Abstract
It is increasingly recognized that cognitive symptoms are a common sequelae of relapsing-remitting multiple sclerosis and are associated with adverse functional consequences. However, estimates of cognitive impairment (CIm) prevalence vary widely. This study aimed to determine the pooled prevalence of CIm among adults with RRMS and investigate moderators of prevalence rates. Following prospective registration (PROSPERO; CRD42021281815), electronic databases (Embase, Scopus, Medline, and PsycINFO) were searched from inception until March 2023. Eligible studies reported the prevalence of CIm among adults with RRMS, as determined through standardized neuropsychological testing and defined as evidence of reduced performance across at least two cognitive domains (e.g., processing speed, attention) relative to normative samples, healthy controls, or premorbid estimates. The electronic database search yielded 8695 unique records, of which 50 met selection criteria. The pooled prevalence of cognitive impairment was 32.5% (95% confidence interval 29.3–36.0%) across 5859 participants. Mean disease duration and age were significant predictors of cognitive impairment prevalence, with samples with longer disease durations and older age reporting higher prevalence rates. Studies which administered more extensive test batteries also reported significantly higher cognitive impairment prevalence. Approximately one third of adults with RRMS experience clinical levels of CIm. This finding supports the use of routine cognitive testing to enable early detection of CIm, and to identify individuals who may benefit from additional cognitive and functional support during treatment planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic, autoimmune disease which affects approximately 36 per 100,000 people worldwide (Walton et al., 2020). The most common disease course, relapsing-remitting MS (RRMS), constitutes 85% of cases and is marked by distinct episodes of symptom relapse and remission (Leray et al., 2016), while the other disease courses involve progressive worsening of symptoms. Although the most prominent symptoms are in sensorimotor function, increasing emphasis has been placed over recent decades on cognitive effects. Cognitive impairment (CIm) may be a particularly disabling consequence of MS, affecting employment status (Clemens & Langdon, 2018), medication adherence (Bruce et al., 2010), management of finances (Goverover et al., 2019), social functioning (Rao et al., 1991a), and ability to perform activities of daily living (Yazgan et al., 2021). Preservation of cognition is frequently endorsed as a priority among people with MS (Day et al., 2018; Heesen et al., 2008), with one qualitative study highlighting that people with MS were supportive of routine cognitive testing as a means to document an under-addressed, ‘invisible’ symptom, and to advance research in this area (Mortensen et al., 2020).
Despite acceptance that CIm is a potential symptom of MS, estimates of impairment prevalence are equivocal and have not been explored meta-analytically or specifically for people with RRMS. Estimates frequently cited in the literature are broad in range, such as the 40–65% range reported in a seminal literature review (k = 11, n = 640) by Amato and colleagues in 2006 (Amato et al., 2006), and do not provide a specific overall prevalence estimate. Additionally, the reviewed studies are now many decades old and do not utilize current best practice methods or tests for assessing CIm prevalence (Parsons et al., 1957). Moreover, the samples within studies which sought to estimate CIm prevalence within the MS population are largely unrepresentative as they are small (n < 100) or recruited from community samples (McIntosh-Michaelis et al., 1991; Rao et al., 1991a) which may vary in CIm prevalence to clinic-based samples (Amato et al., 2006). Furthermore, these studies did not differentiate between those with RRMS and the progressive courses of MS, which typically involve more severe cognitive dysfunction (Johnen et al., 2017). Thus, the current literature lacks a precise, recent, and representative estimate of the overall prevalence of CIm among people with RRMS. This estimate would be of great interest to neurologists and other health professionals involved in the care of people with RRMS, as many newly diagnosed people with RRMS report concerns about their cognition (Day et al., 2018; Heesen et al., 2008). An updated and more rigorous estimate of CIm prevalence may increase confidence in patient communication regarding the risk of developing CIm. This estimate may also guide service provision by informing resource allocation within MS health care settings toward cognitive health.
The aim of this study was to estimate the pooled prevalence of CIm in RRMS through a systematic review and meta-analysis of the literature. The primary outcome of interest was CIm prevalence as determined through standardized neuropsychological testing, where at least two cognitive domains (e.g., attention, memory, executive functioning) must be reduced to meet criteria for CIm. This is not only considered best practice (Hancock et al., 2022) but also allows exclusion of studies which only examine one cognitive domain, given that domains are differentially affected in MS (Prakash et al., 2008) and single-domain studies are thus likely to misrepresent the overall CIm prevalence. This restriction was also adopted to increase the precision of the prevalence estimate, particularly as previous meta-analyses estimating CIm prevalence in other conditions have found the high variability of definitions across studies to be a barrier to interpretation of their findings (Rayes et al., 2018; Sexton et al., 2019; Yohannes et al., 2017). However, other definitional aspects of CIm, such as the standards deemed to indicate impaired test performance, also have the potential to impact estimates of prevalence. Thus, a secondary aim of this study was to review the definitions of CIm used and examine whether this, in addition to clinical, demographic, and methodological variables, moderates reported prevalence rates.
Method
Registration
This study was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) checklist. The protocol was prospectively published on PROSPERO (CRD42021281815).
Eligibility Criteria
Studies were included if they determined the prevalence of CIm using standardized neuropsychological measures among adults (at least 18 years) diagnosed with RRMS, and reported the proportion of participants who were impaired in two or more cognitive domains. Also eligible were studies which used more than one test to measure a single cognitive domain, and defined CIm as two tests in the impaired range spread across at least two different domains.
Exclusion criteria were studies which (1) only used a cognitive screening measure rather than a neuropsychological test battery, e.g., Montreal Cognitive Assessment (MoCA) or Mini-Mental State Exam (MMSE), given reports that screens have limited sensitivity for detecting CIm in MS (Portaccio et al., 2009a, b; Sehanovic et al., 2020); (2) used self-report rating scales to determine CIm; (3) only required impairment in one cognitive domain for CIm and did not report proportion of participants impaired in two or more domains; (4) aggregated performances over multiple cognitive domains to a single index, as it was possible for individuals with an impairment in only one domain to meet CIm criteria under these conditions; (5) recruited participants with various disease courses and did not report the CIm prevalence for those with RRMS; (6) included participants with pediatric-onset MS; and (7) gauged participants’ cognitive status to determine their eligibility to participate (e.g., required a minimum score on a cognitive screen, only recruited people with cognitive complaints).
Where the same cohort was examined across multiple timepoints, only the publication associated with data collected from the first timepoint was included. Additional data were requested from corresponding authors where relevant.
Search Strategy and Study Selection
Embase, Scopus, Medline, and PsycINFO were searched from inception to March 2023, with no restriction to sample size or the year or country of publication. The search strategy (Fig. 1 of the Supplement) combined keywords and Medical Subject Heading terms related to (1) multiple sclerosis; (2) CIm; and (3) neuropsychological testing. Duplicates were removed using an automated EndNote function.
One reviewer (W. W.) screened all titles and abstracts using the application Rayyan (Ouzzani et al., 2016) and a random 20% was independently assessed by a second reviewer (T. W.) to verify the accuracy and consistency of the screening process. Full-text articles were independently assessed by reviewers (W. W. and T. W.) using a standardized eligibility spreadsheet, with excellent agreement (κ = .84). Studies published in non-English languages were reviewed following translation with Google Translate, which was effective for translating articles to review information relevant to the current study. Discrepancies were resolved by consensus, including with a third reviewer (H. F.).
Data Extraction
A standardized data extraction spreadsheet was used by two independent reviewers (W. W. and T. W.). The primary outcome extracted was the number of participants with RRMS deemed to have CIm. Where multiple prevalence rates were reported according to different CIm criteria, the rate corresponding with the authors’ primary definition of CIm was extracted. Other extracted data included study characteristics (country, recruitment setting, RRMS sample size), demographic and clinical variables (age, gender, disease duration, Expanded Disability Status Scale [EDSS]), and details about the measurement and definition of CIm (neuropsychological tests, cut-off used to indicate test impairment, number of impaired domains required for CIm, and whether healthy controls, normative samples, or premorbid estimates were used as the comparison group).
