Abstract
Background
Although kinase inhibitors (KIs) are generally effective, their use has a large impact on the current health care budget. Dosing strategies to reduce treatment costs are warranted. Boosting pharmacokinetic exposure of KIs metabolized by cytochrome P450 (CYP)3A4 with ritonavir might result in lower doses needed and subsequently reduces treatment costs. This study is a proof-of-concept study to evaluate if the dose of erlotinib can be reduced by co-administration with ritonavir.
Methods
In this open-label, cross-over study, we compared the pharmacokinetics of monotherapy erlotinib 150 mg once daily (QD) (control arm) with erlotinib 75 mg QD plus ritonavir 200 mg QD (intervention arm). Complete pharmacokinetic profiles at steady-state were taken up to 24 h after erlotinib intake for both dosing strategies.
Results
Nine patients were evaluable in this study. For the control arm, the systemic exposure over 24 h, maximum plasma concentration and minimal plasma concentration of erlotinib were 29.3 μg*h/mL (coefficient of variation (CV):58%), 1.84 μg/mL (CV:60%) and 1.00 μg/mL (CV:62%), respectively, compared with 28.9 μg*h/mL (CV:116%, p = 0.545), 1.68 μg/mL (CV:68%, p = 0.500) and 1.06 μg/mL (CV:165%, p = 0.150) for the intervention arm. Exposure to the metabolites of erlotinib (OSI-413 and OSI-420) was statistically significant lower following erlotinib plus ritonavir dosing. Similar results regarding safety in both dosing strategies were observed, no grade 3 or higher adverse event was reported.
Conclusions
Pharmacokinetic exposure at a dose of 75 mg erlotinib when combined with the strong CYP3A4 inhibitor ritonavir is similar to 150 mg erlotinib. Ritonavir-boosting is a promising strategy to reduce erlotinib treatment costs and provides a rationale for other expensive therapies metabolized by CYP3A4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Identification of oncogenic driver mutations has shifted the treatment paradigm in cancer towards the use of oral kinase inhibitors (KIs) (1). The last decades, many KIs have been developed for these driver mutations and certainly more will follow. Since the costs of these drugs have a large impact on the healthcare budget (2), new and efficient dosing strategies are warranted to use KIs as effectively as possible.
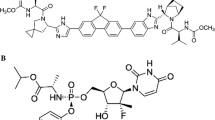
For many KIs, pharmacokinetic exposure at the approved dosing regimen is related to efficacy and/or toxicity and thus plays an important role in treatment outcome (3). Most of the KIs are metabolized via the cytochrome P450 (CYP)3A4 enzyme system (4). Inhibition of this enzyme system can thus result in higher exposure of the drug and might allow for lower dosages to reduce health care costs. Erlotinib is a KI which inhibits the epidermal growth factor receptor (EGFR) and has several indications in e.g. non-small cell lung cancer (NSCLC) and in pancreatic cancer in a dosing regimen of 150 mg once daily (QD) (5). In other tumor types bearing EGFR-driver mutations, erlotinib treatment has been shown to be potentially therapeutic (6, 7). Erlotinib is for approximately 70% metabolized by CYP3A4 and for the remaining part by CYP1A2 (8). The hydroxylation, oxidation and/or O-desmethylation of erlotinib by these CYP-enzymes result in many different metabolites (9). Most of these metabolites are found to be inactive, however, it is thought that the main O-desmethylated products of these metabolic routes, OSI-413 and OSI-420, exhibit some antitumor activity, although, in comparison with erlotinib this effect seems limited (5). It has been postulated that the current dosing of erlotinib is at the top of its exposure-efficacy curve and thus lower doses could be equally beneficially (10). Therefore, this drug is ideally suited as an example KI to study the effects of interacting medications on its pharmacokinetics.
In a previous study, it has been found that ketoconazole, a potent CYP3A4 inhibitor, is able to increase the area under the plasma concentration-time curve from zero to infinity (AUC0-∞) and maximum concentration (Cmax) of erlotinib by approximately a twofold in healthy volunteers (8). A drug, more commonly used to boost the pharmacokinetics of other drugs is ritonavir (11,12,13). Similar to ketoconazole, it is a potent CYP3A4 inhibitor associated with relatively low treatment costs, but has marginal side effects. The aim of this study was to investigate whether it is possible to decrease the dose of erlotinib when it is co-administered with ritonavir.
