Abstract
Long-circulating liposomes, such as PEG-liposomes, are frequently studied for drug delivery and diagnostic purposes. In our group, poly(amino acid) (PAA)-based coatings for long-circulating liposomes have been developed. These coatings provide liposomes with similar circulation times as compared to PEG-liposomes, but have the advantage of being enzymatically degradable. For PEG-liposomes it has been reported that circulation times are relatively independent of their physicochemical characteristics. In this study, the influence of factors such as PAA grafting density, cholesterol inclusion, surface charge, particle size, and lipid dose on the circulation kinetics of PAA-liposomes was evaluated after intravenous administration in rats. Prolonged circulation kinetics of PAA-liposomes can be maintained upon variation of liposome characteristics and the lipid dose given. However, the use of relatively high amounts of strongly charge-inducing lipids and a too large mean size is to be avoided. In conclusion, PAA-liposomes represent a versatile drug carrier system for a wide variety of applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Liposomes have repeatedly shown to be able to improve the therapeutic index of a variety of drugs. Intravenously administered liposomes generally undergo extensive opsonization and are therefore rapidly cleared by macrophages of the mononuclear phagocyte system (MPS), particularly Kupffer cells in the liver and spleen macrophages. As a result, liposome targeting to pathological tissues is impeded. This drawback could be amended by coating liposomes with hydrophilic, neutral polymers such as polyethylene glycol (PEG) (1). PEG increases the hydrophilicity of the liposome surface and provides a steric barrier against opsonization (1, 2). The resulting long-circulating liposomes, also referred to as ‘stealth’ or ‘sterically stabilized’ liposomes, are still removed from the blood circulation, however, removal occurs at a much lower rate and with less involvement of the hepatosplenic macrophages. Consequently, they circulate in the bloodstream for a prolonged period of time, enabling their extravasation into solid tumors and sites of inflammation by virtue of the presence of capillary discontinuities. This so-called enhanced permeability and retention (EPR) effect allows for increased local drug concentrations in the target region (3).
Besides PEG, several other hydrophilic polymers have been successfully applied as coatings for long-circulating liposomes, among them conjugates based on poly(oxazoline) (4), polyglycerol (5), poly(N-(2-hydroxypropyl)methacrylamide)) (6), poly-N-vinylpyrrolidone (7, 8) and polyvinyl alcohol (9). Our group proposed liposome coatings based on poly(amino acid)s (PAA): poly(hydroxyethyl l-glutamine)-N-succinyldioctadecylamine (PHEG-DODASuc) and poly(hydroxyl-ethyl l-asparagine)-DODASuc (PHEA-DODASuc) (Fig. 1) (10, 11). PAAs have the advantage of being degradable by lysosomal proteases, allowing for a complete elimination from the body, and reducing the risk of side effects associated with polymer accumulation, as described to occur in case of some non-degradable polymers (12–15). Their degradability can also be exploited for enzyme-induced drug release and/or target cell interaction, as the coating may be shed by proteolytic cleavage in the extracellular space of tumors and sites of inflammation. It has been demonstrated that PAA coatings can prolong circulation times of liposomes to an equal extent as a PEG coating (10).
An understanding of the effect of physicochemical characteristics of long-circulating liposomes on their pharmacokinetics and biodistribution is crucial for the rational development of therapeutic applications. Liposome clearance is a very complex mechanism and is mediated by a diversity of protein molecules such as immunoglobulins, complement factors and nonimmune opsonins, and the opsonization process can be very different for different types of liposomes (16–18). For long-circulating liposomes with PEG as a ‘stealth' coating, it has been reported that circulation times are relatively independent of factors such as lipid dose, lipid composition, surface charge and liposome size, which makes them versatile drug carriers (19). In the present study, we investigated if this also holds true for PAA-liposomes. Therefore, the influence of PAA grafting density, cholesterol inclusion, surface charge, particle size and lipid dose on the circulation kinetics and biodistribution of PAA-liposomes was evaluated.
