Abstract
Purpose
To compare the clinical, hormonal, and radiological presentation and surgical outcomes of patients with macroadenomas presenting with pituitary apoplexy and patients not presenting pituitary apoplexy.
Methods
Multicentre retrospective study of patients presenting with macroadenomas and pituitary apoplexy in three Spanish tertiary hospitals between 2008 and 2022. We selected as control group (non-pituitary apoplexy), patients with pituitary macroadenomas without apoplexy who underwent pituitary surgery between 2008 and 2020.
Results
A total of 60 patients with apoplexy and 185 without apoplexy were enrolled. Patients with pituitary apoplexy were more frequently men (70% vs. 48.1%, p = 0.003), had higher prevalence of hypertension (43.3% vs. 26.0%, p = 0.011) and of obesity (23.3% vs. 9.7%, P = 0.007), were under treatment with anticoagulants more commonly (11.7% vs. 4.3%, P = 0.039) and had larger (27.5 ± 11.03 vs. 23.6 ± 12.55 mm, p = 0.035) and invasive pituitary macroadenomas more frequently (85.7% vs. 44.3%, P < 0.001) than those without apoplexy. Surgical remission was more frequent in patients with pituitary apoplexy than those without apoplexy (OR 4.55, P < 0.001), but they developed new pituitary deficits (OR 13.29, P < 0.001) and permanent diabetes insipidus (OR 3.40, P = 0.022) more commonly. However, visual improvement (OR 6.52, p < 0.001) and complete pituitary function recovery (OR 2.37, P < 0.001) was more common in patients without apoplexy.
Conclusion
Surgical resection is more common in patients presenting with pituitary apoplexy than those without apoplexy; however, visual improvement and complete recovery of pituitary function is more common in patients without apoplexy. The risk of new pituitary deficits and permanent diabetes insipidus is higher in patients with apoplexy than in those without it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pituitary apoplexy is considered a rare, sometimes life-threatening clinical syndrome that occurs due to an acute or subacute haemorrhage and/or infarction of a pituitary tumour [1]. It complicates 2–12% of pituitary adenomas, especially in non-functioning tumours. Nevertheless, in 75% of the cases, the diagnosis of pituitary tumor was unknown at time of the pituitary apoplexy debut [2]. Regarding the underlaying mechanism leading to pituitary apoplexy, it has been proposed that the growing tumor outstrips its blood supply results in ischemic necrosis. In this regard, several factors, including antiplatelet agents, anticoagulants, dopamine agonists, gonadotrophin agonists, previous surgery, brain trauma, endocrine dynamic tests and systemic diseases have been described as potentially precipitant factors of pituitary apoplexy [1].
The course of pituitary apoplexy is highly variable. Nevertheless, for patients presenting with neurological changes from pituitary tumor apoplexy, urgent surgical intervention is commonly performed for tumor resection, and optic apparatus decompression [2]. The treatment aims are to improve symptoms and relieve compression of local structures. For this purposes, surgical decompression is the most rapid way for achieving them [2] [3]. It has been reported that the surgical outcomes of patients with pituitary apoplexy may be quite poor when compared to the surgical outcomes of patients operated for a pituitary tumor without pituitary apoplexy. Accordingly, a complete recovery of oculomotor palsies has been described in 31–57% of patients presenting pituitary apoplexy after surgery [2, 4, 5], normalization of visual acuity in about 50% of the cases [4, 5], anterior pituitary function normalization in more than 50% of cases and complete tumor resection in most of the patients [6, 7].
Considering this background, the aim of our study was to compare the clinical, hormonal, and radiological presentation of patients with macroadenomas presenting with pituitary apoplexy and patients with macroadenomas without pituitary apoplexy. Moreover, we have analysed if there are differences in surgical outcomes in terms of pituitary function and ophthalmological recovery and surgical cure using a transsphenoidal endoscopic endonasal approach between both groups.
