Abstract
Purpose
A scientifically robust prediction of human dose is important in determining whether to progress a candidate drug into clinical development. A particular challenge for inhaled medicines is that unbound drug concentrations at the pharmacological target site cannot be easily measured or predicted. In the absence of such data, alternative empirical methods can be useful. This work is a post hoc analysis based on preclinical in vivo pharmacokinetic/pharmacodynamic (PK/PD) data with the aim to evaluate such approaches and provide guidance on clinically effective dose prediction for inhaled medicines.
Methods
Five empirically based methodologies were applied on a diverse set of marketed inhaled therapeutics (inhaled corticosteroids and bronchodilators). The approaches include scaling of dose based on body weight or body surface area and variants of PK/PD approaches aiming to predict the therapeutic dose based on having efficacious concentrations of drug in the lung over the dosing interval.
Results
The most robust predictions of dose were made by body weight adjustment (90% within 3-fold) and by a specific PK/PD approach aiming for an average predicted 75% effect level during the dosing interval (80% within 3-fold). Scaling of dose based on body surface area consistently under predicted the therapeutic dose.
Conclusions
Preclinical in vivo data and empirical scaling to man can be used as a baseline method for clinical dose predictions of inhaled medicines. The development of more sophisticated translational models utilizing free drug concentration and target engagement data is a desirable build.


Similar content being viewed by others
Abbreviations
- BID:
-
Twice daily
- BSA-CF:
-
Body surface area conversion factor
- BUD:
-
Budesonide
- Cavg,ED50 :
-
Average lung concentration over the whole challenge period
- CI:
-
Confidence interval
- Clung :
-
Total lung concentration
- COPD:
-
Chronic obstructive pulmonary disease
- DPI:
-
Dry powder inhalation
- DtM:
-
Dose-to-man
- FDA:
-
U S Food and Drug administration
- FF:
-
Fluticasone furoate
- FOR:
-
Formoterol
- FP:
-
Fluticasone propionate
- GP:
-
Glycopyrronium
- HED:
-
Human equivalent dose
- IC50 :
-
Total lung concentration associated with 50% inhibition of challenge induced lung inflammation or bronchoconstriction
- ICS:
-
Inhaled corticosteroids
- Imax :
-
Maximum inhibitory effect of drug on challenge induced lung inflammation or bronchoconstriction
- IND:
-
Indacaterol
- IPRA:
-
Ipratropium
- IT:
-
Intratracheal
- IV:
-
Intravenous
- LABA:
-
Long acting β2 adrenoceptor agonists
- LAMA:
-
Long acting muscarinic antagonists
- LDD:
-
Lung deposited dose
- PD:
-
Pharmacodynamics
- PK:
-
Pharmacokinetics
- PBPK:
-
Physiologically based pharmacokinetic
- PBPK/PD:
-
Physiologically based pharmacokinetic/pharmacodynamic
- PK/PD:
-
Pharmacokinetic/pharmacodynamic
- QD:
-
Once daily
- QID:
-
Four times a day
- SABA:
-
Short acting β2 adrenoceptor agonists
- SALB:
-
Salbutamol
- SALM:
-
Salmeterol
- TID:
-
Three times a day
- TIO:
-
Tiotropium
References
Backman P, Adelmann H, Petersson G, Jones CB. Advances in inhaled technologies: understanding the therapeutic challenge, predicting clinical performance, and designing the optimal inhaled product. Clin Pharmacol Ther. 2014;95(5):509–20.
Cooper AE, Ferguson D, Grime K. Optimisation of DMPK by the inhaled route: challenges and approaches. Curr Drug Metab. 2012;13(4):457–73.
Cook D, Brown D, Alexander R, March R, Morgan P, Satterthwaite G, et al. Lessons learned from the fate of AstraZeneca's drug pipeline: a five-dimensional framework. Nat Rev Drug Discov. 2014;13(6):419–31.
Danhof M, Alvan G, Dahl SG, Kuhlmann J, Paintaud G. Mechanism-based pharmacokinetic-pharmacodynamic modeling-a new classification of biomarkers. Pharm Res. 2005;22(9):1432–7.
Smith DA, Di L, Kerns EH. The effect of plasma protein binding on in vivo efficacy: misconceptions in drug discovery. Nat Rev Drug Discov. 2010;9(12):929–39.
McGinnity DF, Collington J, Austin RP, Riley RJ. Evaluation of human pharmacokinetics, therapeutic dose and exposure predictions using marketed oral drugs. Curr Drug Metab. 2007;8(5):463–79.
Page KM. Validation of early human dose prediction: a key metric for compound progression in drug discovery. Mol Pharm. 2016;13(2):609–20.
