Abstract
Background As an alternative to vitamin K antagonist and low-dose aspirin (< 325 mg), non-vitamin K oral anticoagulants are available for the prevention of stroke in patients with atrial fibrillation. However, the mortality risk associated with these drugs in daily practice remains unclear. Objective To evaluate the risk of all-cause mortality associated with non-Vitamin K antagonist oral anticoagulants, vitamin K antagonists or aspirin in patients with atrial fibrillation. Setting A cohort study conducted among atrial fibrillation patients using the UK Clinical Practice Research Datalink (March 2008–October 2014). Method New users of vitamin K antagonists, non vitamin K oral anticoagulants, low-dose aspirin, or combination therapy were followed from the date of first prescription to the date of death, as recorded in the UK datalink. Cox proportional hazard models estimated the hazard ratio (HR) of all-cause mortality for users of NOACs, aspirin, or combination use, as compared to vitamin K antagonist. Analyses were adjusted for confounders. Main outcome measure All-cause mortality. Results We identified 31,497 patients. Non vitamin K antocoagulant use (adjusted HR [aHR] = 1.42; 95% Confidence Interval [CI] 1.18–1.71) and aspirin use (aHR = 1.64; 95% CI 1.57–1.77) were both significantly associated with a higher mortality risk than use of vitamin K antagonists. The higher mortality risk for the non vitamin K anticoagulant use was observed in men (aHR = 1.72; 95% CI 1.25–2.36), but not in women (aHR = 1.28; 95% CI 0.92–1.79. Compared to vitamin K antagonists, mortality risk associated with the non vitamin K anticoagulants and aspirin use was significantly increased in patients with higher stroke risk (CHA2DS2-VASc > 2). Conclusion Non vitamin K oral anticoagulants are associated with a higher risk on all-cause mortality, particularly in men and in patients with higher stroke risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
The use of NOACs by atrial fibrillation patients is associated with an increased risk of all-cause mortality; the increased risk is promionent among male patients and those with high CHA2DS2-VASc scores.
-
The increased all-cause mortality risk likely reflects clinical practice where high-risk patients receive NOACs over VKA or aspirin.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and is associated with a doubled rate of mortality [1, 2]. Oral anticoagulants have been shown to significantly reduce all-cause mortality rates in AF patients by up to 26% [3]. Until 2012, Vitamin K antagonists (VKAs, such as warfarin or acenocoumarol) were the predominant class of oral anticoagulant therapy for the treatment of AF. However, VKAs require frequent hematological monitoring [4]. As an alternative, non-vitamin K antagonist oral anticoagulants (NOACs) were developed, which are prescribed in fixed doses and administered without hematological monitoring.
The CHA2DS2-VASC risk score is recommended for guiding the choice of antithrombotic treatment and is calculated using known risk factors for stroke [5]. Since 2012, based on the results of randomised controlled trials, it is recommended that patients with a CHA2DS2-VASC ≥ 2 receive NOAC therapy or VKA [6,7,8,9]. This preference was reflected in the 2016 treatment guidelines for AF [5]. Prior to 2012, aspirin was recommended for the treatment of patients at low risk for stroke [5, 6]. However, this is no longer the case due to evidence of the superiority of VKA therapy [3]. These frequent updates to recommendations indicate that anticoagulation is a fast-moving field, making it difficult for the prescriber to immediately adhere to the most recent guidelines [5, 6].
Clinical trial data suggest that NOACs may significantly reduce the risk of stroke and intracranial bleeding when compared with warfarin (VKA) therapy [7,8,9,10,11,12,13]. However, the reduction in mortality risk as a secondary endpoint in clinical trials was not significant for NOACs [7,8,9], with the exception of edoxaban [14]. While some observational studies suggest a reduced risk of all-cause mortality among NOAC users, as compared to VKAs [15,16,17,18,19,20,21,22], the evidence is conflicting. Importantly, many observational studies use an ever versus never exposure definition that does not permit switching between medications. Moreover, in many of these studies, they were unable to statistically adjust for lifestyle factors that may influence mortality, such as body mass index and smoking status. Finally, these studies did not exclude prior aspirin use in AF [15,16,17,18,19,20,21,22,23,24,25,26]. Although low-dose aspirin has been removed from the treatment guidelines for AF, use is still observed.
