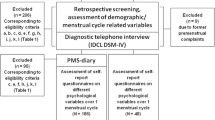
In this observational analytical study, participants were selected purposively from among single students aged 18–30 years, who were residing at university dormitories in Tabriz, Iran, and had moderate or severe dysmenorrhea. They reported quality of their life during the past week using the Quality of Life Enjoyment and Satisfaction Questionnaire-Short Form (Q-LES-Q-SF) at two time points, days 3–4 and 11–12, of their menstrual cycle.
Results
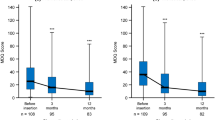
Among 52 participants with PMS and 64 without PMS, about half reported severe dysmenorrhea. The mean total quality score was significantly lower during perimenstrual week than during late follicular phase in both group with PMS [48 vs 79, mean difference − 31 (95% confidence interval − 37 to − 26)] and group without PMS [56 vs 78, − 1 (− 27 to − 18)]. The score was significantly lower in the group with PMS than in those without PMS during perimenstrual week [− 8 (− 13 to − 2)] but not during late follicular phase [2.1 (− 2.9 to 7.0)].
Conclusions
Dysmenorrhea with or without PMS significantly reduces QoL of women during perimenstrual week. The QoL is slightly lower in group with PMS during perimenstrual week but not during late follicular phase.

Similar content being viewed by others
References
Deshpande, P. R., Rajan, S., Sudeepthi, B. L., & Abdul Nazir, C. P. (2011). Patient-reported outcomes: A new era in clinical research. Perspectives in Clinical Research, 2, 137–144. https://doi.org/10.4103/2229-3485.86879.
Meadows, K. A. (2011). Patient-reported outcome measures: An overview. British Journal of Community Nursing, 16, 146–151. https://doi.org/10.12968/bjcn.2011.16.3.146.
The WHOQOL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28, 551–558.
Iacovides, S., Avidon, I., & Baker, F. C. (2015). What we know about primary dysmenorrhea today: A critical review. Human Reproduction Update, 21, 762–778. https://doi.org/10.1093/humupd/dmv039.
Latthe, P. M., Champaneria, R., & Khan, K. S. (2011). Dysmenorrhoea. BMJ Clinical Evidence, 2, 813.
Dawood, M. Y. (2006). Primary dysmenorrhea: advances in pathogenesis and management. Obstetrics & Gynecology, 108, 428–441. https://doi.org/10.1097/01.AOG.0000230214.26638.0c.
Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiologic Reviews, 36, 104–113. https://doi.org/10.1093/epirev/mxt009.
Tavallaee, M., Joffres, M. R., Corber, S. J., Bayanzadeh, M., & Rad, M. M. (2011). The prevalence of menstrual pain and associated risk factors among Iranian women. Journal of Obstetrics and Gynaecology Research, 37, 442–451. https://doi.org/10.1111/j.1447-0756.2010.01362.x.
Smith, R. P., & Kaunitz, A. M. (2018) Primary dysmenorrhea in adult women: Clinical features and diagnosis. In: Eckler K (Ed.). Retrieved July 4, 2018, from https://www.uptodate.com/contents/primary-dysmenorrhea-in-adult-women-clinical-features-and-diagnosis?search=primary%20dysmenorrhea&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
O’Brien, P. M., Backstrom, T., Brown, C., Dennerstein, L., Endicott, J., et al. (2011). Towards a consensus on diagnostic criteria, measurement and trial design of the premenstrual disorders: The ISPMD Montreal consensus. Archives of Women’s Mental Health, 14, 13–21. https://doi.org/10.1007/s00737-010-0201-3.
Yonkers, K. A., O’Brien, P. M., & Eriksson, E. (2008). Premenstrual syndrome. Lancet, 371, 1200–1210. https://doi.org/10.1016/s0140-6736(08)60527-9.
Sahin, S., Ozdemir, K., & Unsal, A. (2014). Evaluation of premenstrual syndrome and quality of life in university students. Journal of Pakistan Medical Association, 64, 915–922.
Potter, J., Bouyer, J., Trussell, J., & Moreau, C. (2009). Premenstrual syndrome prevalence and fluctuation over time: Results from a French population-based survey. Journal of Women’s Health (Larchmt), 18, 31–39. https://doi.org/10.1089/jwh.2008.0932.
Iacovides, S., Avidon, I., Bentley, A., & Baker, F. C. (2014). Reduced quality of life when experiencing menstrual pain in women with primary dysmenorrhea. Acta Obstetricia et Gynecologica Scandinavica, 93, 213–217. https://doi.org/10.1111/aogs.12287.
