Abstract
Purpose
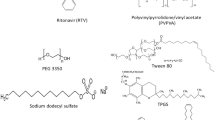
Surfactants are increasingly being added to amorphous solid dispersion (ASDs) formulations to enhance processability and release performance. The goal of the current work was to investigate the impact of cationic, anionic and non-ionic surfactants on the rate and extent of clopidogrel (CPD) release from copovidone-based ASDs.
Methods
CPD release was evaluated for ASDs with different drug loadings using a surface normalized intrinsic dissolution apparatus. Studies were also carried out using dynamic light scattering, zeta potential measurements, and nuclear magnetic resonance spectroscopy to probe the impact of surfactants on drug-rich nanodroplet physical stability and clopidogrel-surfactant interactions.
Results
CPD ASDs showed good release for drug loadings as high as 40%, before the release fell off a cliff at higher drug loadings. Only sodium dodecyl sulfate, added at a 5% level, was able to improve the release at 50% drug loading, with other surfactants proving to be ineffective. However, some of the surfactants evaluated did show some benefits in improving nanodroplet stability against size enlargement. Ionic and non-ionic surfactants were observed to interact differently with CPD-rich nanodroplets, and variations in the kinetics and morphology of water-induced phase separation were noted in the presence and absence of surfactants in ASD films.
Conclusions
In summary, addition of surfactants to ASD formulations may lead to some improvements in formulation performance, but predictive capabilities and mechanisms of surfactant effect still require further studies.
Graphical abstract















Similar content being viewed by others
Abbreviations
- API:
-
Active pharmaceutical ingredient
- ASD:
-
Amorphous solid dispersion
- AUC:
-
Area under the curve
- CMC:
-
Critical micelle concentration
- CPD:
-
Clopidogrel
- CTAB:
-
Cetrimonium bromide
- DLS:
-
Dynamic light scattering
- GLPS:
-
Glass liquid phase separation
- HLB:
-
Hydrophilic lipophilic balance
- HPLC:
-
High performance liquid chromatography
- LLPS:
-
Liquid liquid phase separation
- LoC:
-
Limit of Congruency
- NMR:
-
Nuclear magnetic resonance
- NTA:
-
Nanoparticle tracking analysis
- PVPVA:
-
Copovidone
- SDS:
-
Sodium dodecyl sulfate
- T g :
-
Glass transition temperature
- TPGS:
-
D-α-tocopherol polyethylene glycol 1000 succinate
- TWN:
-
Tween 80
- UV:
-
Ultraviolet
References
Amidon GL, Lennernäs H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res: Off J Am Assoc Pharm Sci. 1995;12:413–20.
Taylor LS, Zhang GGZ. Physical chemistry of supersaturated solutions and implications for oral absorption. Adv Drug Deliv Rev. 2016;101:122–42.
Indulkar AS, Gao Y, Raina SA, Zhang GGZ, Taylor LS. Exploiting the phenomenon of liquid-liquid phase separation for enhanced and sustained membrane transport of a poorly water-soluble drug. Mol Pharm. 2016;13:2059–69.
Lu J, et al. Impact of endogenous bile salts on the thermodynamics of supersaturated active pharmaceutical ingredient solutions. Cryst Growth Des. 2017;17:1264–75.
Indulkar AS, et al. Impact of micellar surfactant on supersaturation and insight into Solubilization mechanisms in supersaturated solutions of Atazanavir. Pharm Res. 2017;34:1276–95.
Coan KED, Shoichet BK. Stoichiometry and physical chemistry of promiscuous aggregate-based inhibitors. J Am Chem Soc. 2008;130:9606–12.
Ilevbare GA, Taylor LS. Liquid-liquid phase separation in highly supersaturated aqueous solutions of poorly water-soluble drugs: implications for solubility enhancing formulations. Cryst Growth Des. 2013. https://doi.org/10.1021/cg301679h.
Paus R, Ji Y, Vahle L, Sadowski G. Predicting the solubility advantage of amorphous pharmaceuticals: A novel thermodynamic approach. Mol Pharm. 2015;12:2823–33.
Mosquera-Giraldo LI, Taylor LS. Glass–liquid phase separation in highly supersaturated aqueous solutions of telaprevir. Mol Pharm. 2015;12:496–503.