Study quality was independently assessed by two reviewers (W. W. and T. W.) according to the modified version of the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool (Broen et al., 2012; Broen et al., 2016; Leboeuf-Yde & Lauritsen, 1995), available in Table 1 of the Supplement. The QUADAS has been recommended by the Cochrane Collaboration (Whiting et al., 2011), and was modified by Broen and colleagues (2012) according to criteria developed by Leboeuf-Yde and Lauritsen (1995) and Walker and colleagues (2000) to increase applicability for prevalence studies. It includes 10 criteria regarding participant representativeness, data quality, description of method and results, and definition of prevalence. Points are allocated for each criterion, which are then summed into a model-free count score without estimation of a statistical model (Scherer & Emslander, 2024). A maximum score of 19 points can be earned, with a score of 14 or higher indicating acceptable quality (Broen et al., 2012).
Statistical Analyses
Comprehensive Meta-Analysis (CMA) version 3.0 (Borenstein et al., 2013) was used to conduct analyses and generate plots. Following logit transformations of the prevalence rates, the pooled prevalence of CIm was estimated using a random-effect model with 95% confidence intervals (CIs). The logit-transformed prevalence rates were back-transformed into proportions to aid interpretability and ease of reporting. Between-study heterogeneity was assessed using the I2 statistic, with values above 40% considered to indicate moderate heterogeneity and values above 60% considered substantial (Deeks et al., 2019).
Meta-regression and subgroup analyses were conducted to determine moderators of CIm prevalence. Continuous variables of interest were year of publication, RRMS sample size, mean age, mean disease duration, proportion of female participants, and number of neuropsychological tests administered. Categorical variables were aspects of the definition of CIm used, including the cut-off used to determine impaired test performance (1.5 standard deviations [SDs], 1.67 SDs, or 2 SDs below the comparator’s mean), number of impaired tests required (2 or >2), and comparison group (normative values or healthy controls). As no studies used premorbid estimates, we were unable to include this as a level within subgroup analyses. Many studies reported EDSS using medians rather than means. We extracted whichever was reported and recoded this to a categorical variable. As no studies reported EDSS scores corresponding to severe neurological disability and only four studies reported scores in the moderate range, those which reported EDSS below 2.0 (i.e., no disability) were recoded as lower EDSS and those 2.0 or greater were recoded as higher EDSS (Kurtzke, 1983). Study quality was also recoded to a categorical variable as it was inappropriate for meta-regression given the modified QUADAS yield model-free sum scores (Scherer & Emslander, 2024) and due to the restricted scores obtained. Majority of studies earned the same score of 12/20, with only one study meeting the minimum acceptable score of 14/20. Hence, studies with scores below 12 were recoded as lower quality and scores at or above 12 were recoded as higher quality, and were subject to subgroup analyses to identify whether the studies which earned a score lower than the mode of 12 reported different prevalence rates to the majority.
Risk of publication bias was assessed using a funnel plot and Egger’s test. Funnel plots which appear asymmetric and significant Egger’s tests are suggestive of publication bias. The trim-and-fill procedure was used to determine whether removal of any studies would improve funnel plot symmetry (Duval & Tweedie, 2000).
Results
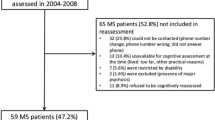
The search yielded 21,878 articles, of which 13,185 were duplicates. Two additional articles were sourced from correspondence with authors and reference lists. Of the 8695 titles and abstracts screened for eligibility, 183 were sought for full-text review. Fifty studies, which included data from 5859 people with RRMS, met the inclusion criteria and were included in the analyses (reference list in Fig. 2 of the Supplement). Details of the selection process are available in Fig. 1.
Study Characteristics
Characteristics of included studies are available in Table 1. Year of publication ranged from 2004 to 2023. All studies which reported the location where participants were recruited did so from a clinical setting (n = 43; 86%), most commonly a MS center (n = 32; 64%), with one study utilizing both clinical and community sampling. Thirty-one studies (62%) solely recruited participants with RRMS, and the remainder recruited mixed samples with different disease courses. Some mixed sample studies did not report demographic data for the participants with RRMS; these studies were included in the overall CIm prevalence estimate but were unable to be included in the moderator analyses if they did not report the relevant moderator.
Demographic and clinical characteristics were variably reported using means or medians, and some studies which recruited mixed samples did not report summary statistics for the subset of participants with RRMS. Thirty-eight (76%) studies reported sex of RRMS participants, with 69% of these being female overall. Mean age of RRMS participants was reported or calculable in 36 (72%) studies and ranged from 30.5 to 58.1 years. Mean disease duration of RRMS participants was reported or calculable in 33 (66%) studies and ranged from 2.1 to 27.0 years. Of studies which used the Expanded Disability Status Scale (EDSS) to measure neurological disability, means of RRMS participants were reported or calculable in 26 (52%) studies and ranged from 1.3 to 4.2, and medians were reported in 11 (22%) studies and ranged from 1.5 to 3.5.
Many studies used standardized batteries developed for use in MS populations. The most common was the Brief Repeatable Battery of Neuropsychological Tests (BRB-N; Bever et al., 1995) used in 29 (58%) studies, which served as a standalone battery for determining CIm in 12 of these. Seven (14%) studies used the Minimal Assessment of Cognitive Function in MS (MACFIMS; Benedict et al., 2002), three (6%) used the Brief International Cognitive Assessment for MS (BICAMS; Benedict et al., 2012), and two (4%) used the Neuropsychological Screening Battery for MS (NSBMS; Bobholz & Rao, 2003). Forty-eight studies (96%) included a verbal fluency measure, though the type (e.g., phonemic or semantic fluency) differed across studies. Beyond this, the most frequently used test was the Symbol Digit Modalities Test (SDMT) used in 44 (88%) studies, followed by the Paced Auditory Serial Addition Test (PASAT) used in 43 (86%) studies. The number of tests administered ranged from 3 to 16. Most studies administered five (k = 13; 26%), six (k = 16; 32%), or seven (k = 10; 20%) tests in total, with seven studies (14%) administering more than six tests and four studies (8%) administering fewer than five tests.
The definitions of CIm varied. Selected studies used one of three cut-off points to indicate impaired performance on a test: 17 (34%) studies used a cut-off of 1.5 SDs (i.e., 7th percentile) below the comparator group’s mean, 17 (34%) used a cut-off of 1.67 SDs (i.e., 5th percentile), and 16 (32%) used a cut-off of 2 SDs (i.e., 2nd percentile). Studies differed in whether they described their criteria as dependent on the number of ‘tests’ or ‘domains’ which were impaired. In some cases, this terminology was functionally equivalent; for instance, many studies used standardized batteries which allocate the same test(s) to each cognitive domain. Most studies (n = 38; 76%) required impairment in at least two tests or cognitive domains for a participant to be considered impaired, while six (12%) required three tests, and one (2%) required four. Five (10%) studies only required one impaired test for CIm but reported the number of participants with two or more impaired tests; this data was extracted for the analyses. Thirty-five (70%) studies compared RRMS participants’ performances against published normative values and the remaining 15 (30%) recruited healthy controls.
Study Quality
Study quality was generally low when examined according to criteria developed for prevalence studies (Table 2 of the Supplement). Only one study (2%) achieved the minimum score for acceptable quality on the modified QUADAS (i.e., 14/19; Broen et al., 2016). There was little variation in scores, with most studies (k = 37; 74%) earning 12 points generally across the same criteria. Several details regarding the representativeness of the sample were rarely reported: no studies used random sampling, only one study (2%) made a statement to indicate the representativeness of their sample, one study (2%) described recruitment non-responders or reasons for non-responding, and three studies (6%) reported the response rate.
CIm Prevalence
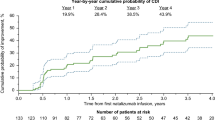
The pooled prevalence of CIm (defined as evidence of relatively reduced performance across at least two cognitive domains) was 32.5% (95% CI 29.3–36.0%) across 5859 people with RRMS. There was substantial heterogeneity between studies (Q49 = 309.62, p < .001, I2 = 84.17, τ2 = 0.23), with reported prevalence rates ranging from 10.2 to 60.0%. The forest plot depicting prevalence and 95% CIs is displayed in Fig. 2. The funnel plot (Fig. 3 of the Supplement) was generally symmetric, Egger’s test was non-significant (p = .104), and the trim-and-fill procedure did not suggest trimming any studies; thus, there was no evidence of publication bias.
