Abstract
Unilateral Spatial Neglect is a disabling neuropsychological deficit. Patients with spatial neglect fail to detect and report events, and to perform actions in the side of space contralateral to a hemispheric cerebral lesion. Neglect is assessed by evaluating the patients’ abilities in daily life activities and by psychometric tests. Computer-based, portable and Virtual Reality technologies may provide more and precise data, and be more sensitive and informative, compared to current paper-and-pencil procedures. Studies since 2010, in which such technologies have been used, are reviewed. Forty-two articles meeting inclusion criteria are categorized according to their technological approaches (computer-, graphics tablet or tablet-, virtual reality-based assessment, and other). The results are promising. However, a definite golden standard, technologically based procedure cannot be still established. Developing technologically based tests is a laborious process, which requires technical and user experience improvements as well as normative data, to increase the evidence of efficacy for clinical evaluation of at least some of the tests considered in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unilateral spatial neglect (henceforth spatial neglect) is a disabling neurological disorder. Patients fail to report events (in different sensory modalities: visual, auditory, and somatosensory; when imaging a familiar visual scene from a given vantage point), which occur in the side of physical and imaginal space and the body contralateral to the side of the hemispheric lesion (contralesional). These patients also fail to perform actions in those sides of extra-personal and personal (i.e., the body) spaces (Chokron et al., 2008; Heilman et al., 2000; Vallar & Bolognini, 2014; Vallar & Calzolari, 2018; Vallar & Maravita, 2009). In most patients, neglect impairs the left side of the space, contralateral to a right-hemispheric lesion. Right spatial neglect, contralateral to a left-hemispheric lesion, is less frequent and severe (Bisiach et al., 1984; Bowen et al., 1999; De Renzi et al., 1970; Ogden, 1985). The reported incidence of spatial neglect after stroke varies across studies (ranging from about 10 to 90%). This wide range depends on a number of factors, including the operational definition of neglect, the patients’ selection criteria, and the assessment methods (Bowen et al., 2013). Spatial neglect is more frequent in the acute stage post-stroke (Bowen et al., 1999). After about three months, spatial neglect is still present in over 15% of right-brain-damaged patients (Ringman et al., 2004). In stroke patients the presence of spatial neglect predicts poor outcome in functional recovery (Di Monaco et al., 2011), entailing a longer time of hospitalization, greater functional dependency, increased risk of falls and a long-term disability in Activities of Daily Living (ADL) (Barer, 1990; Batchelor et al., 2012; Bernspång et al., 1987; Bowen et al., 2013; Czernuszenko & Czlonkowska, 2009; Nijboer et al., 2013). This results in an overall increase of costs for the health system (Barrett & Houston, 2019).
Spatial neglect is not due to lower-level sensorimotor deficits. Many patients show associated sensorimotor deficits, such as hemiplegia, hemianesthesia and hemianopia. However, a double dissociation (Teuber, 1955; Vallar, 2000) has been found between spatial neglect and sensorimotor deficits: patients may show sensorimotor deficits without neglect which, in turn, may be present in isolation (Bisiach et al., 1986). However, sensory and motor deficits may have higher-order components, brought about by spatial neglect itself (Vallar et al., 1991; Vallar, Sandroni, Vallar et al., 1991a, b). In line with these behavioral findings, the neural correlates of spatial neglect involve damage to higher-order associative areas, in perisylvian regions, including the inferior parietal lobule, the temporo-parietal junction, the posterior part of the superior temporal gyrus, the premotor cortex, white matter fiber tracts connecting these regions, the thalamus and the basal ganglia (Corbetta & Shulman, 2011; Karnath & Rorden, 2012; Ptak & Schnider, 2011; Vallar & Calzolari, 2018).
Spatial neglect may be conceived as a multifaceted syndrome with many clinical manifestations that frequently co-occur, but may manifest also in isolation (Halligan et al., 2003; Vallar, 1998). A primary distinction may be drawn between two sets of abnormalities: defective and productive. Defective signs, in which patients exhibit the absence of the appropriate behavior, requested by the experimental task or the ADLs, are the most investigated components of the syndrome. They include the impairment at attending to and exploring the left side of space, and of objects in it (Albert, 1973; Bisiach et al., 1981, 1983; Bisiach & Vallar, 2000; Gainotti et al., 1972; Rode et al., 1995; Schenkenberg et al., 1980; Stone et al., 1991; Vallar & Perani, 1986). Patients with spatial neglect may also show productive manifestations, that consist in gratuitous actions and delusional beliefs. These behaviors are inappropriate in the clinical setting, with respect to the requests by the examiner (as for extra-personal space: Kleinman et al., 2013; Ronchi et al., 2012, 2016; Rusconi et al., 2002; as for bodily space: Vallar & Bolognini, 2014; Vallar & Ronchi, 2009). Spatial neglect may occur in different dimensions or frames, with reference to the body and body parts (the mid-sagittal plane of the trunk, the head). In egocentric spatial neglect, the neglected side is coded with reference to the body’s trunk, the head, or the eyes. Allocentric spatial neglect refers instead to one side of an object, encoded with reference to its intrinsic coordinates (Howard, 1982; Klatzky, 1998, about these reference frames; see Vallar, 1998; Vallar & Bolognini, 2014 for these different manifestations of neglect). Furthermore, depending on the affected sector of space, spatial neglect may concern personal (the body), near peri-personal (the space surrounding the body, and within the reach of body effectors, primarily the hand, also the foot), and far extra-personal (not within the reach of such effectors) sectors of space (Vallar & Maravita, 2009). Finally, spatial neglect may also concern internally generated visual images (representational or imaginal spatial neglect, see Bisiach & Luzzatti, 1978; Bisiach et al., 1981; Meador et al., 1987; Grossi et al., 1989; Rode et al., 1995). All these manifestations of spatial neglect may occur in association, but dissociations among virtually all signs of the deficit have been observed (Bisiach et al., 1986; Guariglia et al., 1993).
Quantitative and Standardized Assessment (“paper-and-pencil”) with Available Normative data
Up to the mid 1930’s (Weisenberg & McBride, 1935), the neuropsychological method coupled a qualitative, often insightful, analysis of the patient’s deficits with, whenever possible, a post-mortem examination of the patient’s brain, to determine the localization of the cerebral lesion, and to relate it with the observed symptoms and signs. Starting from the seminal observations by Broca about aphasia (Broca, 1861; Vallar & Caputi, 2021), the assessment of the patients’ behavioral deficits was qualitative, and consisted in the accurate observation of the behavioral deficits, which were typically apparent and, due to some peculiar features, had captured the attention of the examiner. The neuropsychological examination became then more and more based on standardized tests, which provide quantitative measures (i.e., scores) of the patients’ performances. Moreover, the performances of brain-damaged patients started to be compared, with the support of statistical procedures, with those of control participants, comparable to patients for demographic and socio-cultural variables, and differing from them only for the presence of the cerebral lesion and the putative deficit under investigation. The research work by the Italian neurologist Ennio De Renzi provides an example of this approach (Arrigoni & De Renzi, 1964; De Renzi, 1982). As to spatial neglect, the quantitative assessment of its clinical manifestations has traditionally relied on paper-and-pencil tests, which includes the tasks described in the following.
1) Target cancellation: to find out and mark targets printed on a sheet of paper. In the Line (Albert, 1973) and Circle (Bisiach et al., 1979; Vallar & Perani, 1986) tests only targets are displayed. In the Bells (Gauthier et al., 1989), Star (Wilson et al., 1987), and Letter (Diller & Weinberg, 1977) tests, targets are shown intermingled with distractors. Tests requiring target vs. non-target discrimination are more likely to detect spatial neglect than those in which only targets are present (Arduino et al., 2002; Vallar, 2000). Cancellation tasks, in which patients are required to discriminate between complete and incomplete targets (i.e., the incomplete ones with a left-sided or right-sided missing portion), allow to distinguish between egocentric vs. allocentric, stimulus-based, types of spatial neglect. In target cancellation tests, when left spatial neglect occurs in an egocentric reference frame (e.g., the mid-sagittal plane of the body), complete and incomplete targets, left-sided with reference to such a frame, are not crossed out. In allocentric, object-based left spatial neglect, targets with a left-sided missing part are not crossed out across the whole display, with reference to coordinates based on the target itself (Bickerton et al., 2011; Mancuso et al., 2015; Ota et al., 2001, 2003). Quantitative scores include the total number of omissions and the difference between the number of omissions in the two sides (left and right) of the display (a sheet of paper). Moreover, these tests may provide qualitative information also about other aspects of the patients’ performance, including: (i) the location of the first target crossed out; (ii) the directional pattern of exploration; (iii) the speed of execution, and (iv) the types of error. Errors include the defective omission of targets, that are not crossed out, and the productive manifestations: simple perseveration (repeated crossing out marks), and complex gratuitous productions (various types of drawings, e.g., a hen, the patients’ signature) (Gandola et al., 2013; Ronchi et al., 2009; Rusconi et al., 2002). Another measure of spatial neglect in cancellation tasks is the “center of cancellation”, consisting in the scaled mean position in the horizontal (left-right) dimension of cancelled targets (Rorden & Karnath, 2010; Toraldo et al., 2017).
