Abstract
Purpose
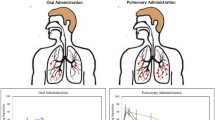
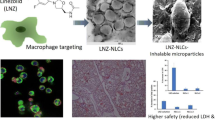
To formulate rifampicin, an anti-tuberculosis antibiotic, for aerosol delivery in a dry powder ‘porous nanoparticle-aggregate particle’ (PNAP) form suited for shelf stability, effective dispersibility and extended release with local lung and systemic drug delivery.
Methods
Rifampicin was encapsulated in PLGA nanoparticles by a solvent evaporation process, spray dried into PNAPs containing varying amounts of nanoparticles, and characterized for physical and aerosol properties. Pharmacokinetic studies were performed with formulations delivered to guinea pigs by intratracheal insufflation and compared to oral and intravenous delivery of rifampicin.
Results
The PNAP formulations possessed properties suitable for efficient deposition in the lungs. In vitro release showed an initial burst of rifampicin, with the remainder available for release beyond eight hours. PNAPs delivered to guinea pigs by insufflation achieved systemic levels of rifampicin detected for six to eight hours. Moreover, rifampicin concentrations remained detectable in lung tissue and cells up to and beyond eight hours. Conversely, after pulmonary delivery of an aerosol without nanoparticles, rifampicin could not be detected in the lungs at eight hours.
Conclusions
Our results indicate that rifampicin can be formulated into an aggregated nanoparticle form that, once delivered to animals, achieves systemic exposure and extends levels of drug in the lungs.






Similar content being viewed by others
Abbreviations
- BAL:
-
Bronchoalveolar lavage
- DCM:
-
Dichloromethane
- FPFTD :
-
Fine particle fraction of the total dose less than 5.8 μm
- NP:
-
Nanoparticles
- PK:
-
Pharmacokinetics
- PLGA:
-
Poly (lactide-co-glycolide)
- PNAP:
-
Porous nanoparticle-aggregate particle
- PNAP40:
-
PNAPs containing 40% NP by weight
- PNAP80:
-
PNAPs containing 80% NP by weight
- PP:
-
Porous particles
- PVA:
-
Poly(vinyl alcohol)
- TB:
-
Tuberculosis
References
WHO. Tuberculosis fact sheet. Geneva: World Health Organization; 2006.
Riley RL, Mills CC, Nyka W, Weinstock N, Storey PB, Sultan LU, et al. Aerial dissemination of pulmonary tuberculosis: a two-year study of contagion in a tuberculosis ward. Am J Epidemiol 1959;70:185–96.
Russell DG. Mycobacterium tuberculosis: here today and here tomorrow. Nat Rev Mol Cell Biol 2001;2:569–86. doi:10.1038/35085034.
Fox W, Ellard GA, Mitchison DA. Studies on the treatment of tuberculosis undertaken by the British Medical Research Council Tuberculosis Units, 1946–1986, with relevant subsequent publications. Int J Tuberc Lung Dis 1999;3:S231–79.
Thomas C. A literature review of the problems of delayed presentation for treatment and non-completion of treatment for tuberculosis in less developed countries and ways of addressing these problems using particular implementations of the DOTS strategy. J Manage Med 2002;16:371–400. doi:10.1108/02689230210446544.
Patton JS. Mechanisms of macromolecule absorption by the lungs. Adv Drug Deliv Rev 1996;19:3–36.
Patton JS, Fishburn CS, Weers JG. The lungs as a portal of entry for systemic drug delivery. Proc Am Thorac Soc 2004;1:338–44. doi:10.1513/pats.200409-049TA.
Heyder J, Gebhart J, Rudolf G, Schiller CF, Stahlhofen W. Deposition of particles in the human respiratory tract in the size range 0.005–15 um. J Aerosol Sci 1986;17:811–25. doi:10.1016/0021-8502(86)90035-2.
Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, et al. Large porous particles for pulmonary drug delivery. Science 1997;276:1868–72. doi:10.1126/science.276.5320.1868.
Tsapis N, Bennett D, O'Driscoll K, Shea K, Lipp MM, Fu K, et al. Direct lung delivery of para-aminosalicylic acid by aerosol particles. Tuberculosis 2003;83:379–85. doi:10.1016/j.tube.2003.08.016.
Fiegel J, Garcia-Contreras L, Thomas M, VerBerkmoes J, Elbert K, Hickey A, et al. Preparation and in vivo evaluation of a dry powder for inhalation of capreomycin. Pharm Res 2007;25:805–11.
Garcia-Contreras L, Fiegel J, Telko MJ, Elbert K, Hawi A, Thomas M, et al. Inhaled large porous particles of capreomycin for treatment of tuberculosis in a guinea pig model. Antimicrob Agents Chemother 2007;51:2830–6. doi:10.1128/AAC.01164-06.
Gelperina S, Kisich K, Iseman MD, Heifets L. The potential advantages of nanoparticle drug delivery systems in chemotherapy of tuberculosis. Am J Respir Crit Care Med 2005;172:1487–90. doi:10.1164/rccm.200504-613PP.