Moderators of CIm Prevalence
Results of moderator analyses are summarized in Table 2. Meta-regression analyses indicated that older age (k = 36, b = 0.034, Q1 = 5.66, p = .017) and greater disease duration (k = 33, b = 0.042, Q1 = 7.96, p = .005) were significantly associated with higher prevalence of CIm. Studies which administered more tests also reported significantly greater CIm prevalence (k = 50, b = 0.073, Q1 = 5.10, p = .024). There were no significant effects of year of publication (k = 50, b = −0.013, Q1 = 0.62, p = .431), RRMS sample size (k = 50, b = 0.000, Q1 = 0.02, p = .875), or the proportion of female participants (k = 38, b = −0.018, Q1 = 1.15, p = .283).
Though there appeared to be a trend toward greater CIm prevalence in studies with a mean or median EDSS of 2.0 or above (36.7%; 95% CI 33.0–40.7%) compared with those with EDSS below 2.0 (29.6%; 95% CI 23.7–36.2%), subgroup analyses indicated that this was non-significant (k = 38, Q1 = 3.39, p = .066). There were no significant effects of the cut-off used to indicate impaired test performance (k = 50, Q2 = 2.14, p = .343), number of impaired tests to indicate CIm (k = 50, Q1 = 0.04, p = .845), the comparison group used (k = 50, Q1 = 0.64, p = .425), or study quality (k = 50, Q1 = 2.87, p = .090).
Discussion
The present meta-analysis estimated that approximately one third (32.5%) of adults with RRMS experience CIm. While previous meta-analytic findings have provided indication of the magnitude of CIm in RRMS (Prakash et al., 2008), our findings extend the literature by providing a quantitative estimate of the proportion of people with RRMS who are affected. Though lower than the 40–65% estimate reported by Amato and colleagues in 2006 (Amato et al., 2006), our estimate is an empirical analysis focused on RRMS which incorporated comprehensive data across 50 studies (n = 5859) and only included studies which adopted a stringent definition of CIm (Hancock et al., 2022).
There was substantial between-study heterogeneity, which was partially accounted for by clinical and demographic factors. Disease duration and age were associated with greater CIm prevalence, such that samples with longer disease durations and higher ages had greater CIm prevalence. These findings are consistent with a past meta-analysis (k = 57; n = 3891) by Prakash et al. (2008), which found that the magnitude of cognitive deficits (defined as the difference in cognitive performance relative to healthy controls) among people with RRMS was moderated by higher age, while greater disease duration moderated the magnitude of deficits in the domain of memory and learning only. The impact on disease duration and age on CIm prevalence is also consistent with expectations given that overall disability in RRMS tends to worsen over time even with treatment (Cree et al., 2016).
One challenge in collating CIm prevalence data across the literature are the disparate definitions of CIm used across studies. Although it would have been ideal to adopt one unified definition of CIm for the current study, this was not possible as prevalence rates for different definitions of CIm were rarely extractable from studies. We attempted to address this variability by including aspects of CIm definitions as moderators in our analyses. However, we found that differences in the definitions of CIm used across studies did not moderate prevalence rates. Specifically, prevalence rates did not vary significantly between studies which utilized cut-offs of 1.5, 1.67, or 2 SDs to indicate impaired test performance, or between those which required at least two impaired tests or at least three impaired tests for a participant to meet criteria for CIm. This may be due to our stringent and best-practice CIm definition (i.e., evidence of reduction in at least two cognitive domains) and exclusion of studies that only required impairment in one domain. Additionally, the prevalence rates reported in studies which compared RRMS participants against healthy controls (34.8%; 95% CI 28.2–41.9%) were not significantly different from those which used published normative values (31.6%; 95% CI 27.8–35.6%), supporting the use of published normative values as a valid comparison group for research purposes.
We also found that studies that used more extensive test batteries reported significantly higher CIm prevalence rates. This finding is somewhat unsurprising considering that the administration of more tests provides greater opportunity for a participant to be detected as having CIm. This is especially the case due to the definitions of CIm adopted in some research, for instance, if multiple tests are used to measure a single cognitive domain and reduction on any of these tests is considered sufficient to indicate impairment in that domain. We note that the majority of included studies administered tests relevant to cognitive changes in MS, such as the SDMT or PASAT, and many studies administered brief batteries developed specifically for people with MS (e.g., the BRB-N used in 58% of studies). While these tests and batteries have been validated to be sensitive to cognitive impairment in MS (Drake et al., 2010; Sumowski et al., 2018; Strober et al., 2009), the finding that a more comprehensive test battery is more likely detect cognitive deficits supports this as standard practice for neuropsychological assessment in clinical settings.
It was not possible to formally estimate domain-specific impairment rates across all participants as many studies did not report how many participants were impaired on each test or domain. Of the studies which did report the most frequently impaired domain, attention and information processing speed, typically measured by the SDMT and/or PASAT, was by far the most common (Altieri et al., 2021; Amato et al., 2008; Bisecco et al., 2015; Conti et al., 2021; d’Ambrosia et al., 2020; Deloire et al., 2005; Gois et al., 2021; Goretti et al, 2014; Jakimovski et al., 2019; Lozano-Soto, 2021; Mashayekhi et al., 2022; Portaccio et al., 2009a, 2009b; Preziosa et al., 2016; Rimkus et al., 2011; Rocca et al., 2014; Ruano et al., 2017; Sacco et al., 2015; Talebi et al., 2022), followed by verbal memory (Conti et al., 2021; Gajofatto et al., 2016; Goretti et al., 2014; Maubeuge et al., 2021; Skorve et al., 2023), and visual memory (Amato et al., 2004; Damasceno et al., 2020; Hulst et al., 2012), with few studies reporting executive function (Rimkus et al., 2019) and visuospatial functioning (Lanzillo et al., 2006) as most affected. This is consistent with other work indicating that attention and processing speed deficits are the most prevalent cognitive difficulty in MS (McNicholas et al., 2018).
There are several caveats to the representativeness of the estimate we obtained. Though we did not place restrictions on the recruitment setting when selecting studies, all included studies which reported this recruited from a clinical setting, and no studies based purely on community samples met inclusion criteria. Thus, our estimate is constrained to people with RRMS who attend clinical services and may not generalize to people with RRMS more generally. In light of this, the current meta-analysis may overestimate the prevalence of CIm, as people with concerns about their cognitive functioning may be more likely to present to a clinical setting, leading to selection bias (Abdelnour et al., 2017; Farias et al., 2009). Future research conducting formal neuropsychological testing in community-based samples is warranted. The scope of our study was also limited to adult-onset RRMS, and specific investigations into CIm prevalence in other MS subpopulations may be informative. Pediatric-onset MS comprises approximately 5% of all MS cases (Harding et al., 2013) and the risk of CIm may be greater than those with adult-onset MS, particularly on measures sensitive to processing speed deficits such as the SDMT and PASAT (McKay et al., 2019; Ruano et al., 2018). Given evidence of greater magnitude of CIm in the progressive disease courses (Johnen et al., 2017; Planche et al., 2016), CIm prevalence among these groups is also likely to differ from that in RRMS. Furthermore, subjective CIm may be an important aspect of patient experience distinct from objective CIm (Hughes et al., 2019; Julian et al., 2007; Kinsinger et al., 2010; Mortensen et al., 2020), which requires future examination.
Our ability to perform meta-regression analyses was also affected by the restricted ranges of obtained scores for some variables, specifically EDSS and study quality. Additionally, the study quality tool used was limited by the heterogeneity of its criteria and could only be used to create a statistical model-free count score rather than a model-based scale (Scherer & Emslander, 2024). We were thus required to generate somewhat crude binary classifications to make these variables suitable for subgroup analyses. Neither study quality nor EDSS were significant moderators in the present study. Future work which estimates CIm prevalence could improve in quality by inclusion of information regarding the possibility of recruitment bias, such as the number of people who were approached but did not participate in the study and reasons for non-participation. Potential relationships between neurological disability and CIm may also be more effectively captured by reporting separate EDSS scores for subgroups of participants with impaired or preserved cognition, allowing for between-group comparisons to be extracted meta-analytically. Otherwise, future meta-analytic work in this area may be done using an individual participant data (IPD) approach, where original participant data is collected rather than aggregate data (Tierney et al., 2023). This approach allows for more rigorous examination of moderators and has been considered a ‘gold standard’ of systematic review.