MATERIALS AND METHODS
Materials
PHEA-DODASuc (average MW = 3,000 Da, determined by NMR and MALDI-ToF MS, corresponding with an average degree of polymerization of 15) and PHEG-DODASuc (average MW = 4,000 Da, determined by NMR and MALDI-ToF MS, corresponding with an average degree of polymerization of 18) were synthesized as described previously (10). Dipalmitoyl phosphatidylcholine (DPPC), egg phosphatidylcholine (EPC) and egg phosphatidylglycerol (EPG) were kindly provided by Lipoid GmbH, Ludwigshafen, Germany. 1,2-Dioleoyl-3-trimethylammonium-propane (DOTAP) and l-α-phosphatidyl serine (PS, porcine brain, sodium salt) were purchased from Avanti Polar Lipids, Inc., Alabaster, AL, USA. Cholesterol was purchased from Sigma-Aldrich Chemie BV, Zwijndrecht, The Netherlands. [3H]-Cholesteryl oleylether was a product of Amersham, Roosendaal, The Netherlands. Ultima Gold liquid scintillation cocktail and Solvable tissue solubilizer were purchased from Perkin Elmer BioScience B.V., Groningen, The Netherlands. All other reagents were of analytical grade.
Animals
Male outbred Wistar rats (body weight approximately 250 g) were obtained from Harlan Nederland, Horst, The Netherlands. Rats were housed in groups of four under standard laboratory conditions and had free access to rat chow and water. All animal experiments were performed according to national regulations and approved by the local animal experiments ethical committee.
Liposome Preparation
Liposomes were prepared as described previously by a lipid film hydration method (20). Appropriate amounts of DPPC, EPC, EPG, cholesterol, PS, or DOTAP were dissolved in ethanol in 50 ml round-bottom flasks (for lipid compositions see Table I). To each formulation 20 μl of the lipid phase marker [3H]-cholesteryl oleylether (approximately 740 kBq) were added. This label has been shown to be non-metabolizable and non-exchangeable (21, 22). The solvent was evaporated under a stream of nitrogen. The obtained lipid film was hydrated by gentle shaking in 2.5 ml HBS (5 mM HEPES, 0.9% NaCl, pH 7.4) resulting in a final concentration of 20 μmol total lipid/ml, except for two formulations to study the effect of the lipid dose: besides the formulation of 20 μmol total lipid/ml, a second formulation was prepared at a concentration of 0.2 μmol/ml and divided into two equal parts. One part was diluted 1:10 in HBS, yielding a lipid concentration of 0.02 μmol total lipid/ml. Liposomes of the different sizes were obtained by multiple extrusion through two stacked polycarbonate filters (Poretics, Livermore, CA, USA, 400, 200, and 100 nm pore size) with a high-pressure extruder. Formulations were stored at 4°C and used within 1 week after preparation.
Liposome Characterization
The mean particle size and polydispersity index (PD) of the liposome dispersions (diluted 1:100 with HBS) were measured by dynamic light scattering on a Malvern ALV/CGS-3 Goniometer, detected at an angle of 90° to the laser beam. The polydispersity index gives information on the particle size distribution, it ranges from 0 for an entirely monodisperse up to 1 for a polydisperse system. The phospholipid content of the liposomal dispersions was determined colorimetrically according to Rouser et al. (23). Radioactivity of the liposomal dispersions was analyzed in an Ultima Gold liquid scintillation cocktail (dilution of 1:1,000) and counted in a Packard Tricarb 2200 CA liquid scintillation counter.
Pharmacokinetics
Rats were put under light isoflurane anesthesia and liposomes were injected via the tail vein. To study the effect of lipid dose, injections of 25, 0.25, and 0.025 μmol total lipid/kg were given. For all other studies the injected dose was 20 μmol total lipid/kg. Blood samples (approximately 150 μl) were drawn under isoflurane anesthesia from the tail vein of each rat immediately after injection (from the opposite vein) and at 1, 4, 8, 24 and 48 h after injection. Hundred microliters of each blood sample were mixed with 100 μl Solvable tissue solubilizer and 100–200 μl 35% hydrogen peroxide to decolorize the samples and incubated overnight. Samples were diluted in 10 ml Ultima Gold scintillation cocktail and radioactivity was subsequently assessed in a Packard Tricarb 2200CA liquid scintillation counter. Forty-eight hours after injection, the rats were sacrificed by cervical dislocation and for the studies involving variations in surface charge, liposome size and lipid dose, liver and spleen were dissected and homogenized in 25 and 5 ml water, respectively. To 0.5 ml of the liver homogenate and 1 ml of the spleen homogenate, 200 μl of Solvable tissue solubilizer and 200 μl 35% hydrogen peroxide were added and mixtures were incubated until samples were dissolved and colorless. Radioactivity of the samples was assessed in 10 ml Ultima Gold scintillation cocktail as described above. Besides tissue and blood samples, also liposome samples were analyzed to determine the radioactivity of the injected amount of liposomes.
