ABSTRACT
Purpose
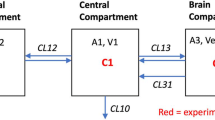
To determine the flow-corrected luminal permeability, Pc, of lipophilic drugs measured by the in situ brain perfusion method under circumstances where the traditional Crone-Renkin equation (CRE) method, using diazepam as a flow marker, often fails.
Methods
The pH-dependent rate of brain penetration of five lipophilic drugs (amitriptyline, atomoxetine, imipramine, indomethacin, maprotiline, sertraline), as well as of atenolol and antipyrine, were measured in Sprague-Dawley rats. A new pH-dependent CRE was derived and applied to remove the hydrodynamic component of effective permeability, Pe, to produce Pc values.
Results
It was shown by the analysis of the in situ data in the pH 6.5–8.5 interval for the lipophilic bases that the average vascular flow Fpf = 0.036 mL∙g−1∙s−1, centered in a “flow-limit window” (FLW) bounded by P mine = 170 and P maxe = 776 (10−6 cm∙s−1 units). It was shown that the traditional CRE is expected not to work for half of the molecules in the FLW and is expected to underestimate (up to 64-fold) the other half of the molecules.
Conclusion
The new pH-CRE flow correction method applied to lipophilic ionizable drugs, based on the pH partition hypothesis, can overcome the limitations of the traditional CRE.





Similar content being viewed by others
Abbreviations
- DRW:
-
dynamic range window for flow-limited drugs, \( {\hbox{DRW }} = { \log }\left( {{{\hbox{F}}_{\rm{pf}}}/{\hbox{S}}} \right){ }--{ \max }\left( {{ \log }{{\hbox{P}}_{\rm{i}}},{ \log }{{\hbox{P}}_{\rm{para}}}} \right) \)
- FLW:
-
flow limit window: \( {\hbox{FLW }} = { \log }\left( {{{\hbox{F}}_{\rm{pf}}}/{\hbox{S}}} \right){ }\pm { 3} \) \( {\hbox{SD }} = { } - {3}.{44 }\pm { }0.{33} \) (SD = standard deviation)
- Fpf :
-
cerebrovascular flow velocity of perfusion fluid (mL·g−1·s−1 brain tissue)
- Kin :
-
unidirectional transfer constant (mL·g−1·s−1): \( {{\hbox{K}}_{\rm{in}}} = { }\left( {{ }{{\hbox{Q}}_{\rm{br}}}/{ }{{\hbox{C}}_{\rm{pf}}}} \right){ }/{\hbox{ T}} \), where Qbr = test compound parenchymal brain concentration (nmol·g−1 brain tissue) (corrected for the vascular volume), Cpf = perfusion fluid concentration (nmol·mL−1), T = perfusion time (s).
- PABL :
-
aqueous boundary layer permeability coefficient (cm·s−1), in vitro or PAMPA model
- Papp :
-
apparent in vitro transcellular permeability coefficient (cm·s−1)
- Pc :
-
corrected-for-flow luminal permeability coefficient (cm·s−1) depends on pH for ionizable permeants (hyperbolic function); basis of the pH partition hypothesis
- Pc S:
-
permeability-surface area product (mL·g−1·s−1), traditionally determined from Kin using Crone-Renkin equation (CRE): \( {{\hbox{P}}_{\rm{c}}}{\hbox{S }} = { } - { }{{\hbox{F}}_{\rm{pf}}}{ \ln }\left( {{1 }--{ }{{\hbox{K}}_{\rm{in}}}/{{\hbox{F}}_{\rm{pf}}}} \right) \)
- Pe :
-
effective permeability coefficient (cm·s−1), not corrected for flow: \( {{\hbox{P}}_{\rm{e}}} = { }{{\hbox{K}}_{\rm{in}}}/{\hbox{ S}} \) depends on pH for ionizable permeants (sigmoidal function)
- pH-CRE:
-
new pH-dependent Crone-Renkin equation (CRE) flow correction method
- Pi :
-
luminal permeability coefficient (cm·s−1) of the ionized form of permeant
- pK fluxa :
-
pH where 50% of the permeation is due to luminal permeability and 50% due to the effective permeability at the hydrodynamic limit
- Pm :
-
PAMPA transmembrane permeability coefficient (cm·s−1), at pH 7.4, corrected for ABL
- Po :
-
intrinsic luminal permeability coefficient (cm·s−1) of the neutral form of permeant for ionizable drugs, \( {{\hbox{P}}_{\rm{o}}} = {{\hbox{P}}_{\rm{c}}}\left( {{1}{0^{\pm ({\rm{pH }} - {\rm{ pKa}})}} + {1}} \right) \), with ‘+’ for acids, ‘-’ for bases
- Ppara :
-
paracellular permeability coefficient (cm·s−1), indicating aqueous diffusion of permeant through the tight junctions formed by the blood-brain barrier
- S:
-
endothelial surface area in a gram of brain tissue (assumed to be 100 cm2∙g−1)
REFERENCES
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Discov. 2010;37:13–25.