Methods
Study Design and Patients
This cross-over, phase I, open-label, pharmacokinetic trial was designed to compare the pharmacokinetics of erlotinib 150 mg monotherapy to the pharmacokinetics of erlotinib 75 mg in combination with ritonavir 200 mg. This study was approved by the medical ethical committee (The Netherlands Cancer Institute, Amsterdam) and performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participating patients. This trial was registered in the Netherlands Trial Register (identifier: NL7542).
All patients ≥18 years old were eligible for study participation, provided that they were currently treated with or planned for treatment with erlotinib in a dosing schedule of 150 mg QD. Patients treated simultaneously with co-medication, which could influence the pharmacokinetics of erlotinib, were excluded. Additional exclusion criteria were: active uncontrolled infections, severe cardiac dysfunction in the past six months prior to treatment, impairment of the hepatic function and pregnancy or breast feeding women. Smoking has been attributed to an increased activity of CYP1A isoforms and thus might have an effect on part of the metabolism of erlotinib (14). Therefore, current smokers (within one week from start) were also excluded from this study.
In Fig. 1 the schematic overview of the trial is provided. Since the elimination half-life of erlotinib is approximately 36 h (5), steady-state erlotinib concentrations were assumed to be reached after 7.5 days. Therefore, all patients were treated with single agent erlotinib 150 mg QD for at least eight days, after which pharmacokinetic exposure was determined (day 1). Subsequently, patients were treated for one week with single agent erlotinib 75 mg QD, followed by the concomitant treatment of erlotinib 75 mg QD with ritonavir 200 mg QD for one additional week. Afterwards, pharmacokinetic exposure was once again determined (day 15). After trial termination, patients continued with erlotinib 150 mg QD monotherapy.
Pharmacokinetic Sampling and Bioanalysis
Pharmacokinetic samples were drawn on day 1 (steady-state of single agent erlotinib 150 mg QD) and day 15 (steady-state erlotinib 75 mg QD plus ritonavir 200 mg QD). During these days, patients were admitted to the hospital and blood samples were drawn. Blood samples were collected on the following time points respective to the erlotinib intake: Pre-dose and 30 min, 1 h, 2 h, 3 h, 4 h, 5 h, 6 h, 8 h and 24 h after intake. Blood samples were drawn in K2-EDTA tubes, centrifuged for 1500 x g for 10 min at 4°C. Subsequently, plasma was collected and stored at −20°C until bioanalysis. Erlotinib and ritonavir concentrations were determined using a previously validated bioanalytical method with a detection range of 20 – 10,000 ng/mL for erlotinib and 2.0 - 2000 ng/mL for ritonavir (15, 16). The metabolites of erlotinib, OSI-413 and OSI-420, were separated and measured as described previously, with a lower limit of quantification of 2.0 ng/mL and 0.465 ng/mL, respectively (17).
Objectives
The primary aim of this study was to investigate the effect of ritonavir on the pharmacokinetics of erlotinib, measured as AUC over 24 h (AUC0-24h), Cmax and trough concentration (Cmin). Secondary objectives included the incidence and severity of adverse events in therapy with and without ritonavir and the effect of ritonavir on the pharmacokinetics of OSI-413 and OSI-420.
Safety
All adverse events were recorded from start of the study until 21 days after the first pharmacokinetic assessment. The incidence, severity and start of the adverse events were collected and graded according to CTCAE version 5.0. Changes in co-medication were recorded during the study.