Methods
Patients
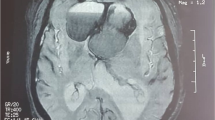
Data were collected from a retrospective database of patients with pituitary macroadenomas who presented clinical pituitary apoplexy at three Spanish centres (Hospital Universitario Ramón y Cajal (HURC), Hospital Universitario La Paz and Hospital Universitario Doce de Octubre) between 2008 and 2022. Inclusion criteria to enter in the study were: (i) diagnosis of clinical pituitary apoplexy based on the demonstration of radiological data of pituitary apoplexy (hemorrhage, and/or necrosis) in MRI in a patient consulting for acute symptoms consistent with pituitary apoplexy (headache, visual disturbances, and/or decreased conscientiousness), (ii) available information about pre- and postoperative clinical, hormonal, ophthalmological and radiological data and (iii) an age older than 18 years at the pituitary apoplexy diagnosis. Patients conservatively managed (n = 10) and those with microadenomas (n = 1) were excluded from the analysis. A total of 60 patients with macroadenomas presenting with pituitary apoplexy who underwent transsphenoidal endoscopic endonasal pituitary surgical resection were included in the study (Fig. 1)
As a control group we included patients coming from the Ramón y Cajal pituitary tumors database, that includes data about of all patients with pituitary tumours who underwent pituitary surgery at our hospital between 2008 and 2021. As we have previously described [8], inclusion criteria in the present study were patients with available information about pre- and postoperative clinical, hormonal, ophthalmological and radiological data, operated by the same neurosurgeon, and pathology reports confirming the diagnosis of pituitary adenoma. For the present study, we have only included those patients who underwent primary pituitary surgery and operated by a transsphenoidal endoscopic endonasal approach. In addition, patients with microadenomas were excluded (n = 34). Thus, a total of 60 patients with macroadenomas presenting with pituitary apoplexy and 185 patients with macroadenomas without apoplexy were included (Fig. 1).
The local Ethical Committee of the HURC reviewed and approved the study (approval date: 4 October 2019, code: ACTA 372 and approval date: February 2022).
Clinical, hormonal, and radiological evaluation and definitions
Collected clinical characteristics include gender, age, history of diabetes, hypertension, cardiovascular disease, hypopituitarism, previous general surgery, pregnancy, and dynamic endocrinological tests. Clinical symptoms and signs at the presentation of pituitary apoplexy and/or at the diagnosis of the pituitary tumor were registered. Pituitary Apoplexy Score (PAS), which represents a clinical staging system including the level of consciousness, visual acuity, and field defects and ocular palsies, was retrospectively calculated [9].
Complete assessment of pituitary hormone function was performed at the time of the pituitary apoplexy presentation or at the diagnosis of the pituitary tumor (non-apoplexy group), including the following laboratory determinations: adrenocorticotropic hormone (ACTH), morning cortisol, thyroid-stimulating hormone (TSH), free thyroxine (FT4), growth hormone (GH), insulin-like growth factor 1 (IGF-1), prolactin, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estradiol or total and free testosterone, depending on patient sex. Hypopituitarism was established according to the current criteria of diagnosis [10]. Visual involvement was defined as the presence of any degree of visual acuity compromise, from mild to severe visual acuity involvement and from partial to complete field conditions. Also, diplopia was registered as visual involvement.
Radiological evaluation was performed using a magnetic resonance imaging (MRI). Tumour characteristics registered were size, parasellar tumour involvement by Knosp grading [11], radiological apoplexy characteristics including haemorrhage, necrosis, and signal intensities on T1 and T2-weighted images. Pituitary tumors with maximum diameter < 10 and ≥ 10 mm were defined as microadenomas and macroadenomas, respectively.
Surgical outcomes
Pituitary surgery was performed by experienced endoscopic pituitary neurosurgeons. An endonasal endoscopic approach was used in all surgeries included in this series [12]. Surgical complications were defined as the development of permanent neurological deficit (oculomotor or visual impairment), postsurgical meningitis, cerebrospinal leakage, postsurgical bleeding requiring reoperation or intraoperative bleeding due to vascular injury. As we have previously defined, diabetes insipidus was considered permanent when there was no recovery after 6 months, and transient if the duration of the diabetes insipidus was shorter than 6 months [13].
