Abstract
Photoacoustic (PA) medical imaging is a crossbred technique relying on light-induced ultrasonic waves due to the PA effect phenomenon recorded primarily in 1880 by A. G. Bell. Numerical simulation, also known as in-silico, studies assist scientists in minimizing incorrect PA experiments in both in-vitro and in-vivo. Numerical modeling techniques help to achieve a fast simulation process in contrast to pure mathematics alone. However, if a suitable facilitated mathematical model can be established prior to applying numerical modeling, it will be of great interest to the whole numeric model. Numerous mathematical equations, theorems, and propositions have been proposed to model the whole PA signal generation and propagation process in biological media. However, most of them are complicated and difficult to be understood by researchers, especially beginners. That’s why this paper was introduced. Our paper aims to simplify the understanding of the generation and propagation process of biomedical PA waves. We have developed a facilitated mathematical model for the entire process. The introduced developed mathematical model is based on three steps: (1) pulsed laser stimulation, (2) light diffusion, and (3) PA stress wave generation and propagation. The developed mathematical model has been implemented utilizing COMSOL Multiphysics, which relies on the finite element method (FEM) numerical modeling principle. The in-silico time-dependent study's results confirmed that the proposed mathematical model is a simple, efficient, accurate, and quick starting point for researchers to simulate biomedical PA signals' generation and propagation process utilizing any suitable software such as COMSOL multiphysics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Photoacoustic imaging (PAI) is a hybrid imaging technique merging optical illumination and ultrasound detection in one modality by utilizing the laser-induced ultrasound signals due to the photoacoustic (PA) effect phenomenon (Wang 2008; Wang et al. 2023; Attia et al. 2019; GadAllah et al. 2022; Wang and Song 2012; Lapierre-Landry et al. 2018; Chu and Chen 2023; Nyayapathi and Xia 2019; Beard 2011; Hui and Cheng 2019; Chen and Tian 2021; Zhang et al. 2023; Liu et al. 2018; Wang and Wang 2018). PAI has been able to produce images almost free of speckle artifacts (Wang 2008; GadAllah et al. 2022; Wang and Song 2012; Guo et al. 2009; Joseph 2013; Narayan, et al. 2014), in contrast to traditional ultrasound imaging (Kirk Shung et al. 1992; Kirk Shung 2006; Wagner 1983; Burckhardt 1978; GadAllah 2015; Najarian and Splinter 2012; Dickinson and Nassiri 2004; Szabo 2014; Webb 2003) and optical coherence tomography (OCT) (Wang and Hsin-i 2007a; Fercher 1996; Huang et al. 1991; Tuchin 2016; Hendon and Rollins 2016). PAI has gained a variety of implementation techniques and applications through the last three decades (Wang et al. 2023; GadAllah et al. 2022; Nyayapathi and Xia 2019; Liu and Zhang 2016; Sung-Liang Chen 2015). For instance: photoacoustic tomography (PAT) (Wang 2008, 2011; Zhou et al. 2016; Attia et al. 2019; Lin et al. 2023; Ntziachristos et al. 2005), multispectral optoacoustic tomography (MSOT) (GadAllah et al. 2022) or multispectral PAT, light emitting diode (LED) based PAI (Chandramoorthi and Thittai 2020), optical detection PAT (OD-PAT) or also named non-contact laser ultrasound (NC-LUS) (Zhang et al. 2019; Haupt et al. 2019; Dong et al. 2017), photoacoustic microscopy (PAM) (Sung-Liang Chen 2015; Zhang et al. 2023), optical resolution photoacoustic microscopy (OR-PAM) (Cao et al. 2023), acoustic resolution photoacoustic microscopy (AR-PAM) (Sung-Liang Chen 2015), raster-scan optoacoustic mesoscopy (RSOM) (GadAllah et al. 2022), LED-based PA microscopy (LD-PAM) (Li et al. 2021), Second generation PA remote sensing based microscopy (Ecclestone et al. 2022), PA endoscopy which is providing molecular contrast at considerable depths allowing for simultaneous imaging of structural and functional information (GadAllah et al. 2022; Yang et al. 2015; Liang et al. 2022), PA topography through an ergodic relay (PATER) (Li and Li 2020), and photoacoustic elastography (PAE) (Hai et al. 2016a, b; Suheshkumar Singh and Thomas 2019). PAI has a big contribution to cancer diagnosis (GadAllah et al. 2022; Bai et al. 2023; Chen et al. 2014) for instance in breast cancer (Attia et al. 2019; GadAllah et al. 2022; Nyayapathi and Xia 2019; Oraevsky et al. 2001), which has a high record in threatening human health, mostly females (Ayana et al. 2022; Zhang et al. 2018), the second most frequent cancer worldwide following lung cancer and the fifth leading cause of cancer death and a major cause of cancer death among women (Mohamed et al. 2022; Badawy et al. 2021a, 2021b). Imaging Alzheimer’s disease would be sensible by PAI of the brain (Park et al. 2019). PAI has been able to help in a real-time assessment of tissue hypoxia (Gerling et al. 2014). PAI’s guidance plays a strong role in more applications of image-guided surgery (IGS) and high intensity focused ultrasound (HIFU) (GadAllah et al. 2022).
It is merit to mention here the main difference between optoacoustic imaging (OAI) and thermoacoustic imaging (TAI). Commonly in the PA scientific community, PAI is a general term due to the PA effect basic phenomenon including two overlapped terms: optoacoustic and thermoacoustic imaging (Kellnberger 2013). The first, OAI, is mentioned to reflect the absorption of optical energy (optical wavelengths range from 400 to 700 nm) by tissue to generate the PA signal. The second, TAI (Aliroteh et al. 2016), is more general and is mentioned to reflect the absorption of any form of energy (popularly it is related to the whole electromagnetic spectrum’s radiation bands including but not restricted to the radiofrequency (RF) and microwave (MW) bands) by biological tissue to induce PA signal (Kellnberger 2013). So, in our opinion, the term thermoacoustic imaging (TAI) could be considered the more general term including basically PAI and OAI.
The basic principle for PAI or OAI (Wang 2008; Zhou et al. 2016; Oraevsky and Karabutov 2003) is the PA effect, been reported firstly in 1880 by Bell (1880, 1881), which can be described in biological tissues (Duck 1990) by two energy exchange processes through three forms of energy: (1) electromagnetic (light) energy, (2) heat energy, and (3) kinetic energy (generated ultrasound mechanical waves). Figure 1 represents the basic idea for PAI or OAI, where; the “target” tissue in the figure is the region of interest (ROI) to be investigated.
Numerical simulation for the generation process of PA signals in biological tissues helps researchers decrease error experiments in vitro, hence increasing safety rates (Sliney and Trokel 1993; Smalley 2013) in vivo. Numerical modeling methods are fast when compared to pure mathematics. If a suitable simplified mathematical model can be obtained to be an easy base for the aimed numerical model, it will be a great advantage.
A variety of scientific theories, equations, and assumptions through the literature of PA imaging have been introduced aiming to completely model the biomedical PA signal generation and propagation process. Starting from light-tissue interaction, heat-tissue interaction, and ending by the mechanical ultrasound pressure wave generation and propagation (Cox and Beard 2009, 2005; Cox et al. 2004; Treeby and Cox 2010; Treeby et al. 2023; Wang et al. 2012a; Wang et al. 2012b; Wang et al. 2012c; Wang et al. 1995; https://www.comsol.com; Metwally and El-Gohary 2014; Wilson and Adam 1983; https://www.ansys.com; El-Gohary et al. 2014; Metwally et al. 2014; Grahn 2017, 2015; Chandramoorthi and Thittai 2017;Liu et al. 2018; ElGohary et al. 2020; Song et al. 2021). However, more of them are complicated and are difficult being understood by researchers, especially beginners. So, this paper was proposed.
In this paper, we have attempted to simplify the modeling for the biomedical PA wave’s generation and propagation process, obtaining an easy simplified deduced mathematical model for the overall process to be a base for any numerical simulation software. This research paper is a conclusion of about two years of research into the deep literature of photoacoustic sensing and imaging. The proposed model here aims to shortcut the way for all beginners to simply but accurately model and simulate the photoacoustic wave generation and propagation through biological tissues. The introduced deduced model is based on three main stages. The first stage is applying pulsed laser irradiation. The second stage is light diffusion through biological tissue. The third stage is the PA pressure wave generation and propagation from the target tissue to the ultrasound transducer surface. The third stage contains inherently two energy transformation processes through three forms of energy: (1) electromagnetic (light) energy to (2) deposited heat energy to (3) kinetic energy (ultrasound pressure mechanical wave).
The proposed deduced mathematical model has been validated numerically by COMSOL Multiphysics. The simulation started with a simulated laser pulse input of about 10 ns duration on a tissue model with an inherent tumor. The produced simulated PA signal has been drawn vs. the time for more than one point containing a point in the center of the modeled target tumor. The results of the numerical simulation study assure that the proposed mathematical model may be considered as a simplified, easy, and fast startup base for scientific researchers to numerically model and simulate PA signals generation and propagation in biological tissues utilizing any numerical simulation platform such as COMSOL Multiphysics.
In the subsequent second section of this paper “Related Work”, we present some of the related research along the PA modeling history. In the following third section “Methods”: we present the mathematical model deduced in this work from the PA literature. Followed by the fourth section “Numerical simulation by COMSOL multiphysics”: illustrates the application of the proposed model on a simulated biomedical tissue including a tumor inside. The subsequent fifth section presents the “Qualitative and analytical results”. Finally, in the following sixth section, we concluded that this research paper may be considered as a simplified, but accurate base for the scientific research of PA signals’ generation and propagation studies using any numerical modeling software.