Sample Size Calculation and Statistical Analysis
The current study was declared successful when the lower boundary of the one-side 95% confidence interval (CI) of the ratio between the geometric mean in AUC0-24h of erlotinib with and without ritonavir exceeded 0.5, where 0.5 indicates no effect of ritonavir on the pharmacokinetics of erlotinib given that the dose in combination with ritonavir was reduced to 50%. For the calculation of the sample size, we assumed that the concomitant intake with ritonavir would result in 64% increase in erlotinib exposure, similar to the results of ketoconazole on the erlotinib exposure (8). In that same study, an intraindividual variability between two erlotinib administrations was found to be approximately 57%. Using these factors, a simulation involving 20,000 trials, showed that 10 patients had to be included in order to obtain a power of 89.5% (with a one-sided α of 0.05). Overall, slow inclusion of patients was encountered, partly due to a halted accrual during the COVID-19 pandemic. Therefore, an interim analysis was performed in October 2021 after inclusion of nine evaluable patients. Assessment of a worst-case scenario for a potentially tenth patient was assessed on the primary endpoint. In this worst-case scenario, it was assumed that in this patient, ritonavir did not affect the pharmacokinetics of erlotinib and thus the ratio between the exposure of erlotinib with and without ritonavir would be equal to 0.5.
Pharmacokinetic parameters were calculated using a non-compartmental analysis. The linear-log trapezoidal method was used to calculate the AUC0-24h. Cmax was defined as the highest measured concentration over 24 h and Cmin was calculated as the average concentration of pre-dose and 24 h after erlotinib intake. The statistical analyses and power calculation were performed using R version 4.1.1 (R-project, Vienna, Austria). When appropriate, paired t-tests or Wilcoxon signed rank tests were used to determine p values, a p value <0.05 was considered to be statistical significant.
Results
Between August 2019 and September 2021, a total of 13 patients were included in this study. In four of the participants the second pharmacokinetic sampling was not performed due to disease progression (n = 2), need for interacting co-medication during the study (n = 1) or discontinuation due to adverse events (grade 2 rash, n = 1), resulting in a total of nine evaluable patients. In Table I the demographic characteristics at baseline of these patients are depicted.
Pharmacokinetics
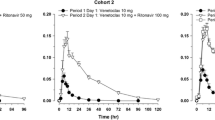
The pharmacokinetic exposure of erlotinib, OSI-413, OSI-420 and ritonavir during erlotinib monotherapy and during erlotinib in combination with ritonavir, are depicted in Table II and Fig. 2. Exposure to erlotinib in terms of AUC0-24h, Cmax and Cmin was not statistically significant different between both groups with ratios of the geometric mean of 0.99 (95% CI: 0.58 – 1.69, p = 0.545), 0.91 (95% CI: 0.55-1.49, p = 0.500) and 1.06 (95% CI: 0.59-1.93, p = 0.150), respectively. The interim analysis after inclusion of nine patients, showed that in a worst-case scenario the ratio of the geometric mean of erlotinib exposure would be 0.92 (0.56-1.51, p = 0.420) still meeting the objective of this study. Therefore, the study was closed after inclusion of nine patients.
Following the combination of erlotinib and ritonavir, a statistically significant decrease in AUC0-24h and Cmax of OSI-413 and OSI-420 and a statistically significant decrease in Cmin of OSI-420 was observed. Coefficients of variability (CV%) of the exposure parameters for erlotinib, its metabolites and ritonavir ranged between 58%-162% for erlotinib alone and 86-443% for erlotinib plus ritonavir. In Table III, the individual change in erlotinib AUC between the control and intervention arm is shown.
Safety
In Table IV, the number of patients experiencing adverse events during treatment with erlotinib alone or during treatment with erlotinib and ritonavir are shown. Overall, only grade 1 or 2 diarrhea, skin rash and/or nausea were noticed, none of the patients experienced a grade 3 or higher adverse event. In four patients (44%), monotherapy erlotinib resulted in a treatment-related adverse event. In two of these patients, their skin rash resolved following the combination of erlotinib with ritonavir. However, three other patients developed adverse events during combination therapy, resulting in five patients (56%) experiencing treatment-related adverse events.
Discussion
In this proof-of-concept study, we investigated if lower doses of erlotinib could be administered when combined with the potent CYP3A4 inhibitor ritonavir. We found that concomitant intake of 75 mg of erlotinib with 200 mg ritonavir resulted in similar steady-state erlotinib exposure in terms of AUC0-24h, Cmax and Cmin as with monotherapy of 150 mg of erlotinib, supporting the concept of halving the dose of erlotinib when concomitantly administrated with a strong CYP3A4 inhibitor. In the treatment of human immunodeficiency virus, pharmacokinetic-boosting with ritonavir has already been shown safe and effective (13, 18). In this study, we showed that ritonavir boosting is also feasible during erlotinib therapy and, therefore, might be implemented for other KIs as well.