Surgical cure was defined as a complete tumoral resection in non-functioning pituitary adenoma (defined by the 3 months postoperative MRI), and as biochemical cure in functioning pituitary adenomas (normal IGF1 for age and sex and normal GH levels in acromegaly; normal urinary free cortisol in Cushing´s disease and normal prolactin levels in prolactinomas).
Statistical analysis
All statistical analyses were conducted with STATA.15. Shapiro Wilk´s test was used to assess normality of continuous variables. Categorical variables were expressed as percentages and absolute values; continuous variables were expressed as mean ± standard deviation or median and interquartile range (IQR)/range depending on the normal distribution of the variable. We used the chi2 test for the comparison of categorial variables and the t-test for the comparison of two means. Univariant logistic regression analysis was employed for the calculation of odds ratios (OR) and confident intervals. In all cases, a two-tailed P value < 0.05 was considered statistically significant.
Results
Differences in baseline characteristics between both groups
A total of 60 patients with macroadenomas presenting with pituitary apoplexy and 185 with macroadenomas without apoplexy were enrolled in the study. Most of the cases were nonfunctioning pituitary macroadenomas (73.5%, n = 180), except for 43 patients with acromegaly (2 with apoplexy), 18 patients with prolactinoma (8 with apoplexy) and 4 with Cushing syndrome (0 with apoplexy). The PAS in the patients with pituitary apoplexy was greater than 4 in the 38.3% (n = 23) (Fig. 2). In the pituitary apoplexy group, other symptoms that were present at diagnosis were nausea/vomiting in 46.7% (n = 28), fever in 18.3% (n = 11) and diplopia in 46.6% (n = 27). Moreover, 30% of the cases had hyponatremia (n = 18), being the median serum sodium level in the entire group of apoplexy of 136.0 ± 7.49 mEq/mL. Moreover, involvement of oculomotor nerves was observed in 46.6% of the patients with pituitary apoplexy. No cases of hemodynamic instability upon the diagnosis of apoplexy were identified.
Patients with pituitary apoplexy were more frequently men, had a higher prevalence of hypertension and of obesity. Furthermore, they were under treatment with anticoagulants more commonly and had larger and invasive pituitary macroadenomas more frequently than those without pituitary apoplexy (Table 1). In addition to anticoagulant treatment, the following risk factors of pituitary apoplexy were identified in the group of patients with pituitary apoplexy: recent previous surgery (n = 7), recent starting of medical treatment for the pituitary tumor (n = 4), covid19 infection (n = 3), craneoenfecalic traumatism (n = 1), pregnancy (n = 1), cocaine abuse (n = 1), bacterial sinusitis (n = 1), meningitis (n = 1) and covid vaccine (n = 1). No differences were detected in the prevalence of risk factors of pituitary apoplexy between men and women (33.3% vs. 33.3%, P = 1.000), but men had larger tumors than women (27.5 ± 11.0 vs. 23.6 ± 12.5 mm; P = 0.035).
Pituitary apoplexy continued being more frequent in men than women after adjusting by tumor size and Knosp > 2 (adjusted OR: 2.36, 95% CI 1.18 to 4.74). In addition, the prevalence of headache, of visual involvement, and of hypopituitarism (including panhypopituitarism) was greater in the former (Table 1). The distribution of pituitary deficiencies by groups is described in Fig. 3.
Differences in surgical outcomes between both groups
Endoscopic endonasal pituitary surgery resection was performed in all cases. The median time from diagnosis to surgery in patients presenting with pituitary apoplexy was of 6 days (range 0 to 134) days. Most of the cases (68.4%) underwent early surgery (< 14 days from the pituitary apoplexy diagnosis), but the 31.6% of the cases were operated after 14 days from the diagnosis. In addition, 9 patients (of the group of early surgery) were operated on the first day of the pituitary apoplexy diagnosis (emergency surgery).