2 Related work
Cox and Beard (2009), have presented Modeling PA propagation in tissue utilizing frequency-wavenumber or k-space techniques, utilizing fast Fourier transform (FFT) and inverse FFT algorithms. Their model was based on the assumption that the produced PA waves distributed within the biomedical tissue often be considered instantaneous, allowing their model to be cast as an initial value problem with an easy k-space solution. Their work may be considered as an extension to their previous k-space based work, in 2005 (Cox and Beard 2005), for a Fast calculation of pulsed PA fields in fluids. An experimental validation for k-space based PA propagation models was introduced in 2004 by Cox et al. (2004), developing propagation models for temporal output prediction of a sensor due to an arbitrary PA generated initial stress distribution.
Treeby and Cox (2010), have introduced a new and freely available MATLAB toolbox to simulate and reconstruct PA wave fields, which they called: the “k-Wave” toolbox. After the birth of the K-wave toolbox, they both and Jiri Jaros (Treeby et al. 2023), have developed the K-Wave open-source toolbox for MATLAB and C+ +.
Wang et al. (2012a), have introduced an evaluation of a finite element method (FEM) (Logan 2023; Zienkiewicz et al. 2005; Reddy 2019) based numerical simulation model for PA signals in biological tissues using COMSOL Multiphysics (https://www.comsol.com). Their model has been built basically on four steps: (1) light energy irradiance described by a diffusion equation, (2) conversion from light to heat energy using a bio-heat transfer equation, (3) conversion from thermal to kinetic energy (PA wave generation) by a stress–strain model, (4) propagation of the induced PA wave by the homogeneous acoustic wave propagation equation. In the same year, they proposed their paper (Wang et al. 2012b) for discussing the applicability of their method introduced in Wang et al. 2012a using COMSOL to develop a new illumination scheme, a light catcher, for improving light penetration into deep tissues, in silico. At almost the end of the same year 2012, they introduced their study (Wang et al. 2012c), based on their last two papers (Wang et al. 2012a, b), improving their new light irradiance approach (the light catcher) for achieving more imaging depths in PA imaging, evaluating their study not only in silico but also by in-vitro experiments applied on different targets at various locations.
Metwally and El-Gohary (2014), introduced their investigation study about the influence of the light fluence distribution on PA back-propagation imaging using: (1) Monte Carlo technique (Wang et al. 1995; Wilson and Adam 1983) to estimate the propagation and distribution of the light fluence, and (2) FEM for numerically simulating the PA wave generation utilizing ANSYS (https://www.ansys.com).
El-Gohary et al. (2014), proposed a design Study for a PA Probe for Prostate Cancer Detection utilizing 3D Monte Carlo Simulation and FEM.
Metwally et al. (2014), presented their study about the influence of the anisotropic mechanical characteristics (elasticity) of Breast Cancer on PAI-based back-propagation technique utilizing FEM (The numerical simulation has been achieved by ANSYS (https://www.ansys.com), while the fluence distribution has been evaluated by light propagation resolving through a tissue model using Monte Carlo technique (Wang et al. 1995; Wilson and Adam 1983).
Grahn (2017), introduced his research article on PA Modeling with COMSOL, simulating a cantilever-based PA sensor popularly utilized in gases analysis and detection. His study’s governing equations have been derived by linearizing the Navier–Stokes equations, continuity equation and energy equation. This study is partially based on his previous study, in 2015 (Grahn 2015), which has been for modeling thermoacoustics of loudspeakers by COMSOL.
Chandramoorthi and Thittai (2017), have introduced a simulated PAT system utilizing: (1) COMSOL (in a four steps scheme such as in: Wang et al. (2012a, 2012b, 2012c)) for a FEM-based numerical simulation study, and (2) MATLAB (https://www.mathworks.com/products/matlab.html) for reconstruct an initial pressure distribution (image reconstruction) from the aggregated raw data from COMSOL with comparing the performance of two popularly utilized image reconstruction techniques called: filtered back projection (FBP) and synthetic aperture (SA) beamforming, resulting in a lateral resolution largely depends on the aperture parameters obtained by FBP versus SA.
Liu et al. (2018), have proposed their study for a handheld real-time PAI system for animal neurological disorder models. In their study, COMSOL has been utilized in numerical simulation (in a four-stage manner like in: Wang et al. (2012a, 2012b, 2012c)) for estimating both light propagation and hence the simulated PA wave generation to investigate the significant factors affecting the generation of PA signals.
El Gohary et al. (2020), introduced a numerical study for PA signals from eye models to discover diabetic retinopathy. Their study has been based on (two steps methodology like in: (Metwally and El-Gohary 2014; El-Gohary et al. 2014; Metwally et al. 2014)): (1) Monte Carlo method utilized to simulate the interaction of a 0.8 ns duration laser pulse with eye tissues at 750 nm wavelength, and (2) thermal structural and acoustical analyses have been carried out utilizing a commercial FEM based analysis program: ANSYS 19 (https://www.ansys.com).
Song et al. (2021), have introduced their work for a spectrum analysis of PA signal based on COMSOL. Their study has utilized COMSOL in studying the relevance between the spectral characteristics of the PA signal and the properties of the absorber, concluding that the spectral characteristics of the PA signal are very related to the size of the absorber (Song et al. 2021).
3 Methods
The proposed model is based on three modules as illustrated in the following framework presented in Fig. 2.
3.1 (A)—Pulsed laser irradiance on the tissue’s surface:
The first operation for the PA signal generation is the pulsed laser irradiance. The measure of laser light intensity, (also called: flux rate or irradiance), is in Joule per second per unit area or (W/m2). The deposited light energy rate per unit volume (lightning function) or the laser light source function is described in W/m3 which is equivalent to Kg. m−1. s−3 in the standard international system of units (SI system) (https://en.wikipedia.org/wiki/International_System_of_Units; Newell and Tiesinga 2019). The unit of W/m3 is the unified unit here for the deposited energy rate per unit volume through the whole model starting from the light energy input rate per unit volume in W/m3, to the deposited heat energy rate per unit volume in W/m3, and ending with the source term for the compact acoustic pressure wave equation for generation (from the deposited heat energy rate per unit volume) and propagation, which can be described as a pressure source generation rate in Pa/s which is equivalent to Kg. m−1. s−3 which is also leading to W/m3.
The input laser pulse can be modeled as a Gaussian (bell shape) signal with a pulse width τp in seconds and a maximum amplitude of Ipmax in W/m3 which represents the energy rate (joule/second) of the input laser pulse per unit volume. Figure 3 illustrates an example of the input laser pulse with τp ≈ 10 ns, that’s means that the full-width half maximum (FWHM) is about 10 ns, at pulse center t0 = 30 ns. The peak value of the pulse was normalized to one and multiplied by the maximum value of the input light signal’s power Ipmax = 400,000 W/m3 (Ipmax = 400 mW/cm3) as shown in Fig. 3.
The analytical input laser pulse (for example the curve shown in Fig. 3) utilized to irradiate a biological tissue surface at a position r (x, y, z) can be described mathematically as:
where:
\(\mathrm{S }(\mathrm{r},\mathrm{t})\): represents the input light pulse of laser irradiance’s energy per unit volume per unit time at location r (x, y, z) and at time t (s), it will be the source term directly W/m3 for the light irradiance diffusion equation in the next step in (B).
\(\mathrm{Ipmax}\): is representing the peak value of the input laser pulse S (r, t), here in Fig. 3, Ipmax = 400,000 W/m3 (i.e.: Ipmax = 400 mW/cm3).
t0: is representing the center time value of the laser input pulse shape, here in Fig. 3: t0 = 30 ns.
τp: represents the pulse width, where: τp ≈ FWHM = \(2\upsigma \sqrt{2ln2 } \approx 2.355\upsigma\); where: σ is representing the standard deviation of the signal [016], as shown in Fig. 2 (τp \(\approx\) 10 ns).
In (1), we utilized a peak value normalization for the Gaussian bell shape signal so that the peak of the input laser pulse is equal to one multiplied by the maximum power for the signal per unit volume (W/m3) as assumed here in this model to be Ipmax = 1 * 400 mW/cm3. For obtaining an integral normalization for the Gaussian distribution, the term (Ipmax) should be equal to (1/ σ \(\sqrt{2\pi } )\) multiplied by a value related to the signal power or energy to obtain a complete term representing the peak value for the pulse signal (COMSOL Multiphysics Reference Manual 2023). The (1/ σ\(\sqrt{2\pi }\)) term is only used to make the total area under the pdf curve equal to one (Smith 1997–1999).
A detailed explanation of deriving Eq. (1) is found in: Appendix-A.
3.2 (B)—Diffusion of light through biological tissues:
Modeling light interaction with biological tissues, an optically complex scattering media (Cheng et al. 2023), has different scientific theories, assumptions, and techniques. Some of these are modeling the light as a function in diffusion distance only and are not concerned with the time distribution of the light pulse irradiance (time-independent) as Beer-Lambert law (https://en.wikipedia.org/wiki/Beer-Lambert_law; https://www.comsol.com/blogs/modeling-laser-material-interactions-with-the-beer-lambert-law/; Ishimaru 2017) and Helmholtz equation (https://en.wikipedia.org/wiki/Helmholtz_equation; Goodman 1996; https://www.atomic.physics.lu.se/fileadmin/atomfysik/Biophotonics/Education/MultiphysicsExercise.pdf), such that stationary studies are suitable into the frequency domain and steady-state studies only. Some others are time-dependent such as the basic time-varying diffusion equation (Ishimaru 1978; Morse and Feshbach 1953; Star 2011), which is originally derived based on approximating the basic equation of transfer or the basic radiative transfer equation (RTE) (Ishimaru 1978). The origin of the RTE returns to the basic radiative transfer theory (RTT) or transport theory which was initiated by Schuster (1905). The RTE (Ishimaru 1978; Manning 1989) is equivalent to the Maxwell–Boltzmann collision equation (Sommerfeld 1956) or Boltzmann’s equation utilized in the kinetic theory of gases and neutron transport theory (Williams 1971).