2) Bisection of a horizontal line: to mark the location corresponding to the physical mid-point of a line, which is then divided it into two segments. In the standard version of line bisection patients set the mid-point using the not paretic arm and hand, ipsilateral to the side of the lesion (right-brain-damaged patients use their right hand, left-brain-damaged patients their left). Lines of different lengths may be presented, with their center aligned with the mid-sagittal plane of the participant’s body, or displaced leftward or rightward (Daini et al., 2002; Schenkenberg et al., 1980; Vallar et al., 2000). Typically, patients with spatial neglect set the mark shifted toward the end of the line ipsilateral to the side of the lesion (i.e., right-brain-damaged patients with left spatial neglect exhibit a rightward deviation from the geometrical mid-point of the line). Typically, the longer the line, the larger the bisection error (Schenkenberg et al., 1980; Vallar, 2000). The Landmark test (Milner et al., 1993) is a variant of manual line bisection, which does not require a motor response. In the Landmark test, in different trials participants decide which of the two halves of pre-bisected lines is longer or shorter, and communicate their response to the examiner, verbally or by pointing. In patients with left spatial neglect, deciding that the right half of the line is longer or shorter than the left half, independent of their actual lengths, and of the question posed by the examiner (longer or shorter?) indicates a response or output bias. By contrast, judging, erroneously with respect to the actual stimulus, that the left half of the line is shorter (and that the right half is longer) indicates a perceptual underestimation of the lateral extent of the left-sided portion of the pre-bisected line.
3) Drawing: to copy a meaningful or meaningless figure presented in front of the participant (Gainotti et al., 1972) or to draw a familiar figure from memory to a verbal command (Bisiach & Vallar, 2000; Rode et al., 2006). Patients’ performances are evaluated considering the extent of the omissions (complete or partial) of details in both the left- and the right-hand sides of the figure, or of each object, when the drawing includes multiple stimuli (Gainotti et al., 1972). Typically, drawings by patients with left spatial neglect are inaccurate and incomplete in their left-hand side. In copying figures including multiple objects, patients may omit either left-hand side objects, with reference to the mid-sagittal plane of their body showing, as discussed above, egocentric spatial neglect, or the left-hand side of each object, with reference to its coordinate frames, showing allocentric spatial neglect (Walker, 1995).
4) Reading: single words and non-words, sentences and passages of prose. Patients showing neglect dyslexia may commit errors of omission, substitution (Ellis et al., 1987; Kinsbourne & Warrington, 1962) and (less frequently) addition (Siéroff, 2017; Vallar et al., 2010) of letters and words (in reading sentences and passages of prose). Reading errors on words and orthographically legal non-words may be classified as neglect errors, using the “neglect point measure” (Ellis et al., 1987). Neglect errors in reading are defined as “errors in which target and error words are identical to the right of an identifiable neglect point in each word but share no letters in common to the left of the neglect point”. Left neglect dyslexia may be also detected using sentences (Antonucci et al., 1995). More ecologically-based reading material (i.e., passages of prose, as in articles or a menu) has been shown to be sensitive to detect the deficit (Galletta et al., 2014).
Patients with spatial neglect may also show a directional bias, or some other forms of neglect, in Activities of Daily Living (ADL). Prompted by several classical observations (see, for instance, Brain, 1941; Paterson & Zangwill, 1944), assessments based on the simulation of realistic conditions have been proposed to quantify the extent of spatial neglect in ADL. The Behavioral Inattention Test (Halligan et al., 1991; Wilson et al., 1987) is a comprehensive standardized battery that includes both conventional paper-and-pencil and behavioral subtests, in which patients are asked to perform tasks reproducing more practical and everyday life activities. Several batteries, including an ADL scale to evaluate extra-personal and personal spatial neglect have been proposed (McIntosh et al., 2000; Pizzamiglio et al., 1989; Zoccolotti et al., 1992; Zoccolotti & Judica, 1991). The Catherine Bergego Scale (CBS) assesses both the functional deficits in extra-personal and personal spaces (e.g., “forgets to eat food on the left side of his/her plate”; “forgets to clean the left side of his/her mouth after eating”), and the patients’ awareness of them, by comparing the observation by the examiner (the physician, the nurse, a relative) with the patients’ evaluation of their own behavior (Azouvi, 1996, 2002; Azouvi et al., 2003; Bergego et al., 1995). The CBS has been repeatedly reported to be a more sensitive tool to detect spatial neglect than the conventional paper-and-pencil tasks (Azouvi, 2002; Azouvi et al., 2003, 2006). Other ecologically valid and straightforward tasks used to assess spatial neglect in personal space require patients to reach contralateral body parts with their ipsilateral hand (Bisiach et al., 1986), or to explore their own body, using the ipsilateral unaffected arm and hand and, with eyes closed, to remove several Velcro stickers previously attached on their clothes, on both sides of the body (Cocchini & Beschin, 2020).
To summarize, a comprehensive clinical assessment of spatial neglect should include: (i) neuropsychological tests, evaluating both near extra-personal (target cancellation, line bisection, drawing by copy and from memory and reading tasks) and personal (body perception, body awareness, assessed by tests requiring patients to explore the two sides of the body, searching for body parts or objects on them) manifestations of the deficit (see Halligan et al., 2003; Menon & Korner-Bitensky, 2004; Vallar & Bolognini, 2014, for reviews); (ii) ADL scales or ecologic tasks, also assessing the patients’ awareness for the disorder (see for review Azouvi, 2017).
Early Attempts to use Information Technologies (IT) for the Neuropsychological Assessment of Spatial Neglect
With increasing time from stroke onset, many patients recover, and may do well in neuropsychological tests, but still have difficulties in ADLs. A more complex control of spatial attention and awareness, and a major contribution from executive processes, may be required since, in everyday life, every activity is a multiple and not repetitive task, at variance from the previously discussed laboratory tests (Bonato et al., 2010, 2012; Della Sala et al., 2018).
Starting from the late 1990s, several computer- and touch-screen-based tasks have been devised and implemented, to provide a more sensitive and informative assessment, allowing to detect impairments in performance even in patients who do within the normal range in paper-and-pencil tests (Deouell et al., 2005; Erez et al., 2009; Rabuffetti et al., 2002; Schendel & Robertson, 2002).
Computerized tests have indeed some pros, typically recording more precisely information such as accuracy and response latencies throughout the execution of the task. To implement the architecture of the test devised by the experimenter, stimuli may be presented in different locations, simultaneously or as a sequence, with equal or varying time intervals between stimuli, across trials, sessions, or both, and may be repeated many times (Bonato et al., 2010; Buxbaum et al., 2012; Deouell et al., 2005). To manipulate the load posed to the participant’s resources, different levels of difficulty of the task can be easily implemented, varying for instance the duration and the number of the stimuli, and adding a concurrent task (Bonato et al., 2013; Bonato & Deouell, 2013). Additional behavioral measures may also be recorded, such as eye movements (Van der Stigchel & Nijboer, 2010), and data available from touch-screen recording (Rabuffetti et al., 2002), such as number and duration of touches, along with response latency measures recorded throughout the execution of the task (Kim et al., 2010). Furthermore, chances for a ceiling effect (namely, most patients obtain the maximum score in a test) are reduced. Quantitative, continuous measures, appropriate for statistical analyses in single patients, may be easily recorded (Robey et al., 1999), including sensitive individual monitoring of variations in performance levels through repeated assessments. Because of the possibility of easily producing unpredictable settings (e.g., presenting stimuli in random locations of the working space, with different shapes, and time duration), computerized tests can be made harder to learn, making more difficult the development of compensatory strategies on the patient’s part. Computerized tests are thus more suitable for test-retest designs, for instance readily allowing the assessment of the generalization effects of a given rehabilitation treatment (Geusgens et al., 2007). Finally, and importantly, computer-based tasks do not pose a general heavy burden on stroke patients in the post-acute and chronic phases. No adverse reactions, such as headache, fatigue, or boredom, have been reported. Conversely, digital tests have been evaluated as funnier, more precise and safer than the traditional paper-and-pencil ones (see, for instance, Pallavicini et al., 2015; Quinn et al., 2018; Smit et al., 2013; Ulm et al., 2013).
