Abstract
The majority of secondary and tertiary healthcare services in New Zealand are provided through public hospitals managed by 20 local District Health Boards. Due to data issues and ill-judged generic public perceptions, efficiency studies are insufficient in spite of the extensive empirical literatures available. This inevitably leads to criticisms about the perverse incentives which might be created by the National Health Targets designed to improve the performance of public health services. Utilizing a multifaceted administrative hospital dataset, this is the first case study to measure both the technical and cost efficiency of New Zealand public hospitals during the period of 2011–2017. More specifically, it deals with the question of how hospital efficiency varies with respect to activities accounted for by the National Health Targets. The empirical results show no evidence that these targets are achieved at the expenses of lowering the overall efficiency of hospital operations. The national technical efficiency is averaged at 86 percent over the period and cost efficiency is 85 percent. The results are derived by stochastic input distance function and cost frontier in order to accommodate multiple outputs and limited number of census observations. Efficiency ranking is sensitive to specifications of the inefficiency error term, but reasonably robust to the choice of functional form and different proxies for capital input.
Similar content being viewed by others
Notes
A non-negligible number of observations incurred negative expenditures on key inputs such as outsourced medical staff, outsourced nurses and allied professionals etc. This will cause problems when the quantity of input is to be derived from related expenditures. The MOH indicates these negative records are the results of balancing the accounts. For example, a hospital might contract medical doctors to do managerial administrations but the corresponding expenses are recorded as outsourced medical instead of outsourced management. This will generate an imbalance in the monthly financial statement and be corrected in the following months by debiting the corresponding expenses from outsourced medical and crediting the account for outsourced management.
The PBFF allocates resources between DHBs based on a core model which assesses the relative healthcare needs of the local populations via historical average expenditures for different demographic groups. The PBFF also incorporates adjusters to account for factors such as populations with low access to healthcare services, rural areas, overseas visitors and refugees.
These population demographics are projections provided by Statistics NZ and do not represent the actual patient profile seen by each DHB.
If η > 0, then uit increases over time, suggesting deteriorated efficiency performance. If η < 0, then uit decreases over time, suggesting improved efficiency performance. A limitation of this specification is that it does not allow for a change in the rank ordering of DHBs over time - a DHB that is ranked n-th at the first time period is always ranked n-th (Coelli et al. 2005, p. 278).
Both the salary payments and employee FTE counts are items available in the monthly financial statements.
This means the outsourcing expenses do not reflect the actual inputs consumed in that month.
This assumes that the average hired medical doctor and outsourced medical doctor receive similar remuneration.
One can refer to Fraser and Nolan (2017) for discussions on the case-mix methodology.
These more conventional specifications include the half/truncated normal distribution for uit, or a frontier with a reduced number of inputs.
References
Aigner D, Lovell CAK, Schmidt P (1977) Formulation and estimation of stochastic frontier production function models. J Econom 6(1):21–37
Aletras V, Kontodimopoulos N, Zagouldoudis A, Niakas D (2007) The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 83(2–3):236–245
Ancarani A, Di Mauro C, Giammanco MD (2009) The impact of managerial and organizational aspects on hospital wards’ efficiency: evidence from a case study. Eur J Oper Res 194(1):280–293
Ashton T (2005) Recent developments in the funding and organisation of the New Zealand health system. Aust New Zealand Health Policy 2:9
Ashton, T (2009) In Cost Containment and Efficiency in National Health Systems, New Zealand (pp 183–206). https://doi.org/10.1002/9783527622962.ch8