Data Analysis
Blood concentrations of liposomes at the different time points were calculated from the radioactivity of the blood samples as the percentage of the radioactivity measured immediately after injection (% injected dose). For the blood samples, a Q-test for identification of outliers was applied. From the blood concentration-time curves, area under the curve values were calculated for the analyzed time interval from zero to 48 hours using the trapezoidal rule [AUC0–48 h (% injected dose × h)]. The percentage of the injected dose (% ID) in the organs was calculated by division of the radioactivity of the organs by the radioactivity of the injected liposome amount. Differences in AUCs and liver and spleen values were compared by a one-way analysis of variance. The Bonferroni method was used to correct for multiple comparison. Differences were considered significant when the p-value was <0.05. All analyses were performed using Graph Pad Prism 4 software.
RESULTS AND DISCUSSION
To study the effect of liposome characteristics on the pharmacokinetics and biodistribution, different liposome types were prepared. Liposome compositions, sizes and polydispersity indices are presented in Table I. Different grafting densities of PAAs on the liposome surface were studied. The bilayer fluidity of liposomes was varied by inclusion of cholesterol. The effect of charge was examined by inclusion of the negatively charged lipids egg phosphatidylglycerol (EPG) and phosphatidylserine (PS) and the positively charged lipid dioleoyl phosphatidyltrimethylammonium propane (DOTAP). The effect of particle size was assessed with liposomes of sizes between 120 and 360 nm. The lipid doses needed in therapeutic settings can differ substantially. PEG-liposomes show dose-independent pharmacokinetics over a broad dose range, however at low doses (<1 μmol/kg) rapid clearance has been reported. To investigate if this also holds true for PAA-liposomes, the effect of lipid dose on the pharmacokinetics of PAA-liposomes was examined. Except for liposome formulations prepared to study the effect of liposome size, the hydrodynamic diameter of liposomes varied between 105 and 160 nm and the polydispersity index was ≤0.14, indicating a relatively narrow size distribution.
Effect of Grafting Density
In Table II the effect of three different grafting levels of PHEA-DODASuc (i.e. 2.5, 7.5 and 15 mol%) on the circulation kinetics of liposomes is shown. For this study the composition of DPPC and cholesterol (2:1) was chosen to be able to compare the data to earlier published results on the effect of grafting density of PHEG-DODASuc (1, 2.5, 7.5 and 15 mol%) on liposome circulation times (10). The blood concentrations at 4 and 24 h post-injection show no significant differences between the formulations. This is in line with the findings on the effect of grafting density of PHEG-DODASuc on liposome circulation times (10). The density of stealth polymers on the liposome surface has been shown to be of importance in the design of long-circulating liposomes. For example, for PEG-liposomes with a PEG2000-conjugate a grafting density of 5 to 7.5 mol% is often used in preclinical studies (24, 25). At PEG levels >4 mol%, a transition from the mushroom state, where PEG chains do not interact laterally, to the denser and thicker brush state of PEG occurs, the latter being the condition for optimal steric stabilization of the liposomes (26). It has been shown that a further increase of the density of PEG up to 20 mol% did not change circulation kinetics and biodistribution. However, considerable foaming made liposome preparation difficult; the foaming was likely related to the presence of PEG-DSPE micelles (24). Our studies show that at grafting densities between 2.5 and 15%, PAAs are able to prolong liposome circulation times similar to PEG. In previous studies a PAA grafting density of 7.5% was used, however, the present study indicates that a lower grafting density of 2.5% is also sufficient to prolong liposome circulation times.