It was notable that none of the selected studies included an estimate of premorbid function as their reference point for impaired cognition. Comparing participants’ test scores to those of other groups without consideration of decline for the individual may impact the CIm prevalence rates reported (Douglas et al., 2018; Tran et al., 2021). For instance, cognitively high-functioning individuals who experience a clinically significant decline from their premorbid abilities, but whose performances on testing do not fall below the chosen normative cut-off, will fail to be classified as having CIm (Sumowski et al., 2018). Conversely, those with a low level of premorbid cognitive functioning may experience relatively mild levels of decline or even no decline, but perform below the cut-off range on testing are deemed cognitively impaired. Use of premorbid estimates may improve the accuracy of prevalence estimates in future studies.
This work has several implications. Our finding that a third of adults with RRMS have CIm is lower than previous ranges cited in the literature for people with MS, such as the 40–65% range previously reported (Amato et al., 2006). This updated, rigorous, and narrower prevalence estimate may provide clinicians with increased confidence when communicating with patients regarding the risk of cognitive difficulties, which is often a concern for newly diagnosed people with MS who are typically of working age (Day et al., 2018; Heesen et al., 2008). Importantly, our estimate is specific to those with a relapsing-remitting disease course, who comprise the majority of MS cases, rather than previous estimates which do not distinguish between relapsing-remitting and progressive courses of MS which experience more severe CIm (Johnen et al., 2017). Our finding can also facilitate management of resource allocation. MS services can make provisions with the view that a third of RRMS patients are likely to require more intensive support for cognitive functioning, such as comprehensive assessment and access to cognitive rehabilitation services. This information may help to determine priorities for funding and staffing. Furthermore, this finding establishes a benchmark for future research into risk profiles, such as factors which predict CIm, to further initiatives into prevention and management.
Conclusion
Ultimately, our finding that approximately one third of adults with RRMS experience CIm, performing below the 7th percentile in two or more cognitive domains, is important for clinical practice. People with RRMS who have CIm are more vulnerable to poor functional outcomes than those without CIm (Bruce et al., 2010; Clemens & Langdon, 2018; Goverover et al., 2019; Rao et al., 1991b; Yazgan et al., 2021), and thus are likely to benefit from additional supports and provision of strategies to manage their symptoms. Routine cognitive testing may be appropriate for those with RRMS to identify such individuals, particularly as patient attitudes to this are positive (Mortensen et al., 2020) and it aligns with both patients’ and clinicians’ priorities for treatment (Singer et al., 2021).
Availability of Data and Materials
No new data was generated in this study. Relevant data appear within the article and supplementary materials. Extracted data may be shared upon reasonable request.
References
Abdelnour, C., Rodríguez-Gómez, O., Alegret, M., Valero, S., Moreno-Grau, S., Sanabria, Á., Hernández, I., Rosende-Roca, M., Vargas, L., Mauleón, A., Sánchez, D., Espinosa, A., Ortega, G., Pérez-Cordón, A., Diego, S., Gailhajanet, A., Guitart, M., Sotolongo-Grau, Ó., Ruiz, A., … Boada, M. (2017). Impact of recruitment methods in subjective cognitive decline. Journal of Alzheimer’s Disease, 57, 625–632. https://doi.org/10.3233/JAD-160915
Akbar, N., Lobaugh, N. J., O’Connor, P., Moradzadeh, L., Scott, C. J., & Feinstein, A. (2010). Diffusion tensor imaging abnormalities in cognitively impaired multiple sclerosis patients. Canadian Journal of Neurological Sciences, 37(5), 608–614. https://doi.org/10.1017/S0317167100010775
Altieri, M., Fratino, M., Maestrini, I., Dionisi, C., Annecca, R., Vicenzini, E., & Di Piero, V. (2021). Cognitive performance in relapsing-remitting multiple sclerosis: At risk or impaired? Dementia and Geriatric Cognitive Disorders, 49(6), 539–543. https://doi.org/10.1159/000514674
Amato, M., Hakiki, B., Goretti, B., Rossi, F., Stromillo, M., Giorgio, A., Roscio, M., Ghezzi, A., Guidi, L., Bartolozzi, M., Portaccio, E., & De Stefano, N. (2012). Association of MRI metrics and cognitive impairment in radiologically isolated syndromes. Neurology, 78(5), 309–314. https://doi.org/10.1212/wnl.0b013e31824528c9
Amato, M., Bartolozzi, M., Zipoli, V., Portaccio, E., Mortilla, M., Guidi, L., Siracusa, G., Sorbi, S., Federico, A., & De Stefano, N. (2004). Neocortical volume decrease in relapsing-remitting MS patients with mild cognitive impairment. Neurology, 63(1), 89–93. https://doi.org/10.1212/01.wnl.0000129544.79539.d5
Amato, M., Portaccio, E., Stromillo, M., Goretti, B., Zipoli, V., Siracusa, G., Battaglini, M., Giorgio, A., Bartolozzi, M., Guidi, L., Sorbi, S., Federico, A., & De Stefano, N. (2008). Cognitive assessment and quantitative magnetic resonance metrics can help to identify benign multiple sclerosis. Neurology, 71(9), 632–638. https://doi.org/10.1212/01.wnl.0000324621.58447.00
Amato, M. P., Portaccio, E., Goretti, B., Zipoli, V., Iudice, A., Della Pina, D., Malentacchi, G., Sabatini, S., Annunziata, P., Falcini, M., Mazzoni, M., Mortilla, M., Fonda, C., De Stefano, N., & Tu, S. S. G. (2010). Relevance of cognitive deterioration in early relapsing-remitting MS: a 3-year follow-up study. Multiple Sclerosis, 16(12), 1474–1482. https://doi.org/10.1177/1352458510380089
Amato, M. P., Zipoli, V., & Portaccio, E. (2006). Multiple sclerosis-related cognitive changes: A review of cross-sectional and longitudinal studies. Journal of the Neurological Sciences, 245(1), 41–46. https://doi.org/10.1016/j.jns.2005.08.019
Benedict, R. H., Amato, M. P., Boringa, J., Brochet, B., Foley, F., Fredrikson, S., Hamalainen, P., Hartung, H., Krupp, L., Penner, I., Reder, A. T., & Langdon, D. (2012). Brief International Cognitive Assessment for MS (BICAMS): International standards for validation. BMC Neurology, 12, 55. https://simsrad.net.ocs.mq.edu.au/login?url=http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med9&AN=22799620https://libkey.io/libraries/590/openurl?sid=OVID:medline&id=pmid:22799620&id=doi:10.1186%2F1471-2377-12-55&issn=1471-2377&isbn=&volume=12&issue=1&spage=55&pages=55&date=2012&title=BMC+Neurology&atitle=Brief+International+Cognitive+Assessment+for+MS+%28BICAMS%29%3A+international+standards+for+validation.&aulast=Benedict
Benedict, R. H., Fischer, J. S., Archibald, C. J., Arnett, P. A., Beatty, W. W., Bobholz, J., Chelune, G. J., Fisk, J. D., Langdon, D. W., Caruso, L., Foley, F., LaRocca, N. G., Vowels, L., Weinstein, A., DeLuca, J., Rao, S. M., & Munschauer, F. (2002). Minimal neuropsychological assessment of MS patients: A consensus approach. The Clinical Neuropsychologist, 16(3), 381–397. https://doi.org/10.1076/clin.16.3.381.13859
Bever, C. T., Jr., Grattan, L., Panitch, H. S., & Johnson, K. P. (1995). The brief repeatable battery of neuropsychological tests for multiple sclerosis: A preliminary serial study. Multiple Sclerosis Journal, 1(3), 165–169. https://doi.org/10.1177/135245859500100306
Bisecco, A., Rocca, M., Pagani, E., Mancini, L., Enzinger, C., Gallo, A., Vrenken, H., Stromillo, M. L., Copetti, M., Thomas, D., Fazekas, F., Tedeschi, G., Barkhof, F., De Stefano, N., & Filippi, M. (2015). Connectivity-based parcellation of the thalamus in multiple sclerosis and its implications for cognitive impairment: A multicenter study. Human Brain Mapping, 36(7). https://doi.org/10.1002/hbm.22809
Bobholz, J. A., & Rao, S. M. (2003). Cognitive dysfunction in multiple sclerosis: A review of recent developments. Current Opinion in Neurology, 16(3), 283–288. https://doi.org/10.1097/01.wco.0000073928.19076.84
Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. (2013). Comprehensive meta-analysis version 3. Biostat.