Hammarlund-Udenaes M, Fridén M, Syvänen S, Gupta A. On the rate and extent of drug delivery to the brain. Pharm Res. 2008;25:1737–50.
Hitchcock SA. Blood-brain barrier permeability considerations for CNS-targeted compound library design. Curr Opin Chem Biol. 2008;12:1–6.
Jeffrey P, Summerfield SG. Challenges for blood-brain barrier (BBB) screening. Xenobiotica. 2007;37:1135–51.
Takasato Y, Rapoport SI, Smith QR. An in situ brain perfusion technique to study cerebrovascular transport in the rat. Am J Physiol. 1984;247:H484–93.
Smith QR. A review of blood-brain barrier transport techniques. Methods Mol Med. 2003;89:193–208.
Parepally JMR, Mandula H, Smith QR. Brain uptake of nonsteroidal anti-inflammatory drugs: ibuprofen, flurbiprofen, and indomethacin. Pharm Res. 2006;23:873–81.
Renkin EM. Capillary permeability to lipid-soluble molecule. Am J Physiol. 1952;168:538–45.
Crone C. The permeability of capillaries in various organs as determined by use of the “indicator diffusion” method. Acta Physiol Scand. 1963;58:292–305.
Crone C, Levitt DG. Capillary permeability to small solutes. In: Renkin EM, Michel CC, editors. Handbook of Physiology, Sec. 2: The Cardiovascular System. Bethesda: Amer. Physiol. Soc; 1984. p. 411–66.
Summerfield SG, Read K, Begley DJ, Obradovic T, Hidalgo IJ, Coggon S, et al. Central nervous system drug disposition: the relationship between in situ brain permeability and brain free fraction. J Pharmacol Exp Ther. 2007;322:205–13.
Dagenais C, Avdeef A, Tsinman O, Dudley A, Beliveau R. P-Glycoprotein deficient mouse in situ blood-brain barrier permeability and its prediction using an in combo PAMPA model. Eur J Pharm Sci. 2009;38:121–37.
Obradovic T, Dobson GG, Shingaki T, Kungu T, Hidalgo IJ. Assessment of the first and second generation antihistamines brain penetration and the role of P-glycoprotein. Pharm Res. 2007;24:318–27.
Zhao R, Kalvass JC, Pollack GM. Assessment of blood-brain barrier permeability using the in situ mouse brain perfusion technique. Pharm Res. 2009. doi:10.1007/S1105-009-9876-4. in press.
Avdeef A, Artursson P, Neuhoff S, Lazorova L, Gråsjö J, Tavelin S. Caco-2 permeability of weakly basic drugs predicted with the Double-Sink PAMPA pK fluxa method. Eur J Pharm Sci. 2005;24:333–49.
Sugano K, Kansy M, Artursson P, Avdeef A, Bendels S, Di L, et al. Coexistence of passive and active carrier-mediated uptake processes in drug transport: a more balanced view. Nature Rev Drug Discov. 2010;9:597–614.
Evans CAN, Reynolds JM, Reynolds ME, Saunders NR. The effect of hypercapnia on a blood-brain barrier mechanism in foetal and new-born sheep. J Physiol. 1976;255:701–14.
Nagy Z, Szabo M, Huttner I. Blood-brain barrier impairment by low pH buffer perfusion via the internal carotid artery in rat. Acta Neuropathol. 1985;68:160–3.
Greenwood J, Hazell AS, Luthert PJ. The effect of a low pH saline perfusate upon the integrity of the enery-depleted rat blood-brain barrier. J Cereb Blood Flow Metab. 1989;9:234–42.
Okura T, Hattori A, Takano Y, Sato T, Hammarlund-Udanenaes M, Terasaki T, et al. Involvement of the pyrilamine transporter, a putative organic cation transporter, in blood-brain barrier transport of oxycodone. Drug Metab Dispos. 2008;36:2005–13.
Avdeef A, Bucher JJ. Accurate measurements of the concentration of hydrogen ions with a glass electrode: calibrations using the Prideaux and other universal buffer solutions and a computer-controlled automatic titrator. Anal Chem. 1978;50:2137–42.
Avdeef A. Absorption and drug development. Hoboken: Wiley-Interscience; 2003.