Effect of Cholesterol Inclusion
The circulation kinetics of EPC-based liposomes without or with 33 mol% cholesterol and coated with PHEA or PHEG were determined (Fig. 2). For both PHEA- and PHEG-liposomes, only small differences in circulation profiles and AUC values of liposomes with or without cholesterol were observed. Cholesterol is known to influence the bilayer fluidity, resulting in increased rigidity and lateral packing and an increased phase transition temperature (27). For conventional PC-based liposomes interaction with proteins was reduced and circulation times were extended upon inclusion of cholesterol (28, 29). For PEGylated liposomes controversial observations have been made. Addition of 20–50 mol% cholesterol resulted in improved circulation kinetics (25). In other studies, however, no differences in circulation times and biodistribution have been observed when 33 mol% cholesterol were added, indicating that differences in bilayer rigidity have only little influence on the circulation kinetics of liposomes that are shielded by a ‘stealth’ coating (30, 31). Our findings are in agreement with this observation made with PEG-liposomes: shielding of liposomes by PAAs diminished the influence of bilayer fluidity on circulation times.
Pharmacokinetic behavior of EPC-liposomes coated with PHEA (top left) and PHEG (top right) without (empty squares) or with (filled squares) 33% cholesterol (% injected dose). Area under the curve (AUC0–48 h) values (bottom) calculated from blood concentration time curves. All results are expressed as mean ± SD (n = 3–4). *p < 0.05; n.s. Not significant.
Effect of Charged Lipids
Charged lipids are often added to liposome formulations to improve drug loading and/or stability of the formulation against aggregation during storage (30, 31). Changing the surface charge of conventional liposomes has been shown to greatly influence their pharmacokinetic behavior (32, 33). For PEG-liposomes it has been reported that the polymer is able to shield liposome charge. For example, PEG-liposomes containing up to 30 mol% of the negatively charged phospholipid EPG showed no altered pharmacokinetic behavior (30, 31). This is in line with our findings that inclusion of 20 mol% of EPG in PAA-coated liposomes did not result in significant changes in circulation kinetics and biodistribution (Fig. 3 and Table III). When 47.5 mol% of this lipid were included, only a slight decrease in circulation times was observed.
Pharmacokinetic behavior of EPC liposomes with a negative charge. EPC-liposomes (filled diamonds), EPC/EPG-liposomes in a molar ratio of 4:1 (filled circles) or 1:1 (filled squares) and EPC/PS-liposomes (9:1) (filled triangles) coated with PHEA (top left) and PHEG (top right) (% injected dose). Area under the curve (AUC0-48h) values (bottom) calculated from blood concentration time curves. All results are expressed as mean ± SD (n = 3–4). **p < 0.01; *p < 0.05; n.s. Not significant.
When the negatively charged phospholipid PS was included in PHEA- and PHEG-liposomes at a level of 10 mol%, a very rapid removal from the circulation was observed. Apparently, at the grafting density level of 5 mol%, PAAs are not able to sufficiently shield PS-containing liposomes from opsonization. This is in line with the findings that 5 mol% of PEG was not effective in protecting PS-containing liposomes from rapid clearance (24). PS containing PAA-liposomes showed an enhanced liver distribution when compared to PAA-liposomes containing EPG. The results indicate that PAA-coatings are able to shield the surface of EPG-containing liposomes more effectively than that of PS-containing liposomes. It has been suggested that the position of the negative charge within the molecule might play a role in the differences in shielding capacity (33). The negatively charged carboxyl group of PS is located at the terminal position of the hydrophilic part of the molecule, directed to the outer fluid, whereas the negatively charged phosphate group of EPG is located closer to the hydrophobic anchor and therefore shielded more effectively by the coating. In addition, the observed differences in pharmacokinetics of both types of liposomes may be related to the involvement of a receptor recognition mechanism in case of the PS-containing PAA-liposomes (33). PS has important physiological functions, it serves as signal for recognition and removal of aged erythrocytes and apoptotic cells by macrophages, which display a PS-specific receptor (34). In addition, it binds to clotting factors and initiates coagulation (35, 36). PS-containing liposomes are known to bind high amounts of plasma proteins. They are rapidly cleared from the circulation by the MPS, show in particular high uptake by Kupffer cells of the liver and activate the complement system (37, 38).
The differences in pharmacokinetics between the differently charged formulations were not reflected in the distribution to liver and spleen. However, it should be realized that the presented data likely give an underestimated impression of the actual hepatosplenic accumulation, as at 48 h post-injection liposomes may have already been subject to substantial degradation and consequently redistribution of the label may have occurred.