The RTE is difficult to solve since it has more independent variables, so the RTE is commonly simplified in the diffusion approximation assuming that the radiance in a high-albedo (\({{\varvec{\mu}}}_{{\varvec{a}}}\ll {{\varvec{\mu}}}_{{\varvec{s}}}^{\mathrm{^{\prime}}}\); i.e., the absorption is very less than the scattering) scattering medium is almost isotropic after sufficient scattering (Wang and Hsin-i 2007b).
In our study, the following time-dependent diffusion Eq. (2), concluded and deduced from Wang et al. 2012c; Liu et al. 2018; Morse and Feshbach 1953; Star 2011; Ishimaru 1978; Wang and Hsin-i 2007b; Arridge 1999; Arridge et al. 2011), has been utilized to describe exactly the light fluence rate \(\mathbf{\varphi }\left(\mathbf{r},\mathbf{t}\right)\) (Named also: the light flux rate or the irradiance or the light intensity) of the incident light pulse beam exactly not only at each location r but also at each time \(\mathbf{t}\) in W/m2.
where:
n is the refractive index of the medium.
C is the light velocity in vacuum = 3 × 108 m/s.
\({\upmu }_{\mathrm{a}}\) is the absorption coefficient for the medium in 1/m at a certain wavelength.
\({\upmu }_{\mathrm{s}}\) is the scattering coefficient for the medium in 1/m at a certain wavelength.
\({\mu }_{s}^{\prime}\) is the reduced scattering coefficient for the medium in 1/m at a certain wavelength.
D is the diffusion coefficient [in m]; D = \(\frac{1}{3\left({\mu }_{a}+{\mu }_{s}{\prime}\right)}\);\({\mu }_{s}{\prime}=(1-\mathrm{g }){\mu }_{s}\); g is anisotropy coefficient. The anisotropy factor g is the average of the cosine value of the deflection angles [048, 10], so it characterizes the average amount of scattering in a medium (Jacques and Wang 1995), ranges from − 1 (backwardly peaked scattering) via 0 (isotropic scattering) to 1 (forwardly peaked scattering) (Wang et al. 2012b). The meaning of isotropy of a medium is that its properties are independent of the direction of the light wave’s polarization i.e., the direction of the electric and magnetic fields vectors (Goodman 1996). The anisotropy coefficient g, an important optical property of biomedical tissues (Jacques 1996, 2013; Bashkatov et al. 2011), is the parameter that determines the asymmetry of the well-known scattering phase function utilized in examining the anisotropy’s influence in light scattering (Peters et al. 1990), originally stated by Henyey and Greenstein (Henyey and Greenstein 1941) (H-G function) for galactic scattering, and verified for single scattering by Jacques et al. with only a slight modification (Jacques et al. 1987).
\(\mathrm{\varphi }\left(\mathrm{r},\mathrm{t}\right)\) is the Light Intensity/Flux rate/ Irradiance/Fluence rate in W/m2. Where: r denotes the location and t is representing time. \(\mathrm{\varphi }\left(\mathrm{r},\mathrm{t}\right)\) is the solution for Eq. (2) and it represents the light energy diffusion through the tissue media per unit time per unit area).
\(\nabla\) is “del” or “napla” differential operator representing the gradient (grad), \(\nabla\) = \(\frac{\partial }{\partial x} i+ \frac{\partial }{\partial y} j+ \frac{\partial }{\partial z} k\),where: i, j, k are unit vectors along x, y, z, respectively (Schey 2005; Kreyszig 2011).
\(\nabla\). is the divergence “div”, for a function [f (x, y, z)]: \(\nabla\). f = (\(\frac{\partial }{\partial x} {f}_{x}+ \frac{\partial }{\partial y} {f}_{y}+ \frac{\partial }{\partial z} {f}_{z}\)Schey 2005).
3.3 (C)—Acoustic pressure wave generation and propagation
The basic idea behind the photoacoustic wave generation and propagation as illustrated in Fig. (3), is three energy forms’ exchange (Two transformations of energies) in the target (light to heat to kinetic) to obtain the final acoustic pressure wave generation and propagation which can be induced with ultrasonic transducers (GadAllah et al. 2022).
To model the two-energy exchanges illustrated before in Fig. 1, there are two steps have been implemented as follows:
3.3.1 From Light energy to heat or thermal energy:
The solution of (2) is \(\mathbf{\varphi }\left(\mathbf{r},\mathbf{t}\right)\): a lightening function representing the light energy per unit time per unit area in W/m2 (at a location r and at a time t). To model the transfer operation from light energy to thermal energy, we will utilize the following equation (Cox and Beard 2009; Wang et al. 2012a; Chandramoorthi and Thittai 2017):
where;
\(H\left(r,t\right)\) represents the heating function induced due to the irradiance from the pulsed laser beam. \(H\left(r,t\right)\) is equivalent to the thermal energy deposited per unit time per unit volume in W/m3 (at a location r and at a time t through the tissue).
\({\mu }_{at}\) is representing the absorption coefficient for the target tissue in m.−1
Note: if the target tissue you need to image is the same tissue that the laser pulse irradiated on its surface, in that case only: \({\mu }_{at}\) will be equal to \({\mu }_{a}\) mentioned in the previous Eq. (2). Otherwise \({\mu }_{at}\) is equal to the absorption coefficient for the target tissue in m−1.
\(Y\) is representing the yield. In other words: it represents the ratio of the deposited light energy that has been converted into thermal energy (Wang et al. 2012a). Here it is assumed that Y = 1 for simplification as in Cox and Beard (2009); Chandramoorthi and Thittai 2017).
3.3.2 From thermal energy to kinetic energy or ultrasound pressure wave (PA wave):
The ultrasound pressure wave (P) resulting from the energy exchange processes due to the photoacoustic phenomena is a function both in location r and time t ( \(P= P\left(r,t\right)\)). The common photoacoustic equation describing the photoacoustic wave generation and propagation in an inviscid medium as biological tissue is (Wang 2008; Zhou et al. 2016; Cox and Beard 2009; Wang et al. 2012a, 2017; Diebold et al. 1990 Oct 5; Wang and Anastasio 2011; Westervelt and Larson 1973; Diebold 2009; Sigrist 1986):
where;
\({v}_{s}\) Is the speed of sound in the target biological tissue (m/s); \({v}_{s}= \sqrt{\frac{1}{\rho k }}\); where: \(\rho \, and \, k,\) are representing the density (in: Kg/m3) and the compressibility (in: Pa−1), respectively (Morse and Uno Ingard 1968).
\({\nabla }^{2}\) is the Laplacian operator, also may be noted as: “\(\Delta\)”, it is equivalent to the divergence \(\nabla\). of the gradient \(\nabla ,\) for a function f (x, y, z): \({\nabla }^{2} f=\Delta f= \nabla .(\nabla f)\) = (\(\frac{{\partial }^{2}}{\partial {x}^{2}} f+ \frac{{\partial }^{2}}{\partial {x}^{2}} f+ \frac{{\partial }^{2}}{\partial {x}^{2}} f\)Schey 2005; Kreyszig 2011).
\(\beta\) is the thermal coefficient of volume expansion for the target biological tissue (K−1).
\({C}_{P}\) is the specific heat capacity at constant pressure for the target biological tissue (J/ Kg· K).
Note 1: the three variables \({v}_{s}^{2}, \beta , {C}_{P}\) mentioned in Eq. (4) are characteristic variables for each biological tissue, and the three are forming the Gruneisen parameter \( {\varvec{\Gamma}}\) (Gamma), where: \(\Gamma = \frac{\beta }{{C}_{P}} {v}_{s}^{2}\). The Gruneisen parameter \( {\varvec{\Gamma}}\) is a dimensionless, temperature-dependent factor proportional to the fraction of thermal energy converted into mechanical stress (Oraevsky and Karabutov 2003; Oraevsky et al. 1882; Shah et al. 2008; Gusev and Karabutov 1993; Oraevsky et al. 1997). Hence, the Grueneisen parameter is a temperature-dependent factor (due to the velocity of sound and the volume expansion coefficient), thus the photoacoustic signal P (r, t) is directly related to temperature (Shah et al. 2008).
Note 2: if the right-hand side of (4), the source term, is equaled to zero, the equation is returned to the familiar three dimensions, linear, lossless, and homogeneous acoustic wave propagation equation (Morse and Uno Ingard 1968; Kinsler et al. 2000). That may happen if the heating function \(H\left(r,t\right)\) is constant (time invariant), so that its first-time derivative \(\frac{\partial H(r, t)}{\partial t}\) will be equal zero. So, time-invariant heating doesn’t turn out acoustic wave (Wang 2008).
Equation (4) can be rearranged in terms of \( {\varvec{\Gamma}}\) as follow (Cox and Beard 2009; Ammari et al. 2010):
Finally: From (3) and (4) and assuming Y = 1, then:
Now, the complete mathematical model has been built and can be concluded in the following Fig. 4:
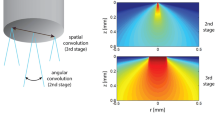
4 Numerical simulation by COMSOL multiphysics
A numerical simulation model is introduced here for applying the proposed developed mathematical model in simulating the generation and propagation of a breast cancer’s PA signal stimulated by pulsed laser irradiation. In this model: COMSOL Multiphysics (https://www.comsol.com), a numerical simulation software based on the finite element method (FEM) (Logan 2023; Zienkiewicz et al. 2005; Reddy 2019), has been utilized for applying numerical modeling of the proposed mathematical model shown in Fig. 4 to simulate the generation and propagation of the PA signal generated from a point inside a simulated breast cancer by a sphere (100 µm in diameter) inherent in a simulated biological tissue (represented by a cylinder measuring 1 mm in diameter and height) as illustrated in Fig. 5.