Hansand ML, Lowman AM. Biodegradable nanoparticles for drug delivery and targeting. Curr Opin Solid State Mater Sci 2002;6:319–27. doi:10.1016/S1359-0286(02)00117-1.
Kawashima Y, Yamamoto H, Takeuchi H, Fujioka S, Hino T. Pulmonary delivery of insulin with nebulized -lactide/glycolide copolymer (PLGA) nanospheres to prolong hypoglycemic effect. J Control Release 1999;62:279–87. doi:10.1016/S0168-3659(99)00048-6.
Yamamoto H, Kuno Y, Sugimoto S, Takeuchi H, Kawashima Y. Surface-modified PLGA nanosphere with chitosan improved pulmonary delivery of calcitonin by mucoadhesion and opening of the intercellular tight junctions. J Control Release 2005;102:373–81. doi:10.1016/j.jconrel.2004.10.010.
Vaughn JM, McConville JT, Burgess D, Peters JI, Johnston KP, Talbert RL, et al. Single dose and multiple dose studies of itraconazole nanoparticles. Eur J Pharm Biopharma 2006;63:95–102. doi:10.1016/j.ejpb.2006.01.006.
Dailey LA, Schmehl T, Gessler T, Wittmar M, Grimminger F, Seeger W, et al. Nebulization of biodegradable nanoparticles: impact of nebulizer technology and nanoparticle characteristics on aerosol features. J Control Release 2003;86:131–44. doi:10.1016/S0168-3659(02)00370-X.
Le Brun PPH, de Boer AH, Frijlink HW, Heijerman HGM. A review of the technical aspects of drug nebulization. Pharm World Sci 2000;22:75–81. doi:10.1023/A:1008786600530.
Wendorf J, Singh M, Chesko J, Kazzaz J, Soewanan E, Ugozzoli M, et al. A practical approach to the use of nanoparticles for vaccine delivery. J Pharm Sci 2006;95:2738–50. doi:10.1002/jps.20728.
Saez A, Guzman M, Molpeceres J, Aberturas MR. Freeze-drying of polycaprolactone and poly(-lactic-glycolic) nanoparticles induce minor particle size changes affecting the oral pharmacokinetics of loaded drugs. Eur J Pharm Biopharma 2000;50:379–87. doi:10.1016/S0939-6411(00)00125-9.
Heyder J, Rudolf G. Mathematical models of particle deposition in the human respiratory tract. J Aerosol Sci 1984;15:697–707. doi:10.1016/0021-8502(84)90007-7.
Tsapis N, Bennett D, Jackson B, Weitz DA, Edwards DA. Trojan particles: large porous carriers of nanoparticles for drug delivery. Proc Natl Acad Sci U S A 2002;99. doi:10.1073/pnas.182233999.
Sung JC, Pulliam BL, Edwards DA. Nanoparticles for drug delivery to the lungs. Trends Biotechnol 2007;25:563–70. doi:10.1016/j.tibtech.2007.09.005.
Chew NYK, Shekunov BY, Tong HHY, Chow AHL, Savage C, Wu J, et al. Effect of amino acids on the dispersion of disodium cromoglycate powders. J Pharm Sci 2005;94:2289–300. doi:10.1002/jps.20426.
Li H-Y, Seville PC, Williamson IJ, Birchall JC. The use of amino acids to enhance the aerosolisation of spray-dried powders for pulmonary gene therapy. J Gene Med 2005;7:343–53. doi:10.1002/jgm.654.
Azarmi S, Tao X, Chen H, Wang Z, Finlay WH, Lobenberg R, et al. Formulation and cytotoxicity of doxorubicin nanoparticles carried by dry powder aerosol particles. Int J Pharm 2006;319:155–61. doi:10.1016/j.ijpharm.2006.03.052.
Hadinoto K, Zhu K, Tan RBH. Drug release study of large hollow nanoparticulate aggregates carrier particles for pulmonary delivery. Int J Pharm 2007;341:195–2061. doi:10.1016/j.ijpharm.2007.03.035.
Grenha A, Seijo B, Remunan-Lopez C. Microencapsulated chitosan nanoparticles for lung protein delivery. Eur J Pharm Sci 2005;25:427–37. doi:10.1016/j.ejps.2005.04.009.
O'Hara P, Hickey AJ. Respirable PLGA microspheres containing rifampicin for the treatment of tuberculosis: manufacture and characterization. Pharm Res 2000;V17:955–61. doi:10.1023/A:1007527204887.
Joshi DP, Lan-Chun-Fung YL, Pritchard JG. Determination of poly(vinyl alcohol) via its complex with boric acid and iodine. Anal Chim Acta 1979;104:153–60. doi:10.1016/S0003-2670(01)83825-3.
Garcia-Contreras L, Hickey AJ. Pharmacokinetics of aerosolized rifampicin in the guinea pig. In: Dalby RN, Byron PR, Peart J, Farr S, editors. Respiratory drug delivery VIII. Raleigh, NC: Horwood; 2002.