Besides liposomes with a negative surface charge, PAA-coated liposomes prepared with 47.5 mol% of the positively charged lipid DOTAP were studied. These cationic liposomes were very rapidly cleared from the bloodstream, independent of the type of PAA-coating. Less than 1% of the administered dose was detected in the blood circulation one hour after injection of PHEA- or PHEG-liposomes. Cationic liposomes have been reported to interact strongly with blood components and may even induce aggregate formation in the circulation (29, 39, 40). PHEA and PHEG at a grafting density of 5 mol% are apparently not capable to shield and prolong the circulation times of cationic liposomes containing high levels of DOTAP (47.5 mol%).
Effect of Particle Size
The circulation kinetics and AUC values of PHEA- and PHEG-liposomes of approximately 360, 230 and 120 nm are shown in Fig. 4. Table IV summarizes their distribution to liver and spleen. Liposomes with a mean size of 120 nm were removed from the bloodstream at a lower rate than liposomes of 230 and 360 nm, respectively, for both PHEA- and PHEG-coated liposomes. This observation has also been reported in independent studies for conventional and PEGylated liposomes (25, 30, 32, 41–43). PEG-liposomes with a diameter of more than 200 nm are more rapidly cleared than liposomes with a diameter between 100 and 200 nm. A decrease in size has been shown to also reduce recognition by the complement system (44–46). At 48 hours after administration, the liposome formulation tested showed only small differences regarding the degree of uptake by liver and spleen. As mentioned above, differences may have been obscured as at this late time point redistribution of the label may already have occurred. Our results indicate that, as observed for PEG-liposomes, also for PHEA- and PHEG-liposomes a particle size below 150 nm is the most optimal to achieve long-circulation properties.
Pharmacokinetic behavior of EPC/EPG (1:1) liposomes coated with PHEA (top left) and PHEG (top right) of 360 nm (filled squares) 230 nm (filled circles) and 120 nm (filled diamonds) (% injected dose). Area under the curve (AUC0–48 h) values (bottom) calculated from blood concentration time curves. All results are expressed as mean±SD (n = 4). **p < 0.01; n.s. Not significant.
Effect of Lipid Dose
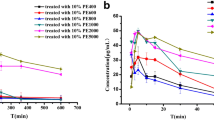
The effect of the administered lipid dose of PHEG-liposomes on the circulation kinetics and AUC values is shown in Fig. 5. No differences in clearance were observed when liposomes were administered at doses of 25, 0.25, and 0.025 μmol/kg. At 48 hours after administration, liver uptake was also independent of the lipid dose but spleen uptake was lower at both lower lipid doses (Table V). For PEG-liposomes dose-independent kinetics have been observed over a dose range between 4 and 400 μmol/kg (47). However, at doses <1 μmol/kg, which are used in case of for instance diagnostic imaging of tumors and sites of inflammation, PEG-liposomes are much more rapidly cleared from the circulation (48, 49).
Pharmacokinetic behavior of EPC/EPG-liposomes coated with PHEG at 25 μmol/kg (filled squares), 0.25 μmol/kg and (filled diamonds) 0.025 μmol/kg (filled squares) (% injected dose) (left). Area under the curve (AUC0–48 h) values (right) calculated from blood concentration time curves. All results are expressed as mean±SD (n = 4). n.s. Not significant.
The mechanism behind this ‘enhanced clearance effect’ at low lipid dose is not yet fully understood. It has been suggested that rapid clearance is mediated by a limited pool of circulating opsonic factors that interact with PEG-liposomes and induce phagocytosis. At higher lipid doses, the influence of this relatively low amount of opsonic factors becomes more restricted and the majority of the administered liposomes will be long-circulating (49, 50). For PHEA-liposomes, a recent study showed dose-independent pharmacokinetics for doses as low as 0.025 μmol/kg (51). The present study demonstrates that this is also the case for PHEG-liposomes. This benefit of PAA-liposomes over PEG-liposomes can be advantageous in situations in which only low lipid doses of liposomes are required for the desired application.
CONCLUSION
This study demonstrates that the prolonged circulation kinetics of PAA-liposomes can be maintained upon variation of liposome characteristics and the lipid dose given. This allows the possibility to tailor the liposome composition to the required properties for achieving efficient drug targeting, without the risk of negative effects on the long-circulation property of the PAA-liposomes. However, the use of relatively high amounts of strongly charge-inducing lipids and a too large mean size is to be avoided.