KIs are notorious for their high pharmacokinetic inter- and intrapatient variability, often showing values up to 80% (19). Since ritonavir is expected to increase the bioavailability of erlotinib by decreasing the first pass effect due to inhibition of intestinal and liver CYP3A4 activity, the variability on the pharmacokinetic exposure of erlotinib was expected to decrease following the erlotinib plus ritonavir treatment. Nonetheless, in this study high CV% were observed for erlotinib, its metabolites and ritonavir for both dosing strategies. Moreover, there seemed to be a trend in which higher CV% were found in the exposure parameters after the combination therapy when compared to erlotinib alone. Several factors, including food intake and pharmacogenetics (via CYP3A4*22 allele variants) have been found to influence the variability in exposure of erlotinib (20, 21). However, in our study, patients were kept fasted, conform drug label (5) and in addition, the CYP3A4*22 allele variant is associated with a minor (approximately 12%) decrease in functional hepatic CYP3A4 (22). Therefore, we advocate that these factors will only have a limited influence on the observed high interpatient variability. In our study, either one tablet of 150 mg erlotinib or three tablets of 25 mg erlotinib were administered. Since erlotinib is hydrophobic compound (23) and the ratio of excipients-to-drug vary in dose strengths, variability might arise from the differences in dissolution caused by number and formulation of tablets ingested. Nonetheless, a bioequivalence study in healthy volunteers has shown no differences in the values of exposure parameters of erlotinib between different dose strength formulations (24). Lastly, it has been reported that CYP1A2 expression is subject to high interindividual variability (25). In the presence of ritonavir, the metabolism of erlotinib is mainly taken over by CYP1A2. This might explain the increase in interindividual variability in erlotinib exposure found after the combination therapy with ritonavir compared to the monotherapy with erlotinib. Since we only included a limited number of patients, conclusions regarding the origin of this variability are difficult to be drawn.
Theoretically, the inhibition of P-glycoprotein (P-gp) by ritonavir might influence the pharmacokinetics of the P-gp-substrate erlotinib as well (5, 26). In rodents, no alternation of the systemic exposure of erlotinib has been observed and the effect was limited to an increase in the penetration of the blood-brain-barrier (27, 28). Therefore, we expect the effect of P-gp inhibition by ritonavir in humans on the exposure of erlotinib to be minimal.
Regarding the metabolites of erlotinib, the AUC0-24h of OSI-413 and OSI-420 were both statistically significant decreased following the combination therapy with ritonavir. Since these metabolites are the main product of the enzymatic conversion of erlotinib via CYP3A4, it was to be expected that the exposure to these metabolites was lower. However, one needs to assure that lower exposure to these metabolites does not influence the efficacy of therapy. Due to the low abundance of OSI-413 and OSI-420, it has been reported that their contribution to the antitumor activity is very limited in comparison with parent erlotinib (5, 29). Therefore, the decreased exposure of these metabolites following the combination therapy with ritonavir is most likely not clinically relevant.
The majority of the currently approved KIs are metabolized via CYP3A4 (30). The exposure of many of these drugs has been shown to be substantially influenced by concomitant intake with highly potent CYP3A4 inhibitors (4). Consequently, the concomitant intake with ritonavir is often advised to be avoided. However, the increase in drug exposure can also be used in favor of precision dosing. While target therapies are becoming more expensive and already cover large parts of health care budgets (2), strategies to reduce these costs need to be implemented to ensure affordable health care systems. Decreasing the dose or dose frequencies might be one way for cost saving. The concomitant intake of KIs with ritonavir can therefore be helpful to decrease the costs in healthcare but maintain the therapeutic exposure of these drugs. The therapeutic potential of ritonavir might not only be limited to pharmacokinetic boosting of the systemic exposure of drugs. It has been reported that enhanced intratumoral drug metabolism by an increased expression of CYP3A4 could play an important role in the development of drug resistance (31). Administration of CYP3A4 inhibitors have been found to decrease the intratumoral metabolism of drugs with a CYP3A4-dependent metabolism (32, 33). Additional research should investigate this promising strategy to overcome resistance mechanisms or inadequate intratumoral drug exposure.