Overall, surgical cure was achieved in 65.4% of the patients (biochemical control of functioning pituitary adenomas of 57.4% and complete tumor resection of nonfunctioning pituitary adenomas of 67.8%). Most of the patients with presurgical visual affectation experienced improvement or total recovery after surgery (78.0%). We found that patients presenting with pituitary apoplexy had a probability four times higher of achieving surgical remission than those without apoplexy. However, they had visual improvement and recovery of complete pituitary function less frequently than those without apoplexy. In addition, the former developed new pituitary deficits, and permanent diabetes insipidus more commonly than those without apoplexy (Table 2). These differences continued being statistically significant after adjusting by tumor size and by Knosp grade ≥ 2 (see footer of Table 2). When we analyzed the rate of surgical complications and of surgical cure after excluding the first three years of the neurosurgeons learning curve, the rate of complications was significantly lower in the second period (28.6% vs. 4.7%, P < 0.001), including the rate of cerebrospinal leakage (22.7% vs. 2.0%, P < 0.001).
When we compared the group of patients with pituitary apoplexy who underwent to an early surgery and those underwent delayed surgery, no differences were detected in the rate of surgical cure (83.3% vs. 86.8%, P = 0.726), visual improvement (50% vs. 66.7%, P = 0.290) or recovery of pituitary function after surgery (21.4% vs. 20.7%, P = 0.955).
Discussion
In this article we describe the differences in the clinical, hormonal and radiological presentation of patients with macroadenomas presenting with and without pituitary apoplexy, as well as the differences in surgical outcomes between both groups. The main findings of our study were the following: (i) pituitary apoplexy is more common in men, in hypertensive and obese patients, in patients under treatment with anticoagulants drugs and in those patients with large and invasive pituitary macroadenomas; (ii) the prevalence of headache, visual involvement, and hypopituitarism was greater in the pituitary apoplexy group than in the non-apoplexy group; (iii) surgical remission was four times more common in patients with pituitary apoplexy, but visual improvement and recovery of complete pituitary function was less frequent in this group of patients when compared with patients without pituitary apoplexy and (iv) the development of postsurgical hypopituitarism and permanent diabetes insipidus occurred more commonly in patients with pituitary apoplexy than in those without it.
Regarding demographic and clinical features, we noted a male preponderance in patients with pituitary apoplexy. This finding is in line with the reported in other series of patients with apoplexy [7, 14, 15]. For example, Möller-Goede DL. et al. [14] found that pituitary apoplexy occurred about 3 times more often in men (12%) than in women (4%) (OR 3.36, CI = 1.68–6.71). In addition, the male/female ratio was more than 3:1 in the series of 48 patients reported by Qiang Zhu et al. [15]. Nevertheless, other authors described a higher proportion of females than males in pituitary apoplexy cases [16] or a similar proportion of males and females in other series [17]. Considering that males usually had larger pituitary tumors, it could be expected that the higher prevalence of males in these patients would be related with a larger tumor size and a higher prevalence of invasive pituitary tumors in males than females. Nevertheless, we observed that differences in sex continued being statistically significative after adjusting by tumor size and Knosp grade, so other possible factors may explain these differences.
Among the risk factors of pituitary apoplexy, we identified hypertension, obesity, treatment with anticoagulants and having a large and invasive pituitary macroadenomas. In accordance with our study, precipitating factors are identified in 10–40% of patients who develop a pituitary apoplexy, but this prevalence widely varies depending on which factors are considered risk factors [2,3,4]. According to previous reports, the precipitating factors of pituitary apoplexy include pituitary irradiation, head trauma, hormonal therapy, pregnancy, diabetes mellitus, anticoagulant drugs, pituitary function stimulation test such as insulin, TRH, GnRH, CRH or GHRH tests, and recent surgery, among others [1,2,3,4]. Other more modern precipitating risk factors include COVID-19 vaccination [18] and even the COVID-19 infection itself [19]. Therefore, in accordance with our and previous studies, anticoagulant drugs are a well-known risk factor of pituitary apoplexy. However, male sex and hypertension had not been previously described in other series. The potential link between hypertension and pituitary apoplexy may be explained easily since it has been postulated that any factor that may cause acute changes in vascular supply of pituitary adenomas may potentially be considered a risk factor for pituitary apoplexy. Regarding the association between male sex and apoplexy, it is probably related with the larger tumor size of the pituitary adenoma in males compared to women.