Aim of the study
We aimed to evaluate the risk of all-cause mortality in AF patients newly prescribed NOACs, VKAs or low dose aspirin in a UK general practice population.
Ethics approval
The study protocol was approved by the Independent Scientific Advisory Committee for the Medicines and Healthcare products Regulatory Agency database research, protocol 14-121.
Method
Data source
We conducted a population-based cohort study using primary care data from the Clinical Practice Research Datalink (CPRD; www.cprd.com). The CRPD primary care database is one of the world’s largest routinely collected databases, containing medical records of approximately 7% of the UK population [27]. Data includes demographic information, laboratory tests, specialist referrals, hospital admissions, prescription details, and some lifestyle variables such as body mass index (BMI) [28]. Previous studies have shown a high degree of accuracy and completeness [29, 30]. Additionally, data undergo regular quality checks and practices are considered up to research standard from the date they meet the specified data quality criteria.
Study population
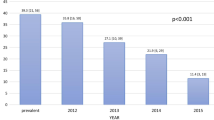
The study population consisted of patients aged 18 years or older with a first ever-recorded diagnosis of AF during the period of valid data collection. We identified patients between 18 March 2008 (the date of market introduction of the first NOAC) and 1 October 2014. Within this cohort of AF patients, we identified new users of antithrombotic drugs: VKAs, NOACs and low dose (≤ 325 mg) aspirin. Patients receiving combinations of the eligible study drugs were identified as combination users, thereby generating mutually exclusive exposure groups. The index date (or start of follow-up) began on the first prescription date of an eligible antithrombotic drug prescription by the general practitioner. All patients had a minimum of one year of valid data collection prior to their index date, and new users were defined as patients who were not exposed to the drugs of interest in the year prior to their index date. Patients were followed from the index date to the end of data collection, date of transfer of the patient out of the practice area or death (outcome of interest), whichever came first.
Exposure
The period of follow-up was divided into 30-day periods, starting with the index date. The 30-day periods were selected as the median prescription length in the UK is 28-days. At the start date of each 30-day period, exposure to antithrombotic agents was identified and patients were categorized as current or past users based on the time since last prescription. Patients who received a prescription for an antithrombotic agent in the 30 days before the start of an interval was defined as current user, while those with a prescription > 30-days prior to the start of an interval were defined as past users. All patients were current users of one of the eligible study drugs at the index date and classified into mutually exclusive exposure groups: VKA only (warfarin, acenocoumarol or phenindione), NOAC only (dabigatran, rivaroxaban or apixaban), aspirin only, or combined use of more than one of the three main study drugs. During the period of analysis edoxaban was not yet registered in the UK.
Outcome
The primary outcome of interest was all-cause mortality. Patients were followed from the index date until the end of data collection, date of transfer of the patient out of the practice, or death recorded in CPRD, whichever came first.
Potential confounders
Confounders were identified using read-codes following a review of the literature and clinical expert advice. Sex, body mass index (BMI), smoking status and alcohol use were identified at baseline. In addition to age, a history of the following conditions were included time-dependently, as evaluated prior to the start of each 30-day interval: congestive heart failure, cerebrovascular disease, history of acute myocardial infarction (AMI), ischaemic heart disease, peripheral artery disease, family history of vascular disease, acute or chronic renal failure, liver dysfunction and malignancies. The presence of a comorbidity was identified as a read-code any time prior to the start of index, or the start of an interval. In addition, the following drug prescriptions were assessed in the 6 months prior to the start of a 30-day interval; statins, calcium channel blockers, glucocorticoids, Angiotensin Converting Enzyme-inhibitors (ACE-inhibitors), Angiotensin II-blockers (ATII-blockers), diuretics, beta-blockers, proton pump inhibitors (PPIs), antiplatelet drugs (excluding aspirin), anticoagulant drugs (excluding VKAs and NOACs), anti-arrhythmic drugs, nitrates, antidiabetic drugs and insulin. To correct for changes in prescribing guidelines for antithrombotic therapy of AF patients, we adjusted for calendar year.