The simulation model geometry for the illustrative example to verify the application of the proposed developed mathematical model presented in Fig. 4. Where: P1:(0,0,0.5): the laser irradiance point source on the surface of the tissue, P2:(0,0,0.4): a point inside the tumor, P3: (0,0,0): a point away from the tumor and is about 0.5mm away from P1
Table 1 presents the definitions of the parameters utilized in the model. The majority of numerical simulation parameter values used are largely compatible with the laser wavelengths in the near-infrared region (NIR) as extracted from reference sources (Metwally et al. 2014) and (Chandramoorthi and Thittai 2017). The references of the parameters' values are listed in the right column notes, while any unmentioned references imply that the values were added by the authors.
A clarification tutorial for programming the proposed mathematical model on COMSOL is mentioned in Appendix-B.
The proposed COMSOL-based numerical simulation program (a COMSOL application file ) is attached as a supplementary material.
5 Qualitative and analytical results
In Fig. 6, six slices are presented to depict the spatial distribution of the PA pressure signal. The different shapes of the PA signal propagation are shown at six different time snapshots: 30, 40, 50, 60, 80, and 100 ns.
In the following Fig. 7, the simulated laser light intensity’s distribution \(\mathbf{\varphi }\left(\mathbf{r},\mathbf{t}\right)\) in W/m2 along time is demonstrated from (0–150) ns for a three sample measuring points: P1, P2, and P3 showing the difference in amplitude of each point making a sense that the diffused flux is decreasing by increasing the measuring depth.
Figure 8 displays the distribution of the induced PA signal over time for the three points, P1, P2, and P3, from (0–150) ns. This graph illustrates the difference in amplitude for each point, indicating that the major pressure originated from the simulated tumor at P2, with the highest amplitude. On the other hand, the pressure at P1 on the surface decreased due to attenuation from the simulated breast tissue. Figure 9 presents the frequency spectrum distribution for the three output PA signals shown in Fig. 8. The output spectrum for the three points ranges from less than 100 MHz.
Frequency spectrum of the three samples from output photoacoustic pressure signal solution \(\mathbf{P}\left(\mathbf{r},\mathbf{t}\right)\) shown in Fig. 8
In Fig. 10, a trial is presented that explores both light and acoustic signals at a specific point within a simulated tumor. This is particularly helpful for new researchers who want to simulate the real production of the PA signal with pulsed laser irradiation. Figure 11 displays the frequency spectrum of Fig. 10.
comparing the light intensity diffusion \(\mathbf{\varphi }\left(\mathbf{r},\mathbf{t}\right)\) simultaneously vs the photoacoustic pressure generation and propagation \(\mathbf{P}\left(\mathbf{r},\mathbf{t}\right)\), inside the target tumor model at r = P2 (illustrated in Fig. 5), and t: from (0–150) ns
comparing the frequency spectrum for the light intensity diffusion \(\mathbf{\varphi }\left(\mathbf{r},\mathbf{t}\right)\) vs the frequency spectrum of the photoacoustic pressure generation and propagation \(\mathbf{P}\left(\mathbf{r},\mathbf{t}\right)\), inside the target tumor model at r = P2 (illustrated into Fig. 5) into one graph
6 Conclusion
A mathematical model has been created using information from previous research on photoacoustic (PA) imaging to simulate how PA signals are generated and travel through biological tissues. The model was examined using a time-dependent study in COMSOL Multiphysics, a simulation platform. The results of this simulation can be used to understand better PA signal generation and propagation in a virtual environment, which can assist with both in-vitro and in-vivo studies. The study's analytical and theoretical findings confirm that the proposed mathematical model is valid for the numerical simulation of biomedical PA signals using platforms such as COMSOL Multiphysics. This research will be beneficial for researchers who are new to studying, modeling, and simulating different biomedical photoacoustic algorithms, prototypes, and systems.
Availability of supporting data and materials
All data generated or analyzed during this study are included in this published articl and its supplementary material file.
Abbreviations
- PA:
-
Photoacoustic
- FEM:
-
Finite element method
- PAI:
-
Photoacoustic imaging
- OAI:
-
Optoacoustic imaging
- TAI:
-
Thermoacoustic imaging
- OCT:
-
Optical coherence tomography
- PAT:
-
Photoacoustic tomography
- MSOT:
-
Multispectral optoacoustic tomography
- LED:
-
Light emitting diode
- OD-PAT:
-
Optical detection PAT
- NC-LUS:
-
Non-contact laser ultrasound
- PAM:
-
Photoacoustic microscopy
- OR-PAM:
-
Optical resolution photoacoustic microscopy
- AR-PAM:
-
Acoustic resolution photoacoustic microscopy
- RSOM:
-
Raster-scan optoacoustic mesoscopy
- LD-PAM:
-
LED based PAM
- PATER:
-
PA topography through an ergodic relay
- PAE:
-
Photoacoustic elastography
- IGS:
-
Image-guided surgery
- HIFU:
-
High intensity focused ultrasound
- RF:
-
Radiofrequency
- MW:
-
Microwave
- ROI:
-
Region of interest
- FFT:
-
Fast Fourier transform
- FBP:
-
Filtered back projection
- SA:
-
Synthetic aperture
- SI system:
-
Standard international system of units
- HM:
-
Half maximum
- FWHM:
-
Full width at half maximum
- RTE:
-
Radiative transfer equation
- RTT:
-
Radiative transfer theory
- PDE:
-
Partial differential equation
- NIR:
-
Near-InfraRed
References
Aliroteh, M., Nan, H., Arbabian, A.: Microwave-induced thermoacoustic tomography for subcutaneous vascular imaging. In: 2016 IEEE International Ultrasonics Symposium (IUS), Tours, France (2016). https://doi.org/10.1109/ULTSYM.2016.7728643
Ammari, H., Bossy, E., Jugnon, V., Kang, H.: Mathematical modeling in photoacoustic imaging of small absorbers. SIAM Rev. 52(4), 677–695 (2010). https://doi.org/10.1137/090748494
Arridge, S.R.: Optical tomography in medical imaging. Inverse Prob. 15, R41–R93 (1999). https://doi.org/10.1088/0266-5611/15/2/022
Arridge, S.R., Kaipio, J.P., Kolehmainen, V., Tarvainen, T.: Optical imaging. Ch. 17. In: Handbook of Mathematical Methods in Imaging, Edited by: O. Scherzer, ISBN: 9780387929194, Online ISBN: 9780387929200, Springer (2011). https://doi.org/10.1007/978-0-387-92920-0_17
Attia, A.B.E., Balasundaram, G., Moothanchery, M., Dinish, U.S., Bi, R., Ntziachristos, V., Olivo, M.: A review of clinical photoacoustic imaging: current and future trends. Photoacoustics (2019). https://doi.org/10.1016/j.pacs.2019.100144
Ayana, G., Park, J., Jeong, J.-W., Choe, S.-W.: A novel multistage transfer learning for ultrasound breast cancer image classification. Diagnostics 12, 135 (2022). https://doi.org/10.3390/diagnostics12010135
Badawy, S.M., Mohamed, A.A., Hefnawy, A.A., Zidan, H.E., GadAllah, M.T., El-Banby, G.M.: Automatic semantic segmentation of breast tumors in ultrasound images based on combining fuzzy logic and deep learning—a feasibility study. PLoS ONE 16(5), 0251899 (2021a). https://doi.org/10.1371/journal.pone.0251899
Badawy, S.M., Mohamed, A.A., Hefnawy, A.A., Zidan, H.E., GadAllah, M.T., El-Banby, G.M.: Classification of breast ultrasound images based on convolutional neural networks — a comparative study. In: The 2021 International Telecommunications Conference (ITC-Egypt’2021) (2021). https://doi.org/10.1109/ITC-Egypt52936.2021.9513972
Bai, J.W., Qiu, S.Q., Zhang, G.J.: Molecular and functional imaging in cancer-targeted therapy: current applications and future directions. Sig. Transduct. Target Ther. 8, 89 (2023). https://doi.org/10.1038/s41392-023-01366-y
Bashkatov, A.N., Genina, E.A., Tuchin, V.V.: Optical properties of skin, subcutaneous, and muscle tissues: a review. J. Innov. Opt. Health Sci. 4(1), 9–38 (2011). https://doi.org/10.1142/S1793545811001319