In our series patients presenting with apoplexy had headache, visual involvement, and hypopituitarism more commonly than those without pituitary apoplexy. Headache has been described as the most common initial symptom of patients presenting with apoplexy, reaching up to 95% of the patients [15, 20]. Similarly, rates of visual loss and/or ocular palsy close to 95% has been described in some series [15]. Most previous studies agree that ophthalmoplegia is significantly more common in patients with apoplexy than without [14]; however, some studies did not find differences in the prevalence of headache and hypopituitarism between patients with and without pituitary apoplexy [14]. Nevertheless, these authors also agree that pituitary deficiencies are more common in patients with pituitary apoplexy [21]. It is possible, as it has been previously suggested by other authors [22], that pituitary apoplexy can be approached as a spectrum of disease with three main subtypes, with a different initial presentation and different in-hospital route resulting in different management. In this regard, MC Guijt [22] proposed that pituitary apoplexy may be classified in three groups according with its presentation: Type A (acute pituitary apoplexy); type B (subacute pituitary apoplexy) and type C (non-acute pituitary apoplexy), and the prevalence of the different clinical symptoms varied in these 3 groups. For example, for headache, it occurred in 98.0% of type A pituitary apoplexies, in 90.9% of type B and in 76.0% of type C (p = 0.008). This point is important since we have only included patients who underwent surgery, discarding conservatively managed patients, so it is possible that headache and other clinical manifestations were less common in the group of pituitary apoplexy who did not underwent surgery.
It is no doubt that pituitary apoplexy must be managed by an expert multidisciplinary team including an ophthalmologist, neuroradiologist, endocrinologist, and neurosurgeon. However, even in multidisciplinary teams, surgery may also be harmful, thus, it should be performed in experienced pituitary centers to obtain the best surgical outcomes. Contrary to what has been previously described by other authors [14], we found that surgical remission was four times higher in patients with pituitary apoplexy than in those without. In our series, surgery led to relatively good surgical outcomes in most of the cases, with a rate of surgical cure of 86%, visual improvement in 59% and anterior pituitary function recovery in 22%. Similar rates of complete surgical resection were reported by other authors, ranging from 75 to up to 90% [20, 23]. However, other uncontrolled and retrospective studies have suggested that the outcomes of conservative treatments would be more favorable than surgery [24, 25]. Moreover, several studies have demonstrated that early surgical treatment of the pituitary apoplexy may lead to better outcomes in terms of the preservation of pituitary function compared to delayed surgery [26, 27]. Nevertheless, in light of our results and in agreement with others authors [28], we consider that conservative treatment is only appropriate for selected patients with mild and nonprogressive neuro-ophthalmic defects. The reason why complete resection was higher in patients with pituitary apoplexy than in those without in our series may be related to the fact that intra-adenoma hemorrhage could have facilitated the surgical procedure since the soft consistency and the presence of cystic components allow straightforward removal of the lesion with use of microsuction and curettes in most cases. Nevertheless, we were not able to demonstrate differences in tumor consistency between patients with and without pituitary apoplexy. Another potential explanation may be related to the fact that in apoplexy the entire tumor and gland suffer a vascular insult, and even when tumors are invasive into the cavernous sinus and this area of tumor is not totally resected during surgery, these areas will often disappear on follow-up imaging due to infarction.