In addition to their advantage of being enzymatically degradable, PAAs are able to sterically stabilize a broad range of liposomes varying in physicochemical properties and therefore PAA-liposomes represent a versatile drug carrier system for a wide variety of applications.
References
A. L. Klibanov, K. Maruyama, V. P. Torchilin, and L. Huang. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett. 268:235–237 (1990).
A. Mori, A. L. Klibanov, V. P. Torchilin, and L. Huang. Influence of the steric barrier activity of amphipathic poly(ethyleneglycol) and ganglioside GM1 on the circulation time of liposomes and on the target binding of immunoliposomes in vivo. FEBS Lett. 284:263–266 (1991).
H. Maeda, J. Wu, T. Sawa, Y. Matsumura, and K. Hori. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release. 65:271–284 (2000).
M. C. Woodle, C. M. Engbers, and S. Zalipsky. New amphipatic polymer–lipid conjugates forming long-circulating reticuloendothelial system-evading liposomes. Bioconjug Chem. 5:493–496 (1994).
K. Maruyama, S. Okuizumi, O. Ishida, H. Yamauchi, H. Kikuchi, and M. Iwatsuru. Phosphatidylpolyglycerols prolong liposome circulation in vivo. Int J Pharm. 111:103–107 (1994).
K. Whiteman. Poly(HPMA)-coated liposomes demonstrate prolonged circulation in mice. Journal of Liposome Research. 11:153–164 (2001).
V. P. Torchilin, M. I. Shtilman, V. S. Trubetskoy, K. Whiteman, and A. M. Milstein. Amphiphilic vinyl polymers effectively prolong liposome circulation time in vivo. Biochim Biophys Acta. 1195:181–184 (1994).
V. P. Torchilin, T. S. Levchenko, K. R. Whiteman, A. A. Yaroslavov, A. M. Tsatsakis, A. K. Rizos, E. V. Michailova, and M. I. Shtilman. Amphiphilic poly-N-vinylpyrrolidones: synthesis, properties and liposome surface modification. Biomaterials. 22:3035–3044 (2001).
H. Takeuchi, H. Kojima, H. Yamamoto, and Y. Kawashima. Evaluation of circulation profiles of liposomes coated with hydrophilic polymers having different molecular weights in rats. J Control Release. 75:83–91 (2001).
J. M. Metselaar, P. Bruin, L. W. de Boer, T. de Vringer, C. Snel, C. Oussoren, M. H. Wauben, D. J. Crommelin, G. Storm, and W. E. Hennink. A novel family of l-amino acid-based biodegradable polymer–lipid conjugates for the development of long-circulating liposomes with effective drug-targeting capacity. Bioconjug Chem. 14:1156–1164 (2003).
B. Romberg, J. M. Metselaar, T. de Vringer, K. Motonaga, J. J. Kettenes-van den Bosch, C. Oussoren, G. Storm, and W. E. Hennink. Enzymatic degradation of liposome-grafted poly(hydroxyethyl l-glutamine). Bioconjug Chem. 16:767–774 (2005).
S. M. Moghimi, and J. Szebeni. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog Lipid Res. 42:463–478 (2003).
A. Bendele, J. Seely, C. Richey, G. Sennello, and G. Shopp. Short communication: renal tubular vacuolation in animals treated with polyethylene–glycol-conjugated proteins. Toxicol Sci. 42:152–157 (1998).
K. Miyasaki. Experimental polymer storage disease in rabbits. An approach to the histogenesis of sphingolipidoses. Virchows Arch A Pathol Anat Histol. 365:351–365 (1975).
M. Christensen, P. Johansen, and C. Hau. Storage of polyvinylpyrrolidone (PVP) in tissues following long-term treatment with a PVP-containing vasopressin preparation. Acta Med Scand. 204:295–298 (1978).
D. V. Devine, and J. M. Marjan. The role of immunoproteins in the survival of liposomes in the circulation. Crit Rev Ther Drug Carrier Syst. 14:105–131 (1997).
J. Szebeni. The interaction of liposomes with the complement system. Crit Rev Ther Drug Carrier Syst. 15:57–88 (1998).
X. Yan, G. L. Scherphof, and J. A. Kamps. Liposome opsonization. J Liposome Res. 15:109–139 (2005).
D. C. Drummond, O. Meyer, K. Hong, D. B. Kirpotin, and D. Papahadjopoulos. Optimizing liposomes for delivery of chemotherapeutic agents to solid tumors. Pharmacol Rev. 51:691–743 (1999).