Beard, P.: Biomedical photoacoustic imaging. Interface Focus 1, 602–631 (2011). https://doi.org/10.1098/rsfs.2011.0028
Bell, A.G.: On the production and reproduction of sound by light. Am. J. Sci. 20, 305–324 (1880). https://doi.org/10.2475/ajs.s3-20.118.305
Bell, A.G.: LXVIII Upon the production of sound by radiant energy. Lond. Edinb. Dublin Philos. Mag. J. Sci. 11(71), 510–528 (1881). https://doi.org/10.1080/14786448108627053
Burckhardt, C.B.: Speckle in ultrasound B-mode scans. IEEE Trans. Son. Ultrason. (1978). https://doi.org/10.1109/T-SU.1978.30978
COMSOL Multiphysics Reference Manual (5.5). https://doc.comsol.com/5.5/doc/com.comsol.help.comsol/COMSOL_ReferenceManual.pdf. Last Seen in: 25 Jan. 2023
Cao, R., Zhao, J., Li, L., et al.: Optical-resolution photoacoustic microscopy with a needle-shaped beam. Nat. Photon. 17, 89–95 (2023). https://doi.org/10.1038/s41566-022-01112-w
Chandramoorthi, S., Thittai, A.K.: Simulation of photoacoustic tomography (PAT) system in COMSOL and comparison of two popular reconstruction techniques. In: Proc SPIE 10137, medical imaging 2017: biomedical applications in molecular, structural, and functional imaging, 101371O (2017). https://doi.org/10.1117/12.2254450
Chandramoorthi, S., Thittai, A. K.: Ultrasound receive-side strategies for image quality enhancement in low-energy illumination based photoacoustic imaging. A Book Chapter in: Singh, M.K.A.: LED-Based Photoacoustic Imaging: From Bench to Bedside. Springer, pp. 79–112 (2020). https://doi.org/10.1007/978-981-15-3984-8_4
Chen, S.-L., Tian, C.: Recent developments in photoacoustic imaging and sensing for nondestructive testing and evaluation Ind. Biomed. Art. Visual Comput. (2021). https://doi.org/10.1186/s42492-021-00073-1
Chen, Y.-S., Yeager, D., Emelianov, S. Y.: Photoacoustic imaging for cancer diagnosis and therapy guidance, Ch.: 9. In: Chen, X., Wong, S.: Cancer Theranostics. Academic Press. ISBN: 9780124078840 (2014). https://doi.org/10.1016/B978-0-12-407722-5.00009-8, pp. 139–159
Cheng, Z., Li, C., Khadria, A., et al.: High-gain and high-speed wavefront shaping through scattering media. Nat. Photon. (2023). https://doi.org/10.1038/s41566-022-01142-4
Chu, B., Chen, Z., et al.: Fluorescence, ultrasonic and photoacoustic imaging for analysis and diagnosis of diseases. Chem. Commun. 59, 2399–2412 (2023). https://doi.org/10.1039/D2CC06654H
Cox, B.T., Laufer, J., Kostli, K., Beard, P.: Experimental validation of photoacoustic k-space propagation models. In Proc. SPIE 5320, Photons Plus Ultrasound: Imaging and Sensing, (2004). https://doi.org/10.1117/12.531178
Cox, B.T., Beard, P.C.: “Fast calculation of pulsed photoacoustic fields in fluids using k-space methods. J. Acoust. Soc. Am. 117(6), 3616–3627 (2005). https://doi.org/10.1121/1.1920227
Cox, B., Beard, P.C.: Modeling photoacoustic propagation in tissue using k-space techniques, Ch. 3. In L.V.Wang (eds.): Photoacoustic Imaging and Spectroscopy. ISBN: 9781420059915, CRC Press, Taylor & Francis Group (2009)
Dickinson, R.J., Nassiri, D.K.: Reflection and scattering, Ch. 6. In: Hill, C.R., Bamber, J.C., ter Haar, G.R. Physical Principles of Medical Ultrasonics (2nd Edn). ISBN:9780471970026, Online ISBN: 9780470093979, Wiley (2004). https://doi.org/10.1002/0470093978.ch6
Diebold, G.J., Khan, M.I., Park, S.M.: Photoacoustic “signatures” of particulate matter: optical production of acoustic monopole radiation. Science 250(4977), 101–104 (1990). https://doi.org/10.1126/science.250.4977.101
Diebold, G.J.: Photoacoustic monopole radiation: waves from objects with symmetry in one, two, and three dimensions, Ch. 1. In: Wang, L.V.: Photoacoustic Imaging and Spectroscopy. ISBN: 9781420059915, CRC Press, Taylor & Francis Group (2009)
Dong, B., Sun, C., Zhang, H.F.: Optical detection of ultrasound in photoacoustic imaging. IEEE Trans. Biomed. Eng. (2017). https://doi.org/10.1109/TBME.2016.2605451
Duck, F.A.: Physical Properties of Tissue: A Comprehensive Reference Book (Ch.: 2, Ch.: 3, and Ch.: 4). ISBN: 0122228006, Academic Press Limited (1990).
Ecclestone, B.R., Bell, K., Sparkes, S., et al.: Label-free complete absorption microscopy using second generation photoacoustic remote sensing. Sci. Rep. 12, 8464 (2022). https://doi.org/10.1038/s41598-022-11235-3
El-Gohary, S.H., Metwally, M.K., Eom, S., Jeon, S.H., Byun, K.M., Kim, T.S.: Design study on photoacoustic probe to detect prostate cancer using 3D Monte Carlo simulation and finite element method. Biomed. Eng. Lett. 4, 250–257 (2014). https://doi.org/10.1007/s13534-014-0150-2
ElGohary, S.H., Azab, S.A., Metwally, M.K., Hassan, N.S.: Numerical computational study of photoacoustic signals from eye models to detect diabetic retinopathy. Open Biomed. Eng. J. 14, 11–19 (2020). https://doi.org/10.2174/1874120702014010011
Fercher, A.F.: Optical coherence tomography. J. Biomed. Opt. 1(2), 157–173 (1996). https://doi.org/10.1117/12.231361
GadAllah, M.T., Mohamed, A.E.-N.A., Hefnawy, A.A., Zidan, H.E., El-Banby, G.M., Badawy, S.M.: Photoacoustic Imaging in Medicine: A Review. Mansoura Eng. J., 47(2), 17–31, 2022. https://doi.org/10.21608/bfemu.2022.233516
GadAllah, M.T.: Ultrasound quantitative tissue characterization by wavelet. A Thesis Submitted for fulfillment of the Degree of Master in Electronic Engineering, Under supervision of: “Prof. Dr. Mohammed Mabrouk Sharaf, Dr. Samir Mohamed Badawy”, Control Systems and Measurements Engineering Department, Faculty of Electronic Engineering (FEE), Menoufia University, Egypt (2015)
Gerling, M., Zhao, Y., Nania, S., Norberg, K.J., Verbeke, C.S., Englert, B., Kuiper, R.V., Bergström, A., Hassan, M., Neesse, A., Löhr, J.M., Heuchel, R.L.: Real-time assessment of tissue hypoxia in vivo with combined photoacoustics and high-frequency ultrasound. Theranostics 4(6), 604–613 (2014). https://doi.org/10.7150/thno.7996
Goodman, J.W.: Introduction to Fourier Optics, 2 Edn. Ch.: 3. ISBN: 0-07-024254-2, McGraw-Hill Companies Inc. (1996)
Grahn, P.: Thermoacoustics modeling of loudspeakers with COMSOL Multiphysics. Corpus ID: 140112166 (2015). https://www.akustinenseura.fi/wp-content/uploads/2015/09/AP2015_Paperin_palautus_34.pdfAccessed: 15th March 2023
Grahn, P.: Photoacoustics modeling with COMSOL Multiphysics. Corpus ID: 221965890, (2017). https://www.akustinenseura.fi/wp-content/uploads/2017/08/akustiikkapaivat_2017_s335.pdfAccessed: 15th March 2023
Guo, Z., Li, Li., Wang, L.V.: On the speckle-free nature of photoacoustic tomography. Med. Phys. 36, 9 (2009). https://doi.org/10.1118/1.3187231
Gusev, V.E., Karabutov, A.A.: Laser optoacoustics. Ch: Introduction, pp: xiv, Translated by: Kevin Hendzel. ISBN: 1563960362, ISBN-13: 9781563960369. AIP Press, 1993
Hai, P., Yao, J., Li, G., Li, C., Wang, L.V.: Photoacoustic elastography. Opt. Lett. 41(4), 725–728 (2016a). https://doi.org/10.1364/OL.41.000725
Hai, P., Zhou, Y., Gong, L., Wang, L.V.: Quantitative photoacoustic elastography in humans. J. Biomed. Opt. 21(6), 066011 (2016b). https://doi.org/10.1117/1.JBO.21.6.066011
Haupt, R., Zhang, X., Fincke, J., Richardson, J., Hughes, J., Anthony, B., Samir, A.: Non-contact laser ultrasound (N-CLUS) system for medical imaging and elastography. In: 2019 IEEE International Ultrasonics Symposium (IUS), Glasgow, UK. (2019). https://doi.org/10.1109/ULTSYM.2019.8925569
Hendon, C.P., Rollins, A.M.: Real-time imaging of microstructure and function using optical coherence tomography, Ch.: 7. In: Handbook of Optical Biomedical Diagnostics, 2 Edition, Volume 2: Methods, edited by: V. V. Tuchin, ISBN: 9781628419139, PDF-ISBN: 9781628419122, SPIE (2016). https://doi.org/10.1117/3.2219608
Henyey, L.G., Greenstein, J.L.: Diffuse radiation in the galaxy. Astrophys. J. 93, 70–83 (1941). https://doi.org/10.1086/144246
https://en.wikipedia.org/wiki/Beer-Lambert_law. Accessed 17th March 2023