We observed that visual improvement and recovery of complete pituitary function was less frequent in patients with pituitary apoplexy than without. The justification of this finding may be related to the fact the acute and high-intensity damage caused by the sudden increase in intrasellar pressure on the optic and oculomotor nerves or the pituitary stalk, that could be much worse tolerated than the chronic and progressive damage caused by a growing progressive pituitary adenoma and could cause partially irreversible lesions [29]. In agreement with these results, a previous study described a rate of 0% of pituitary function recovery in patients who underwent pituitary surgery resection due to pituitary apoplexy, and development of postsurgical hypopituitarism in 33.3% [30]. In relation to visual improvement after surgery for a pituitary apoplexy, some series reported that ophthalmoplegia was alleviated in all patients after surgery, with the recovery of normal vision in 78% and vision improvement in 17% [20]. Similarly, another large series of 75 cases found that ophthalmoplegia improved or normalized in 71% of the patients and visual symptoms in 85.5% [20]. Jackson A. Gondim, et al. [23] also described visual fields and oculomotor improvement in 74.1% and in 67.7% of the patients, respectively. Thus, there is a general agreement that visual symptoms usually improved or disappeared in more than 70% of the cases after surgery, being visual defects one of the main indications of surgery in patients with pituitary apoplexy.
One previous study also described a higher rate of new pituitary deficiencies after surgery in patients with apoplexy than without it [14]. In this study, the authors compared surgical outcomes of patients with and without pituitary apoplexy, and they found that the frequency of hypopituitarism increased (from 45% at presentation to 71% during follow-up, OR = 4.7, CI = 1.30–25.33) in the patients with pituitary apoplexy, whereas it did not change in the control group [14]. One study of 75 patients with pituitary apoplexy who underwent surgery also reported that hypopituitarism worsened in 20% of the patients and diabetes insipidus occurred in 5.3% of the patients after surgery [20]. This is similar to the reported by other authors, even higher rates of postsurgical hypopituitarism, reaching to up to 80% of the patients has been described [23]. So, when surgery is indicated due to pituitary apoplexy, it should be taken into account, that despite the clear benefits of surgery regarding surgical cure and visual improvement, there is a no negligible risk of producing hypopituitarism and diabetes insipidus. These findings suggest that in cases of pituitary apoplexy without visual involvement, conservative management may be more appropriate.
We are aware that our study is not free of some limitations, including, mainly, its retrospective nature. In addition, the surgeries were performed by experienced neurosurgeons at three tertiary pituitary centers. So, the results may not be applicable to all institutions with less skilled neurosurgeons. Furthermore, we know that the differences in surgical outcomes between patients with and without apoplexy should be interpreted with caution since they are two totally different groups of patients, including a higher proportion of large and invasive pituitary macroadenomas in the group of patients presenting with pituitary apoplexy compared with those without pituitary apoplexy. However, one of the main strengths of our study is the relatively large of patients included, the direct comparation with a control group without pituitary apoplexy and the consecutively inclusion of the cases in a predefined period. Moreover, the multicenter nature of the study should be considered as another strength of our study, providing a higher external validity of our results.
Conclusion
Surgical resection is more common in patients presenting with pituitary apoplexy than those without pituitary apoplexy; however, visual improvement and recovery of complete pituitary function is more common in patients without apoplexy. The risk of new pituitary deficits and permanent diabetes insipidus is higher in patients with apoplexy than in those without it.
Availability of data and materials
Data might be available upon reasonable request to the authors.