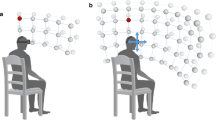
Also Augmented and Virtual Reality-CNADs should address all the above-mentioned issues. Augmented Reality (AR) can be defined as a set of techniques and tools, which add information to physical reality. AR has been used in many fields, including clinical psychology (Chicchi et al., 2015 for review), while its applications to neuropsychology are still limited. Virtual Reality (VR) is a computer-based multisensory, stimulating, and interactive environment, which occurs in real-time. Participants are engaged in activities that appear similar to real-world objects and events (Rizzo et al., 2004). VR can be subdivided in non-immersive (2-dimensional screen presentations, with interaction devices, such as a joystick), and immersive (requiring the integration of computers with further devices, such as Head-Mounted Displays, HDMs, VR controllers, or body-tracking sensors) applications. The immersive applications allow users to experience the virtual environment, and to interact with it, based on the movements of the head or body. For these reasons, starting from the 2000s, several VR paradigms have been implemented in both clinical and research settings (Neguț et al., 2016; Parsons, 2015; Rizzo et al., 2004). As compared to both paper-and-pencil and computer-based assessments, VR may be a useful tool to adequately evaluate ADLs in patients with spatial neglect, through scenarios that resemble everyday life situations (see for reviews Ogourtsova et al., 2017; Pedroli et al., 2015; Tsirlin et al., 2009). Several issues need however to be considered, although several neuropsychological VR paradigms have been developed in the last few years, facilitated by the decreasing costs of the hardware components and the increasing availability of open-access systems. Open issues include: (i) VR-Induced adverse Symptoms and Effects – VRISE (nausea, dizziness, disorientation, fatigue and instability). These symptoms and effects are mainly related to hardware and software inadequacies, not shared/overcome by more contemporary VR hardware and software (Kourtesis et al., 2019a, b). The virtual reality neuroscience questionnaire (VRNQ) is a tool which may facilitate the quantitative assessment of software attributes and intensity of VRISE (Kourtesis et al., 2019b). (ii) Ergonomic features of VR tools. Ergonomic and naturalistic interactions also minimize the risk of VRISE (Kourtesis et al., 2019a). Realistic interfaces, with direct hand interactions and wands with six degrees of freedom of movement, facilitate naturalistic and ergonomic interactions. Direct hand interactions are easier in terms of familiarization with their controls and efficiency and offer a more pleasant user experience; however, they appear less accurate than wands with six degrees of freedom of movement (Figueiredo et al., 2018; Sportillo et al., 2017). Stroke patients often use a wheelchair for locomotion, due to the presence of motor deficits, such as hemiparesis or hemiplegia. VR systems, that can be controlled with one hand (in patients with a hemispheric stroke, the non-paretic ipsilesional upper limb and hand), substantially improve the user experience of the tool itself (Fordell et al., 2011; Kim et al., 2011; Tsirlin et al., 2009). (iii) Psychometric features of the developed systems. Ecological validity is crucial for the assessment of spatial neglect because, with increasing time from stroke onset, patients may still show difficulties in ADLs, despite doing well in neuropsychological paper-and-pencil tests (Bonato et al., 2010, 2012; Della Sala et al., 2018). Immersive VR technology allows to collect data through the employment of dynamic stimuli and interactions with a high degree of control within an ecologically valid environment (Kourtesis et al., 2020; Rizzo et al., 2004). However, immersion depends on the placement, plausibility, and embodiment illusions (Maister et al., 2015; Slater, 2009, 2018). The placement illusion consists in the deception of users to be in a real and not in a virtual environment. The plausibility illusion is the deception of users that the environment reacts to their actions: they thus consider plausible that they are immersed in a real environment. The embodiment illusion refers to the deception that users own the body of the virtual avatar. (iv) Competences. Software developers and researchers are required to have adequate technological abilities, to opt for the appropriate hardware and software and to achieve their research, clinical aims, or both (Kourtesis et al., 2019a). Since a clinical staff typically has no programming skills, cooperation with software developers is needed, to develop and customize these systems (Fordell et al., 2011; Mainetti et al., 2013; Sedda et al., 2013; Sugarman et al., 2011). (v) User experience. This factor is affected by the used hardware, the quality of the sound and graphics, the level of immersion experienced by the user and the level of the enjoyment of the VR experience (Kourtesis et al., 2019b).
Notwithstanding the available evidence, the American Academy of Clinical Neuropsychology (AACN) and the National Academy of Neuropsychology (NAN), raise eight key issues regarding the development, dissemination and implementation of Computerized Neuropsychological Assessment Devices (CNADs), for both research and clinical aims: (i) safety and effectivity, (ii) identity of the end-user, (iii) technical features of hardware and software, (iv) privacy and data security, (v) psychometrics properties, (vi) examinee’s issues, (vii) use of reporting services, and (viii) reliability of responses and results. CNADs could be a standalone device or software, that can be run on a personal computer, a laptop, a tablet, or a smartphone (Bauer et al., 2012; see Kourtesis & MacPherson, 2021 for VR-related issues).
The Review
Up to present, the manifestations of spatial neglect are mainly detected through neuropsychological paper-and-pencil tests, in both clinical and research settings. As noted above, in the subacute and chronic phases post stroke (Rehme et al., 2012), due to spontaneous recovery and cognitive rehabilitation, patients with spatial neglect may do well in neuropsychological tests, but still have difficulty in ADLs (Bonato et al., 2010, 2012; Della Sala et al., 2018). Information Technology (IT)-based devices (computer-, touch-screen- and VR-based) are useful tools for neuropsychological assessment, recording more information than paper-and-pencil tests and allowing to replicate and alter the surrounding world, to evaluate the patients’ behavior in contexts simulating real life (see for reviews Ogourtsova et al., 2017; Pedroli et al., 2015; Tsirlin et al., 2009). However, as previously mentioned, when developing, disseminating and implementing CNADs, for both research and clinical aims, several issues must be taken into account (Bauer et al., 2012; Kourtesis & MacPherson, 2021 for VR-specific issues).
The aim of this scoping review was to present an overview of studies from 2010 onwards, in which IT-based devices were used as a potential tool for the assessment of spatial neglect. Scoping reviews represent indeed a useful instrument to identify and map all available research on a specific topic, and to report information about how studies have been conducted (Munn et al., 2018). Only studies since 2010 onwards were included in this review for two reasons. Firstly, studies prior to 2010 have already been reviewed (Ogourtsova et al., 2017; Pedroli et al., 2015; Tsirlin et al., 2009); secondly, this review aimed at critically verifying whether the tools developed in the last decade successfully target the AACN & NAN Criteria (Bauer et al., 2012; see Kourtesis & MacPherson, 2021 for VR-related issues).
Methods
The norms previously established by the PRISMA-P Group for scoping reviews (Tricco et al., 2018) were adopted. The protocol for this review was not previously registered.
Search Strategy and Selection Criteria
The study search was initially kept broad to capture all relevant articles concerning the use of IT devices [computer, tablet and virtual (VR) or augmented (AR) reality], as possible tools for the clinical assessment of manifestations of the syndrome of spatial neglect. The following electronic databases were used for the identification of papers, up to July 2022: MEDLINE, ScienceDirect, Web of Science and Scopus. The search sting was: (“technology” OR “computer” OR “tablet” OR “virtual reality” OR “augmented reality”) AND [“neglect” OR (“spatial neglect” OR “visual neglect” OR “visuospatial neglect” OR “hemispatial neglect” OR “unilateral spatial neglect”)]. The reference lists of included articles and relevant reviews were checked to identify additional studies. The selection process was performed using Rayyan – a web and mobile app for systematics reviews (access from: https://www.rayyan.ai) (Ouzzani et al., 2016). Titles, abstracts, and full-text articles were screened independently by four out of the six authors (ST, FA, GM and RE), and evaluated for eligibility, based on the following inclusion and exclusion criteria:
-
Inclusion criteria.
-
Related to, and making use of, any of the technologies employed in the clinical assessment of spatial neglect in brain-damaged patients (studies concerning nanotechnologies, technologies applied to eating behavior, nano-molecules, functional Magnetic Resonance Imaging - fMRI, Transcranial Magnetic Stimulation - TMS, transcranial Direct Current Stimulation - tDCS techniques and drug therapies were not included).
-
Focusing on adult brain-damaged patients with spatial neglect (i.e., at least one patient entered the study) and using the abovementioned technologies to assess neglect in patients with a clinical diagnostic aim.
-
Published since 2010.
-
Published in peer-reviewed journals.
-
Published in English.
-
-
Exclusion Criteria.
-
Technical papers with no clinical application in patients with spatial neglect.
-
Literature reviews.
-
Unpublished data, conference proceedings or articles not reporting quantitative data.
-
These criteria are in line with those of other published reviews (Bucur & Papagno, 2021, 2022). A preliminary selection based on title, abstract and keywords was run, excluding those articles not matching selection criteria. A further selection was then made by inspecting full text manuscripts and applying inclusion and exclusion criteria. Unresolved papers were discussed by all authors, to reach a consensus. Duplicates were identified and removed through hand search.
In line with several review articles on neuropsychological topics (Bucur & Papagno, 2021, 2022; Ogourtsova et al., 2017; Zhang et al., 2017) we chose: (i) to include only papers published in English, (ii) not to include articles from gray literature (e.g., unpublished Ph.D. thesis) for two main reasons: (a) often, Ph.D. students embargo their dissertations, and (b) good level theses may be subsequently published in journals as research articles (see, for instance, Bucur & Papagno, 2019, 2022). With these inclusion and exclusion criteria, it is likely that only papers, which have passed the peer review process at an international level, are included in the present review.
Results
The literature search retrieved 9764 articles. After duplicate removal, 5344 were screened for further evaluation because they were potentially relevant research articles, that explored the use of technologies (computer, tablet, VR or AR) as possible tools for the clinical assessment of spatial neglect. After Title and Abstract screening, 52 articles were assessed for eligibility, and, finally, 42 articles met all inclusion criteria and were further analyzed. Figure 1 shows the entire search and selection process.