Reigner BG, Blesch KS. Estimating the starting dose for entry into humans: principles and practice. Eur J Clin Pharmacol. 2002;57(12):835–45.
Fernandes CA, Vanbever R. Preclinical models for pulmonary drug delivery. Expert Opin Drug Deliv. 2009;6(11):1231–45.
Rohatagi S, Rhodes GR, Chaikin P. Absolute oral versus inhaled bioavailability: significance for inhaled drugs with special reference to inhaled glucocorticoids. J Clin Pharmacol. 1999;39(7):661–3.
Haddad E-B, Underwood SL, Dabrowski D, Birrel MA, McCluskie K, Battram CH, et al. Critical role for T cells in sephadex-induced airway inflammation: pharmacological and immunological characterization and molecular biomarker identification. J Immunol. 2002;168(6):3004–16.
Raab OG, Yeh HC, Newton GJ, Phalen RF, Velasquez DJ. Deposition of inhaled monodisperse aerosols in small rodents. Inhaled Part. 1975;4(Pt 1):3–21.
US Food and Drug Administration. Guidance for industry estimating the maximum safe starting dose in initial clinical trials for therapeutics in adult healthy volunteers. 2005. Access December 2016. Available from: http://www.fda.gov/downloads/Drugs/.../Guidances/UCM078932.pdf.
Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. J R Stat Soc Ser D (The Statistician). 1983;32:307–17.
Villetti G, Bergamaschi M, Bassani F, Bolzoni PT, Harrison S, Gigli PM, et al. Pharmacological assessment of the duration of action of glycopyrrolate vs tiotropium and ipratropium in guinea-pig and human airways. Br J Pharmacol. 2006;148(3):291–8.
Molimard M, Naline E, Zhang Y, Le Gros V, Begaud B, Advenier C. Long- and short-acting beta2 adrenoceptor agonists: interactions in human contracted bronchi. Eur Respir J. 1998;11(3):583–8.
Stocks MJ, Alcaraz L, Bailey A, Bonnert R, Cadogan E, Christie J, et al. Discovery of AZD3199, an inhaled ultralong acting beta2 receptor agonist with rapid onset of action. ACS Med Chem Lett. 2014;5(4):416–21.
Stoeck M, Riedel R, Hochhaus G, Hafner D, Masso JM, Schmidt B, et al. In vitro and in vivo anti-inflammatory activity of the new glucocorticoid ciclesonide. J Pharmacol Exp Ther. 2004;309(1):249–58.
Rohrschneider M, Bhagwat S, Krampe R, Michler V, Breitkreutz J, Hochhaus G. Evaluation of the transwell system for characterization of dissolution behavior of inhalation drugs: effects of membrane and surfactant. Mol Pharm. 2015;12(8):2618–24.
Ramakrishnan R, DuBois DC, Almon RR, Pyszczynski NA, Jusko WJ. Fifth-generation model for corticosteroid pharmacodynamics: application to steady-state receptor down-regulation and enzyme induction patterns during seven-day continuous infusion of methylprednisolone in rats. J Pharmacokinet Pharmacodyn. 2002;29(1):1–24.
Clewell HJ, Reddy MB, Lave T, Andersen ME. Physiologically based pharmacokinetic modelling. In: Gad SC, editor. Pre-clinical development handbook: ADME and biopharmaceutical properties. Hoboken: John Wiley & Sons, Inc.; 2008. p. 1167–227.
Caniga M, Cabal A, Mehta K, Ross DS, Gil MA, Woodhouse JD, et al. Preclinical experimental and mathematical approaches for assessing effective doses of inhaled drugs, using mometasone to support human dose predictions. J Aerosol Med Pulm Drug Deliv. 2016;29(4):362–77.
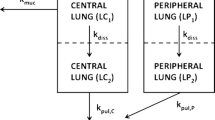
Boger E, Evans N, Chappell M, Lundqvist A, Ewing P, Wigenborg A, et al. Systems pharmacology approach for prediction of pulmonary and systemic pharmacokinetics and receptor occupancy of inhaled drugs. CPT Pharmacometrics Syst Pharmacol. 2016;5(4):201–10.
Mullane K, Williams M. Animal models of asthma: reprise or reboot? Biochem Pharmacol. 2014;87(1):131–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ericsson, T., Fridén, M., Kärrman-Mårdh, C. et al. Benchmarking of Human Dose Prediction for Inhaled Medicines from Preclinical In Vivo Data. Pharm Res 34, 2557–2567 (2017). https://doi.org/10.1007/s11095-017-2218-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2218-z