Broen, M. P., Braaksma, M. M., Patijn, J., & Weber, W. E. (2012). Prevalence of pain in Parkinson’s disease: A systematic review using the modified QUADAS tool. Movement Disorders, 27(4), 480–484. https://doi.org/10.1002/mds.24054
Broen, M. P. G., Narayen, N. E., Kuijf, M. L., Dissanayaka, N. N. W., & Leentjens, A. F. G. (2016). Prevalence of anxiety in Parkinson’s disease: A systematic review and meta-analysis. Movement Disorders, 31(8), 1125–1133. https://doi.org/10.1002/mds.26643
Bruce, J. M., Hancock, L. M., Arnett, P., & Lynch, S. (2010). Treatment adherence in multiple sclerosis: Association with emotional status, personality, and cognition. Journal of Behavioral Medicine, 33(3), 219–227. https://doi.org/10.1007/s10865-010-9247-y
Caceres, F., Vanotti, S., Benedict, R. H., & RELACCEM Work Group. (2014). Cognitive and neuropsychiatric disorders among multiple sclerosis patients from Latin America: Results of the RELACCEM study. Multiple Sclerosis and Related Disorders, 3(3), 335–340. https://doi.org/10.1016/j.msard.2013.10.007
Carotenuto, A., Valsasina, P., Schoonheim, M. M., Geurts, J. J. G., Barkhof, F., Gallo, A., Tedeschi, G., Tommasin, S., Pantano, P., Filippi, M., & Rocca, M. A. (2022). Investigating functional network abnormalities and associations with disability in multiple sclerosis. Neurology, 99(22), e2517–e2530. https://doi.org/10.1212/wnl.0000000000201264
Clemens, L., & Langdon, D. (2018). How does cognition relate to employment in multiple sclerosis? A systematic review. Multiple Sclerosis and Related Disorders, 26, 183–191. https://doi.org/10.1016/j.msard.2018.09.018
Conti, L., Preziosa, P., Meani, A., Vizzino, C., Riccitelli, G., Pagani, E., Valsasina, P., Marchesi, O., Filippi, M., & Rocca, M. A. (2021). Unraveling the substrates of cognitive impairment in multiple sclerosis: The contribution of a multiparametric structural and functional mri approach. Multiple Sclerosis Journal, 26, 513. https://doi.org/10.1111/ene.15023
Cree, B. A., Gourraud, P. A., Oksenberg, J. R., Bevan, C., Crabtree-Hartman, E., Gelfand, J. M., Goodin, D. S., Graves, J., Green, A. J., Mowry, E., Okuda, D. T., Pelletier, D., von Büdingen, H. C., Zamvil, S. S., Agrawal, A., Caillier, S., Ciocca, C., Gomez, R., Kanner, R., … & Hauser, S. L. (2016). Long-term evolution of multiple sclerosis disability in the treatment era. Annals of Neurology, 80(4), 499–510. https://doi.org/10.1002/ana.24747
Damasceno, A., Pimentel-Silva, L. R., Damasceno, B. P., & Cendes, F. (2020). Cognitive trajectories in relapsing-remitting multiple sclerosis: A longitudinal 6-year study. Multiple Sclerosis Journal, 26(13), 1740–1751. https://doi.org/10.1177/1352458519878685
d’Ambrosio, A., Valsasina, P., Gallo, A., De Stefano, N., Pareto, D., Barkhof, F., Ciccarelli, O., Enzinger, C., Tedeschi, G., Stromillo, M. L., Arévalo, M. J., Hulst, H. E., Muhlert, N., Koini, M., Filippi, M., & Rocca, M. A. (2020). Reduced dynamics of functional connectivity and cognitive impairment in multiple sclerosis. Multiple Sclerosis Journal, 26(4), 476–488. https://doi.org/10.1177/1352458519837707
Day, G. S., Rae-Grant, A., Armstrong, M. J., Pringsheim, T., Cofield, S. S., & Marrie, R. A. (2018). Identifying priority outcomes that influence selection of disease-modifying therapies in MS. Neurology Clinical Practice, 8(3), 179–185. https://doi.org/10.1212/cpj.0000000000000449
Deeks, J. J., Higgins, J. P. T., & Altman, D. G. (2019). Analysing data and undertaking meta-analyses (Vol. 2nd Edition). John Wiley & Sons.
Deloire, M. S., Salort, E., Bonnet, M., Arimone, Y., Boudineau, M., Amieva, H., Barroso, B., Ouallet, J. C., Pachai, C., Galliaud, E., Petry, K. G., Dousset, V., Fabrigoule, C., & Brochet, B. (2005). Cognitive impairment as marker of diffuse brain abnormalities in early relapsing remitting multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry, 76(4), 519–526. https://doi.org/10.1136/jnnp.2004.045872
Douglas, K. M., Gallagher, P., Robinson, L. J., Carter, J. D., McIntosh, V. V., Frampton, C. M., Watson, S., Young, A. H., Ferrier, I. N., & Porter, R. J. (2018). Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disorders, 20(3), 260–274. https://doi.org/10.1111/bdi.12602
Drake, A. S., Weinstock-Guttman, B., Morrow, S. A., Hojnacki, D., Munschauer, F. E., & Benedict, R. H. (2010). Psychometrics and normative data for the Multiple Sclerosis Functional Composite: Replacing the PASAT with the Symbol Digit Modalities Test. Multiple Sclerosis, 16(2), 228–237. https://doi.org/10.1177/1352458509354552
Dusankova, J. B., Kalincik, T., Havrdova, E., & Benedict, R. H. B. (2012). Cross cultural validation of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) and the brief international cognitive assessment for multiple sclerosis (BICAMS). Clinical Neuropsychologist, 26(7), 1186–1200. https://doi.org/10.1080/13854046.2012.725101
Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. http://www.jstor.org/stable/2676988
Eshaghi, A., Riyahi-Alam, S., Roostaei, T., Haeri, G., Aghsaei, A., Aidi, M. R., Pouretemad, H. R., Zarei, M., Farhang, S., Saeedi, R., Nazeri, A., Ganjgahi, H., Etesam, F., Azimi, A. R., Benedict, R. H. B., & Sahraian, M. A. (2012). Validity and reliability of a Persian translation of the Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS). Clinical Neuropsychologist, 26(6), 975–984. https://doi.org/10.1080/13854046.2012.694912
Farias, S. T., Mungas, D., Reed, B. R., Harvey, D., & DeCarli, C. (2009). Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Archives of Neurology, 66(9), 1151–1157. https://doi.org/10.1001/archneurol.2009.106
Gajofatto, A., Turatti, M., Bianchi, M., Forlivesi, S., Gobbin, F., Azzara, A., Monaco, S., & Benedetti, M. (2016). Benign multiple sclerosis: Physical and cognitive impairment follow distinct evolutions. Acta Neurologica Scandinavica, 133(3), 183–191. https://doi.org/10.1111/ane.12442
Gois, L. C. P., Pimentel-Silva, L. R., Damasceno, B. P., & Damasceno, A. (2021). Associations between cognitive and clinical disability across MS subtypes: The role of the underlying brain damage. Multiple Sclerosis and Related Disorders, 48, 102701. https://doi.org/10.1016/j.msard.2020.102701
Goretti, B., Viterbo, R., Portaccio, E., Niccolai, C., Hakiki, B., Piscolla, E., Iaffaldano, P., Trojano, M., & Amato, M. (2014). Anxiety state affects information processing speed in patients with multiple sclerosis. Neurological Sciences, 35(4), 559–563. https://doi.org/10.1007/s10072-013-1544-0
Goverover, Y., Chiaravalloti, N., & DeLuca, J. (2019). Money management in multiple sclerosis: The role of cognitive, motor, and affective factors [Original Research]. Frontiers in Neurology, 10(1128). https://doi.org/10.3389/fneur.2019.01128
Hancock, L. M., Hermann, B., Schoonheim, M. M., Hetzel, S. J., Brochet, B., & DeLuca, J. (2022). Comparing diagnostic criteria for the diagnosis of neurocognitive disorders in multiple sclerosis. Multiple Sclerosis and Related Disorders, 58, 103479. https://doi.org/10.1016/j.msard.2021.103479
Harding, K. E., Liang, K., Cossburn, M. D., Ingram, G., Hirst, C. L., Pickersgill, T. P., Te Water Naude, J., Wardle, M., Ben-Shlomo, Y., & Robertson, N. P. (2013). Long-term outcome of paediatric-onset multiple sclerosis: A population-based study. Journal of Neurology, Neurosurgery & Psychiatry, 84(2), 141. https://doi.org/10.1136/jnnp-2012-303996