Indulkar AS, Box KJ, Taylor R, Ruiz R, Taylor LS. pH-dependent liquid-liquid phase separation of highly supersaturated solutions of weakly basic drugs. Mol Pharm. 2015;12:2365–77.
Kesisoglou F, et al. Effect of amorphous nanoparticle size on bioavailability of Anacetrapib in dogs. J Pharm Sci. 2019;108:2917–25.
Que C, et al. Insights into the dissolution behavior of Ledipasvir-Copovidone amorphous solid dispersions: role of drug loading and intermolecular interactions. Mol Pharm. 2019;16:5054–67.
Saboo S, Kestur US, Flaherty DP, Taylor LS. Congruent release of drug and polymer from amorphous solid dispersions: insights into the role of drug-polymer hydrogen bonding, surface crystallization, and glass transition. Mol Pharm. 2020;17:1261–75.
Ganesh AN, Donders EN, Shoichet BK, Shoichet MS. Colloidal aggregation: from screening nuisance to formulation nuance. Nano Today. 2018;19:188–200.
Raina SA, et al. Impact of solubilizing additives on supersaturation and membrane transport of drugs. Pharm Res. 2015;32:3350–64.
Indulkar AS, Lou X, Zhang GGZ, Taylor LS. Insights into the dissolution mechanism of ritonavir-Copovidone amorphous solid dispersions: importance of congruent release for enhanced performance. Mol Pharm. 2019;16:1327–39.
Auch C, Jede C, Harms M, Wagner C, Mäder K. Impact of amorphization and GI physiology on supersaturation and precipitation of poorly soluble weakly basic drugs using a small-scale in vitro transfer model. Int J Pharm. 2020. https://doi.org/10.1016/j.ijpharm.2019.118917.
Dressman JB, Reppas C. In vitro-in vivo correlations for lipophilic, poorly water-soluble drugs. Eur J Pharm Sci. 2000. https://doi.org/10.1016/S0928-0987(00)00181-0.
Wilson V, et al. Relationship between amorphous solid dispersion in vivo absorption and in vitro dissolution: phase behavior during dissolution, speciation, and membrane mass transport. J Control Release. 2018;292:172–82.
Harmon P, et al. Mechanism of dissolution-induced nanoparticle formation from a Copovidone-based amorphous solid dispersion. Mol Pharm. 2016;13:1467–81.
Stewart AM, et al. Impact of Drug-Rich Colloids of Itraconazole and HPMCAS on Membrane Flux in Vitro and Oral Bioavailability in Rats. Mol Pharm. 2017. https://doi.org/10.1021/acs.molpharmaceut.7b00338.
Sugano K. Possible reduction of effective thickness of intestinal unstirred water layer by particle drifting effect. Int J Pharm. 2010. https://doi.org/10.1016/j.ijpharm.2009.12.014.
Ilevbare GA, Liu H, Pereira J, Edgar KJ, Taylor LS. Influence of additives on the properties of nanodroplets formed in highly supersaturated aqueous solutions of ritonavir. Mol Pharm. 2013;10:3392–403.
Lindfors L, et al. Amorphous drug nanosuspensions. 2. Experimental determination of bulk monomer concentrations. Langmuir. 2006;22:911–6.
Ueda K, Yamamoto N, Higashi K, Moribe K. Molecular mobility suppression of ibuprofen-rich amorphous Nanodroplets by HPMC revealed by NMR Relaxometry and its significance with respect to crystallization inhibition. Mol Pharm. 2019. https://doi.org/10.1021/acs.molpharmaceut.9b00840.
Urbina-villalba G, Cruz-Barrios E. Influence of creaming and ripening on the aggregation rate of non-ionic Dodecane-in-water Nanoemulsions. Rev del CEIF. 2014;3:22–9.
Sun Y, Deac A, Zhang GGZ. Assessing physical stability of colloidal dispersions using a Turbiscan optical analyzer. Mol Pharm. 2019;16:877–85.
Tadros TF. Applied surfactants: principles and applications: Wiley-VCH Velag GmbH & Co; 2006.
Chen J, Ormes JD, Higgins JD, Taylor LS. Impact of surfactants on the crystallization of aqueous suspensions of celecoxib amorphous solid dispersion spray dried particles. Mol Pharm. 2015;12:533–41.