Articles meeting the inclusion criteria were then categorized into four groups, depending on the digital instruments used to administering the digital tasks: computer (pc and laptop) (13), graphics tablet and touch-screen tablet (8), virtual reality (16), and other (5). The main features of the included studies are summarized in Table 1. In all studies, the presence/absence of spatial neglect was defined according to the neurological exam, a neuropsychological paper-and-pencil assessment, or both. Ten out of 12 studies describing computer-based tools included only patients suffering from a cerebrovascular attack (CVA). Two out these 12 studies (Bonato et al., 2013; Rabuffetti et al., 2012) included patients with different aetiologies (CVA, brain tumor, and traumatic brain injury). One study included also a control group of patients with Mild Cognitive Impairment (Blini et al., 2016). All 13 studies included right-brain-damaged patients; left-brain-damaged patients were included in six out of 13 studies (Blini et al., 2016; Kocanaogullari et al., 2020; Rabuffetti et al., 2012; Villarreal et al., 2020, 2021, 2022). All eight studies, describing graphics tablet- and touch-screen tablet-based assessment tools, included right-brain-damaged patients suffering from CVA; left-brain-damaged patients were included in two out of eight studies (Chung et al., 2016; Pierce et al., 2021). All 16 studies but one (Mesa-Gresa et al., 2011, which included also patients with a brain tumour) using VR-based tools included patients suffering from CVA. Left-brain-damaged patients were included in three out of the 16 studies (Aravind et al., 2015; Aravind & Lamontagne, 2014; Fordell et al., 2011). Immersive VR paradigms were used in all but two studies (Buxbaum et al., 2012; Grattan & Woodbury, 2017). Finally, among the other group, all the five studies included patients suffering from CVA and only two (Peru et al., 2017; Spreij et al., 2020) left-brain-damaged patients.
Analysis of the Quality of the Studies
The quality of the included studies was analyzed using the ad-hoc quality criteria of Corti et al. (2021). Four of the authors (ST, FA, GM and RE) independently evaluated the quality of the studies; no discrepancies in ratings among the evaluators were found. The evaluation criteria, based on parameters considered as relevant for performing experimental and clinical neuropsychological studies, considered the presence (1 = yes, 0 = no) of:
-
1.
Sample size calculation, based on power analysis, to avoid underpowered studies with unclear results, and the occurrence of publication bias. Recent literature points out the need to calculate the required sample size by using power analysis (Brysbaert, 2019; Kühberger et al., 2014). Specifically, for studies focused on tools for clinical neuropsychological assessment, power analysis can be performed by estimating the sample size needed to detect a significant difference in performance, with a specific power, with respect to a control group of participants not presenting impairments in the target construct, namely: healthy controls or patients without the impairment of interest (spatial neglect in the present review, see criterion below).
-
2.
Control group of healthy participants, of patients not presenting an impairment in the target construct, or of both. The comparison of the patients’ performances with those of a control group of participants, matched for age, sex, and educational level, is a standard neuropsychological practice, to evaluate the performance of a patients’ sample with a specific diagnosis (in this review, spatial neglect), with respect to participants who do not show that specific impairment, namely: healthy control participants, patients without spatial neglect or both (Kan et al., 2019; Vallar, 2000). Statistical corrections, such as using co-variates in the analysis of variance (Capitani & Laiacona, 1997), can be performed to control for the possible effects of concomitant variables (age, sex, educational level, duration of disease in stroke patients, severity of the overall neurological impairment, etc.) on the patients’ performances in the tests assessing the target construct of interest (in this review, neglect).
-
3.
Sensitivity or specificity reporting. Sensitivity is the ability of a test to correctly identify patients with a disease; specificity is the ability of a test to correctly identify people without the disease (Swift et al., 2020). Sensitivity and specificity are two psychometric properties that are used to assess target construct validity (i.e., the extent to which an instrument provides a measure of a theoretical construct).
-
4.
Measures of construct validity (the degree to which a test or instrument can measure a concept, trait, or other theoretical entity): convergent and divergent or discriminant validity reporting (Strauss & Smith, 2009). Convergent or congruent validity is the extent to which responses to a test or to an instrument exhibit a strong relationship with responses to similar tests or instruments, namely the extent to which a measure correlates with other measures of the same or of a similar construct. Divergent or discriminant validity is the degree to which a test or measure diverges from (i.e., does not correlate with) another measure, whose underlying construct is conceptually unrelated to it.
-
5.
Ecological validity reporting. Ecological validity indicates if the findings of a study can be generalized to realistic situations in everyday life. It is a subtype of external validity, that can be defined as the extent to which the measures of outcome correlate with, or predict, performance in ADLs (see also Holleman et al., 2020).
-
6.
User experience reporting. This criterion was added to those proposed by Corti et al. (2021), to evaluate the presence of negative (i.e., heavy burden or adverse reactions, as headache, fatigue or boredom) or positive (i.e., feelings of fun and safety) reporting about the experience of using these digital tools, as compared to the traditional paper-and-pencil ones. This criterion was considered as met if user experience reporting was obtained from healthy participants, brain-damaged patients, clinicians, or from all of them.
The analysis of the quality of each study was then based on these six ad-hoc established criteria. With respect to sample size calculation based on power analysis, only two studies (Aravind & Lamontagne, 2014; Quinn et al., 2018) applied this procedure (4.76%). Twenty-six studies included a control group of healthy participants (61.90%), 19 had a control group of patients without spatial neglect (45.23%), and 12 included both (28.57%). As for psychometric properties, 23 studies reported sensitivity or specificity measures (45.23%), 20 convergent or discriminant validity (46.61%) and nine ecological validity (14.28%). Furthermore, among the studies reporting specificity or sensitivity, only two (Buxbaum et al., 2012; Chung et al., 2016) also reported the cut-off for impairment. This means that only for two out of 42 studies data to classify the patients’ performance as impaired or non-impaired (4.76%) were available. Finally, with respect to user experience reporting, only nine studies showed these data (21.42%). Table 2 shows the analysis of the quality of each study, based on the six criteria reported above.
Discussion
At present, the main manifestations of spatial neglect are mainly detected through clinical observation and neuropsychological paper-and-pencil tests, that allow to explore its features (e.g., egocentric vs. allocentric, personal vs. extra-personal) in a standardized way, and to quantify its severity (Heilman et al., 2003; Lezak et al., 1995; Vallar & Bolognini, 2014). However, some pieces of evidence point out that, the longer the duration of the disease after stroke onset, the better the patients’ performances in neuropsychological tests, although difficulties are still found with ADLs (Bonato et al., 2010, 2012; Della Sala et al., 2018). This improvement of spatial neglect in stroke patients is due to both spontaneous recovery of neurological and neuropsychological deficits (Corbetta et al., 2005; Murphy & Corbett, 2009; Stefaniak et al., 2020; Stinear, 2017), and the effects of rehabilitation (Azouvi et al., 2017; Bowen et al., 2013; Kerkhoff & Schenk, 2012). Emerging literature suggests that IT-based devices could be an important tool for neuropsychological assessment. These technologies allow to record much more information with respect to paper-and-pencil tests, and to replicate and alter the surrounding world, permitting to evaluate the patients’ behavior in contexts resembling real life conditions (Ogourtsova et al., 2017; Pedroli et al., 2015; Tsirlin et al., 2009). Despite the potential of these technologies, several issues need to be taken into account when developing, disseminating and implementing CNADs (Bauer et al., 2012; see Kourtesis & MacPherson, 2021 for VR-related issues).
This scoping review aimed at presenting an overview of the studies in which IT-based devices were used as tools to assess manifestations of spatial neglect. The inclusion criteria were met by 42 articles, which were categorized into five groups, depending on their technological approaches: computer (13), graphics tablet or tablet (8), virtual reality-based assessment (16), and other (5).
Computer (pc/laptop)
Computer tools have proved to be effective for the evaluation of manifestations of spatial neglect. These systems appear to be more sensitive in recording difficulties along the left-right spatial dimension, with respect to the gold standard and time-honoured paper-and-pencil tests. Many advantages of this kind of technology are acknowledged by the AACN and the NAN, as well as by this review. Relevant issues include the following: (i) testing large numbers of participants quickly (e.g., parallel administration); (ii) tests available at any time; (iii) enhanced accuracy and precision (e.g., reaction times, or exploration time of the two sides of space, Machner et al., 2018; Mizuno et al., 2016; Rabuffetti et al., 2012; Rossa et al., 2019; Villarreal et al., 2020, 2021); (iv) shorter administration times and reduced costs for test administration and scoring; (v) when appropriate, test versions for different languages; (vi) automatically exporting recorded data to databases (Chiba et al., 2010; Jee et al., 2015, for a digital version of the line bisection task); (vii) increased accessibility, for instance from remote; (viii) integration of algorithms for making decisions on issues such as the identification of an impairment or of a statistically reliable change in performance. These technologies can be easily integrated with other systems, thus providing a wider range of measures (e.g., Electroencephalography, Kocanaogullari et al., 2020). Finally, computerized tests adequately suit the purpose of being administered via telematics from remote: the currently ongoing SARS-CoV-2 world pandemic has emphasized this need.
On the other hand, the present qualitative evaluation of the studies points out several critical issues that must be addressed. With respect to sample size calculation, none of the studies applied power analyses. Ten studies included a control group of healthy participants, and four studies a control group of patients without spatial neglect. Only three out of 13 studies included both. This means that the ability of about 75% of the studies to distinguish different levels of performance among different groups of participants (healthy, affected or not affected by the deficit under investigation, as indicated by other tasks) was not completely assessed, making uncertain the possible clinical validity of most of the proposed IT-based tasks for distinguishing a defective from a preserved performance. As for psychometric properties, eight studies reported sensitivity or specificity measures; two studies report convergent or discriminant validity and only one ecological validity (only Machner et al., (2018) reported both). None of the studies reporting specificity or sensitivity, provided cut-offs for detecting performance impairments. Finally, with respect to user experience reporting, only Ulm et al. (2013) showed these data. The parameters of ecological validity and user experience reporting are most relevant, considering that ADL scales are most sensitive to detect spatial neglect (Azouvi, 2017) and the used IT-based devices are novel tools for both clinicians and patients.