https://www.ansys.com. Accessed 15th march 2023
https://www.comsol.com/blogs/modeling-laser-material-interactions-with-the-beer-lambert-law/. Accessed 17th March 2023
https://www.comsol.com. Accessed 16th March 2023
https://www.mathworks.com/products/matlab.html. Accessed in 15th march 2023
Huang, D., et al.: Optical coherence tomography. Science 254(5035), 1178–1181 (1991). https://doi.org/10.1126/science.1957169
Hui, J., Cheng, J.-X.: Intravascular photoacoustic imaging of lipid-laden plaques: from fundamental concept toward clinical translation, Ch.: 4. In: Zhou, Q., Chen, Z. (eds.) Multimodality Imaging for Intravascular Application. eBook ISBN: 978-981-10-6307-7, Springer, Singapore (2019). https://doi.org/10.1007/978-981-10-6307-7_4
Ishimaru, A.: Diffusion of a pulse in densely distributed scatterers. J. Opt. Soc. Am. 68(8), 1045–1050 (1978). https://doi.org/10.1364/JOSA.68.001045
Ishimaru, A.: Wave propagation and scattering in random media, Vol 1: Single Scattering and Transport Theory”, [Ch. 9: Diffusion Approximation”, and Ch. 7: “Transport Theory of Wave Propagation in Random Particles”], ISBN: 0123747015, Academic Press (1978)
Ishimaru, A.: Electromagnetic wave propagation, radiation, and scattering: from fundamentals to applications, Ch. 20. In: 2nd Edn Biomedical Em, Optics, and Ultrasound, ISBN: 9781118098813, Online ISBN: 9781119079699, IEEE Press Series on Electromagnetic Wave Theory, IEEE Press, Wiley (2017). https://doi.org/10.1002/9781119079699.ch20
Jacques, S.L.: Optical properties of biological tissues: a review. Phys. Med. Biol. 58(11), R37–R61 (2013). https://doi.org/10.1088/0031-9155/58/11/r37
Jacques, S.L., Alter, C.A., Prahl, S.A.: Angular dependence of HeNe laser light scattering by human dermis. Lasers Life Sci. 1(4), 309–333 (1987)
Jacques, S.L.: Origins of tissue optical properties in the UVA, visible, and nir regions, Advances in Optical Imaging and Photon Migration, Technical Digest Series (Optica Publishing Group), paper OPC364 (1996). https://doi.org/10.1364/AOIPM.1996.OPC364
Jacques, S.L., Wang, L.: Monte Carlo modeling of light transport in tissues, Chapter 4 In: Welch, A.J., van Gemert, M.J.C. (eds) Optical-thermal response of laser-irradiated tissue, 1st Ed., Plenum Press, e-ISBN: 978-1-4757-6092-7, Springer, Boston (1995). https://doi.org/10.1007/978-1-4757-6092-7_4
Joseph, W.: Goodman, “speckle: Friend or foe?” AIP Conf. Proc. 1537, 5–7 (2013). https://doi.org/10.1063/1.4809685
Kellnberger, S.: thermoacoustic imaging in time and frequency domain. Theory and experiments, Engineering PhD Dissertation, Department of Electrical and Computer Engineering, Technical University of Munich (TUM) (2013). https://mediatum.ub.tum.de/doc/1113396/1113396.pdf.Accessed: 5th March 2023
Kinsler, L.E., Frey, A.R., Coppens, A.B., Sanders, J.V.: Fundamentals of acoustics, 4th Edn., Ch. 5: The Acoustic Wave Equation and Simple Solutions, ISBN: 9780471847892, Wiley (2000)
Kreyszig, E.: Advanced engineering mathematics, 10th Edn., by: E. Kreyszig, in collaboration with: Herbert Kreyszig, and Edward J. Norminton, Ch. 9: Vector Differential Calculus. Grad, Div, Curl, pp. 354–412, ISBN: 9780470458365, e-ISBN: 9780470913611, Wiley (2011)
Lapierre-Landry, M., Carroll, J., Skala, M.C.: Imaging retinal melanin: a review of current technologies. J. Biol. Eng. 12, 29 (2018). https://doi.org/10.1186/s13036-018-0124-5
Li, Y., Li, L., et al.: Snapshot photoacoustic topography through an ergodic relay for high-throughput imaging of optical absorption. Nat. Photonics 14, 164–170 (2020). https://doi.org/10.1038/s41566-019-0576-2
Li, X., Tsang, V.T.C., Kang, L., Zhang, Y., Wong, T.T.W.: High-speed high-resolution laser diode based photoacoustic microscopy for in vivo microvasculature imaging. Visual Comput Ind Biomed Art (2021). https://doi.org/10.1186/s42492-020-00067-5
Liang, Y., Fu, W., Li, Q., et al.: Optical-resolution functional gastrointestinal photoacoustic endoscopy based on optical heterodyne detection of ultrasound. Nat. Commun. 13, 7604 (2022). https://doi.org/10.1038/s41467-022-35259-5
Light propagation modelling using COMSOL Multiphysics. Last Seen 25 Jan 2023. https://www.atomic.physics.lu.se/fileadmin/atomfysik/Biophotonics/Education/MultiphysicsExercise.pdf
Lin, L., Tong, X., Cavallero, S., et al.: Non-invasive photoacoustic computed tomography of rat heart anatomy and function. Light Sci. Appl. 12, 12 (2023). https://doi.org/10.1038/s41377-022-01053-7
Liu, Y.-H., Xu, Y., Liao, L.-D., Chan, K.C., Thakor, N.V.: A handheld real-time photoacoustic imaging system for animal neurological disease models: from simulation to realization. Sensors. 18(11), 4081 (2018). https://doi.org/10.3390/s18114081
Liu, W., Zhang, H.F.: Photoacoustic imaging of the eye: a mini review. Photoacoustics 4(3), 112–123 (2016). https://doi.org/10.1016/j.pacs.2016.05.001
Logan, D.L.: A First Course in the Finite Element Method, Enhanced 6th Edn, SI Version. Ch.: 1, ISBN: 978-0-357-67643-1, © 2023 Cengage Learning Inc. (2022)
Manning, R.M.: Radiative transfer theory for inhomogeneous media with random extinction and scattering coefficients. J. Math. Phys. 30(10), 2432–2440 (1989). https://doi.org/10.1063/1.528520
Metwally, M.K., El-Gohary, S.H., Byun, K.M., Han, S.M., Lee, S.Y., Cho, M.H., Khang, G., Cho, J., Kim, T.-S.: Influence of optical fluence distribution on photoacoustic imaging. International Science Index Vol: 8 No: 8 Part IX, Pp. 1201–1205, 16th International Conference on Biomedical Engineering at: Istanbul, Turkey, ICBE 2014. http://mesl.khu.ac.kr/research/paper/icbe14.pdf. Accessed in: 23 Feb. 2023
Metwally, M.K., EI-Gohary, S.H., Ran, S.M., Byun, K.M., Kim, T.-S.: Influence of the anisotropic mechanical properties of the breast cancer on photoacoustic imaging. In: 2014 7th Cairo International Biomedical Engineering Conference Cairo, Egypt, December 11–13 (2014). https://doi.org/10.1109/CIBEC.2014.7020958
Mohamed, E.A., Gaber, T., Karam, O., Rashed, E.A.: A Novel CNN pooling layer for breast cancer segmentation and classification from thermograms. PLoS ONE 17(10), e0276523 (2022). https://doi.org/10.1371/journal.pone.0276523
Morse, P.M., Feshbach, H.: Methods of Theoretical Physics (Part I & Part II), Part I, Ch. 2: Equal ions Governing Fields, Section: 2.4: Diffusion and Other Percolative Fluid Motion, McGraw Hill Book Company (1953)
Morse, P.M., Ingard, K.U.: Theoretical acoustics, Ch 6: Acoustic Wave Motion, ISBN: 0691024014, ISBN-13: 9780691024011, McGraw-Hill, Inc. (1968)
Najarian, K., Splinter, R.: Biomedical signal and image processing. In: 2nd Edn., Ch. 16: Ultrasound Imaging. ISBN: 9781439870334, CRC Press, Taylor & Francis Group, 2012
Narayan, N.S. et al.: Speckle in ultrasound images: Friend or Foe?. In: IEEE International Conference on Image Processing (ICIP), pp. 5816–5820. (2014). https://doi.org/10.1109/ICIP.2014.7026176
Newell, D.B., Tiesinga, E.: The International System of Units (SI), National Institute of Standards and Technology (NIST), NIST Special Publication 330 (SP 330) 2019 Edn. https://doi.org/10.6028/NIST.SP.330-2019
Ntziachristos, V., Ripoll, J., Wang, L.V., Weissleder, R.: Looking and listening to light: the evolution of whole-body photonic imaging. Nat. Biotechnol. 23(11), 313–320 (2005). https://doi.org/10.1038/nbt1074
Nyayapathi, N., Xia, J.: Photoacoustic imaging of breast cancer: a mini review of system design and image features. J. Biomed. Opt. 24(12), 121911 (2019). https://doi.org/10.1117/1.jbo.24.12.121911
Oraevsky, A.A., Jacques, S.L., Tittel, F.K.: Measurement of tissue optical properties by time-resolved detection of laser-induced transient stress. Appl. Opt. 36(1), 402–415 (1997). https://doi.org/10.1364/AO.36.000402
Oraevsky, A.A., Karabutov, A.A.: Optoacoustic tomography, Ch: 34 in: Biomedical photonics handbook, Editor-in-Chief: Tuan Vo-Dinh, ISBN: 978–0849311161, CRC Press LLC (2003). http://library.nuft.edu.ua/ebook/file/Vo-Dinh2003.pdf.Accessed in: 23 Feb. 2023