Statistical analyses
Baseline characteristics were stratified by drug group and summarized as means and standard deviations, or counts and proportions, where appropriate. Crude incidence rates of all-cause mortality per 1000 person-years (py) were calculated. Cox proportional hazard models estimated the adjusted hazard ratios (HR) using the SAS 9.2 PHREG procedure. Sensitivity analyses stratified by sex and CHA2DS2-VASc score were additionally conducted. The CHA2DS2-VASc score was calculated at baseline and time-dependently (at the start of each period), and categorized into three groups: high (≥ 4), medium (> 1 and < 4) or low (≤ 1).
In all models, VKA use was the reference group. Potential confounders were included in the final model if they independently changed the beta-coefficient by at least 5%, or when a consensus about inclusion existed among co-authors, and was supported by clinical evidence from the literature. Missing data for BMI, smoking status and alcohol use were included in the model using an indicator for missingness.
Results
We identified a total of 31,497 eligible AF patients aged ≥ 18 years, and with use of an antithrombotic agent (Fig. 1). At index prescription, 1306 (4.1%) patients were NOAC users, 13,643 (43.3%) were VKA users, 16,094 (51.1%) were aspirin users, and 454 individuals (1.4%) were prescribed more than one type of antithrombotic agent (Table 1). In the NOAC group, the majority of patients were prescribed rivaroxaban (71.5%), and 28.5% were prescribed dabigatran. We did not identify any users of apixaban at index date during our study period. Age, BMI, smoking status and alcohol use was comparable between exposure groups at baseline. The mean CHA2DS2-VASc score was also comparable across all groups at baseline. The mean duration of follow-up was shorter for users of NOACs (0.6 years) than for users of VKAs (1.9 years) or aspirin (1.9 years). Users of NOACs (18.9%) more often had a history of cerebrovascular disease, as compared with users of VKAs (13.4%) or low dose aspirin (6.1%). Supplementary Table 1 provides the baseline characteristics stratified by CHA2DS2-VASc score.
Table 2 presents the primary analysis identifying the risk of all-cause mortality associated with antithrombotic use. NOAC use (adjusted HR [aHR] = 1.42; 95% Confidence Interval [CI] 1.18–1.71) and aspirin use (aHR = 1.64; 95% CI 1.57–1.77) were associated with a significantly higher mortality risk, as compared to VKA users (Table 2). Among those with combined anticoagulation therapy, no statistically significant (aHR = 1.22; 95% CI 0.93–1.61) difference in all-cause mortality was observed, when compared to VKA users.
Sex stratified analysis
Table 3 presents the sex-stratified analyses for users. Among females, only aspirin use was associated with a significant risk of all-cause mortality (aHR = 1.67; 95% CI 1.51–1.86), as compared to female VKA users. In contrast, the risk of all-cause mortality in males was highest among users of NOACs (aHR = 1.72; 95% CI 1.25–2.36) and aspirin (aHR = 1.63; 95% CI 1.46–1.82), as compared to male users of VKAs. In both sexes, combined use was associated with a non-significant increase in all-cause mortality.
CHA2DS2-VASc stratified analysis
The risk of mortality associated with antithrombotic therapy as stratified by the three CHA2DS2-VASc groups (high, medium and low) is provided in Table 4. Patients with a CHA2DS2-VASc ≤ 1 (low) did not show a significantly increased risk for all-cause mortality in any of the exposure groups when compared to users of VKAs with a low CHA2DS2-VASc score (Table 4). Among patients with a medium CHA2DS2-VASc score (2–3), NOAC use (aHR = 1.54; 95% CI 1.17–2.03) and aspirin use (aHR = 1.97; 95% CI 1.77–2.19) were associated with a significantly increased risk for all-cause mortality, compared to users of VKAs. Similarly, when examining patients with a high CHA2DS2-VASc score (≥ 4), patients using NOACs (aHR = 1.38; 95% CI 1.06–1.80), and aspirin (aHR = 1.74; 95% CI 1.57–1.94) had a significantly increased risk for all-cause mortality, as compared to users of VKAs. Similar to the previous results, combined use of the antithrombotic agents was not associated with an increased mortality risk in any of the strata.
Discussion
In this population-based cohort study of adult AF patients, we observed an increased risk of all-cause mortality for patients receiving NOACs, as compared to users of VKAs. This increased risk was mainly driven by patients with a CHA2DS2-VASc score above 2 (medium to high stroke risk), and was stronger among male patients.