Heesen, C., Böhm, J., Reich, C., Kasper, J., Goebel, M., & Gold, S. M. (2008). Patient perception of bodily functions in multiple sclerosis: Gait and visual function are the most valuable. Multiple Sclerosis Journal, 14(7), 988–991. https://doi.org/10.1177/1352458508088916
Hughes, A. J., Bhattarai, J., Paul, S., & Beier, M. (2019). 2019/05/01/). Depressive symptoms and fatigue as predictors of objective-subjective discrepancies in cognitive function in multiple sclerosis. Multiple Sclerosis and Related Disorders, 30, 192–197. https://doi.org/10.1016/j.msard.2019.01.055
Hulst, H. E., Schoonheim, M. M., Roosendaal, S. D., Popescu, V., Schweren, L. J., van der Werf, Y. D., Visser, L. H., Polman, C. H., Barkhof, F., & Geurts, J. J. (2012). Functional adaptive changes within the hippocampal memory system of patients with multiple sclerosis. Hum Brain Mapp, 33(10), 2268–2280. https://doi.org/10.1002/hbm.21359
Iaffaldano, P., Viterbo, R. G., Goretti, B., Portaccio, E., Amato, M. P., & Trojano, M. (2014). Emotional and neutral verbal memory impairment in multiple sclerosis. Multiple Sclerosis, 1, 408–409. https://doi.org/10.1016/j.jns.2014.03.038
Jakimovski, D., Weinstock-Guttman, B., Roy, S., Jaworski, M., Hancock, L., Nizinski, A., Srinivasan, P., Fuchs, T. A., Szigeti, K., Zivadinov, R., & Benedict, R. H. (2019). Cognitive profiles of aging in multiple sclerosis. Frontiers in Aging Neuroscience. https://doi.org/10.3389/fnagi.2019.00105
Jandric, D., Lipp, I., Paling, D., Rog, D., Castellazzi, G., Haroon, H., Parkes, L., Parker, G., Tomassini, V., & Muhlert, N. (2021). Mechanisms of network changes in cognitive impairment in multiple sclerosis. Neurology, 97, 19. https://doi.org/10.1212/WNL.0000000000012834
Johnen, A., Landmeyer, N. C., Bürkner, P.-C., Wiendl, H., Meuth, S. G., & Holling, H. (2017). Distinct cognitive impairments in different disease courses of multiple sclerosis—A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 83, 568–578. https://doi.org/10.1016/j.neubiorev.2017.09.005
Jonkman, L., Rosenthal, D. M., Sormani, M. P., Miles, L., Herbert, J., Grossman, R. I., & Inglese, M. (2015). Gray matter correlates of cognitive performance differ between relapsing-remitting and primary-progressive multiple sclerosis. Multiple Sclerosis, 1, 362. https://doi.org/10.1371/journal.pone.0129380
Julian, L., Merluzzi, N. M., & Mohr, D. C. (2007). The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Multiple Sclerosis Journal, 13(1), 81–86. https://doi.org/10.1177/1352458506070255
Kinsinger, S. W., Lattie, E., & Mohr, D. C. (2010). Relationship between depression, fatigue, subjective cognitive impairment, and objective neuropsychological functioning in patients with multiple sclerosis. Neuropsychology, 24(5), 573–580. https://doi.org/10.1037/a0019222
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS). Neurology, 33(11), 1444–1452. https://doi.org/10.1212/wnl.33.11.1444
Lanzillo, R., Prinster, A., Scarano, V., Liuzzi, R., Coppola, G., Florio, C., Salvatore, E., Schiavone, V., Brunetti, A., Muto, M., Orefice, G., Alfano, B., Bonavita, V., & Morra, V. B. (2006). Neuropsychological assessment, quantitative MRI and ApoE gene polymorphisms in a series of MS patients treated with IFN beta-1b. Journal of the Neurological Sciences, 245(1–2), 141–145. https://doi.org/10.1016/j.jns.2005.08.023
Leboeuf-Yde, C., & Lauritsen, J. M. (1995). The prevalence of low back pain in the literature. A structured review of 26 Nordic studies from 1954 to 1993. Spine (Phila Pa 1976), 20(19), 2112–2118. https://doi.org/10.1097/00007632-199510000-00009
Leray, E., Moreau, T., Fromont, A., & Edan, G. (2016). Epidemiology of multiple sclerosis. Revue Neurologique, 172(1), 3–13. https://doi.org/10.1016/j.neurol.2015.10.006
Lozano-Soto, E., Cruz-López, Á., Gutiérrez, R., González, M., Sanmartino, F., Rashid-Lopez, R., Espinosa-Rosso, R., Forero, L., & González-Rosa, J. J. (2021). Predicting neuropsychological impairment in relapsing remitting multiple sclerosis: The Role of clinical measures, treatment, and neuropsychiatry symptoms. Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists, 36(4), 475–484. https://doi.org/10.1093/arclin/acaa088
Ma, A. Y., Vitorino, R. C., Hojjat, S. P., Mulholland, A. D., Zhang, L., Lee, L., Carroll, T. J., Cantrell, C. G., Figley, C. R., & Aviv, R. I. (2017). The relationship between white matter fiber damage and gray matter perfusion in largescale functionally defined networks in multiple sclerosis. Multiple Sclerosis Journal, 23, 1884–1892. https://doi.org/10.1177/1352458517691149
Maarouf, A., Audoin, B., Pariollaud, F., Gherib, S., Rico, A., Soulier, E., Confort-Gouny, S., Guye, M., Schad, L., Pelletier, J., Ranjeva, J.-P., & Zaaraoui, W. (2017). Increased total sodium concentration in gray matter better explains cognition than atrophy in MS. Neurology, 88(3), 289–295. https://doi.org/10.1212/WNL.0000000000003511
Mashayekhi, F., Sadigh-Eteghad, S., Naseri, A., Asadi, M., Abbasi Garravnd, N., & Talebi, M. (2022). ApoE4-positive multiple sclerosis patients are more likely to have cognitive impairment: A cross-sectional study. Neurol Sci, 43(2), 1189–1196. https://doi.org/10.1007/s10072-021-05383-z
Maubeuge, N., Deloire, M. S. A., Brochet, B., Ehrle, N., Charre-Morin, J., Saubusse, A., Ruet, A., BICAFMS Study Investigators. (2021). Validation of the French version of the Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS). Multiple Sclerosis and Related Disorders, 48, 102692. https://doi.org/10.1016/j.msard.2020.102692
McIntosh-Michaelis, S. A., Roberts, M. H., Wilkinson, S. M., Diamond, I. D., McLellan, D. L., Martin, J. P., & Spackman, A. J. (1991). The prevalence of cognitive impairment in a community survey of multiple sclerosis. British Journal of Clinical Psychology, 30(4), 333–348. https://doi.org/10.1111/j.2044-8260.1991.tb00954.x
McKay, K. A., Manouchehrinia, A., Berrigan, L., Fisk, J. D., Olsson, T., & Hillert, J. (2019). Long-term cognitive outcomes in patients with pediatric-onset vs adult-onset multiple sclerosis. JAMA Neurology, 76(9), 1028–1034. https://doi.org/10.1001/jamaneurol.2019.1546
McNicholas, N., O’connell, K., Yap, S. M., Killeen, R. P., Hutchinson, M., & McGuigan, C. (2018). Cognitive dysfunction in early multiple sclerosis: A review. QJM: An International Journal of Medicine, 111(6), 359–364. https://doi.org/10.1093/qjmed/hcx070
Meijer, K. A., Eijlers, A. J. C., Douw, L., Uitdehaag, B. M., Barkhof, F., Geurts, J. J., & Schoonheim, M. M. (2017). Increased connectivity of hub networks and cognitive impairment in multiple sclerosis. Neurology, 88(22), 2107–2114. https://doi.org/10.1212/WNL.0000000000003982
Migliore, S., Ghazaryan, A., Simonelli, I., Pasqualetti, P., Squitieri, F., Curcio, G., Landi, D., Palmieri, M., Moffa, F., Filippi, M., & Vernieri, F. (2017). Cognitive impairment in relapsing-remitting multiple sclerosis patients with very mild clinical disability. Behavioural Neurology, 2017, 7404289. https://doi.org/10.1155/2017/7404289