Graphic Tablet and Touch-Screen Tablet
The same list of pros discussed in the previous section readily applies to graphics and touch-screen tablets. The present qualitative evaluation raises several critical issues also for the studies included in this group. In the first place, sample size calculation based on power analysis was applied by only one study (Quinn et al., 2018). A control group of healthy participants was included in four studies and five studies included a control group of patients without spatial neglect; only two out of eight studies had both. This means, as for the computer group, that in about 75% of the studies, the possible clinical validity of most of the proposed IT-based tasks for distinguishing a defective from a preserved performance is uncertain. As for psychometric properties, sensitivity, or specificity measures and convergent or discriminant validity were more frequently reported than in the computer group: five studies reported sensitivity or specificity measures (62.5%) however, among them, only Chung et al. (2016) reported cut-offs for detecting impaired performances. Four studies (50%) reported convergent or discriminant validity. Ecological validity was underreported also in this group: only the article by Pallavicini et al. (2015) provided these measures. Finally, only two out of eight studies mentioned user experience reporting (Pallavicini et al., 2015; Quinn et al., 2018), showing high ratings of acceptance and usability of the NeglectApp and of the StrokeVision app.
Virtual Reality
Among the 16 studies included in this group, non-immersive paradigms were used only in two studies (Buxbaum et al., 2012; Grattan & Woodbury, 2017). The Virtual Reality Lateralized Attention Test (VRLAT) consists indeed of a 2-dimensional screen presentation of a virtual, nonbranching path, in which participants interact with the environment using a joystick. The VRLAT detects manifestation of spatial neglect better than the traditional paper-and-pencil tasks; moreover, scores obtained at the VRLAT correlate with those obtained in the CBS and in the Naturalistic Action Test (Schwartz et al., 2002). However, Buxbaum et al. (2012) report that six out of 70 right brain-damaged patients (about 9%) did not complete the experimental procedure, due to difficulties in operating with the joystick; no other measures of user experience are provided. All the remaining 14 studies included in the VR group employed instead immersive paradigms: in particular, 10 studies integrated computers with head-mounted display, two used shutter glasses (Dvorkin et al., 2012; Fordell et al., 2011), and two body-tracking sensors (Mesa-Gresa et al., 2011; Sugarman et al., 2011). Regarding the methodological aspects, only Aravind and Lamongagne (2014) applied sample size calculation based on power analysis. Eight studies included a control group of healthy participants and eight a control group of patients without spatial neglect; six studies included both groups. As for psychometric properties, seven studies (43.75%) reported sensitivity or specificity measures, but only Buxbaum et al. (2012), also cut-offs for detecting performance impairments. Twelve studies reported instead convergent or discriminant validity measures (75%).
VR paradigms allow to replicate and alter the surrounding world to evaluate the patients’ behavior in contexts simulating real life (Ogourtsova et al., 2017; Pedroli et al., 2015; Tsirlin et al., 2009). However, only Buxbaum et al. (2012), who employed a non-immersive paradigm, and Kim et al. (2021), who used instead an immersive paradigm, provided ecological validity measures (12.5%). The paucity of measures regarding ecological validity is worth noticing, considering that one possible advantage of VR paradigms is to create scenarios that resemble real life situations, thus giving leeway to the evaluation of the patients’ behaviour in these contexts. In particular, the fact that only one out of 14 studies adopting immersive paradigms reported these measures is even more notable, considering that immersive VR technology allows to collect data through the employment of dynamic stimuli and interactions with a high degree of control within an ecologically valid environment (Kourtesis et al., 2020; Rizzo et al., 2004). Finally, with respect to user experience ratings, data, although encouraging, are few: as for non-immersive VR-paradigms, about 9% of the clinical sample did not complete Buxbaum et al.’s (2012) test, due to difficulties in operating with the joystick. As for the immersive VR-paradigms, Fordell et al. (2011) employed a three-item questionnaire: results show that, during the VR-DiSTRO battery administration, 41% of the clinical sample reported to feel focused, 22% to feel pleased during the administration of the task, and 25% to feel alert. Sugarman et al. (2011) made use of the Short Feedback Questionnaire (Rand et al., 2008): the only patient tested with the VR react task of the SeeMe system reported feelings of enjoy, control and success in the VR environment. In the study by Knobel et al. (2020), the administration of the System Usability Scale (Brooke, 1996) to the clinical sample revealed high ratings of acceptance and usability of their VR cancellation task. Conversely, Ogourtsova et al. (2018a, b) conducted focus groups and administered questionnaires directly involving the clinician: experts showed interest and availability to use VR paradigms in their clinical practice. Finally, only two studies investigated VRISE: no participant reported nausea or other adverse effects during or after the administration of the VR-DiSTRO battery of Fordell et al. (2011). Furthermore, cybersickness connected to the VR cancellation task of Knobel et al.‘s (2020) was rated as “very low” at the Simulator Sickness Questionnaire (Kennedy et al., 1993).
Other
Studies included in this section employ an interactive table (Peru et al., 2017), a planar end-effector robot (REAplan®robot) (Montedoro et al., 2019), a tangible user interface system consisting in an integrated system of concrete objects that participants can manipulate (E-TAN platform) (Cerrato et al., 2020) and a driving simulator (Sotokawa et al., 2015; Spreij et al., 2020). None of the included study applied sample size calculation procedures. Four out of five studies included a control group of healthy participants, but only one (Spreij et al., 2020) also a control group of patients without neglect. Sensitivity or specificity measures were reported in three studies, convergent or discriminant validity measures in two. Only Spreij et al. (2020) reported measures of ecological validity. Finally, with respect to user experience, only Cerrato et al. (2020) provided the reports of some patients, who spontaneously described the task as agreeable and quick to perform, and as a welcome change after so many boring paper-and-pencil tests.
For sure, the simulated driving-based assessment offers an evaluation based on tasks like the situations people face in real life while driving; however, the two studies included in this section share the same limitations previously mentioned for VR paradigms. Furthermore, a requirement of driving simulators and VR devices is that both the experimenter and the participant have to be trained to be able to use them; this can be difficult for patients with cognitive impairment, such as memory deficits (Baddeley et al., 2003; Ferbinteanu, 2019). The same problem concerns all the innovative devices included in this section, that are realized with proprietary hardware and software components, since a specific training for each technological proposal is required.
Taken together, data emerging from the present qualitative synthesis of the studies included in this scoping review, although encouraging, are still few and leave than room for several critical issues. In the first place, from a methodological point of view, the recent literature points out the need to calculate the required sample size by using power analysis (Brysbaert, 2019; Kühberger et al., 2014). Accordingly, underpowered studies which may provide unclear results, and then the occurrence of publication biases, are to be avoided. However, despite the above mentioned methodolological critical issues, only two studies included in our review (about the 5%) used sample size calculation procedures. Furthermore, only 12 studies (less than 30%) included both a control group of healthy participants and patients without neglect: the comparison of the patients’ performances with those of a control group of participants, is indeed standard neuropsychological practice, to evaluate the performance of a patients’ sample with a specific diagnosis (in this review, spatial neglect), with respect to participants who do not show that specific impairment, namely: healthy control participants, patients without spatial neglect or both (Kan et al., 2019; Vallar, 2000). As for psychometric features, sensitivity, sensibility measures and convergent or divergent validity were reported in about 50% of the reviewed studies. Moreover, considering that in the subacute, and particularly in the chronic phase post-stroke, patients may still show difficulties in ADLs despite doing well in neuropsychological paper-and-pencil tests (Bonato et al., 2010, 2012; Della Sala et al., 2018), it is even more notable that ecological validity was addressed only in about 13% of the studies. Ecological validity is a subtype of external validity, that can be defined as the extent to which the measures of outcome correlate with, or predict, performance in ADLs (see also Holleman et al. 2020). Finally, despite user experience represents a further critical issue that should be addressed to benefit from the advantages of CNADs (Bauer et al., 2012; see Kourtesis and MacPherson, 2021 for VR-related issues), only about the 20% of the included studies reported user experience measures.
Conclusion
The current findings make it difficult to establish golden standard tests or assessment procedures other than those (i.e., paper-and-pencil tests), that are extensively used in clinical settings for the evaluation of spatial neglect. Moreover, the process of developing IT-based tests in clinical neuropsychology should take into account the issues raised for the development, implementation and dissemination of CNADs and VR paradigms (Bauer et al., 2012; see Kourtesis & MacPherson, 2021 for VR-related issues). This is a laborious procedure, requiring the cooperation of a multidisciplinary team, including clinicians, researchers, informatics, interaction designers and engineers. While embracing technology is necessary, it is also essential to be aware of every aspect that leads to an efficient and effective assessment (see, for instance, Kourtesis & MacPherson, 2021). Nevertheless, it is our view that, through technical and user experience improvements, studies in brain-damaged patients and control participants, comparing paper-and-pencil and IT-based devices, and normative studies providing the cut-off scores, needed for the diagnostic process (e.g., Mancuso et al., 2015; Vallar et al., 1994), it will be possible to gather increasing evidence about the efficacy of at least some of the tests considered in this review. This, in turn, will provide additional support for changes and improvements in clinical practice, for diagnostic and follow up purposes. This review and the discussion of the available IT-based studies provides a database of information for the future developments of this line of research.