Al-Jefout, M., Seham, A. F., Jameel, H., Randa, A. Q., Ola, A. M., et al. (2015). Dysmenorrhea: Prevalence and impact on quality of life among young adult Jordanian females. Journal of Pediatric and Adolescent Gynecology, 28, 173–185. https://doi.org/10.1016/j.jpag.2014.07.005.
Isik, H., Ergol, S., Aynioglu, O., Sahbaz, A., Kuzu, A., et al. (2016). Premenstrual syndrome and life quality in Turkish health science students. Turkish Journal of Medical Sciences, 46, 695–701. https://doi.org/10.3906/sag-1504-140.
Farrokh-Eslamlou, H., Oshnouei, S., Heshmatian, B., & Akbari, E. (2015). Premenstrual syndrome and quality of life in Iranian medical students. Sexual & Reproductive Healthcare, 6, 23–27. https://doi.org/10.1016/j.srhc.2014.06.009.
Heinemann, L. A., Minh, T. D., Heinemann, K., Lindemann, M., & Filonenko, A. (2012). Intercountry assessment of the impact of severe premenstrual disorders on work and daily activities. Health Care for Women International, 33, 109–124. https://doi.org/10.1080/07399332.2011.610530.
Raval, C. M., Panchal, B. N., Tiwari, D. S., Vala, A. U., & Bhatt, R. B. (2016). Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian Journal of Psychiatry, 58, 164–170. https://doi.org/10.4103/0019-5545.183796.
Ware, J. E. Jr., & Gandek, B. (1998). Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. Journal of Clinical Epidemiology, 51, 903–912.
Endicott, J., Nee, J., Harrison, W., & Blumenthal, R. (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: A new measure. Psychopharmacology Bulletin, 29, 321–326.
Baker, F. C., Sassoon, S. A., Kahan, T., Palaniappan, L., Nicholas, C. L., et al. (2012). Perceived poor sleep quality in the absence of polysomnographic sleep disturbance in women with severe premenstrual syndrome. Journal of Sleep Research, 21, 535–545. https://doi.org/10.1111/j.1365-2869.2012.01007.x.
Hawker, G. A., Mian, S., Kendzerska, T., & French, M. (2011). Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care and Research (Hoboken), 63(Suppl 11), S240–S252. https://doi.org/10.1002/acr.20543.
The American College of Obestetricians and Gynecologists (2015) Premenstural syndrom (PMS). Retrieved January 14, 2016, from https://www.acog.org/-/media/For-Patients/faq057.pdf?dmc=1&ts=20180212T0642252466.
Stevanovic, D. (2011). Quality of Life Enjoyment and Satisfaction Questionnaire-short form for quality of life assessments in clinical practice: A psychometric study. Journal of Psychiatric and Mental Health Nursing, 18, 744–750. https://doi.org/10.1111/j.1365-2850.2011.01735.x.
Lee, Y. T., Liu, S. I., Huang, H. C., Sun, F. J., Huang, C. R., et al. (2014). Validity and reliability of the Chinese version of the Short Form of Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-SF). Quality of Life Research, 23, 907–916. https://doi.org/10.1007/s11136-013-0528-0.
Tagharrobi, Z., Sharifi, K., Sooky, Z., & Tagharrobi, L. (2012). Psychometric evaluation of the Iranian version of Quality of Life Enjoyment and Satisfaction Questionnaire Short Form (Q-LES-QSF). Payesh, 11, 235–244.
Delara, M., Ghofranipour, F., Azadfallah, P., Tavafian, S. S., Kazemnejad, A., et al. (2012). Health related quality of life among adolescents with premenstrual disorders: A cross sectional study. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-10-1.
Issa, B. A., Yussuf, A. D., Olatinwo, A. W., & Ighodalo, M. (2010). Premenstrual dysphoric disorder among medical students of a Nigerian university. Annals of African medicine, 9, 118–122. https://doi.org/10.4103/1596-3519.68354.
Acknowledgements
This paper has been extracted from thesis of MSc student in Midwifery. Appreciation goes to research deputy of the Tabriz University of Medical Sciences for their financial support. This project was approved by ethics committee of the university (Ethical Code: TBZMED.rec.1394.881, Date 2016-01-04). We send our deep appreciation to all students who patiently participated in this study.
Author information
Authors and Affiliations
Contributions
All of the authors contributed to the conception and design of the study. FQ recruited the participants, collected the data, and wrote the first draft of the paper. FQ and SMAC analyzed the data. SMAC and MM revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Rights and permissions
About this article
Cite this article
Quick, F., Mohammad-Alizadeh-Charandabi, S. & Mirghafourvand, M. Primary dysmenorrhea with and without premenstrual syndrome: variation in quality of life over menstrual phases. Qual Life Res 28, 99–107 (2019). https://doi.org/10.1007/s11136-018-1999-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1999-9