Jermain SV, Brough C, Williams RO. Amorphous solid dispersions and nanocrystal technologies for poorly water-soluble drug delivery – an update. Int J Pharm. 2018;535:379–92.
Solanki NG, et al. Effects of surfactants on Itraconazole-HPMCAS solid dispersion prepared by hot melt extrusion. I: miscibility and drug release. J Pharm Sci. 2018;1–13. https://doi.org/10.1016/j.xphs.2018.10.058.
Tadros TF. 2. Interfacial aspects of pharmaceutical systems. Interfacial Phenom Colloid Stab. 2015. https://doi.org/10.1515/9783110366471-004.
Merisko-Liversidge E, Liversidge GG, Cooper ER. Nanosizing: A formulation approach for poorly-water-soluble compounds. Eur J Pharm Sci. 2003;18:113–20.
Gershanik T, Benita S. Self-dispersing lipid formulations for improving oral absorption of lipophilic drugs. Eur J Pharm Biopharm. 2000;50:179–88.
Chavda VP, Shah D. Self-emulsifying delivery systems: One step ahead in improving solubility of poorly soluble drugs. Nanostructures for Cancer Therapy: Elsevier Inc; 2017. https://doi.org/10.1016/B978-0-323-46144-3.00025-8.
Mosquera-Giraldo LI, Trasi NS, Taylor LS. Impact of surfactants on the crystal growth of amorphous celecoxib. Int J Pharm. 2014;461:251–7.
Indulkar AS, Gao Y, Raina SA, Zhang GGZ, Taylor LS. Impact of monomeric versus micellar surfactant and surfactant-polymer interactions on nucleation-induction times of Atazanavir from supersaturated solutions. Cryst Growth Des. 2020;20:62–72.
Ananthapadmanabhan KP, Goddard ED, Turro NJ, Kuo PL. Fluorescence probes for critical micelle concentration. Langmuir. 1985;1:352–5.
Bhattacharjee S. DLS and zeta potential - what they are and what they are not? J Control Release. 2016;235:337–51.
Claridge TDW. High-resolution NMR techniques in organic chemistry. Chapter 12: Elsevier; 2016. https://doi.org/10.1016/B978-0-08-099986-9/00012-9.
RStudio Team. Rstudio: integrated development environment for R. (2020).
Purohit HS, Taylor LS. Phase behavior of ritonavir amorphous solid dispersions during hydration and dissolution. Pharm Res. 2017;34:2842–61.
Purohit HS, et al. Insights into Nano- and Micron-scale phase separation in amorphous solid dispersions using fluorescence-based techniques in combination with solid state nuclear magnetic resonance spectroscopy. Pharm Res. 2017;34:1364–77.
Wang L, Gaigalas AK, Reipa V. Optical properties of Alexa™ 488 and cy™5 immobilized on a glass surface. Biotechniques. 2005;38:127–31.
ICI Americas Inc. The HLB System. A time-saving Guid Emuls Sel. 1980;37:1390–3.
Miraglia DB, Rodríguez JL, Minardi RM, Schulz PC. Critical micelle concentration and HLB of the sodium oleate- hexadecyltrimethylammonium bromide mixed system. J Surfactant Deterg. 2011;14:401–8.
Zhang Z, Tan S, Feng SS. Vitamin E TPGS as a molecular biomaterial for drug delivery. Biomaterials. 2012;33:4889–906.
Fuguet E, Ràfols C, Rosés M, Bosch E. Critical micelle concentration of surfactants in aqueous buffered and unbuffered systems. Anal Chim Acta. 2005:95–100. https://doi.org/10.1016/j.aca.2005.05.069.
Chauhan S, Chauhan MS, Kaushal D, Syal VK, Jyoti J. Study of micellar behavior of SDS and CTAB in aqueous media containing furosemide-A cardiovascular drug. J Solut Chem. 2010;39:622–38.
Mahmood M, Al-koofee D. Effect of temperature changes on critical micelle concentration for tween series surfactant. Glob J Sci Front Res Chem. 2013;13:1–7.
Patist A, Bhagwat SS, Penfield KW, Aikens P, Shah DO. On the measurement of critical micelle concentrations of pure and technical-grade nonionic surfactants. J Surfactant Deterg. 2000;3:53–8.