Battese GE, Coelli TJ (1992) Frontier production functions, technical efficiency and panel data: with application to paddy farmers in India. J Prod Anal 3(1–2):153–169
Battese GE, Coelli TJ (1995) A model for technical inefficiency effects in a stochastic frontier production function for panel data. Empir Econ 20(2):325–332
Blank JL, Valdmanis VG (2010) Environmental factors and productivity on Dutch hospitals: a semi-parametric approach. Health Care Manage Sci 13(1):27–34
Bogetoft P, Otto L (2011) Benchmarking with DEA, SFA, and R. Springer-Verlag, New York, NY
Brown HS (2003) Managed care and technical efficiency. Health Econ 12(2):149–158
Chang H, Cheng M-A, Das S (2004) Hospital ownership and operating efficiency: Evidence from Taiwan. Eur J Oper Res 159(2):513–527
Charnes A, Cooper WW, Lewin AY, Seiford LM (1995) Data envelopment analysis: theory, methodology, and applications. Springer, Netherlands. https://doi.org/10.1007/978-94-011-0637-5
Chowdhury H, Zelenyuk V (2016) Performance of hospital services in Ontario: DEA with truncated regression approach. Omega 63:111–122
Coelli TJ (1996) A Guide to DEAP Version 2.1: A Data Envelopment Analysis Program, Centre for Efficiency and Productivity Analysis Working Paper 96/08
Coelli TJ, Rao DSP, O’Donnell CJ, Battese GE (2005) An Introduction to Efficiency and Productivity Analysis. Springer US. https://doi.org/10.1007/b136381
Cooper WW, Seiford LM, Tone K (2007) Data Envelopment Analysis: A Comprehensive Text with Models, Applications, References and DEA-Solver Software. Springer US. https://doi.org/10.1007/978-0-387-45283-8
Cristian NI, Matthew Fannin J (2013) Analyzing cost efficiency of critical access hospitals. Journal of Policy Modeling 35(1):183–195
Cumming, J, McDonald, J, Barr, C, Martin, G, Gerring, Z, Daubé, J (2014) New Zealand health system review. Health Systems in Transition, 4(2):152–179. WHO Regional Office for the Western Pacific
Dyson RG, Shake EA (2010) Data envelopment analysis, operational research and uncertainty. J Oper Res Soc 61(1):25–34
Färe R (1988) Fundamentals of production theory. Springer-Verlag, Berlin Heidelberg
Färe R, Grosskopf S, Lovell CAK (1993) Production frontiers. Cambridge University Press, Cambridge, United Kingdom
Farrell MJ (1957) The Measurement of Productive Efficiency. J R Stat Soc Series A (General) 120(3):253–290
Fethi MD, Jackson P, Weyman-Johns T (2001) European Airlines: a Stochastic DEA study of efficiency with market liberalisation. Tech. rep., University of Leicester Efficiency and Productivity Research Unit, Leicester, England
Friesner D, Mittelhammer R, Rosenman R (2013) Inferring the incidence of industry inefficiency from DEA estimates. Eur J Oper Res 224(2):414–424
Gannon B (2005) Testing for variation in technical efficiency of hospitals in Ireland. Econ Soc Rev (Irel) 36(3):273–294
Griffin RC, Montgomery JM, Rister ME (1987) Selecting functional form in production function analysis. Wes J Agric Econ 12(2):216–227
Heathfield D, Wibe S (1987) An introduction to cost and production functions. Macmillan Education Ltd, Humanities Press International, Basingstoke, United Kingdom
Herr A (2008) Cost and technical efficiency of German hospitals: does ownership matter? Health Econ 17:1057–1071
Herr A, Schmitz H, Augurzky B (2011) Profit efficiency and ownership of German hospitals. Health Econ 20:660–674
Huang CJ, Liu JT (1994) Estimation of a non-neutral stochastic frontier production function. Journal of Productivity Analysis 5(2):171–180
Kao C, Liu S-T (2009) Stochastic data envelopment analysis in measuring the efficiency of Taiwan commercial banks. Eur J Oper Res 196(1):312–322
Kodde DA, Palm FC (1986) Wald criteria for jointly testing equality and inequality restrictions. Econometrica 54(5):1243–1248
Kontodimopoulos N, Nanos P, Niakas D (2006) Balancing efficiency of health services and equity of access in remote areas in Greece. Health Policy 76(1):49–57
Kumbhakar S, Lovell C (2000) Stochastic frontier analysis. Cambridge University Press. https://doi.org/10.1017/CBO9781139174411
Land KC, Lovell CA, Thore S (1993) Chance‐constrained data envelopment analysis. Managerial and Decision Economics 14:541–554
