Abstract
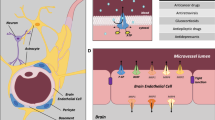
Drug bioavailability to the developing brain is a major concern in the treatment of neonates and infants as well as pregnant and breast-feeding women. Central adverse drug reactions can have dramatic consequences for brain development, leading to major neurological impairment. Factors setting the cerebral bioavailability of drugs include protein-unbound drug concentration in plasma, local cerebral blood flow, permeability across blood-brain interfaces, binding to neural cells, volume of cerebral fluid compartments, and cerebrospinal fluid secretion rate. Most of these factors change during development, which will affect cerebral drug concentrations. Regarding the impact of blood-brain interfaces, the blood-brain barrier located at the cerebral endothelium and the blood-cerebrospinal fluid barrier located at the choroid plexus epithelium both display a tight phenotype early on in embryos. However, the developmental regulation of some multispecific efflux transporters that also limit the entry of numerous drugs into the brain through barrier cells is expected to favor drug penetration in the neonatal brain. Finally, drug cerebral bioavailability is likely to be affected following perinatal injuries that alter blood-brain interface properties. A thorough investigation of these mechanisms is mandatory for a better risk assessment of drug treatments in pregnant or breast-feeding women, and in neonate and pediatric patients.



Similar content being viewed by others
Abbreviations
- ADR:
-
Adverse drug reaction
- BBB:
-
Blood-brain barrier
- BCSFB:
-
Blood-CSF barrier
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
References
Agency EM. Report on the survey of all paediatric uses of medicinal products in Europe. 2010 http://www.ema.europa.eu/docs/en_GB/document_library/Report/2011/01/WC500101006.pdf.
Smyth RM, Gargon E, Kirkham J, Cresswell L, Golder S, Smyth R, et al. Adverse drug reactions in children--a systematic review. PLoS One. 2012;7(3):e24061.
Bellis JR, Kirkham JJ, Thiesen S, Conroy EJ, Bracken LE, Mannix HL, et al. Adverse drug reactions and off-label and unlicensed medicines in children: a nested case-control study of inpatients in a pediatric hospital. BMC Med. 2013;11:238.
Agency EM. Evidence of harm from off-label or unlicensed medicines in children. 2004 http://www.ema.europa.eu/docs/en_GB/document_library/Other/2009/10/WC500004021.pdf.
Elzagallaai AA, Greff M, Rieder MJ. Adverse drug reactions in children: the double-edged sword of therapeutics. Clin Pharmacol Ther. 2017;101(6):725–35.
Cliff-Eribo KO, Sammons H, Choonara I. Systematic review of paediatric studies of adverse drug reactions from pharmacovigilance databases. Expert Opin Drug Saf. 2016;15(10):1321–8.
Andropoulos DB. Effect of anesthesia on the developing brain: infant and fetus. Fetal Diagn Ther. 2018;43(1):1–11.
Jain KK. Drug-induced neurological disorders. Hogrefe Publishing; 2011.
Hanke U, May K, Rozehnal V, Nagel S, Siegmund W, Weitschies W. Commonly used nonionic surfactants interact differently with the human efflux transporters ABCB1 (p-glycoprotein) and ABCC2 (MRP2). Eur J Pharm Biopharm. 2010;76(2):260–8.
Agency EM. Reflection paper on extrapolation of efficacy and safety in 4 paediatric medicine development. 2016 http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2016/04/WC500204187.pdf.
Administration UFad. Pediatric Science and Research Activities. https://www.fda.gov/ScienceResearch/SpecialTopics/PediatricTherapeuticsResearch/ucm106614.htm.
Agency EM. Needs for paediatric medicines. http://www.ema.europa.eu/ema/indexjsp?curl=pages/regulation/document_listing/document_listing_000096jsp&mid=WC0b01ac0580925b1e.
Ward RM, Benjamin DK, Jr., Davis JM, Gorman RL, Kauffman R, Kearns GL, et al. The need for pediatric drug development. J Pediatr 2017.
Rai A, Bhalla S, Rebello SS, Kastrissios H, Gulati A. Disposition of morphine in plasma and cerebrospinal fluid varies during neonatal development in pigs. J Pharm Pharmacol. 2005;57(8):981–6.
Hausler M, Schafer C, Osterwinter C, Jahnen-Dechent W. The physiologic development of fetuin-a serum concentrations in children. Pediatr Res. 2009;66(6):660–4.