Data Availability
data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Albert, M. L. (1973). A simple test of visual neglect. Neurology, 23(6), 658–658. https://doi.org/10.1212/WNL.23.6.658.
Antonucci, G., Guariglia, C., Judica, A., Magnotti, L., Paolucci, S., Pizzamiglio, L., & Zoccolotti, P. (1995). Effectiveness of neglect rehabilitation in a randomized group study. Journal of Clinical and Experimental Neuropsychology, 17(3), 383–389.
Aravind, G., Darekar, A., Fung, J., & Lamontagne, A. (2015). Virtual reality-based Navigation Task to reveal obstacle avoidance performance in individuals with Visuospatial Neglect. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 23(2), 179–188. https://doi.org/10.1109/TNSRE.2014.2369812.
Aravind, G., & Lamontagne, A. (2014). Perceptual and locomotor factors affect obstacle avoidance in persons with visuospatial neglect. Journal of NeuroEngineering and Rehabilitation, 11(1), 38. https://doi.org/10.1186/1743-0003-11-38.
Aravind, G., & Lamontagne, A. (2018). Effect of visuospatial neglect on spatial navigation and heading after stroke. Annals of Physical and Rehabilitation Medicine, 61(4), 197–206. https://doi.org/10.1016/j.rehab.2017.05.002.
Arduino, L. S., Burani, C., & Vallar, G. (2002). Lexical decision in Left Neglect Dyslexia: Word frequency and Nonword Orthographic Neighborhood Effects. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 38(5), 829–832. https://doi.org/10.1016/S0010-9452(08)70050-9.
Arrigoni, G., & De Renzi, E. (1964). Constructional apraxia and hemispheric locus of lesion. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 1(2), 170–197.
Azouvi, P. (1996). Functional consequences and awareness of unilateral neglect: study of an evaluation scale. Neuropsychological Rehabilitation, 6(2), 133–150. https://doi.org/10.1080/713755501.
Azouvi, P. (2002). Sensitivity of clinical and behavioural tests of spatial neglect after right hemisphere stroke. Journal of Neurology Neurosurgery & Psychiatry, 73(2), 160–166. https://doi.org/10.1136/jnnp.73.2.160.
Azouvi, P. (2017). The ecological assessment of unilateral neglect. Annals of Physical and Rehabilitation Medicine, 60(3), 186–190.
Azouvi, P., Bartolomeo, P., Beis, J. M., Perennou, D., Pradat-Diehl, P., & Rousseaux, M. (2006). A battery of tests for the quantitative assessment of unilateral neglect. Restorative neurology and neuroscience, 24(4–6), 273–285.
Azouvi, P., Jacquin-Courtois, S., & Luauté, J. (2017). Rehabilitation of unilateral neglect: evidence-based medicine. Annals of physical and rehabilitation medicine, 60(3), 191–197.
Azouvi, P., Olivier, S., de Montety, G., Samuel, C., Louis-Dreyfus, A., & Tesio, L. (2003). Behavioral assessment of unilateral neglect: study of the psychometric properties of the Catherine Bergego Scale. Archives of Physical Medicine and Rehabilitation, 84(1), 51–57. https://doi.org/10.1053/apmr.2003.50062.
Baddeley, A. D., Kopelman, M. D., & Wilson, B. A. (2003). The handbook of memory disorders. John Wiley & Sons.
Barbieri, C., & De Renzi, E. (1989). Patterns of neglect dissociation. Behavioural Neurology, 2(1), 13–24. https://doi.org/10.1155/1989/728487.
Barer, D. H. (1990). The influence of visual and tactile inattention on predictions for recovery from acute stroke. QJM: An International Journal of Medicine, 74(1), 21–32.
Barrett, A. M., & Houston, K. E. (2019). Update on the Clinical Approach to spatial neglect. Current Neurology and Neuroscience Reports, 19(5), 25. https://doi.org/10.1007/s11910-019-0940-0.
Batchelor, F. A., Mackintosh, S. F., Said, C. M., & Hill, K. D. (2012). Falls after stroke. International Journal of Stroke, 7(6), 482–490. https://doi.org/10.1111/j.1747-4949.2012.00796.x.
Bauer, R. M., Iverson, G. L., Cernich, A. N., Binder, L. M., Ruff, R. M., & Naugle, R. I. (2012). Computerized neuropsychological assessment devices: joint position paper of the American Academy of Clinical Neuropsychology and the National Academy of Neuropsychology. Archives of Clinical Neuropsychology, 27(3), 362–373.
Bergego, C., Azouvi, P., Samuel, C., Marchal, F., Louis-Dreyfus, A., Jokic, C. (1995). Validation d’une échelle d’évaluation fonctionnelle de l’héminégligence dans la vie quotidienne: l’échelle CB. Annales de Réadaptation et de Médecine Physique, 38(4), 183–189. https://doi.org/10.1016/0168-6054(96)89317-2
Bernspång, B., Asplund, K., Eriksson, S., & Fugl-Meyer, A. R. (1987). Motor and perceptual impairments in acute stroke patients: effects on self-care ability. Stroke, 18(6), 1081–1086. https://doi.org/10.1161/01.STR.18.6.1081.
Bickerton, W. L., Samson, D., Williamson, J., & Humphreys, G. W. (2011). Separating forms of neglect using the Apples Test: validation and functional prediction in chronic and acute stroke. Neuropsychology, 25(5), 567–580. https://doi.org/10.1037/a0023501.
Bisiach, E., Bulgarelli, C., Sterzi, R., & Vallar, G. (1983). Line bisection and cognitive plasticity of unilateral neglect of space. Brain and Cognition, 2(1), 32–38. https://doi.org/10.1016/0278-2626(83)90027-1.
Bisiach, E., Capitani, E., Luzzatti, C., & Perani, D. (1981). Brain and conscious representation of outside reality. Neuropsychologia, 19(4), 543–551. https://doi.org/10.1016/0028-3932(81)90020-8.
Bisiach, E., Cornacchia, L., Sterzi, R., & Vallar, G. (1984). Disorders of perceived auditory lateralization after lesionsof the right hemisphere. Brain, 107(1), 37–52. https://doi.org/10.1093/brain/107.1.37.
Bisiach, E., & Faglioni, P. (1974). Recognition of random shapes by patients with unilateral lesions as a function of complexity, association value and delay. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 10(2), 101–110.
Bisiach, E., & Luzzatti, C. (1978). Unilateral neglect of Representational Space. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 14(1), 129–133. https://doi.org/10.1016/S0010-9452(78)80016-1.
Bisiach, E., Luzzatti, C., & Perani, D. (1979). Unilateral neglect, representational schema and consciousness. Brain: a journal of neurology, 102(3), 609–618.
Bisiach, E., Perani, D., Vallar, G., & Berti, A. M. (1986). Unilateral neglect: personal and extra-personal. Neuropsychologia, 24(6), 759–767. https://doi.org/10.1016/0028-3932(86)90075-8.
Bisiach, E., & Vallar, G. (2000). Unilateral neglect in humans. In F. Boller, J. Grafman, & G. Rizzolatti (Eds.), Handbook of Neuropsychology (1 vol., pp. 459–502). Elsevier Science Publishers BV.
Blini, E., Romeo, Z., Spironelli, C., Pitteri, M., Meneghello, F., Bonato, M., & Zorzi, M. (2016). Multi-tasking uncovers right spatial neglect and extinction in chronic left-hemisphere stroke patients. Neuropsychologia, 92, 147–157. https://doi.org/10.1016/j.neuropsychologia.2016.02.028.
Bonato, M., & Deouell, L. Y. (2013). Hemispatial Neglect: computer-based testing allows more sensitive quantification of Attentional Disorders and Recovery and might lead to Better evaluation of Rehabilitation. Frontiers in Human Neuroscience. https://doi.org/10.3389/fnhum.2013.00162. 7.
Bonato, M., Priftis, K., Marenzi, R., Umiltà, C., & Zorzi, M. (2010). Increased attentional demands impair contralesional space awareness following stroke. Neuropsychologia, 48(13), 3934–3940. https://doi.org/10.1016/j.neuropsychologia.2010.08.022.
Bonato, M., Priftis, K., Marenzi, R., Umiltà, C., & Zorzi, M. (2012). Deficits of contralesional awareness: a case study on what paper-and-pencil tests neglect. Neuropsychology, 26(1), 20–36. https://doi.org/10.1037/a0025306.
Bonato, M., Priftis, K., Umiltà, C., & Zorzi, M. (2013). Computer-based attention-demanding testing unveils severe neglect in apparently intact patients. Behavioural Neurology, 26(3), 179–181. https://doi.org/10.1155/2013/139812.
Bowen, A., Hazelton, C., Pollock, A., & Lincoln, N. B. (2013). Cognitive rehabilitation for spatial neglect following stroke. The Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD003586.pub3.
Bowen, A., McKenna, K., & Tallis, R. C. (1999). Reasons for variability in the reported rate of occurrence of unilateral spatial neglect after stroke. Stroke, 30(6), 1196–1202. https://doi.org/10.1161/01.STR.30.6.1196.