References
Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P (2015) Pituitary Apoplexy. Endocr Rev 36:622–645. https://doi.org/10.1210/ER.2015-1042
Ayuk J, McGregor EJ, Mitchell RD, Gittoes NJL (2004) Acute management of pituitary apoplexy–surgery or conservative management? Clin Endocrinol (Oxf) 61:747–752. https://doi.org/10.1111/J.1365-2265.2004.02162.X
Dubuisson AS, Beckers A, Stevenaert A (2007) Classical pituitary tumour apoplexy: clinical features, management and outcomes in a series of 24 patients. Clin Neurol Neurosurg 109:63–70. https://doi.org/10.1016/J.CLINEURO.2006.01.006
Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF et al (2004) Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases, vol 7. Pituitary. https://doi.org/10.1007/s11102-005-1050-3
Gruber A, Clayton J, Kumar S, Robertson I, Howlett T, Mansell P (2006) Pituitary apoplexy: retrospective review of 30 patients–is surgical intervention always necessary? Br J Neurosurg 20:379–385. https://doi.org/10.1080/02688690601046678
Nawar RN, AbdelMannan D, Selman WR, Arafah BM (2008) Pituitary tumor apoplexy: a review. J Intensive Care Med 23:75–90. https://doi.org/10.1177/0885066607312992
Arbunea-Ghenoiu S, Ciubotaru GV, Dumitrascu A, Alexandrescu D, Capatina C, Poiana C Pituitary apoplexy: a retrospective study of 36 cases from a single Center. Cureus 2022;14. https://doi.org/10.7759/CUREUS.29769
Araujo-Castro M, Pascual-Corrales E, Acitores Cancela A, García Duque S, Ley Urzaiz L, Rodríguez Berrocal V (2020) Status and clinical and radiological predictive factors of presurgical anterior pituitary function in pituitary adenomas. Study of 232 patients. Endocrine 70:584–592. https://doi.org/10.1007/S12020-020-02455-6
Rajasekaran S, Vanderpump M, Baldeweg S, Drake W, Reddy N, Lanyon M et al (2011) UK guidelines for the management of pituitary apoplexy. Clin Endocrinol (Oxf) 74:9–20. https://doi.org/10.1111/J.1365-2265.2010.03913.X
Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R et al (2016) Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2016-2118
Knosp E, Steiner E, Kitz K, Matula C, E K (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–618. https://doi.org/10.1227/00006123-199310000-00008
Jho HD, Carrau RL, Ko Y, Daly MA (1997) Endoscopic pituitary surgery: an early experience. Surg Neurol 47:213–222. https://doi.org/10.1016/S0090-3019(96)00452-1
Araujo-Castro M, Mariño-Sánchez F, Acitores Cancela A, García Fernández A, García Duque S, Rodríguez Berrocal V (2020) Is it possible to predict the development of diabetes insipidus after pituitary surgery? Study of 241 endoscopic transsphenoidal pituitary surgeries. J Endocrinol Invest. https://doi.org/10.1007/s40618-020-01448-6
Möller-Goede DL, Brändle M, Landau K, Bernays RL, Schmid C (2011) Pituitary apoplexy: re-evaluation of risk factors for bleeding into pituitary adenomas and impact on outcome. Eur J Endocrinol 164:37–43. https://doi.org/10.1530/EJE-10-0651
Zhu Q, Liang Y, Fan Z, Liu Y, Zhou C, Zhang H et al (2022) Ischemic infarction of Pituitary Apoplexy: a retrospective study of 46 cases from a single Tertiary Center. Front Neurosci 15. https://doi.org/10.3389/fnins.2021.808111
Galal A, Ahmed OEF (2022) Determinants of visual and endocrinological outcome after early endoscopic endonasal surgery for pituitary apoplexy. Surg Neurol Int 13. https://doi.org/10.25259/SNI_642_2022
Geyi̇k AM, Durmz MO, Dogan A, Ugur BK, Geyik S, Erkutlu İ et al (2022) Pituitary apoplexy: an emergent and potential life-threatening complication of pituitary adenomas. Ulus Travma Acil Cerrahi Derg 28:483–489. https://doi.org/10.14744/TJTES.2021.93539
Aliberti L, Gagliardi I, Rizzo R, Bortolotti D, Schiuma G, Franceschetti P et al (2022) Pituitary apoplexy and COVID-19 vaccination: a case report and literature review. Front Endocrinol (Lausanne) 13. https://doi.org/10.3389/FENDO.2022.1035482