Oraevsky, A.A., Jacques, S.L. Tittel, F.K.: Determination of tissue optical properties by piezoelectric detection of laser-induced stress waves. In: Proc. SPIE 1882, Laser-Tissue Interaction IV, (1993); https://doi.org/10.1117/12.147694
Oraevsky, A.A., Karabutov, A.A., Solomatin, S.V., Savateeva, E.V., Andreev, V.A., Gatalica, Z., Singh, H.: Declan Fleming, R.: Laser optoacoustic imaging of breast cancer in vivo, In: Proc. SPIE: 4256, Biomedical Optoacoustics II, (2001). https://doi.org/10.1117/12.429300
Park, S.J., et al.: Visualizing Alzheimer’s disease mouse brain with multispectral optoacoustic tomography using a fluorescent probe - CDnir7. Sci. Rep. 9, 12052 (2019). https://doi.org/10.1038/s41598-019-48329-4
Peters, V.G., Wyman, D.R., Patterson, M.S., Frank, G.L.: Optical properties of normal and diseased human breast tissues in the visible and near infrared. Phys. Med. Biol. 35(9), 1317–1334 (1990). https://doi.org/10.1088/0031-9155/35/9/010
Reddy, J.N.: Introduction to the Finite Element Method, Fourth Edn, (Ch.: 1), ISBN: 978-1-25-986191–8, MHID: 1-25-986191-0, McGraw-Hill Education (2019)
Schey, H.M.: Div, Grad, Curl, and All That: An Informal Text on Vector Calculus, 4th Edn, ISBN: 9780393925166, W. W. Norton & Company (2005)
Schuster, A.: Radiation through a Foggy atmosphere. Astrophys. J. 21, 1 (1905). https://doi.org/10.1086/141186
Shah, J., Park, S., Aglyamov, S.R., Larson, T., Ma, Li., Sokolov, K.V., Johnston, K.P., Milner, T.E., Emelianov, S.Y.: Photoacoustic imaging and temperature measurement for photothermal cancer therapy. J. Biomed. Opt. 13(3), 034024 (2008). https://doi.org/10.1117/1.2940362
Shung, K.K.: Diagnostic ultrasound imaging and blood flow measurements, 1st Edn, Ch. 4: Gray-Scale Ultrasonic Imaging, pp. 79–101, ISBN: 0824740963, ISBN-13: 9780824740962, eBook ISBN: 9780849338922, 9780429147449, CRC Press, Taylor & Francis Group, LLC (2006). https://doi.org/10.1201/9780849338922
Shung, M.B., Smith, B., Tsui, M.W.: Principles of medical imaging, Ch. 2: Ultrasound, pp. 78–161, ISBN: 0126409706, ISBN-13: 9780126409703, Academic Press Inc., Elsevier (1992). https://doi.org/10.1016/B978-0-12-640970-3.50007-7
Sigrist, M.W.: Laser generation of acoustic waves in liquids and gases. J. Appl. Phys. 60(7), 83 (1986). https://doi.org/10.1063/1.337089
Sliney, D.H., Trokel, S.L.: Medical Lasers and Their Safe Use, ISBN: 9781461392545, e-ISBN: 9781461392521, Springer-Verlag, (1993). https://doi.org/10.1007/978-1-4613-9252-1
Smalley, P.J.: Laser safety: regulations, standards, and guidelines for practice, Ch. 24, in: Lasers for medical applications: diagnostics, therapy and surgery, Edited by: Helena Jelínková, ISBN: 9780857092373, eISBN: 9780857097545, Woodhead Publishing Limited, pp. 725–759 (2013). https://doi.org/10.1533/9780857097545.4.725
Smith, S.W.: Statistics, probability and noise, Ch. 2 in The Scientist and Engineer's Guide to Digital Signal Processing, 2nd edn., 1997–1999 by California Technical Publishing. http://www.dspguide.com/ch2/5.htm
Sommerfeld, A.: Thermodynamics and statistical mechanics: lectures on theoretical physics, Volume: V, Ch.: 5: Outline of an exact kinetic theory of gases, Section: 41: The Maxwell-Boltzmann collision equation, pp. 293–302, ISBN: 9780126546828, edited by: Bopp, F., Meixner, J. Translated by: J. Kestin, Academic Press (1956)
Song, X., Wang, S., Li, X., Teng, A., Chen, Z., Wei, J., Zhao, A., Li, B., Li, Z., He, Q., Zhang, J., Song, L.: Research on spectrum analysis of photoacoustic signal based on COMSOL platform. In: Proc. SPIE 11781, 4th Optics Young Scientist Summit (OYSS 2020), 117811O (2021). https://doi.org/10.1117/12.2591387
Song, X., Wang, S., Li, X., Teng, A., Wei, J., Zhao, A., Li, B., Li, Z., He, Q., Zhang, J., Song, L.: Spectrum analysis of photoacoustic signal based on COMSOL. In: Proc. SPIE 11642, Photons Plus Ultrasound: Imaging and Sensing 2021, 116423S (2021). https://doi.org/10.1117/12.2589250
Star, W.M.: Diffusion theory of light transport, Chapter 6. In: Welch, A.J., van Gemert, M.J.C. Optical-thermal response of laser-irradiated tissue, 2nd edn. e-ISBN: 978-90-481-8831-4, Springer, Dordrecht (2011). https://doi.org/10.1007/978-90-481-8831-4_6
Stroud, K.A., Booth, D.J.: Engineering mathematics, Part I: Foundation Topics. In: Programme F.2: Introduction to Algebra, Powers and Logarithms, 7th Edn Pp. 72–81, ISBN: 9781137031204, e-ISBN: 9781137031228, Palgrave Macmillan (2013)
SuheshkumarSingh, M., Thomas, A.: Photoacoustic elastography imaging: a review. J. Biomed. Opt. 24(4), 040902 (2019). https://doi.org/10.1117/1.JBO.24.4.040902
Sung-Liang Chen, L., Guo, J., Wang, X.: All-optical photoacoustic microscopy. Photoacoustics 3(4), 143–150 (2015). https://doi.org/10.1016/j.pacs.2015.11.001
Szabo, T.L., Diagnostic ultrasound imaging: inside out, 2nd Edn, Ch. 8. In: Wave Scattering and Imaging. ISBN: 9780123964878, eBook ISBN: 9780123965424, Academic Press, Elsevier (2014). https://doi.org/10.1016/B978-0-12-396487-8.00008-2
Treeby, B.E., Cox, B.T.: k-Wave: MATLAB toolbox for the simulation and reconstruction of photoacoustic wave fields. J. Biomed. Opt. 15(2), 021314 (2010). https://doi.org/10.1117/1.3360308
Treeby, B., Cox, B., Jaros, J.: k-Wave: A MATLAB toolbox for the time-domain simulation of acoustic wave fields. Accessed in 14th March 2023. http://www.k-wave.org/index.php
Tuchin, V.V.: Optical Methods for Biomedical Diagnosis. Editor’s Introduction. In: Tuchin, V.V., Handbook of Optical Biomedical Diagnostics, 2nd Edn, Volume 1: Light–Tissue Interaction. ISBN: 9781628419092, PDF-ISBN: 9781628416701, SPIE (2016). https://doi.org/10.1117/3.2219603
Wagner, R.F.: Statistics of speckle in ultrasound B-scans. IEEE Trans. Son. Ultrason. (1983). https://doi.org/10.1109/T-SU.1983.31404
Wang, L.V.: Tutorial on photoacoustic microscopy and computed tomography. IEEE J. Sel. Top. Quantum Electron. (2008). https://doi.org/10.1109/JSTQE.2007.913398
Wang, Z., Ha, S., Kim, K.: A new design of light illumination scheme for deep tissue photoacoustic imaging. Opt. Express 20(20), 22649–22659 (2012c). https://doi.org/10.1364/OE.20.022649
Wang, L., Jacques, S.L., Zheng, L.: MCML - Monte Carlo modeling of light transport in multi-layered tissues. Comput. Methods Programs Biomed. 47(2), 131–146 (1995). https://doi.org/10.1016/0169-2607(95)01640-F
Wang, L.V., Song, Hu.: Photoacoustic tomography: in vivo imaging from organelles to organs. Science 335(6075), 1458–1462 (2012). https://doi.org/10.1126/science.1216210
Wang, J., Wang, Y.: Photoacoustic imaging reconstruction using combined nonlocal patch and total-variation regularization for straight-line scanning. BioMed. Eng. Online 17, 105 (2018). https://doi.org/10.1186/s12938-018-0537-x
Wang, Z., Yang, F., Zhang, W., et al.: Towards in vivo photoacoustic human imaging: shining a new light on clinical diagnostics. Fundam. Res. (2023). https://doi.org/10.1016/j.fmre.2023.01.008
Wang, J., Zhang, C., Wang, Y.: A photoacoustic imaging reconstruction method based on directional total variation with adaptive directivity. BioMed. Eng. Online 16, 64 (2017). https://doi.org/10.1186/s12938-017-0366-3
Wang, L.V.: Photoacoustic tomography, Chapter 19. In: Welch, A.J., van Gemert, M.J.C. Optical-Thermal Response of Laser-Irradiated Tissue, 2nd Ed. e-ISBN: 978-90-481-8831-4, Springer, Dordrecht (2011). https://doi.org/10.1007/978-90-481-8831-4_19
Wang, K., Anastasio, M. A.: Photoacoustic and thermoacoustic tomography: Image formation principles, Ch. 18. In: Scherzer, O., Handbook of Mathematical Methods in Imaging. ISBN: 9780387929194, Online ISBN: 9780387929200, Springer (2011). https://doi.org/10.1007/978-0-387-92920-0_18
Wang, L.V., Wu, H.: Optical coherence tomography, Ch. 9. In: Biomedical Optics Principles and Imaging, Wiley. ISBN: 978-0-471-74304-0, 2007.