Wan LSC, Lee PFS. CMC of polysorbates. J Pharm Sci. 1974;63:136–7.
Croy SR, Kwon GS. Polysorbate 80 and Cremophor EL micelles Deaggregate and solubilize nystatin at the Core – Corona Interface. J Pharm Sci. 2005;94:2345–54.
Tang X, Huston KJ, Larson RG. Molecular dynamics simulations of structure-property relationships of tween 80 surfactants in water and at interfaces. J Phys Chem B. 2014;118:12907–18.
Amani A, York P, De Waard H, Anwar J. Molecular dynamics simulation of a polysorbate 80 micelle in water. Soft Matter. 2011;7:2900–8.
Sadoqi M, Lau-cam CA, Wu SH. Investigation of the micellar properties of the tocopheryl polyethylene glycol succinate surfactants TPGS 400 and TPGS 1000 by steady state fluorometry. J Colloid Interface Sci. 2009;333:585–9.
Pant D, Levinger NE. Polar solvation dynamics of H2O and D2O at the surface of zirconia nanoparticles. J Phys Chem B. 1999;103:7846–52.
Claridge TDW. High-resolution NMR techniques in organic chemistry. Chapter 2: Elsevier; 2016. https://doi.org/10.1016/B978-0-08-099986-9/00002-6.
Apperley DC, et al. Characterisation of indomethacin and nifedipine using variable-temperature solid-state NMR. Magn Reson Chem. 2005;43:881–92.
Ueda K, Taylor LS. Polymer type impacts amorphous solubility and drug-rich phase colloidal stability: A mechanistic study using nuclear magnetic resonance spectroscopy. Mol Pharm. 2020. https://doi.org/10.1021/acs.molpharmaceut.0c00061.
Ueda K, Higashi K, Moribe K. Direct NMR monitoring of phase separation behavior of highly supersaturated Nifedipine solution stabilized with Hypromellose derivatives. Mol Pharm. 2017;14:2314–22.
Ueda K, Taylor LS. Partitioning of surfactant into drug-rich nanodroplets and its impact on drug thermodynamic activity and droplet size. J Control Release. 2021;330:229–43.
Aguiar J, Carpena P, Molina-Bolívar JA, Carnero Ruiz C. On the determination of the critical micelle concentration by the pyrene 1:3 ratio method. J Colloid Interface Sci. 2003;258:116–22.
Williams RJ, Phillips JN, Mysels KJ. The critical micelle concentration of sodium lauryl sulphate at 25° C. Trans Faraday Soc. 1955;51:728–37.
Furihata K, Zhang J, Koda M, Miyakawa T, Tanokura M. Broadband WET: A novel technique for quantitative characterization of minor components in foods. Magn Reson Chem. 2014;52:333–8.
Adams RW, Holroyd CM, Aguilar JA, Nilsson M, Morris GA. “Perfecting” WATERGATE: clean proton NMR spectra from aqueous solution. Chem Commun. 2013;49:358–60.
Maiwald M, Steinhof O, Sleigh C, Bernstein M, Hasse H. Quantitative high-resolution online NMR spectroscopy in pharmaceutical reaction and process monitoring. NMR Spectrosc Pharm Anal. 2008:471–91. https://doi.org/10.1016/B978-0-444-53173-5.00020-2.
Saboo S, Bapat P, Moseson DE, Kestur US, Taylor LS. Exploring the role of surfactants in enhancing drug release from amorphous solid dispersions at higher drug loadings. Pharmaceutics. 2021;13:1–22.
Han YR, Ma Y, Lee PI. Impact of phase separation morphology on release mechanism of amorphous solid dispersions. Eur J Pharm Sci. 2019;136:104955.
Greenspan P, Fowler SD. Spectrofluorometric studies of the lipid probe, nile red. J Lipid Res. 1985;26:781–9.
Sackett DL, Wolff J. Nile red as a polarity-sensitive fluorescent probe of hydrophobic protein surfaces. Anal Biochem. 1987;167:228–34.
Zanetti-Domingues LC, Tynan CJ, Rolfe DJ, Clarke DT, Martin-Fernandez M. Hydrophobic fluorescent probes introduce artifacts into single molecule tracking experiments due to non-specific binding. PLoS One. 2013;8.