S. Amselem, A. Gabizon, and Y. Barenholz. A large-scale method for the preparation of sterile and non-pyrogenic liposomal formulations of defined size distributions for clinical use. In G. Gregoriadis (ed), Liposome Technology, CRC press, Boca Raton, FL, 1993, pp. 501–525.
Y. Stein, G. Halperin, and O. Stein. Biological stability of [3H]cholesteryl oleyl ether in cultured fibroblasts and intact rat. FEBS Lett. 111:104–106 (1980).
G. L. Pool, M. E. French, R. A. Edwards, L. Huang, and R. H. Lumb. Use of radiolabeled hexadecyl cholesteryl ether as a liposome marker. Lipids. 17:448–452 (1982).
G. Rouser, S. Fleischer, and A. Yamamoto. Two dimensional thin layer chromatographic separation of polar lipids and determination of phospholipids by phosphorus analysis of spots. Lipids. 5:494–496 (1970).
T. M. Allen, C. Hansen, F. Martin, C. Redemann, and A. Yau-Young. Liposomes containing synthetic lipid derivatives of poly(ethylene glycol) show prolonged circulation half-lives in vivo. Biochimica et Biophysica Acta (BBA)-Biomembranes. 1066:29–36 (1991).
K. Maruyama, T. Yuda, A. Okamoto, S. Kojima, A. Suginaka, and M. Iwatsuru. Prolonged circulation time in vivo of large unilamellar liposomes composed of distearoyl phosphatidylcholine and cholesterol containing amphipathic poly(ethylene glycol). Biochim Biophys Acta. 1128:44–49 (1992).
A. K. Kenworthy, S. A. Simon, and T. J. McIntosh. Structure and phase behavior of lipid suspensions containing phospholipids with covalently attached poly(ethylene glycol). Biophys J. 68:1903–1920 (1995).
R. A. Demel, and B. De Kruyff. The function of sterols in membranes. Biochim Biophys Acta. 457:109–132 (1976).
J. Senior, and G. Gregoriadis. Stability of small unilamellar liposomes in serum and clearance from the circulation: the effect of the phospholipid and cholesterol components. Life Sci. 30:2123–2136 (1982).
P. R. Cullis, A. Chonn, and S. C. Semple. Interactions of liposomes and lipid-based carrier systems with blood proteins: relation to clearance behaviour in vivo. Adv Drug Deliv Rev. 32:3–17 (1998).
M. C. Woodle, K. K. Matthay, M. S. Newman, J. E. Hidayat, L. R. Collins, C. Redemann, F. J. Martin, and D. Papahadjopoulos. Versatility in lipid compositions showing prolonged circulation with sterically stabilized liposomes. Biochim Biophys Acta. 1105:193–200 (1992).
R. M. Schiffelers, I. A. Bakker-Woudenberg, S. V. Snijders, and G. Storm. Localization of sterically stabilized liposomes in Klebsiella pneumoniae-infected rat lung tissue: influence of liposome characteristics. Biochim Biophys Acta. 1421:329–339 (1999).
J. H. Senior. Fate and behavior of liposomes in vivo: a review of controlling factors. Crit Rev Ther Drug Carrier Syst. 3:123–193 (1987).
A. Gabizon, and D. Papahadjopoulos. The role of surface charge and hydrophilic groups on liposome clearance in vivo. Biochim Biophys Acta. 1103:94–100 (1992).
M. Otsuka, K. Goto, S. Tsuchiya, and Y. Aramaki. Phosphatidylserine-specific receptor contributes to TGF-beta production in macrophages through a MAP kinase, ERK. Biol Pharm Bull. 28:1707–1710 (2005).
R. S. Schwartz, Y. Tanaka, I. J. Fidler, D. T. Chiu, B. Lubin, and A. J. Schroit. Increased adherence of sickled and phosphatidylserine-enriched human erythrocytes to cultured human peripheral blood monocytes. J Clin Invest. 75:1965–1972 (1985).
R. F. A. Zwaal, P. Comfurius, and E. M. Bevers. Lipid–protein interactions in blood coagulation. Biochimica et Biophysica Acta (BBA)-Reviews on Biomembranes. 1376:433–453 (1998).