In conclusion, this study shows that the pharmacokinetic exposure at a dose of 75 mg QD erlotinib, when combined with 200 mg QD ritonavir, is similar to 150 mg QD erlotinib. A substantial decrease in the costs of therapy is expected with this ritonavir-boosting strategy. Based on these results, boosting with strong CYP3A4 inhibitor like ritonavir seems a promising dosing strategy for other CYP3A4 metabolically-dependent KIs to reduce their financial footprint on the health care budget.
References
Faehling M, Schwenk B, Kramberg S, Eckert R, Volckmar A-L, Stenzinger A, et al. Oncogenic driver mutations, treatment, and EGFR-TKI resistance in a Caucasian population with non-small cell lung cancer: survival in clinical practice. Oncotarget. 2017;8(44):77897–914. https://doi.org/10.18632/oncotarget.20857.
Shih YC, Smieliauskas F, Geynisman DM, Kelly RJ, Smith TJ. Trends in the cost and use of targeted Cancer therapies for the privately insured nonelderly: 2001 to 2011. J Clin Oncol. 2015;33(19):2190–6. https://doi.org/10.1200/jco.2014.58.2320.
Verheijen RB, Yu H, Schellens JHM, Beijnen JH, Steeghs N, Huitema ADR. Practical recommendations for therapeutic drug monitoring of kinase inhibitors in oncology. Clin Pharmacol Ther. 2017;102(5):765–76. https://doi.org/10.1002/cpt.787.
Teo YL, Ho HK, Chan A. Metabolism-related pharmacokinetic drug-drug interactions with tyrosine kinase inhibitors: current understanding, challenges and recommendations. Br J Clin Pharmacol. 2015;79(2):241–53. https://doi.org/10.1111/bcp.12496.
European medicines agency. Tarceva: EPAR-Product information 2019.
Townsley CA, Major P, Siu LL, Dancey J, Chen E, Pond GR, et al. Phase II study of erlotinib (OSI-774) in patients with metastatic colorectal cancer. Br J Cancer. 2006;94(8):1136–43. https://doi.org/10.1038/sj.bjc.6603055.
Philip PA, Mahoney MR, Allmer C, Thomas J, Pitot HC, Kim G, et al. Phase II study of erlotinib in patients with advanced biliary cancer. J Clin Oncol. 2006;24(19):3069–74. https://doi.org/10.1200/jco.2005.05.3579.
Rakhit A, Pantze MP, Fettner S, Jones HM, Charoin J-E, Riek M, et al. The effects of CYP3A4 inhibition on erlotinib pharmacokinetics: computer-based simulation (SimCYP™) predicts in vivo metabolic inhibition. Eur J Clin Pharmacol. 2008;64(1):31–41. https://doi.org/10.1007/s00228-007-0396-z.
Ling J, Johnson KA, Miao Z, Rakhit A, Pantze MP, Hamilton M, et al. Metabolism and excretion of erlotinib, a small molecule inhibitor of epidermal growth factor receptor tyrosine kinase, in healthy male volunteers. Drug Metab Dispos. 2006;34(3):420–6. https://doi.org/10.1124/dmd.105.007765.
Boosman RJ, Burgers JA, Smit EF, Steeghs N, van der Wekken AJ, Beijnen JH, et al. Optimized dosing: the next step in precision medicine in non-small-cell lung Cancer. Drugs. 2022;82(1):15–32. https://doi.org/10.1007/s40265-021-01654-3.
Vermunt M, Marchetti S, Beijnen J. Pharmacokinetics and toxicities of Oral docetaxel formulations co-administered with ritonavir in phase I trials. Clin Pharmacol. 2021;13:21–32. https://doi.org/10.2147/cpaa.S292746.
López-Cortés LF, Castaño MA, López-Ruz MA, Rios-Villegas MJ, Hernández-Quero J, Merino D, et al. Effectiveness of ritonavir-boosted protease inhibitor monotherapy in clinical practice even with previous Virological failures to protease inhibitor-based regimens. PLoS One. 2016;11(2):e0148924. https://doi.org/10.1371/journal.pone.0148924.