Wang, L.V., Wu, H.: Radiative transfer equation and diffusion theory, Ch. 5. In: Biomedical Optics Principles and Imaging, Wiley. ISBN: 978-0-471-74304-0 (2007)
Wang, Z., Ha, S., Kim, K.: Evaluation of finite element based simulation model of photoacoustics in biological tissues. In: Proceedings Vol. 8320, Medical Imaging 2012: Ultrasonic Imaging, Tomography, and Therapy; 83201L (2012a) https://doi.org/10.1117/12.912152
Wang, Z., Ha, S., Kim, K.: Photoacoustic design parameter optimization for deep tissue imaging by numerical simulation. In: Proc. SPIE 8223, Photons Plus Ultrasound: Imaging and Sensing 2012, 822346 (2012b). https://doi.org/10.1117/12.912973
Webb, A.G.: Ultrasonic imaging, Ch. 3, pp. 107–156. In: Introduction to Biomedical Imaging., ISBN: 0471237663, ISBN-13: 9780471237662, e-ISBN:9781119485940, Online ISBN:9780470544983, IEEE Press, Wiley-Interscience, New York (2003). https://doi.org/10.1109/9780470544983.ch3
Westervelt, P.J., Larson, R.S.: Laser-excited broadside array. J. Acoust. Soc. Am. 54, 121 (1973). https://doi.org/10.1121/1.1913551
Wikipedia, International System of Units (SI System). https://en.wikipedia.org/wiki/International_System_of_Units. Accessed in: 27th Feb. 2023
Wikipedia, Full width at half maximum . https://en.wikipedia.org/wiki/Full_width_at_half_maximum. Last Seen in: 25 Jan. 2023
Wikipedia, the free encyclopedia, “Helmholtz equation”. https://en.wikipedia.org/wiki/Helmholtz_equation. Accessed in: 23 Feb. 2023
Williams, M.M.R.: Mathematical methods in particle transport theory, Ch. 2. In: The Boltzmann equation for gas atoms and neutrons, pp. 11–49, ISBN: 9780408700696, Butterworth & Co Publishers Ltd, Waltham (1971)
Wilson, B.C., Adam, G.: A Monte Carlo model for the absorption and flux distributions of light in tissue. Med. Phys. 10(6), 824–830 (1983). https://doi.org/10.1118/1.595361
Yang, J.M., Favazza, C., Yao, J., Chen, R., Zhou, Q., Shung, K.K., Wang, L.V.: Three-dimensional photoacoustic endoscopic imaging of the rabbit esophagus. PLoS ONE 10(4), e0120269 (2015). https://doi.org/10.1371/journal.pone.0120269
Zhang, J., Chen, B., Zhou, M., Lan, H., Gao, F.: Photoacoustic image classification and segmentation of breast cancer: a feasibility study. IEEE Access 7, 5457–5466 (2018). https://doi.org/10.1109/ACCESS.2018.2888910
Zhang, X., Fincke, J.R., Wynn, C.M., Johnson, M.R., Haupt, R.W., Anthony, B.W.: Full noncontact laser ultrasound: first human data. Light Sci. Appl. 8, 119 (2019). https://doi.org/10.1038/s41377-019-0229-8
Zhang, W., Luo, X., Yang, F., Tong, Z., Liang, J., Yuan, B., Yang, S., Wang, Z.: Photoacoustic (532 and 1064 nm) and ultrasonic coscanning microscopy for in vivo imaging on small animals: a productized strategy. J. Biophotonics (2023). https://doi.org/10.1002/jbio.202300007
Zhou, Y., Yao, J., Wang, L.V.: Tutorial on photoacoustic tomography. J. Biomed. Opt. 21(6), 061007 (2016). https://doi.org/10.1117/1.JBO.21.6.061007
Zienkiewicz, O.C., Taylor, R.L., Zhu, J.Z.: The Finite Element Method: Its Basis and Fundamentals, 6th Edn. Ch.: 1, Elsevier, Oxford (2005). eBook ISBN: 9780080472775.
Acknowledgements
The first author hereby would like to introduce great thanks and appreciation to the major author of this research paper: Dr. Samir Mohamed Badawy who is the founder of this research paper's idea and the major participant, supervisor and supporter for performing this work. Also, It's merit here by the first author to mention that Dr. Samir Mohamed Badawy is the founder of the Ph.D's research point for him in 2018 entitled: "Efficient Media Characterization and Classification with Ultrasound and Photo-Acoustics", (registered in 2018 at industrial electronics and control engineering department, Faculty of electronic engineering, Menoufia university, Menoufia, Egypt), which this research paper has been emerged from.
Funding
Open access funding was provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). There was no funding for the entire research.
Author information
Authors and Affiliations
Contributions
The following is a statement outlining the authors’ individual contributions to the paper through the relevant roles:
(1) - Samir Mohmed Badawy: Comprehensive mentoring; research work ideation, delineation and designing; resources; collection, processing, analysis and interpretation of data; investigation; visualization; conceptualization; methodology; software programming support; validation; main research outlines’ writing, revising and rectification; comprehensive supervision and advising.
(2) - Mohammed Tarek GadAllah: Research work ideation, delineation and designing; resources; collection, processing, analysis and interpretation of data; investigation; visualization; conceptualization; methodology; software programming; validation; main research outlines’ writing, revising and rectification.
(3) - Hassan E. Zidan: Hardware support, resources, and supervision.
(4) - Abd El-Naser A. Mohamed, Alaa A. Hefnawy, and Ghada M. El-Banby: Supervision.
Corresponding authors
Ethics declarations
Conflict of interests:
There are no competenig interests at all.
Ethical Approval and Consent to participate:
Not applicable.
Consent for publication:
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the applied full numerical simulation program - ( a COMSOL application file ).
Appendices
Appendix-A:
1.1 Deriving Eq. (1):
We can drive Eq. (1) from the basic gaussian distribution formula (https://en.wikipedia.org/wiki/Full_width_at_half_maximum; Smith 1997–1999) as follow:
where; \(\sigma\) is representing the standard deviation.
r is representing the location in Cartesian coordinates x, y, z.
t is representing the time (x-axis).
\(\mu\) (Or: t0) is representing the mean of the full bell shape’s actual data distributed on the x-axis (here: time axis), in other words it is equivalent to the center time value of the pulse shape (t0).
The variable (r) in equation (A-1) representing the location in the three Cartesian coordinates x, y, z, the main importance of r is that it determines exactly the point source that the tissue will be irradiated from.
Starting from equation (A-1):
From (A-1), we can notice that the maximum value of f (r, t) = fmax = \(\frac{1}{\sigma \sqrt{2\pi }}\) (at: t = \(\mu\) = t0), and f (r, t) = fmax/2 at time t = t0 ± FWHM/2; then at time t = t0 + FWHM/2, f (r, t) = \(0.5*\frac{1}{\sigma \sqrt{2\pi }}\), hence:
Leading to:
Taking the natural logarithm for the two sides for the equation (A-2) leading to:
From the logarithmic rules (Stroud and Booth 2013):
ln (0.5) = ln (\(\frac{1}{2}\)) = ln (1) – ln (2) = 0 – ln (2) =—ln (2).
then equation (A-3) will become:
From (A-4), then:
Leading to: τp ≈ FWHM = 2 \(\sigma \sqrt{2ln2}\) \(\approx 2.355 \sigma\), then:
For a peak value normalization (making the peak value equal to one) for equation (A-1), we will divide the right-hand side on fmax (= \(\frac{1}{\sigma \sqrt{2\pi }}\)), and substituting for \(\sigma \approx \frac{1}{2.355}\) τp from (A-6) then; the peak value normalized f (r, t) in τp instead of \(\sigma\) will be Sn (r, t) where:
From (A-7) and multiplying by the maximum input laser light energy rate per unit volume \(\mathrm{Ipmax}\), hence: \(\mathbf{S}\mathbf{n}\boldsymbol{ }\left({\varvec{r}},{\varvec{t}}\right)\boldsymbol{ }\mathrm{will leading to }(\mathbf{A}-8)\) which is identical to Eq.(1):
Appendix-B:
2.1 Clarification Tutorial on COMSOL programming of the proposed mathematical model presented in Fig. 4:
Coefficient Form PDE and Wave Equation modules in COMSOL have been utilized in programming (2), and (6), respectively; while, (1) has been programmed to be input point source to (2). Note: the output solution (dependent variable) of (2) is the intensity distribution in location and time \(\boldsymbol{\varphi }\left({\varvec{r}},{\varvec{t}}\right)\) W/m2 and it is utilized to complete the input source formula of the next last stage of the proposed mathematical model (6).
In COMSOL, there is the following equation:
This equation (B-1) called in COMSOL: “Coefficient Form PDE (c)”, found under “PDE Interfaces”, found under “Mathematics”, found under “Add Physics” section, found in “Physics” tab found into COMSOL Multiphysics 6.0.
To program (B-1) in COMSOL to apply (2), the terms.
\({e}_{a }, {d}_{a }, c, \alpha , \gamma , \beta , a, and f\) must be defined as follow:\({e}_{a }=0; \alpha = \gamma = \beta =0, 0, 0\); \({d}_{a }=\) n/C; c = D;\(a= {\mu }_{a}\); and finally the source term from (1) was applied as a “Point Source” at position P1 as shown into Fig. 5, (Right click on Coefficient Form PDE (c) founded under the model builder section, then: “Points”, then: “Point Source”): \({\varvec{f}}=\) \(\mathbf{I}\mathbf{p}\mathbf{m}\mathbf{a}\mathbf{x}\mathbf{*}\mathbf{e}\mathbf{x}\mathbf{p}(-2.77\mathbf{*}((\mathbf{t}-\mathbf{t}0)/\mathbf{t}\mathbf{p})^2)\) Where: t0 = t0, tp = \({\tau }_{p}\), and t is the study time instants from 0 to 150 ns.
Also, in COMSOL, there is the following equation:
This equation (B-2), called in COMSOL: “Wave Equation (waeq)”, found under “Classical PDEs”, found under “Mathematics”, found under “Add Physics” section, found in “Physics” tab found into COMSOL Multiphysics 6.0.
To program (B-2) in COMSOL to apply (6), the terms.
\({e}_{a }, c, and f\) must be defined as follow: \({e}_{a }=1/ ( {v}_{s} (\mathrm{target}) ) ^2;\) c = 1; and finally the source term f was applied as a “Source” for the tumor sphere domain founded inside the breast cylinder as shown into Fig. 5, (Right click on Wave Equation (waeq) founded under the model builder section, then: “Source”), where, from (14), \(f=\) ( \({\mu }_{at}\) (target) \(*\) ut \(* \beta\) (target)) / \({C}_{P}\) (target)). Where: ut (in COMSOL language) = \(\frac{\partial u}{\partial t}\), and t is the study time instants from 0 to 150 ns.
The time step, relative tolerance, and mesh size applied in the numerical simulation are as follow:
Start time: 0 ns.
Step time: 1 ns.
Stop time: 150 ns.
Relative tolerance: 0.01.
Maximum element size: 0.15 mm.
Minimum element size: 0.028 mm.
Maximum element growth rate: 1.6
Curvature factor: 0.7
Resolution of narrow regions: 0.4
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
GadAllah, M.T., Mohamed, AN.A., Hefnawy, A.A. et al. A mathematical model for simulating photoacoustic signal generation and propagation in biological tissues. Opt Quant Electron 56, 5 (2024). https://doi.org/10.1007/s11082-023-05481-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11082-023-05481-6