D. Liu, F. Liu, and Y. K. Song. Recognition and clearance of liposomes containing phosphatidylserine are mediated by serum opsonin. Biochim Biophys Acta. 1235:140–146 (1995).
T. M. Allen, P. Williamson, and R. A. Schlegel. Phosphatidylserine as a determinant of reticuloendothelial recognition of liposome models of the erythrocyte surface. Proc Natl Acad Sci U S A. 85:8067–8071 (1988).
J. H. Senior, K. R. Trimble, and R. Maskiewicz. Interaction of positively-charged liposomes with blood: implications for their application in vivo. Biochim Biophys Acta. 1070:173–179 (1991).
W. Yeeprae, S. Kawakami, S. Suzuki, F. Yamashita, and M. Hashida. Physicochemical and pharmacokinetic characteristics of cationic liposomes. Pharmazie. 61:102–105 (2006).
A. L. Klibanov, K. Maruyama, A. M. Beckerleg, V. P. Torchilin, and L. Huang. Activity of amphipathic poly(ethylene glycol) 5000 to prolong the circulation time of liposomes depends on the liposome size and is unfavorable for immunoliposome binding to target. Biochim Biophys Acta. 1062:142–148 (1991).
D. C. Litzinger, A. M. Buiting, N. van Rooijen, and L. Huang. Effect of liposome size on the circulation time and intraorgan distribution of amphipathic poly(ethylene glycol)-containing liposomes. Biochim Biophys Acta. 1190:99–107 (1994).
V. D. Awasthi, D. Garcia, B. A. Goins, and W. T. Phillips. Circulation and biodistribution profiles of long-circulating PEG-liposomes of various sizes in rabbits. Int J Pharm. 253:121–132 (2003).
R. L. Richards, R. C. Habbersett, I. Scher, A. S. Janoff, H. P. Schieren, L. D. Mayer, P. R. Cullis, and C. R. Alving. Influence of vesicle size on complement-dependent immune damage to liposomes. Biochim Biophys Acta. 855:223–230 (1986).
H. Harashima, T. M. Huong, T. Ishida, Y. Manabe, H. Matsuo, and H. Kiwada. Synergistic effect between size and cholesterol content in the enhanced hepatic uptake clearance of liposomes through complement activation in rats. Pharm Res. 13:1704–1709 (1996).
A. J. Bradley, D. V. Devine, S. M. Ansell, J. Janzen, and D. E. Brooks. Inhibition of liposome-induced complement activation by incorporated poly(ethylene glycol)-lipids. Arch Biochem Biophys. 357:185–194 (1998).
T. M. Allen, and C. Hansen. Pharmacokinetics of stealth versus conventional liposomes: effect of dose. Biochim Biophys Acta. 1068:133–141 (1991).
P. Laverman, A. H. Brouwers, E. T. Dams, W. J. Oyen, G. Storm, N. van Rooijen, F. H. Corstens, and O. C. Boerman. Preclinical and clinical evidence for disappearance of long-circulating characteristics of polyethylene glycol liposomes at low lipid dose. J Pharmacol Exp Ther. 293:996–1001 (2000).
M. G. Carstens, B. Romberg, P. Laverman, O. C. Boerman, C. Oussoren, and G. Storm. Observations on the disappearance of the stealth property of PEGylated liposomes. Effects of lipid dose and dosing frequency. In G. Gregoriadis (ed), Liposome Technology, Vol. III CRC,London, 2006, pp. 79–93.
S. M. Moghimi, and J. Szebeni. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog Lipid Res. 42:463–478 (2003).
B. Romberg, C. Oussoren, C. J. Snel, M. G. Carstens, W. E. Hennink, and G. Storm. Pharmacokinetics of poly(hydroxyethyl-l-asparagine)-coated liposomes is superior over that of PEG-coated liposomes at low lipid dose and upon repeated administration. Biochimica et Biophysica Acta (BBA)-Biomembranes. 1768:737–743 (2007).
Acknowledgement
This work was financially supported by Astellas Pharma Inc., Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Romberg, B., Oussoren, C., Snel, C.J. et al. Effect of Liposome Characteristics and Dose on the Pharmacokinetics of Liposomes Coated with Poly(amino acid)s. Pharm Res 24, 2394–2401 (2007). https://doi.org/10.1007/s11095-007-9393-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-007-9393-2