Hull MW, Montaner JS. Ritonavir-boosted protease inhibitors in HIV therapy. Ann Med. 2011;43(5):375–88. https://doi.org/10.3109/07853890.2011.572905.
Hamilton M, Wolf JL, Rusk J, Beard SE, Clark GM, Witt K, et al. Effects of smoking on the pharmacokinetics of Erlotinib. Clin Cancer Res. 2006;12(7):2166–71. https://doi.org/10.1158/1078-0432.Ccr-05-2235.
Lankheet NA, Hillebrand MJ, Rosing H, Schellens JH, Beijnen JH, Huitema AD. Method development and validation for the quantification of dasatinib, erlotinib, gefitinib, imatinib, lapatinib, nilotinib, sorafenib and sunitinib in human plasma by liquid chromatography coupled with tandem mass spectrometry. Biomed Chromatogr. 2013;27(4):466–76. https://doi.org/10.1002/bmc.2814.
Hendrikx JJ, Hillebrand MJ, Thijssen B, Rosing H, Schinkel AH, Schellens JH, et al. A sensitive combined assay for the quantification of paclitaxel, docetaxel and ritonavir in human plasma using liquid chromatography coupled with tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2011;879(28):2984–90. https://doi.org/10.1016/j.jchromb.2011.08.034.
Rood JJM, Toraño JS, Somovilla VJ, Beijnen JH, Sparidans RW. Bioanalysis of erlotinib, its O-demethylated metabolites OSI-413 and OSI-420, and other metabolites by liquid chromatography-tandem mass spectrometry with additional ion mobility identification. J Chromatogr B. 2021;1166:122554. https://doi.org/10.1016/j.jchromb.2021.122554.
Horberg M, Klein D, Hurley L, Silverberg M, Towner W, Antoniskis D, et al. Efficacy and safety of ritonavir-boosted and unboosted atazanavir among antiretroviral-naïve patients. HIV Clin Trials. 2008;9(6):367–74. https://doi.org/10.1310/hct0906-367.
Groenland SL, Mathijssen RHJ, Beijnen JH, Huitema ADR, Steeghs N. Individualized dosing of oral targeted therapies in oncology is crucial in the era of precision medicine. Eur J Clin Pharmacol. 2019;75(9):1309–18. https://doi.org/10.1007/s00228-019-02704-2.
Ling J, Fettner S, Lum BL, Riek M, Rakhit A. Effect of food on the pharmacokinetics of erlotinib, an orally active epidermal growth factor receptor tyrosine-kinase inhibitor, in healthy individuals. Anti-Cancer Drugs. 2008;19(2):209–16. https://doi.org/10.1097/CAD.0b013e3282f2d8e4.
Mulder TAM, van Eerden RAG, de With M, Elens L, Hesselink DA, Matic M, et al. CYP3A4∗22 genotyping in clinical practice: ready for implementation? Front Genet. 2021;12(1237). https://doi.org/10.3389/fgene.2021.711943.
Wang D, Sadee W. CYP3A4 intronic SNP rs35599367 (CYP3A4*22) alters RNA splicing. Pharmacogenet Genomics. 2016;26(1):40–3. https://doi.org/10.1097/fpc.0000000000000183.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 21743 Review – Erlotinib 2015.
Frohna P, Lu J, Eppler S, Hamilton M, Wolf J, Rakhit A, et al. Evaluation of the absolute oral bioavailability and bioequivalence of erlotinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in a randomized, crossover study in healthy subjects. J Clin Pharmacol. 2006;46(3):282–90. https://doi.org/10.1177/0091270005284193.
Haraya K, Kato M, Chiba K, Sugiyama Y. Prediction of inter-individual variability on the pharmacokinetics of CYP1A2 substrates in non-smoking healthy volunteers. Drug Metab Pharmacokinet. 2016;31(4):276–84. https://doi.org/10.1016/j.dmpk.2016.03.003.