Thermo Fisher. Thermo Fisher Scientific. https://www.thermofisher.com/us/en/home/brands/molecular-probes/key-molecular-probes-products/alexa-fluor/alexa-fluor-frequently-asked-questions.html#chem. Accessed 9 July 2021.
De Aguiar HB, Strader ML, De Beer AGF, Roke S. Surface structure of sodium dodecyl sulfate surfactant and oil at the oil-in-water droplet liquid/liquid interface: A manifestation of a nonequilibrium surface state. J Phys Chem B. 2011;115:2970–8.
Stache H. Anionic surfactants: organic chemistry: Marcel Dekker; 1996.
Magee RW. Evaluation of the external surface area of carbon black by nitrogen adsorption. Rubber Chem Technol. 1994;68:11–4.
Saboo S, Moseson DE, Kestur US, Taylor LS. Patterns of drug release as a function of drug loading from amorphous solid dispersions: A comparison of five different polymers. Eur J Pharm Sci. 2020;155:105514.
Chen Y, et al. Drug-polymer-water interaction and its implication for the dissolution performance of amorphous solid dispersions. Mol Pharm. 2015;12:576–89.
Mosquera-Giraldo LI, et al. Influence of polymer and drug loading on the release profile and membrane transport of telaprevir. Mol Pharm. 2018. https://doi.org/10.1021/acs.molpharmaceut.8b00104.
Indulkar AS, et al. Origin of Nanodroplet formation upon dissolution of an amorphous solid dispersion: A mechanistic isotope scrambling study. J Pharm Sci. 2017;106:1998–2008.
Saboo S, Mugheirbi NA, Zemlyanov DY, Kestur US, Taylor LS. Congruent release of drug and polymer: A “sweet spot” in the dissolution of amorphous solid dispersions. J Control Release. 2019;298:68–82.
Papanu JS, Soane SDS, Bell AT, Hess DW. Transport models for swelling and dissolution of thin polymer films. J Appl Polym Sci. 1989;38:859–85.
Ouano AC, Carothers JA. Dissolution dynamics of some polymers: solvent-polymer boundaries. Polym Eng Sci. 1980;20:160–6.
Yang R, et al. Drug release and Nanodroplet formation from amorphous solid dispersions: insight into the roles of drug physicochemical properties and polymer selection. Mol Pharm. 2021. https://doi.org/10.1021/acs.molpharmaceut.1c00055.
Cooper WJ, Krasicky PD, Rodriguez F. Effects of molecular weight and plasticization on dissolution rates of thin polymer films. Polymer (Guildf). 1985;26:1069–72.
(2020), N. C. for B. I. PubChem Compound Summary for CID 60606, Clopidogrel. Retrieved November 19, 2020. https://pubchem.ncbi.nlm.nih.gov/compound/Clopidogrel. Accessed 19 Nov 2020.
Qi S, et al. Insights into the role of polymer-surfactant complexes in drug solubilisation/stabilisation during drug release from solid dispersions. Pharm Res. 2013;30:290–302.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
Liquid-liquid phase separation in the presence of surfactants, nanodroplet size stabilization by surfactants, 1H solution NMR spectra and analysis, ASD surface normalized dissolution. (DOCX 1683 kb)
ACKNOWLEDGMENTS AND DISCLOSURES
The authors would like to thank Abbvie Inc., for the financial support. The authors declare the following competing financial interest(s): Purdue University and AbbVie jointly participated in study design, research, data collection, analysis and interpretation of data, writing, reviewing, and approving the publication. C.C.S. is a graduate students; L.S.T. is a professor; all are at Purdue University. K.U. was a visiting scholar at Purdue University at the time of the study; They all have no additional conflicts of interest to report. A.S.I., Y.G., and G.G.Z.Z. are employees of AbbVie and may own AbbVie stock.
Rights and permissions
About this article
Cite this article
Correa Soto, C.E., Gao, Y., Indulkar, A.S. et al. Impact of Surfactants on the Performance of Clopidogrel-Copovidone Amorphous Solid Dispersions: Increased Drug Loading and Stabilization of Nanodroplets. Pharm Res 39, 167–188 (2022). https://doi.org/10.1007/s11095-021-03159-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-021-03159-w