Peloquin CA, Namdar R, Singleton MD, Nix DE. Pharmacokinetics of rifampin under fasting conditions, with food, and with antacids. Chest 1999;115:12–8. doi:10.1378/chest.115.1.12.
Garcia-Contreras L, Sethuraman V, Kazantseva M, Godfrey V, Hickey AJ. Evaluation of dosing regimen of respirable rifampicin biodegradable microspheres in the treatment of tuberculosis in the guinea pig. J Antimicrob Chemother 2006;58:980–6. doi:10.1093/jac/dkl369.
Suarez S, O'Hara P, Kazantseva M, Newcomer CE, Hopfer R, McMurray DN, et al. Respirable PLGA microspheres containing rifampicin for the treatment of tuberculosis: screening in an infectious disease model. Pharm Res 2001;V18:1315–9. doi:10.1023/A:1013094112861.
Suarez S, O'Hara P, Kazantseva M, Newcomer CE, Hopfer R, McMurray DN, et al. Airways delivery of rifampicin microparticles for the treatment of tuberculosis. J Antimicrob Chemother 2001;48:431–4. doi:10.1093/jac/48.3.431.
Coowanitwong I, Arya V, Kulvanich P, Hochhaus GN. Slow release formulations of inhaled rifampin. AAPS J 2008;10:342–8. doi:10.1208/s12248–008–9044–5.
Pandey R, Sharma A, Zahoor A, Sharma S, Khuller GK, Prasad B. Poly (DL-lactide-co-glycolide) nanoparticle-based inhalable sustained drug delivery system for experimental tuberculosis. J Antimicrob Chemother 2003;52:981–6. doi:10.1093/jac/dkg477.
Sharma A, Sharma S, Khuller GK. Lectin-functionalized poly (lactide-co-glycolide) nanoparticles as oral/aerosolized antitubercular drug carriers for treatment of tuberculosis. J Antimicrob Chemother 2004;54:761–6. doi:10.1093/jac/dkh411.
Zahoor A, Sharma S, Khuller GK. Inhalable alginate nanoparticles as antitubercular drug carriers against experimental tuberculosis. Int J Antimicrobial Agents 2005;26:298–303. doi:10.1016/j.ijantimicag.2005.07.012.
Esmaeili F, Hosseini-Nasr M, Rad-Malekshahi M, Samadi N, Atyabi F, Dinarvand R. Preparation and antibacterial activity evaluation of rifampicin-loaded poly lactide-co-glycolide nanoparticles. Nanomed Nanotechnol Biol Med 2007;3:161–7. doi:10.1016/j.nano.2007.03.003.
Birnbaum DT, Kosmala JD, Brannon-Peppas L. Optimization of preparation techniques for poly(lactic acid-co-glycolic acid) nanoparticles. J Nanopart Res 2000;V2:173–81. doi:10.1023/A:1010038908767.
Dailey LA, Jekel N, Fink L, Gessler T, Schmehl T, Wittmar M, et al. Investigation of the proinflammatory potential of biodegradable nanoparticle drug delivery systems in the lung. Toxicol Appl Pharmacol 2006;215:100–8. doi:10.1016/j.taap.2006.01.016.
Birnbaum DT, Brannon-Peppas L. Molecular weight distribution changes during degradation and release of PLGA nanoparticles containing epirubicin HCl. J Biomater Sci Polym Ed 2003;14:87–102. doi:10.1163/15685620360511155.
Peloquin C, Vernon A. Antimycobacterial agents: rifamycins for mycobacterial infections. In: Yu V, Edwards G, McKinnon P, Peloquin C, Morse G, editors. Antimicrobial chemotherapy and vaccines, vol. II: antimicrobial agents. 2nd ed. Pittsburg: Esun Technologies; 2005. p. 383–402.
Peloquin C. Clinical pharmacology of the anti-tuberculosis drugs. In: Davies P, Barnes P, Gordon S, editors. Clinical tuberculosis. 4th ed. London: Hodder Arnold; 2008.
Dickinson JM, Mitchison DA. Suitability of rifampicin for intermittent administration in the treatment of tuberculosis. Tubercle 1970;51:82–94. doi:10.1016/0041-3879(70)90131-5.
Acknowledgements
The authors thank Plastiape for their generous donation of inhaler devices and Shionogi for supplying capsules, Prof. Patrick Couvreur for fruitful discussions and Annalicia Poehler for research assistance. Electron microscopy work was performed at the Center for Nanoscale Systems (CNS), part of the Faculty of Arts and Sciences at Harvard University. This work was supported by a grant from the National Institute of Health/NIAID under Grant Number 5 U01 61336-02 and a National Science Foundation Graduate Research Fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sung, J.C., Padilla, D.J., Garcia-Contreras, L. et al. Formulation and Pharmacokinetics of Self-Assembled Rifampicin Nanoparticle Systems for Pulmonary Delivery. Pharm Res 26, 1847–1855 (2009). https://doi.org/10.1007/s11095-009-9894-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-009-9894-2