Ehrnebo M, Agurell S, Jalling B, Boreus LO. Age differences in drug binding by plasma proteins: studies on human foetuses, neonates and adults. Eur J Clin Pharmacol. 1971;3(4):189–93.
Sammons HM, Choonara I. Learning lessons from adverse drug reactions in children. Children (Basel). 2016;3(1):1.
Thyagarajan B, Deshpande SS. Cotrimoxazole and neonatal kernicterus: a review. Drug Chem Toxicol. 2014;37(2):121–9.
Strazielle N, Ghersi-Egea JF. Physiology of blood-brain interfaces in relation to brain disposition of small compounds and macromolecules. Mol Pharm. 2013;10(5):1473–91.
Workman AD, Charvet CJ, Clancy B, Darlington RB, Finlay BL. Modeling transformations of neurodevelopmental sequences across mammalian species. J Neurosci. 2013;33(17):7368–83.
Fenstermacher JD. The pharmacology of the blood-brain barrier. In: Neuwelt E, editor. Implications of the blood-brain barrier and its manipulation. New York: Plenum; 1989. p. 137–55.
Westerhout J, Danhof M, De Lange EC. Preclinical prediction of human brain target site concentrations: considerations in extrapolating to the clinical setting. J Pharm Sci. 2011;100(9):3577–93.
Nehlig A, Pereira de Vasconcelos A, Boyet S. Postnatal changes in local cerebral blood flow measured by the quantitative autoradiographic [14C]iodoantipyrine technique in freely moving rats. J Cereb Blood Flow Metab. 1989;9(5):579–88.
Wei L, Otsuka T, Acuff V, Bereczki D, Pettigrew K, Patlak C, et al. The velocities of red cell and plasma flows through parenchymal microvessels of rat brain are decreased by pentobarbital. J Cereb Blood Flow Metab. 1993;13(3):487–97.
Strazielle N, Ghersi-Egea JF. Choroid plexus in the central nervous system: biology and physiopathology. J Neuropathol Exp Neurol. 2000;59(7):561–74.
Caley DW, Maxwell DS. Development of the blood vessels and extracellular spaces during postnatal maturation of rat cerebral cortex. J Comp Neurol. 1970;138(1):31–47.
Dziegielewska KM, Ek J, Habgood MD, Saunders NR. Development of the choroid plexus. Microsc Res Tech. 2001;52(1):5–20.
Szmydynger-Chodobska J, Chodobski A, Johanson CE. Postnatal developmental changes in blood flow to choroid plexuses and cerebral cortex of the rat. Am J Phys. 1994;266(5 Pt 2):R1488–92.
Hammarlund-Udenaes M, Friden M, Syvanen S, Gupta A. On the rate and extent of drug delivery to the brain. Pharm Res. 2008;25(8):1737–50.
Daneman R, Zhou L, Kebede AA, Barres BA. Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature. 2010;468(7323):562–6.
Lehmenkuhler A, Sykova E, Svoboda J, Zilles K, Nicholson C. Extracellular space parameters in the rat neocortex and subcortical white matter during postnatal development determined by diffusion analysis. Neuroscience. 1993;55(2):339–51.
Yang S, Wang Y, Li K, Tang X, Zhang K, Shi C, et al. Extracellular space diffusion analysis in the infant and adult rat striatum using magnetic resonance imaging. Int J Dev Neurosci. 2016;53:1–7.
Ghersi-Egea JF, Finnegan W, Chen JL, Fenstermacher JD. Rapid distribution of intraventricularly administered sucrose into cerebrospinal fluid cisterns via subarachnoid velae in rat. Neuroscience. 1996;75(4):1271–88.
Knopf PM, Cserr HF, Nolan SC, Wu TY, Harling-Berg CJ. Physiology and immunology of lymphatic drainage of interstitial and cerebrospinal fluid from the brain. Neuropathol Appl Neurobiol. 1995;21(3):175–80.
Ghersi-Egea JF, Babikian A, Blondel S, Strazielle N. Changes in the cerebrospinal fluid circulatory system of the developing rat: quantitative volumetric analysis and effect on blood-CSF permeability interpretation. Fluids Barriers CNS. 2015;12:8.
Bass NH, Lundborg P. Postnatal development of bulk flow in the cerebrospinal fluid system of the albino rat: clearance of carboxyl-( 14 C)inulin after intrathecal infusion. Brain Res. 1973;52:323–32.