Kageyama M, Namiki H, Fukushima H, Terasaka S, Togawa T, Tanaka A, et al. Effect of chronic administration of ritonavir on function of cytochrome P450 3A and P-glycoprotein in rats. Biol Pharm Bull. 2005;28(1):130–7. https://doi.org/10.1248/bpb.28.130.
van Tellingen O, Marchetti S, de Vries N, Zhao J, Buckle T, Beijnen J, et al. The impact of the ABC transporters P-gp and BCRP on the oral bioavailability and brain penetration of erlotinib using drug transporter knockout mouse models. Cancer Res 2007;67(9 Supplement):LB-373-LB-.
de Vries NA, Buckle T, Zhao J, Beijnen JH, Schellens JH, van Tellingen O. Restricted brain penetration of the tyrosine kinase inhibitor erlotinib due to the drug transporters P-gp and BCRP. Investig New Drugs. 2012;30(2):443–9. https://doi.org/10.1007/s10637-010-9569-1.
European medicines agency. Tarceva: EPAR-Scientific discussion 2005.
Jackson KD, Durandis R, Vergne MJ. Role of cytochrome P450 enzymes in the metabolic activation of tyrosine kinase inhibitors. Int J Mol Sci. 2018;19(8):2367. https://doi.org/10.3390/ijms19082367.
van Eijk M, Boosman RJ, Schinkel AH, Huitema ADR, Beijnen JH. Cytochrome P450 3A4, 3A5, and 2C8 expression in breast, prostate, lung, endometrial, and ovarian tumors: relevance for resistance to taxanes. Cancer Chemother Pharmacol. 2019;84(3):487–99. https://doi.org/10.1007/s00280-019-03905-3.
Hendrikx JJMA, Lagas JS, Song J-Y, Rosing H, Schellens JHM, Beijnen JH, et al. Ritonavir inhibits intratumoral docetaxel metabolism and enhances docetaxel antitumor activity in an immunocompetent mouse breast cancer model. Int J Cancer. 2016;138(3):758–69. https://doi.org/10.1002/ijc.29812.
Lubberman FJE, van Erp NP, Ter Heine R, van Herpen CML. Boosting axitinib exposure with a CYP3A4 inhibitor, making axitinib treatment personal. Acta Oncol. 2017;56(9):1238–40. https://doi.org/10.1080/0284186x.2017.1311024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
R.J. Boosman, C.J. de Gooijer, S.L. Groenland, P. Baas, V. van der Noort and A.D.R. Huitema declare they have no conflict of interest to report.
J.A. Burgers attended advisory boards for Roche and received grants for the institute from MSD.
J.H. Beijnen has received payment for expert testimony for Hoyng Tokh Monegier (paid to their institution), is a part-time employee and (in)direct stockholder of Modra Pharmaceuticals and (jointly) holds a patent on oral taxane formulations, which are clinically developed by Modra Pharmaceuticals. Modra Pharmaceuticals is a small spin-off company of the Netherlands Cancer Institute. All of these conflicts are outside of the submitted work.
N. Steeghs provided consultation or attended advisory boards for Boehringer Ingelheim, Ellipses Pharma. N Steeghs received research grants for the institute from AB Science, Abbvie, Actuate Therapeutics, ADCtherapeutics, Amgen, Array, Ascendis Pharma, Astex, AstraZeneca, Bayer, Blueprint Medicines, Boehringer Ingelheim, BridgeBio, Bristol-Myers Squibb, Cantargia, Celgene, CellCentric, Cresecendo, Cytovation, Deciphera, Eli Lilly, Exelixis, Genentech, Genmab, Gilead, GlaxoSmithKline, Incyte, InteRNA, Janssen/Johnson&Johnson, Kinate, Merck, Merck Sharp & Dohme, Merus, Molecular Partners, Novartis, Numab, Pfizer, Pierre Fabre, Regeneron, Roche, Sanofi, Seattle Genetics, Servier, Taiho, Takeda (outside the submitted work).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boosman, R.J., de Gooijer, C.J., Groenland, S.L. et al. Ritonavir-Boosted Exposure of Kinase Inhibitors: an Open Label, Cross-over Pharmacokinetic Proof-of-Concept Trial with Erlotinib. Pharm Res 39, 669–676 (2022). https://doi.org/10.1007/s11095-022-03244-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03244-8