Moccia, M., Lanzillo, R., Palladino, R., Chang, K. C., Costabile, T., Russo, C., De Rosa, A., Carotenuto, A., Sacca, F., Maniscalco, G. T., & Brescia Morra, V. (2016). Cognitive impairment at diagnosis predicts 10-year multiple sclerosis progression. Multiple Sclerosis, 22(5), 659–667. https://doi.org/10.1177/1352458515599075
Mortensen, G. L., Theódórsdóttir, Á., Sejbæk, T., & Illes, Z. (2020). Patient attitudes to routine cognitive testing in multiple sclerosis. Patient preference and adherence, 14, 693–704. https://doi.org/10.2147/PPA.S245623
Niccolai, C., Portaccio, E., Goretti, B., Hakiki, B., Giannini, M., Pastò, L., Righini, I., Falautano, M., Minacapelli, E., Martinelli, V., Incerti, C., Nocentini, U., Fenu, G., Cocco, E., Marrosu, M. G., Garofalo, E., Ambra, F. I., Maddestra, M., Consalvo, M., Viterbo, R. G., Trojano, M., Losignore, N. A., Zimatore, G. B., Pietrolongo, E., Lugaresi, A., Pippolo, L., Roscio, M., Ghezzi, A., Castellano, D., Stecchi, S., & Amato, M. P. (2015). A comparison of the brief international cognitive assessment for multiple sclerosis and the brief repeatable battery in multiple sclerosis patients. BMC Neurology, 15(1), 204. https://doi.org/10.1186/s12883-015-0460-8
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan — A web and mobile app for systematic reviews. Systematic Reviews, 5(210). https://doi.org/10.1186/s13643-016-0384-4
Ozkul, C., Guclu-Gunduz, A., Eldemir, K., Apaydin, Y., Yazici, G., & Irkec, C. (2020). Clinical features and physical performance in multiple sclerosis patients with and without cognitive impairment: a cross-sectional study. International Journal of Rehabilitation Research, 43(4), 316–323. https://doi.org/10.1097/mrr.0000000000000428
Parsons, O. A., Stewart, K. D., & Arenberg, D. (1957). Impairment of abstracting ability in multiple sclerosis. The Journal of Nervous And Mental Disease, 125(2), 221–225. https://doi.org/10.1097/00005053-195704000-00007
Patti, F., Amato, M. P., Trojano, M., Bastianello, S., Tola, M. R., Goretti, B., Caniatti, L., Di Monte, E., Ferrazza, P., Brescia Morra, V., Lo Fermo, S., Picconi, O., Luccichenti, G., & COGIMUS Study Group. (2009). Cognitive impairment and its relation with disease measures in mildly disabled patients with relapsing-remitting multiple sclerosis: baseline results from the Cognitive Impairment in Multiple Sclerosis (COGIMUS) study. Multiple Sclerosis, 15(7), 779–788. https://doi.org/10.1177/1352458509105544
Planche, V., Gibelin, M., Cregut, D., Pereira, B., & Clavelou, P. (2016). Cognitive impairment in a population-based study of patients with multiple sclerosis: Differences between late relapsing-remitting, secondary progressive and primary progressive multiple sclerosis. European Journal of Neurology, 23(2), 282–289. https://doi.org/10.1111/ene.12715
Portaccio, E., Goretti, B., Zipoli, V., Nacmias, B., Stromillo, M. L., Bartolozzi, M. L., Siracusa, G., Guidi, L., Federico, A., Sorbi, S., De Stefano, M., & Amato, M. P. (2009a). APOE-ε4 is not associated with cognitive impairment in relapsing-remitting multiple sclerosis. Multiple Sclerosis, 15(12), 1489–1494. https://doi.org/10.1177/1352458509348512
Portaccio, E., Goretti, B., Zipoli, V., Siracusa, G., Sorbi, S., & Amato, M. (2009b). A short version of Rao’s Brief Repeatable Battery as a screening tool for cognitive impairment in multiple sclerosis. The Clinical Neuropsychologist, 23(2), 268–275. https://doi.org/10.1080/13854040801992815
Prakash, R. S., Snook, E. M., Lewis, J. M., Motl, R. W., & Kramer, A. F. (2008). Cognitive impairments in relapsing-remitting multiple sclerosis: A meta-analysis. Multiple Sclerosis Journal, 14(9), 1250–1261. https://doi.org/10.1177/1352458508095004
Preziosa, P., Rocca, M. A., Pagani, E., Stromillo, M. L., Enzinger, C., Gallo, A., Hulst, H. E., Atzori, M., Pareto, D., Riccitelli, G. C., Copetti, M., De Stefano, N., Fazekas, F., Bisecco, A., Barkhof, F., Yousry, T. A., Arevalo, M. J., Filippi, M., MS Group. (2016). Structural MRI correlates of cognitive impairment in patients with multiple sclerosis: A multicenter study. Human Brain Mapping, 37(4), 1627–1644. https://doi.org/10.1002/hbm.23125
Rao, S. M., Leo, G. J., Bernardin, L., & Unverzagt, F. (1991a). Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology, 41(5), 685–691. https://doi.org/10.1212/wnl.41.5.685
Rao, S. M., Leo, G. J., Ellington, L., Nauertz, T., Bernardin, L., & Unverzagt, F. (1991b). Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology, 41(5), 692–696. https://doi.org/10.1212/wnl.41.5.692
Rayes, H. A., Tani, C., Kwan, A., Marzouk, S., Colosimo, K., Medina-Rosas, J., Mustafa, A., Su, J., Lambiris, P., Mosca, M., & Touma, Z. (2018). What is the prevalence of cognitive impairment in lupus and which instruments are used to measure it? A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism, 48(2), 240–255. https://doi.org/10.1016/j.semarthrit.2018.02.007
Rimkus, Cd. M., Junqueira Tde, F., Lyra, K. P., Jackowski, M. P., Machado, M. A., Miotto, E. C., Callegaro, D., Otaduy, M. C., & Leite Cda, C. (2011). Corpus callosum microstructural changes correlate with cognitive dysfunction in early stages of relapsing-remitting multiple sclerosis: Axial and radial diffusivities approach. Multiple Sclerosis International, 2011, 304875. https://doi.org/10.1155/2011/304875
Rimkus, C. M., Schoonheim, M. M., Steenwijk, M. D., Vrenken, H., Eijlers, A. J., Killestein, J., Wattjes, M. P., Leite, C. C., Barkhof, F., & Tijms, B. M. (2019). Gray matter networks and cognitive impairment in multiple sclerosis. Multiple Sclerosis, 25(3), 382–391. https://doi.org/10.1177/1352458517751650
Rocca, M. A., Valsasina, P., Hulst, H. E., Abdel-Aziz, K., Enzinger, C., Gallo, A., Pareto, D., Riccitelli, G., Muhlert, N., Ciccarelli, O., Barkhof, F., Fazekas, F., Tedeschi, G., Arevalo, M. J., & Filippi, M. (2014). Functional correlates of cognitive dysfunction in multiple sclerosis: A multicenter fMRI study. Human Brain Mapping, 35(12), 5799–5814. https://doi.org/10.1002/hbm.22586
Ruano, L., Branco, M., Portaccio, E., Goretti, B., Niccolai, C., Patti, F., Chisari, C., Gallo, P., Grossi, P., Ghezzi, A., Roscio, M., Mattioli, F., Stampatori, C., Simone, M., Viterbo, R. G., & Amato, M. P. (2018). Patients with paediatric-onset multiple sclerosis are at higher risk of cognitive impairment in adulthood: An Italian collaborative study. Multiple Sclerosis Journal, 24(9), 1234–1242. https://doi.org/10.1177/1352458517717341
Ruano, L., Portaccio, E., Goretti, B., Niccolai, C., Severo, M., Patti, F., Cilia, S., Gallo, P., Grossi, P., Ghezzi, A., Roscio, M., Mattioli, F., Stampatori, C., Trojano, M., Viterbo, R. G., & Amato, M. P. (2017). Age and disability drive cognitive impairment in multiple sclerosis across disease subtypes. Multiple Sclerosis Journal, 23(9), 1258–1267. https://doi.org/10.1177/1352458516674367
Sacco, R., Bisecco, A., Corbo, D., Della Corte, M., d’Ambrosio, A., Docimo, R., Gallo, A., Esposito, F., Esposito, S., Cirillo, M., Lavorgna, L., Tedeschi, G., & Bonavita, S. (2015). Cognitive impairment and memory disorders in relapsing-remitting multiple sclerosis: The role of white matter, gray matter and hippocampus. Journal of Neurology, 262(7), 1691–1697. https://doi.org/10.1007/s00415-015-7763-y