Our primary analysis, showing a 42% increased risk in mortality associated with NOACs, is not directly in-line with the phase-III randomised trials [7,8,9, 14, 31]. As our analysis included dabigitran and rivaroxaban exposure, the ROCKET and RELY trials are of particular interest. In these studies, there was no significant difference in all-cause mortality identified for dabigitran 110 mg (HR 0.91 95% CI 0.80–1.03), dabigitran 150 (HR 0.88 95% CI 0.77–1.00) and rivaroxaban (HR 0.85 95% CI 0.70–1.02), when compared with warfarin exposure [7, 8]. Naturally, it is expected that the population in our observational study would differ from randomised controlled trials, as patients in clinical practice are not prescribed based on randomization, but rather clinical judgement and the most recent prescribing guidelines. Indeed, despite applying a new user design, sicker (high-risk) patients may have been channeled to the NOAC patients group, and thus had a higher mortality risk at baseline. Additionally, sicker patients may have switched to NOACs if they had a thromboembolic event while on VKA or aspirin therapy. The higher risk of mortality observed among aspirin users, compared to VKA, is comparable to earlier studies [3].
Moreover, we identified a significantly increased mortality risk associated with NOAC and aspirin use among patients with a medium or high CHA2DS2-VASc score. When examining the baseline differences, NOAC patients with a high stroke risk had an increased history of cerebrovascular disease or myocardial infarction compared to VKA users (Supplementary Table 1). While we did adjust for this in our analysis, the confounding by indication may explain the differences in mortality risk observed in our study when compared to clinical trial data. Moreover, as patients in our study were permitted to switch between exposure groups, it is possible that the patients who switched to NOAC therapy during follow-up were, again, the higher-risk patients. Finally, the high mortality risk among aspirin users is noteworthy as this seemingly confirms prior evidence on the lack of effectiveness, especially among patients with a moderate to high stroke risk [3].
Interestingly, in this study we identified differences in all-cause mortality between sexes, particularly with regard to NOAC exposure. As compared to VKA users of the same sex, we observed a significant 1.7-fold increase in all-cause mortality risk among males exposed to NOACs, yet a non-significant increased risk was observed for females. In the UK, males had a higher risk of death due to heart disease than females aged 50–79 in 2015 [32]. Additionally, a previous study using a similar cohort indicated a higher risk of AMI in males using NOAC than in males using VKA [33]. In a recent study comparing rivaroxaban to dabigatran, rivaroxaban was significantly associated with an increased risk of bleeding and intracranial hemorrhage in both males and females, while mortality risk associated with rivaroxaban was greater in males [34]. While there is no underlying mechanism of action to explain the observed sex differences, this finding may reflect differential prescribing. However, since the available evidence on gender differences in the utilization, safety, and effectiveness of NOACs is mixed, further research in this area is warranted.
There have been a number of observational studies examining the safety and effectiveness of NOACs with conflicting results [15,16,17,18,19,20,21,22,23,24,25,26, 34]. When comparing results with other observational studies, it is important to note that rivaroxaban was the most frequently prescribed NOAC in our cohort (71.5%). This is important in light of the growing body of evidence indicating that there may be differences between the available NOACs. Recent observational studies [17, 24, 25, 35] identified that mortality was lower for dabigatran when compared to warfarin, but not for rivaroxaban. [17, 24, 25, 35]. In contrast, two other studies identified a higher mortality rate for rivaroxaban [23, 26], yet all-cause mortality was not higher among dabigatran users [23, 26].
Many of the conflicting results [15,16,17,18,19,20,21,22] may be explained by key methodological differences that make comparisons difficult. Previous observational studies have used propensity score-matched cohort designs to examine differences in mortality risk between NOAC and VKA use. While propensity score-matching mimics the randomization in clinical trials and allows for the assessment of the comparative safety of the two drugs, it does not reflect real life clinical practice. Thus, these studies answer very different questions. Importantly, these studies also do not permit a time-dependent analysis of exposure. We defined exposure time-dependently, thereby capturing all patient-time and permitting patients to switch between therapies and discontinue use (i.e., past users). Most existing studies examined only monotherapy or censored patients at time of treatment switch/discontinuation, thereby truncating the follow-up time. Consequently, if a patient initiated on warfarin (VKA) and then switched to a NOAC during follow-up they would be included in our study yet excluded from the published studies. This may lead to an underestimation of outcomes and effect, particularly in the NOAC group. We believe this is an important methodological consideration, as all person time should be accounted for in follow-up.