Jones HC, Deane R, Bucknall RM. Developmental changes in cerebrospinal fluid pressure and resistance to absorption in rats. Dev Brain Res. 1987;33(1):23–30.
Johanson CE, Duncan JA 3rd, Klinge PM, Brinker T, Stopa EG, Silverberg GD. Multiplicity of cerebrospinal fluid functions: new challenges in health and disease. Cerebrospinal Fluid Res. 2008;5:10.
Dziegielewska KM, Evans CA, Malinowska DH, Mollgard K, Reynolds JM, Reynolds ML, et al. Studies of the development of brain barrier systems to lipid insoluble molecules in fetal sheep. J Physiol. 1979;292:207–31.
Saunders NR, Knott GW, Dziegielewska KM. Barriers in the immature brain. Cell Mol Neurobiol. 2000;20(1):29–40.
Dickens D, Webb SD, Antonyuk S, Giannoudis A, Owen A, Radisch S, et al. Transport of gabapentin by LAT1 (SLC7A5). Biochem Pharmacol. 2013;85(11):1672–83.
Lee NY, Choi HO, Kang YS. The acetylcholinesterase inhibitors competitively inhibited an acetyl L-carnitine transport through the blood-brain barrier. Neurochem Res. 2012;37(7):1499–507.
Vlieghe P, Khrestchatisky M. Medicinal chemistry based approaches and nanotechnology-based systems to improve CNS drug targeting and delivery. Med Res Rev. 2013;33(3):457–516.
Goasdoue K, Miller SM, Colditz PB, Bjorkman ST. Review: the blood-brain barrier; protecting the developing fetal brain. Placenta. 2017;54:111–6.
Strazielle N, Khuth ST, Ghersi-Egea JF. Detoxification systems, passive and specific transport for drugs at the blood-CSF barrier in normal and pathological situations. Adv Drug Deliv Rev. 2004;56(12):1717–40.
Schlachetzki F, Zhu C, Pardridge WM. Expression of the neonatal Fc receptor (FcRn) at the blood-brain barrier. J Neurochem. 2002;81(1):203–6.
Mollgard K, Dziegielewska KM, Holst CB, Habgood MD, Saunders NR. Brain barriers and functional interfaces with sequential appearance of ABC efflux transporters during human development. Sci Rep. 2017;7(1):11603.
Kratzer I, Vasiljevic A, Rey C, Fevre-Montange M, Saunders N, Strazielle N, et al. Complexity and developmental changes in the expression pattern of claudins at the blood-CSF barrier. Histochem Cell Biol. 2012;138(6):861–79.
Liddelow SA, Dziegielewska KM, Ek CJ, Habgood MD, Bauer H, Bauer HC, et al. Mechanisms that determine the internal environment of the developing brain: a transcriptomic, functional and ultrastructural approach. PLoS One. 2013;8(7):e65629.
Ek CJ, Dziegielewska KM, Stolp H, Saunders NR. Functional effectiveness of the blood-brain barrier to small water-soluble molecules in developing and adult opossum (Monodelphis domestica). J Comp Neurol. 2006;496(1):13–26.
Armulik A, Genove G, Mae M, Nisancioglu MH, Wallgard E, Niaudet C, et al. Pericytes regulate the blood-brain barrier. Nature. 2010;468(7323):557–61.
Conrad MS, Johnson RW. The domestic piglet: an important model for investigating the neurodevelopmental consequences of early life insults. Annu Rev Anim Biosci. 2015;3:245–64.
Stonestreet BS, Burgess GH, Cserr HF. Blood-brain barrier integrity and brain water and electrolytes during hypoxia/hypercapnia and hypotension in newborn piglets. Brain Res. 1992;590(1–2):263–70.
Leino RL, Gerhart DZ, Drewes LR. Monocarboxylate transporter (MCT1) abundance in brains of suckling and adult rats: a quantitative electron microscopic immunogold study. Brain Res Dev Brain Res. 1999;113(1–2):47–54.
Strazielle N, Ghersi-Egea JF. Efflux transporters in blood-brain interfaces of the developing brain. Front Neurosci. 2015;9:21.
Gazzin S, Strazielle N, Schmitt C, Fevre-Montange M, Ostrow JD, Tiribelli C, et al. Differential expression of the multidrug resistance-related proteins ABCb1 and ABCc1 between blood-brain interfaces. J Comp Neurol. 2008;510(5):497–507.