Al-Salameh A, Balmain J, Desailloud R (2022) Pituitary apoplexy and SARS-CoV-2 infection: we need to look beyond the acute phase. Eur J Endocrinol 187:L3–4. https://doi.org/10.1530/EJE-22-0736
Sun Z, Cai X, Li Y, Shao D, Jiang Z (2021) Endoscopic endonasal Transsphenoidal Approach for the Surgical treatment of Pituitary Apoplexy and Clinical Outcomes. Technol Cancer Res Treat 20. https://doi.org/10.1177/15330338211043032
Takeshita K, Abe I, Kameda W, Ishii K, Fujita Y, Nagata M et al (2022) Clinical evaluations of pituitary apoplexy in incidental nonfunctional pituitary adenomas. Med (Baltim) 101:e32026. https://doi.org/10.1097/MD.0000000000032026
Guijt MC, Zamanipoor Najafabadi AH, Notting IC, Pereira AM, Verstegen MJT, Biermasz NR et al (2022) Towards a pituitary apoplexy classification based on clinical presentation and patient journey. Endocrine 76:132–141. https://doi.org/10.1007/S12020-022-02983-3
Gondim JA, de Albuquerque LAF, Almeida JP, Bulcao T, Gomes E, Schops M et al (2017) Endoscopic endonasal surgery for treatment of Pituitary Apoplexy: 16 years of experience in a Specialized Pituitary Center. World Neurosurg 108:137–142. https://doi.org/10.1016/J.WNEU.2017.08.131
Pal A, Capatina C, Tenreiro AP, Guardiola PD, Byrne JV, Cudlip S et al (2011) Pituitary apoplexy in non-functioning pituitary adenomas: long term follow up is important because of significant numbers of tumour recurrences. Clin Endocrinol (Oxf) 75:501–504. https://doi.org/10.1111/J.1365-2265.2011.04068.X
Teixeira JC, Lavrador J, Simão D, Miguéns J (2018) Pituitary Apoplexy: should endoscopic surgery be the Gold Standard? World Neurosurg 111:e495–e499. https://doi.org/10.1016/J.WNEU.2017.12.103
Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P (2015) Pituitary apoplexy. vol. 36. Endocr Rev; https://doi.org/10.1210/er.2015-1042
Chacko AG, Chacko G, Seshadri MS, Chandy MJ (2002) Hemorrhagic necrosis of pituitary adenomas. Neurol India 50:490–493
Bujawansa S, Thondam SK, Steele C, Cuthbertson DJ, Gilkes CE, Noonan C et al (2014) Presentation, management and outcomes in acute pituitary apoplexy: a large single-centre experience from the United Kingdom. Clin Endocrinol (Oxf). https://doi.org/10.1111/cen.12307
Carlson AP, Stippler M, Myers O (2013) Predictive factors for vision recovery after optic nerve decompression for chronic compressive neuropathy: systematic review and meta-analysis. J Neurol Surg B Skull Base 74:20–38. https://doi.org/10.1055/S-0032-1329624
Shaikh AA, Williams DM, Stephens JW, Boregowda K, Udiawar MV, Price DE (2022) Natural history of pituitary apoplexy: a long-term follow-up study. Postgrad Med J. https://doi.org/10.1136/POSTGRADMEDJ-2022-141836
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Marta Araujo-Castro wrote the draft of the manuscript and prepared figures and tables; all authors collected the data of the patients included in the study and reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the participants of the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study has been approved by the local Ethical Committee of the HURC (approval date: 4 October 2019, code: ACTA 372 and approval date: February 2022).
Competing interests
The authors have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Araujo-Castro, M., Paredes, I., Pérez-López, C. et al. Differences in clinical, hormonal, and radiological presentation and in surgical outcomes in patients presenting with and without pituitary apoplexy. A multicenter study of 245 cases. Pituitary 26, 250–258 (2023). https://doi.org/10.1007/s11102-023-01315-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-023-01315-6