Scherer, R. & Emslander, V. (2024). Utilizing primary study quality in meta-analyses in psychology: A step-by-step tutorial. PsyArXiv. https://doi.org/10.31234/osf.io/8emsa
Schoonhoven, D. N., Fraschini, M., Tewarie, P., Uitdehaag, B. M., Eijlers, A. J., Geurts, J. J., Hillebr, A., Schoonheim, M. M., Stam, C. J., & Strijbis, E. M. (2019). Resting-state MEG measurement of functional activation as a biomarker for cognitive decline in MS. Multiple Sclerosis, 25(14), 1896–1906. https://doi.org/10.1177/1352458518810260
Sehanovic, A., Smajlovic, D., Tupkovic, E., Ibrahimagic, O. C., Kunic, S., Dostovic, Z., Zoletic, E., & Pasic, Z. (2020). Cognitive disorders in patients with multiple sclerosis. Materia Sociomedica, 32(3), 191. https://simsrad.net.ocs.mq.edu.au/login?url=http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=pmnm&AN=33424448https://libkey.io/libraries/590/openurl?sid=OVID:medline&id=pmid:33424448&id=doi:10.5455%2Fmsm.2020.32.191-195&issn=1512-7680&isbn=&volume=32&issue=3&spage=191&pages=191-195&date=2020&title=Materia+Sociomedica&atitle=Cognitive+Disorders+in+Patients+with+Multiple+Sclerosis.&aulast=Sehanovic
Sexton, E., McLoughlin, A., Williams, D. J., Merriman, N. A., Donnelly, N., Rohde, D., Hickey, A., Wren, M. A., & Bennett, K. (2019). Systematic review and meta-analysis of the prevalence of cognitive impairment no dementia in the first year post-stroke. European Stroke Journal, 4(2), 160–171. https://doi.org/10.1177/2396987318825484
Singer, B. A., Keith, S., Howerter, A., Doll, H., Pham, T., & Mehta, R. (2021). A study comparing patient and clinician perspectives of treatments for multiple sclerosis via group concept mapping. Patient Preference and Adherence, 15, 975–987. https://doi.org/10.2147/ppa.S297052
Skorve, E., Lundervold, A. J., Torkildsen, O., & Myhr, K. M. (2023). Assessment of cognitive function in early stages of multiple sclerosis. Validation of BICAMS in Norway. Multiple Sclerosis Journal, 24, 798. https://doi.org/10.1016/j.msard.2022.104398
Strober, L., Englert, J., Munschauer, F., Weinstock-Guttman, B., Rao, S., & Benedict, R. H. (2009). Sensitivity of conventional memory tests in multiple sclerosis: Comparing the Rao Brief Repeatable Neuropsychological Battery and the Minimal Assessment of Cognitive Function in MS. Multiple Sclerosis, 15(9), 1077–1084. https://doi.org/10.1177/1352458509106615
Sumowski, J. F., Benedict, R., Enzinger, C., Filippi, M., Geurts, J. J., Hamalainen, P., Hulst, H., Inglese, M., Leavitt, V. M., Rocca, M. A., Rosti-Otajarvi, E. M., & Rao, S. (2018). Cognition in multiple sclerosis: State of the field and priorities for the future. Neurology, 90(6), 278–288. https://doi.org/10.1212/wnl.0000000000004977
Talebi, M., Sadigh-Eteghad, S., Talebi, M., Naseri, A., & Zafarani, F. (2022). Predominant domains and associated demographic and clinical characteristics in multiple sclerosis-related cognitive impairment in mildly disabled patients. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery, 58(1), 48. https://doi.org/10.1186/s41983-022-00485-7
Tierney, J. F., Stewart, L. A., & Clarke, M. (2023) Chapter 26: Individual participant data. In: J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, V. A. Welch (Eds.) Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. Available from www.training.cochrane.org/handbook
Topcular, B., Ozcan, M., Kurt, E., Kuscu, D., Icen, N., Sutlas, P., Kirbas, D., & Bingol, A. (2012). Cognitive impairment in relapsing-remitting multiple sclerosis. Noropsikiyatri Arsivi, 49(3), 178–182. https://doi.org/10.4274/npa.y6089
Tran, T., Milanovic, M., Holshausen, K., & Bowie, C. R. (2021). What is normal cognition in depression? Prevalence and functional correlates of normative versus idiographic cognitive impairment. Neuropsychology, 35(1), 33. https://doi.org/10.1037/neu0000717
Walker, B. F. (2000). The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. J Spinal Disord, 13(3), 205–217. https://doi.org/10.1097/00002517-200006000-00003
Walton, C., King, R., Rechtman, L., Kaye, W., Leray, E., Marrie, R. A., Robertson, N., La Rocca, N., Uitdehaag, B., van der Mei, I., Wallin, M., Helme, A., Angood Napier, C., Rijke, N., & Baneke, P. (2020). Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Multiple Sclerosis, 26(14), 1816–1821. https://doi.org/10.1177/1352458520970841
Whiting, P. F., Rutjes, A. W., Westwood, M. E., Mallett, S., Deeks, J. J., Reitsma, J. B., Leeflang, M. M., Sterne, J. A., & Bossuyt, P. M. (2011). QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine, 155(8), 529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Yazgan, Y. Z., Tarakcı, E., Gungor, F., & Kurtuncu, M. (2021). Understanding the impact of cognitive impairment and disease severity on activities of daily living in MS patients with different disability levels. Clinical Neurology and Neurosurgery, 200, 106398. https://doi.org/10.1016/j.clineuro.2020.106398
Yohannes, A. M. P. M. F., Chen, W. P. M. P. H. M., Moga, A. M. M., Leroi, I. M., & Connolly, M. J. M. D. (2017). Cognitive impairment in chronic obstructive pulmonary disease and chronic heart failure: A systematic review and meta-analysis of observational studies. Journal of the American Medical Directors Association, 18(5), 451.e451-451.e411. https://doi.org/10.1016/j.jamda.2017.01.014
Van Schependom, J., D’Hooghe, M. B., Cleynhens, K., D’Hooge, M., Haelewyck, M. C., De Keyser, J., & Nagels, G. (2014). The Symbol Digit Modalities Test as sentinel test for cognitive impairment in multiple sclerosis. European Journal of Neurology, 21(9), 1219–e72. https://doi.org/10.1111/ene.12463
Winter, M., Tallantyre, E. C., Brice, T. A. W., Robertson, N. P., Jones, D. K., & Chamberland, M. (2021). Tract-specific MRI measures explain learning and recall differences in multiple sclerosis. Brain Communications, 3(2), fcab065. https://doi.org/10.1093/braincomms/fcab065
Zhang, X., Zhang, F., Huang, D., Wu, L., Ma, L., Liu, H., Zhao, Y., Yu, S., & Shi, J. (2016). Contribution of gray and white matter abnormalities to cognitive impairment in multiple sclerosis. International Journal of Molecular Sciences, 18(1), 27. https://doi.org/10.3390/ijms18010046
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions Dr. Milena Gandy is currently supported by a Postdoctoral Fellowship from MS Australia. The sponsor had no role in the design and conduct of the study, interpretation of results, review of the manuscript, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Ms. Wu had full access to all data in the study and takes responsibility and for the integrity of the data and the accuracy of the data analysis. Concept and design: Francis, Gandy, Wu, Lucien. Acquisition, analysis, or interpretation of data: Wu, Wheeler, Francis, Gandy. Drafting of the manuscript: Wu. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Wu, Gandy. Obtained funding: N/A. Administrative, technical, or material support: N/A. Supervision: Francis, Gandy.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, W., Francis, H., Lucien, A. et al. The Prevalence of Cognitive Impairment in Relapsing-Remitting Multiple Sclerosis: A Systematic Review and Meta-analysis. Neuropsychol Rev (2024). https://doi.org/10.1007/s11065-024-09640-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11065-024-09640-8