Brain, W. R. (1941). Visual disorientation with special reference to lesions of the right cerebral hemisphere. Brain, 64(4), 244–272. https://doi.org/10.1093/brain/64.4.244.
Broca, P. (1861). Remarques sur le siège de la faculté du langage articulé, suivies d’une observation d’aphémie (perte de la parole) (6 vol., pp. 330–357). Bulletin et Memoires de la Societe anatomique de Paris.
Brooke, J. (1996). Sus: a “quick and dirty’usability. Usability evaluation in industry, 189.
Brysbaert, M. (2019). How many participants do we have to include in properly powered experiments? A tutorial of power analysis with reference tables. Journal of Cognition, 2(1), 16. https://doi.org/10.5334/joc.72.
Bucur, M., & Papagno, C. (2019). Are transcranial brain stimulation effects long-lasting in post-stroke aphasia? A comparative systematic review and meta-analysis on naming performance. Neuroscience & Biobehavioral Reviews, 102, 264–289. https://doi.org/10.1016/j.neubiorev.2019.04.019.
Bucur, M., & Papagno, C. (2021). An ALE meta-analytical review of the neural correlates of abstract and concrete words. Scientific Reports, 11(1), 15727. https://doi.org/10.1038/s41598-021-94506-9.
Bucur, M., & Papagno, C. (2022). Deep brain stimulation in Parkinson Disease: a Meta-analysis of the long-term neuropsychological outcomes. Neuropsychology Review. https://doi.org/10.1007/s11065-022-09540-9.
Buxbaum, L. J., Dawson, A. M., & Linsley, D. (2012). Reliability and validity of the virtual reality lateralized attention test in assessing hemispatial neglect in right-hemisphere stroke. Neuropsychology, 26(4), 430–441. https://doi.org/10.1037/a0028674.
Buxbaum, L. J., Ferraro, M. K., Veramonti, T., Farne, A., Whyte, J., Ladavas, E., et al. (2004). Hemispatial neglect: subtypes, neuroanatomy, and disability. Neurology, 62(5), 749–756. https://doi.org/10.1212/01.WNL.0000113730.73031.F4.
Buxbaum, L. J., Palermo, M. A., Mastrogiovanni, D., Read, M. S., Rosenberg-Pitonyak, E., Rizzo, A. A., & Coslett, H. B. (2008). Assessment of spatial attention and neglect with a virtual wheelchair navigation task. Journal of Clinical and Experimental Neuropsychology, 30(6), 650–660. https://doi.org/10.1080/13803390701625821.
Buxbaum, L. J., Palermo, M., Mastrogiovanni, D., Read, M. S., Rosenberg-Pitonyak, E., Rizzo, A. A., & Coslett, H. B. (2006). Assessment of Spatial Neglect with a Virtual Wheelchair Navigation Task. In 2006 International Workshop on Virtual Rehabilitation (pp. 94–99). Presented at the 2006 International Workshop on Virtual Rehabilitation, New York, NY: IEEE. https://doi.org/10.1109/IWVR.2006.1707534
Capitani, E., & Laiacona, M. (1997). Composite neuropsychological batteries and demographic correction: standardization based on equivalent scores, with a review of published data. Journal of Clinical and Experimental Neuropsychology, 19(6), 795–809. https://doi.org/10.1080/01688639708403761.
Cerrato, A., Pacella, D., Palumbo, F., Beauvais, D., Ponticorvo, M., Miglino, O., & Bartolomeo, P. (2020). E-TAN, a technology-enhanced platform with tangible objects for the assessment of visual neglect: a multiple single-case study. Neuropsychological Rehabilitation, 1–15. https://doi.org/10.1080/09602011.2020.1762671.
Chiba, Y., Nishihara, K., & Haga, N. (2010). Evaluating visual bias and effect of proprioceptive feedback in unilateral neglect. Journal of Clinical Neuroscience, 17(9), 1148–1152. https://doi.org/10.1016/j.jocn.2010.02.017.
Chicchi, G. I. A., Pallavicini, F., Pedroli, E., Serino, S., & Riva, G. (2015). Augmented Reality: A Brand New Challenge for the Assessment and Treatment of Psychological Disorders. Computational and Mathematical Methods in Medicine, 2015, 1–12. https://doi.org/10.1155/2015/862942
Chokron, S., Bartolomeo, P., & Siéroff, É. (2008). La négligence spatiale unilatérale: trente ans de recherches, de découvertes, d’espoirs et (surtout) de questions. Revue Neurologique, 164, S134–S142. https://doi.org/10.1016/S0035-3787(08)73304-6.
Chung, S. J., Park, E., Ye, B. S., Lee, H. S., Chang, H. J., Song, D., et al. (2016). The computerized table setting test for detecting unilateral neglect. PLOS ONE, 11(1), e0147030. https://doi.org/10.1371/journal.pone.0147030.
Cocchini, G., & Beschin, N. (2020). The Fluff test: improved scoring system to account for different degrees of contralesional and ipsilesional personal neglect in brain damaged patients. Neuropsychological Rehabilitation, 1–15. https://doi.org/10.1080/09602011.2020.1797828.
Cocchini, G., Beschin, N., & Jehkonen, M. (2001). The Fluff Test: a simple task to assess body representation neglect. Neuropsychological Rehabilitation, 11(1), 17–31. https://doi.org/10.1080/09602010042000132.
Colarusso, R. P., & Hammill, D. D. (1972). Motor-free visual perception test. Academic Therapy Pub.
Corbetta, M., Kincade, M. J., Lewis, C., Snyder, A. Z., & Sapir, A. (2005). Neural basis and recovery of spatial attention deficits in spatial neglect. Nature Neuroscience, 8(11), 1603–1610. https://doi.org/10.1038/nn1574.
Corbetta, M., & Shulman, G. L. (2011). Spatial neglect and attention networks. Annual Review of Neuroscience, 34(1), 569–599. https://doi.org/10.1146/annurev-neuro-061010-113731.
Corti, C., Oprandi, M. C., Chevignard, M., Jansari, A., Oldrati, V., Ferrari, E., et al. (2021). Virtual-reality performance-based Assessment of cognitive functions in adult patients with acquired Brain Injury: a scoping review. Neuropsychology Review. https://doi.org/10.1007/s11065-021-09498-0.
Czernuszenko, A., & Czlonkowska, A. (2009). Risk factors for falls in stroke patients during inpatient rehabilitation. Clinical Rehabilitation, 23(2), 176–188. https://doi.org/10.1177/0269215508098894.
Daini, R., Angelelli, P., Antonucci, G., Cappa, S. F., & Vallar, G. (2002). Exploring the syndrome of spatial unilateral neglect through an illusion of length. Experimental Brain Research, 144(2), 224–237. https://doi.org/10.1007/s00221-002-1034-8.
Dawson, A. M., Buxbaum, L. J., & Rizzo, A. A. (2008). The virtual reality lateralized attention test: Sensitivity and validity of a new clinical tool for assessing hemispatial neglect (pp.77–82). Presented at the 2008 Virtual Rehabilitation, IEEE.
Delis, D. C., Kaplan, E., & Kramer, J. H. (2012). October 8). Delis-Kaplan executive function system. American Psychological Association. https://doi.org/10.1037/t15082-000.
Della Sala, S., Beschin, N., & Cubelli, R. (2018). Persistent neglect in everyday life. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 103, 382–384. https://doi.org/10.1016/j.cortex.2017.09.010.
Deouell, L. Y., Sacher, Y., & Soroker, N. (2005). Assessment of spatial attention after brain damage with a dynamic reaction time test. Journal of the International Neuropsychological Society, 11(06), https://doi.org/10.1017/S1355617705050824.
De Renzi, E. (1982). Disorders of space exploration and cognition. John Wiley.
De Renzi, E., Faglioni, P., & Scotti, G. (1970). Hemispheric Contribution to Exploration of Space through the visual and tactile modality. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 6(2), 191–203. https://doi.org/10.1016/S0010-9452(70)80027-2.
Diller, L., & Weinberg, J. (1977). Hemi-inattention in rehabilitation. The evolution of a rational remediation program. Advances in Neurology. Hemi-Inattention and Hemisphere Specialization, 18, 63–82.
Di Monaco, M., Schintu, S., Dotta, M., Barba, S., Tappero, R., & Gindri, P. (2011). Severity of unilateral spatial neglect is an independent predictor of functional Outcome after Acute Inpatient Rehabilitation in individuals with Right Hemispheric Stroke. Archives of Physical Medicine and Rehabilitation, 92(8), 1250–1256. https://doi.org/10.1016/j.apmr.2011.03.018.
Dvorkin, A. Y., Bogey, R. A., Harvey, R. L., & Patton, J. L. (2012). Mapping the neglected space: gradients of detection revealed by virtual reality. Neurorehabilitation and Neural Repair, 26(2), 120–131. https://doi.org/10.1177/1545968311410068.
Ellis, A. W., Flude, B. M., & Young, A. W. (1987). “Neglect dyslexia” and the early visual processing of letters in words and nonwords. Cognitive Neuropsychology, 4(4), 439–464. https://doi.org/10.1080/02643298708252047.