Marcinko DE, Hetico HR (2012) Capital formation techniques for hospitals. In: Marcinko, DE (ed) Hospitals & Health Care Organizations: Management strategies, operational techniques, tools, templates, and case studies, CRC Press, Florida, FL, p 96
Mays N, Marney J, King E (2013) Fiscal Challenges and Changing Patterns of Need for Health and Long-Term Care in New Zealand. Policy Quarterly, 9(4):35–46. http://igps.victoria.ac.nz/publications/files/f16f9432dc3.pdf
New Zealand Productivity Commission (2017) Measuring and improving state sector productivity: draft report. www.productivity.govt.nz/current-inquiries
Olesen OB, Petersen NC (2002) The use of data envelopment analysis with probabilistic assurance regions for measuring hospital efficiency. J Prod Anal 17(1–2):83–109
Parkin D, Hollingsworth B (1997) Measuring production efficiency of acute hospitals in Scotland, 1991–94: validity issues in data envelopment analysis. Appl Econ 29(11):1425–1433
Rasmussen S (2011) Production economics. Springer-Verlag, Berlin Heidelberg
Ronald S (1970) Theory of cost and production functions. Princeton University Press, Princeton, United States
Salmond C, Crampton P, Atkinson J (2007) NZDep2006 Index of Deprivation Research Report. Department of Public Health, University of Otago, Wellington
Sandiford P, Consuelo DJ, Rouse P (2017) How efficient are New Zealand’s District Health Boards at producing life expectancy gains for Māori and Europeans? Aust N Z J Public Health 41:125–129
Simar L, Wilson PW (1998) Sensitivity analysis of efficiency scores: how to bootstrap in nonparametric frontier models. Manage Sci 44(1):49–61
Simar L, Wilson PW(2000) A general methodology for bootstrapping in non-parametric frontier models. J Appl Stat 27(6):779–802
Simar L, Wilson PW (2007) Estimation and inference in two-stage, semi-parametric models of production processes. J Econom 136(1):31–64
Worthington AC (2004) Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Med Care Res Rev 61(2):135–170
Zelman WN, McCue MJ, Millikan AR, Glick ND (2009) Financial management of health care organizations: an introduction to fundamental tools, concepts, and applications. Blackwell Publishing, United Kingdom
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
See Table 5
Appendix B
See Table 6
Appendix C
See Table 7
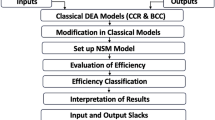
Appendix D: The DEA Model
With price information and under the behavioural objective of cost minimization, both technical and cost efficiencies can be measured using the standard DEA model as outlined in Färe et al. (1993) and the software DEAP 2.1 developed by Coelli 1996).
First the input-oriented DEA model is run to obtain technical efficiencies (i.e. TE_DEA in Table 4), assuming there is data on K inputs and M outputs on each of N firms or decision making units (DMUs). For the i-th DMU these are represented by the vectors xi and yi, respectively. The K × N input matrix, X, and the M × N output matrix, Y, represent the data of all N DMU’s. The purpose of DEA is to construct a non-parametric envelopment frontier over the data points such that all observed points lie on or below the production frontier. This is accomplished by solving the corresponding variable returns to scale (VRS) linear programming problem:
where θ is a scalar and λ is a N × 1 vector of constants for all NDMUs. N1 is an N × 1 vector of ones. The value of θ obtained will be the efficiency score for the i-th DMU. It will satisfy θ ≤ 1, with a value of 1 indicating a point on the frontier and hence a technically efficient DMU. Note that the linear programming problem must be solved N times, once for each DMU in the sample. A value of θ is then obtained for each DMU.
Next the following cost minimization DEA model is run to obtain cost efficiencies (i.e. CE_DEA in Table 4):
where wi is a vector of input prices for the i-th DMU and \({\boldsymbol{x}}_{\boldsymbol{i}}^ \ast\) (which is calculated by the Linear Programming) is the cost minimizing vector of input quantities for the i-th DMU, given the input prices wi and the output levels yi. The total cost efficiency (CE) of the i-th DMU would be calculated as:
Rights and permissions
About this article
Cite this article
Jiang, N., Andrews, A. Efficiency of New Zealand’s District Health Boards at Providing Hospital Services: A stochastic frontier analysis. J Prod Anal 53, 53–68 (2020). https://doi.org/10.1007/s11123-019-00550-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11123-019-00550-z