Street JA, Hemsworth BA, Roach AG, Day MD. Tissue levels of several radio labelled beta-adrenoceptor antagonists after intravenous administration in rats. Arch Int Pharmacodyn Thér. 1979;237:180–90.
Wang Q, Rager JD, Weinstein K, Kardos P, Dobson GL, Li J, et al. Evaluation of teh MDR-MDCK cell line as a permeability screen for the blood-brain barrier. Int J Pharm. 2005;288:349–59.
Smith QR, Ziylan YZ, Robinson PJ, Rappoport SI. Kinetics and distribution volumes for tracers of different sizes in the brain plasma space. Brain Res. 1988;462:1–9.
Abbruscato TJ, Thomas SA, Hruby VJ, Davis TP. Blood-brain barrier permeability and bioavailability of a highly potent and μ-selective opioid receptor antagonist, CTAP: comparison with morphine. J Pharmacol Exp Ther. 1997;280:402–9.
Ohno K, Pettigrew KD, Rapoport SI. Lower limits of cerebrovascular permeability to nonelectrolytes in the conscious rat. Am J Physiol. 1978;235:H299–307.
Avdeef A. Leakiness and size exclusion of paracellular channels in cultured epithelial cell monolayers—interlaboratory comparison. Pharm Res. 2010;27:480–9.
Ruell JA, Tsinman KL, Avdeef A. a drug absorption in vitro model. 5. Unstirred water layer in iso-pH mapping assays and pK fluxa —optimized design (pOD-PAMPA). Eur J Pharm Sci. 2003;20:393–402.
Avdeef A, Nielsen PE, Tsinman O. a drug absorption in vitro model. 11. Matching the in vivo unstirred water layer thickness by individual-well stirring in microtitre plates. Eur J Pharm Sci. 2004;22:365–74.
Avdeef A, Kansy M, Bendels S, Tsinman K. Absorption-excipient-pH classification gradient maps: sparingly-soluble drugs and the pH partition hypothesis. Eur J Pharm Sci. 2008;33:29–41.
Avdeef A, Tsinman O. Miniaturized rotating disk intrinsic dissolution rate measurement: effects of buffer capacity in comparisons to traditional Wood’s apparatus. Pharm Res. 2008;25:2613–27.
Fagerberg JH, Tsinman O, Tsinman K, Sun N, Avdeef A, Bergström CAS. Dissolution Rate and Apparent Solubility of Poorly Soluble Compounds in Biorelevant Dissolution Media. Mol Pharm. 2010, June 24 Epub ahead of print.
Tsinman O, Tsinman K, Sun N, Avdeef A. Physicochemical selectivity of the BBB microenvironment governing passive diffusion—matching with a porcine brain lipid extract artificial membrane permeability model. Pharm Res. 2010, in press.
Murakami H, Takanaga H, Matsuo H, Ohtani H, Sawada Y. Comparison of blood-brain barrier permeability in mice and rats using in situ brain perfusion technique. Am J Physiol Heart Circ Physiol. 2000;279:H1022–9.
Chikhale EG, Burton PS, Borchardt RT. The effect of verapamil on the transport of peptides across the blood-brain barrier in rats: kinetic evidence for an apically polarized efflux mechanism. J Pharmacol Exp Ther. 1995;273:298–303.
Pardridge WM, Triguero D, Yang J, Cancilla PA. Comparison of in vitro and in vivo models of drug transcytosis through the blood-brain barrier. J Pharmacol Exp Ther. 1990;253:884–91.
Liu X, Tu M, Kelley RS, Chen C, Smith BJ. Development of a computational approach to predict blood-brain barrier permeability. Drug Metab Dispos. 2004;32:132–9.
Cisternino S, Rousselle C, Debray M, Scherrmann J-M. In situ transport of vinblastine and selected P-glycoprotein substances: implications for drug-drug interactions at the mouse blood-brain barrier. Pharm Res. 2004;21:1382–9.
ACKNOWLEDGMENTS
We thank Drs. Feng Zhou and Ismael J. Hidalgo of Absorption Systems for their effort in the in situ brain perfusion measurements and for the valuable background discussions. The technical assistance of Oksana Tsinman (pION) is gratefully acknowledged. Part of this work was supported by Grant Number R44MH75211 from the National Institutes of Health (to pION). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
The current article is contribution number 32 in the Drug Absorption In Vitro Model series from pION. Ref. 16 is part 31 in the series.
Rights and permissions
About this article
Cite this article
Avdeef, A., Sun, N. A New In Situ Brain Perfusion Flow Correction Method for Lipophilic Drugs Based on the pH-Dependent Crone-Renkin Equation. Pharm Res 28, 517–530 (2011). https://doi.org/10.1007/s11095-010-0298-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0298-0