Baello S, Iqbal M, Gibb W, Matthews SG. Astrocyte-mediated regulation of multidrug resistance p-glycoprotein in fetal and neonatal brain endothelial cells: age-dependent effects. Phys Rep. 2016;4(16):e12853.
Saunders NR, Dziegielewska KM, Mollgard K, Habgood MD, Wakefield MJ, Lindsay H, et al. Influx mechanisms in the embryonic and adult rat choroid plexus: a transcriptome study. Front Neurosci. 2015;9:123.
Shawahna R, Uchida Y, Decleves X, Ohtsuki S, Yousif S, Dauchy S, et al. Transcriptomic and quantitative proteomic analysis of transporters and drug metabolizing enzymes in freshly isolated human brain microvessels. Mol Pharm. 2011;8(4):1332–41.
Kratzer I, Liddelow SA, Saunders NR, Dziegielewska KM, Strazielle N, Ghersi-Egea JF. Developmental changes in the transcriptome of the rat choroid plexus in relation to neuroprotection. Fluids Barriers CNS. 2013;10(1):25.
Virgintino D, Robertson D, Benagiano V, Errede M, Bertossi M, Ambrosi G, et al. Immunogold cytochemistry of the blood-brain barrier glucose transporter GLUT1 and endogenous albumin in the developing human brain. Brain Res Dev Brain Res. 2000;123(1):95–101.
Strazielle N, Ghersi-Egea JF. Potential pathways for CNS drug delivery across the blood-cerebrospinal fluid barrier. Curr Pharm Des. 2016;22(35):5463–76.
Moretti R, Pansiot J, Bettati D, Strazielle N, Ghersi-Egea JF, Damante G, et al. Blood-brain barrier dysfunction in disorders of the developing brain. Front Neurosci. 2015;9:40.
Stolp HB, Dziegielewska KM, Ek CJ, Habgood MD, Lane MA, Potter AM, et al. Breakdown of the blood-brain barrier to proteins in white matter of the developing brain following systemic inflammation. Cell Tissue Res. 2005;320(3):369–78.
Hutton LC, Castillo-Melendez M, Walker DW. Uteroplacental inflammation results in blood brain barrier breakdown, increased activated caspase 3 and lipid peroxidation in the late gestation ovine fetal cerebellum. Dev Neurosci. 2007;29(4–5):341–54.
Kratzer I, Chip S, Vexler ZS. Barrier mechanisms in neonatal stroke. Front Neurosci. 2014;8:359.
Muramatsu K, Fukuda A, Togari H, Wada Y, Nishino H. Vulnerability to cerebral hypoxic-ischemic insult in neonatal but not in adult rats is in parallel with disruption of the blood-brain barrier. Stroke. 1997;28(11):2281–8. discussion 8-9
Fernandez-Lopez D, Faustino J, Daneman R, Zhou L, Lee SY, Derugin N, et al. Blood-brain barrier permeability is increased after acute adult stroke but not neonatal stroke in the rat. J Neurosci. 2012;32(28):9588–600.
Gazzin S, Berengeno AL, Strazielle N, Fazzari F, Raseni A, Ostrow JD, et al. Modulation of Mrp1 (ABCc1) and Pgp (ABCb1) by bilirubin at the blood-CSF and blood-brain barriers in the Gunn rat. PLoS One. 2011;6(1):e16165.
Neuhaus W, Schlundt M, Fehrholz M, Ehrke A, Kunzmann S, Liebner S, et al. Multiple antenatal dexamethasone treatment alters brain vessel differentiation in newborn mouse pups. PLoS One. 2015;10(8):e0136221.
Iqbal M, Baello S, Javam M, Audette MC, Gibb W, Matthews SG. Regulation of multidrug resistance P-glycoprotein in the developing blood-brain barrier: interplay between glucocorticoids and cytokines. J Neuroendocrinol. 2016;28(3):12360.
Ghersi-Egea JF, Gazzin S, Strazielle N. Blood-brain interfaces and bilirubin-induced neurological diseases. Curr Pharm Des. 2009;15(25):2893–907.
Acknowledgements and disclosures
This work was funded by ANR-10-IBHU-0003 CESAME grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: Sara Eyal
Rights and permissions
About this article
Cite this article
Ghersi-Egea, JF., Saudrais, E. & Strazielle, N. Barriers to Drug Distribution into the Perinatal and Postnatal Brain. Pharm Res 35, 84 (2018). https://doi.org/10.1007/s11095-018-2375-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2375-8