In addition to those already mentioned, our study has limitations that merit consideration. While we adjusted for the factors that were independently associated in a univariate model, we cannot rule out the potential for residual confounding. While we were able to include lifestyle factors that are important for all-cause mortality such as patient BMI, smoking status and alcohol use, we cannot rule out the possibility of other unmeasured confounding. Second, we lacked the power to differentiate between the NOACs and the different dosages. Therefore, we were unable to identify any potential differences in mortality risk between NOACs that may have been of clinical interest [3, 13, 22,23,24,25]. Additionally, while four NOACs are currently (as of 2019) approved by the European Medicine’s Agency (dabigatran, rivaroxaban, apixaban and edoxaban) we were unable to include apixaban and edoxaban as there was no use in our population at the time of inclusion. Furthermore we were unable to directly assess renal function, which affects NOAC concentrations and can impact their efficacy. Finally, there are some limitations to our data. It is possible that the true start date may have been misclassified if the first prescription was dispensed in hospital or over the counter for aspirin. Additionally, our data is not linked to the official death certificates, meaning we do not have the official cause of death, allowing the evaluation of cause-specific mortality.
Despite the limitations, our study has a number of strengths. The CPRD data includes extensive clinical information and therefore permitted the inclusion of important confounders, including lifestyle factors not included in most datasets (e.g., BMI, smoking status and alcohol use). To our knowledge, this is the first study of antithrombotic efficacy to include aspirin as a separate treatment category and not combined with other therapies. Moreover, we excluded users with past aspirin use, creating a true new user design. Importantly, patients were followed time-dependently, allowing dynamic exposure patterns. By allowing patients to be variably exposed to different treatments over time, we minimized the potential for bias, a pitfall inherent to time-invariant exposure models. Simultaneously, our focus on total person-years of exposure per treatment rather than on unique users allowed us to more accurately assess patient exposure to each antithrombic agent.
Conclusion
Adult patients with AF using NOACs or aspirin were have an increased risk for all-cause mortality when compared to VKA users. More research into the underlying mechanisms for this finding is required, particularly for rivaroxaban.
References
Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–52.
Stewart S, Hart CL, Hole DJ, Mc Murray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–64.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
Heidbuchel H, Verhamme P, Alings M, Antz M, Hacke W, Oldgren J, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15(5):625–51.
Kirchof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18(11):1609–78.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 Focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Europace. 2012;14:1385–413.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel M, Mahaffey K, Garg J, Pan G, Singer D, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Granger C, Alexander J, McMurray JJ, Lopes R, Hylek E, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Miller C, Grandi S, Shimony A, Filion K, Eisenberg M. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110:453–60.
Ruff C, Giugliano R, Braunwald E, Hoffman E, Deenadayalu N, Ezekowitz M, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Dentali F, Riva N, Crowther M, Turpie AG, Lip GY, Ageno W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126:2381–91.
Ntaios G, Papavasileiou V, Diener H, Makaritsis K, Michel P. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298–304.
Guigliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131(2):157–64.
Larsen TB, Rasmussen LH, Skjøth F, Due KM, Callréus T, Rosenzweig M, et al. Efficacy and safety of dabigatran etexilate and warfarin in “real-world” patients with atrial fibrillation: a prospective nationwide cohort study. J Am Coll Cardiol. 2013;61(22):2264–73.
Larsen TB, Skjøth F, Nielsen PB, Kjældgaard JN, Lip GY. Comparative effectiveness and safety of non-vitamin K anatagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.
Villines TD, Schnee J, Fraeman K, Siu K, Reynolds MW, Collins J, et al. A comparison of the safety and effectiveness of dabigatran and warfarin in non-valvular atrial fibrillation patients in a large healthcare system. Thromb Haemost. 2015;114:1290–8.
Leef G, Qin D, Althouse A, Alam MB, Rattan R, Munir MB, et al. Risk of stroke and death in atrial fibrillation by type of anticoagulation: a propensity-matched analysis. Pacing Clin Electrophysiol. 2015;38(11):1310–6.
Friberg L, Oldgren J. Efficacy and safety of non-vitamin K antagonist oral anticoagulants compared with warfarin in patients with atrial fibrillation. Open Heart. 2017;4:000682.
Serebruany V, Cherepanov V, Fortmann S, Kim MH. Mortality and oral anticoagulants in the Food and Drug Administration adverse event reporting system. Open Heart. 2017;4:e000629.
Graham DJ, Baro E, Zhang R, Liao J, Wernecke M, Reichman ME, et al. Comparative stroke, bleeding, and mortality risks in older Medicare patients treated with oral anticoagulants for nonvalvular atrial fibrillation. Am J Med. 2019;000:1–9.
Ujeyl M, Köster I, Stammschulte T, Hein R, Harder S, Gundert-Remy U. Comparative risk of bleeding, ischemic stroke and mortality with direct oral anticoagulants versus phenprocoumon in patients with atrial fibrillation. Eur J Clin Pharmacol. 2018;74:1317–25.
Esteve-Pastor MA, Rivera-Caravaca JM, Roldán V, Orenes-Piñero E, Romiti GF, Romanazzi I, et al. Estimated effectiveness and safety of nonvitamin K antagonist oral anticoagulants compared with optimally acenocoumarol anticoagulated “real-world” in patients with atrial fibrillation. Am J Cardiol. 2018;122:785–92.
Hohnloser SH, Basic E, Hohmann C, Nabauer M. Effectiveness and safety of non-vitamin K oral anticoagulants in comparison to phenprocoumon: data form 61,00 patients with atrial fibrillation. Thromb Hamost. 2018;118:803–5.
Nielsen PB, Skjoth F, Sogaard M, Nordstrom Kjaeldgaard J, Lip GY, Bjerregaard Larsen T. Effectiveness and safety of reduced dos non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510.
Herrett E, Gallagher A, Bhaskaran K, Forbes H, Mathur R, van Staa T, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44:827–36.
Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:e128.
Lewis JD, Brensinger C. Agreement between GPRD smoking data: a survey of general practitioners and a population-based survey. Pharmacoepidemiol Drug Saf. 2004;13(7):437–41.
Van Staa TP, Abenhaim L, Cooper C, Zhang B, Leufkens HG. The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf. 2000;9(5):359–66.
Kim IS, Kim HJ, Kim TH, Uhm JS, Joung B, Lee MH, et al. Non-vitamin K antagonist oral anticoagulants have better efficacy and equivalent safety compared to warfarin in elderly patients with atrial fibrillation: a systematic review and meta-analysis. J Cardiol. 2018;72:105–12.
Office for National Statistics. Does our sex affect what we die from? 13 July 2016 [Cited 2017 March 6]. http://www.ons.gov.uk/.
Stolk LM, de Vries F, Ebbelaar C, de Boer A, Schalekamp T, Souverein P, et al. Risk of myocardial infarction in patients with atrial fibrillation using vitamin K antagonists, aspirin of direct acting oral anticoagulants. Br J Clin Pharmacol. 2017;83(8):1835–43.
Graham DJ, Reichman ME, Wernecke M, Hsueh YH, Izem R, Southworth MR, et al. Stroke, bleeding, and mortality risks in elderly Medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation. JAMA Intern Med. 2016;176(11):1662–71.
Gorst-Rasmussen A, Lip GY, Larsen TB. Rivaroxaban versus warfarin and dabigatran in atrial fibrillation: comparative effectiveness and safety in Danish routine care. Pharmacoepidemiol Drug Saf. 2016;25:1236–44.
Acknowledgements
We would like to thank Prof. Dr. Hubert Leufkens for his thoughtful discussions provided during the preparation of the manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors that they have declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Gieling, E., de Vries, F., Williams, R. et al. Mortality risk in atrial fibrillation: the role of aspirin, vitamin K and non-vitamin K antagonists. Int J Clin Pharm 41, 1536–1544 (2019). https://doi.org/10.1007/s11096-019-00916-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00916-1