Erez, A. B. H., Katz, N., Ring, H., & Soroker, N. (2009). Assessment of spatial neglect using computerised feature and conjunction visual search tasks. Neuropsychological Rehabilitation, 19(5), 677–695. https://doi.org/10.1080/09602010802711160.
Fels, M., & Geissner, E. (1997). Neglect-Test (NET): ein Verfahren zur Erfassung visueller Neglectphänomene; Handanweisung; deutsche überarbeitete Adaption des Behavioural Inattention Test (Wilson, Cockburn & Halligan, 1987). Hogrefe, Verlag für Psychologie.
Ferbinteanu, J. (2019). Memory systems 2018 – towards a new paradigm. Neurobiology of Learning and Memory, 157, 61–78. https://doi.org/10.1016/j.nlm.2018.11.005.
Figueiredo, L., Rodrigues, E., Teixeira, J., & Teichrieb, V. (2018). A comparative evaluation of direct hand and wand interactions on consumer devices. Computers & Graphics, 77, 108–121. https://doi.org/10.1016/j.cag.2018.10.006.
Fordell, H., Bodin, K., Bucht, G., & Malm, J. (2011). A virtual reality test battery for assessment and screening of spatial neglect: VR-test battery for assessment and screening of spatial neglect. Acta Neurologica Scandinavica, 123(3), 167–174. https://doi.org/10.1111/j.1600-0404.2010.01390.x.
Gainotti, G., Messerli, P., & Tissot, R. (1972). Qualitative analysis of unilateral spatial neglect in relation to laterality of cerebral lesions. Journal of Neurology Neurosurgery & Psychiatry, 35(4), 545–550. https://doi.org/10.1136/jnnp.35.4.545.
Galletta, E. E., Campanelli, L., Maul, K. K., & Barrett, A. M. (2014). Assessment of Neglect Dyslexia with Functional Reading materials. Topics in Stroke Rehabilitation, 21(1), 75–86. https://doi.org/10.1310/tsr2101-75.
Gandola, M., Toraldo, A., Invernizzi, P., Corrado, L., Sberna, M., Santilli, I., et al. (2013). How many forms of perseveration? Evidence from cancellation tasks in right hemisphere patients. Neuropsychologia, 51(14), 2960–2975. https://doi.org/10.1016/j.neuropsychologia.2013.10.023.
Gauthier, L., Dehaut, F., & Joanette, Y. (1989). The bells test: a quantitative and qualitative test for visual neglect. International journal of clinical neuropsychology, 11(2), 49–54.
Geeraerts, S., Lafosse, C., Vandenbussche, E., & Verfaillie, K. (2005). A psychophysical study of visual extinction: ipsilesional distractor interference with contralesional orientation thresholds in visual hemineglect patients. Neuropsychologia, 43(4), 530–541. https://doi.org/10.1016/j.neuropsychologia.2004.07.012.
Geusgens, C. A. V., Winkens, I., van Heugten, C. M., Jolles, J., & van den Heuvel, W. J. A. (2007). Occurrence and measurement of transfer in cognitive rehabilitation: a critical review. Journal of Rehabilitation Medicine, 39(6), 425–439.
Grattan, E. S., & Woodbury, M. L. (2017). Do neglect assessments detect neglect differently? American Journal of Occupational Therapy, 71(3), 7103190050p1. https://doi.org/10.5014/ajot.2017.025015.
Grossi, D., Modafferi, A., Pelosi, L., & Trojano, L. (1989). On the different roles of the cerebral hemispheres in mental imagery: the “o’Clock Test” in two clinical cases. Brain and Cognition, 10(1), 18–27. https://doi.org/10.1016/0278-2626(89)90072-9.
Guariglia, C., Padovani, A., Pantano, P., & Pizzamiglio, L. (1993). Unilateral neglect restricted to visual imagery. Nature, 364(6434), 235–237. https://doi.org/10.1038/364235a0.
Halligan, P. W., Cockburn, J., & Wilson, B. A. (1991). The behavioural assessment of visual neglect. Neuropsychological Rehabilitation, 1(1), 5–32. https://doi.org/10.1080/09602019108401377.
Halligan, P. W., Fink, G. R., Marshall, J. C., & Vallar, G. (2003). Spatial cognition: evidence from visual neglect. Trends in Cognitive Sciences, 7(3), 125–133. https://doi.org/10.1016/S1364-6613(03)00032-9.
Halligan, P. W., Marshall, J. C., & Wade, D. T. (1989). Visuospatial neglect: underlying factors and test sensitivity. The Lancet, 334(8668), 908–911. https://doi.org/10.1016/S0140-6736(89)91561-4.
Heilman, K. M., Valenstein, E., & Watson, R. T. (2000). Neglect and related Disorders. Seminars in Neurology, 20(04), 463–470. https://doi.org/10.1055/s-2000-13179.
Heilman, K. M., Watson, R. T., & Valenstein, E. (2003). Neglect and related disorders.
Holleman, G. A., Hooge, I. T. C., Kemner, C., & Hessels, R. S. (2020). The ‘Real-World Approach’ and its problems: a critique of the term ecological validity. Frontiers in Psychology, 11, 721. https://doi.org/10.3389/fpsyg.2020.00721.
Hooper, E. H. (1983). Hooper visual organization test (VOT). Western Psychological Services.
Howard, I. P. (1982). Human visual orientation. John Wiley & Sons.
Ishiai, S., Furukawa, T., & Tsukagoshi, H. (1989). Visuospatial processes of line bisection and the mechanisms underlying unilateral spatia neglect. Brain, 112(6), 1485–1502. https://doi.org/10.1093/brain/112.6.1485.
Isiai, S. (1999). Behavioural inattention test, japanese edition. Tokyo, Japan: Shinkoh Igaku Shuppan, Co, Ltd.
Jee, H., Kim, J., Kim, C., Kim, T., & Park, J. (2015). Feasibility of a semi-computerized line bisection test for Unilateral Visual Neglect Assessment. Applied Clinical Informatics, 06(02), 400–417. https://doi.org/10.4338/ACI-2015-01-RA-0002.
Jewell, G., & McCourt, M. E. (2000). Pseudoneglect: a review and meta-analysis of performance factors in line bisection tasks. Neuropsychologia, 38(1), 93–110. https://doi.org/10.1016/S0028-3932(99)00045-7.
Kan, K. C., Subramaniam, P., Shahrizaila, N., Kamaruzzaman, S. B., Razali, R., & Ghazali, S. E. (2019). Validation of the malay version of Addenbrooke’s cognitive examination III in detecting mild cognitive impairment and dementia. Dementia and Geriatric Cognitive Disorders Extra, 9(1), 66–76. https://doi.org/10.1159/000495107.
Karnath, H. O., & Rorden, C. (2012). The anatomy of spatial neglect. Neuropsychologia, 50(6), 1010–1017. https://doi.org/10.1016/j.neuropsychologia.2011.06.027.
Kennedy, R. S., Lane, N. E., Berbaum, K. S., & Lilienthal, M. G. (1993). Simulator Sickness Questionnaire: an enhanced method for quantifying Simulator sickness. The International Journal of Aviation Psychology, 3(3), 203–220. https://doi.org/10.1207/s15327108ijap0303_3.
Kerkhoff, G., & Schenk, T. (2012). Rehabilitation of neglect: an update. Neuropsychologia, 50(6), 1072–1079.
Kertesz, A. (1982). Western aphasia battery test manual. Psychological Corporation.
Kühberger, A., Fritz, A., & Scherndl, T. (2014). Publication Bias in psychology: a diagnosis based on the correlation between Effect size and sample size. Plos One, 9(9), e105825. https://doi.org/10.1371/journal.pone.0105825.
Kim, D. Y., Ku, J., Chang, W. H., Park, T. H., Lim, J. Y., Han, K., et al. (2010). Assessment of post-stroke extrapersonal neglect using a three-dimensional immersive virtual street crossing program. Acta Neurologica Scandinavica, 121(3), 171–177. https://doi.org/10.1111/j.1600-0404.2009.01194.x.
Kim, T. L., Kim, K., Choi, C., Lee, J. Y., & Shin, J. H. (2021). FOPR test: a virtual reality-based technique to assess field of perception and field of regard in hemispatial neglect. Journal of NeuroEngineering and Rehabilitation, 18(1), 39. https://doi.org/10.1186/s12984-021-00835-1.
Kim, Y. M., Chun, M. H., Yun, G. J., Song, Y. J., & Young, H. E. (2011). The effect of virtual reality training on unilateral spatial neglect in stroke patients. Annals of rehabilitation medicine, 35(3), 309.
Kinsbourne, M., & Warrington, E. K. (1962). A variety of reading disability associated with right hemisphere lesions. Journal of Neurology Neurosurgery and Psychiatry, 25(4), 339.
Klatzky, R. L. (1998). Allocentric and egocentric spatial representations: definitions, distinctions, and interconnections (pp. 1–17). Presented at the Spatial cognition, Springer.
Kleinman, J., Dubois, J. C., Newhart, M., & Hillis, A. E. (2013). Disentangling the neuroanatomical correlates of perseveration from unilateral spatial neglect. Behavioural Neurology, 26(1–2), 131–138. https://doi.org/10.1155/2013/438965.
Knobel, S. E. J., Kaufmann, B. C., Gerber, S. M., Cazzoli, D., Müri, R. M., Nyffeler, T., & Nef, T. (2020). Immersive 3D virtual reality Cancellation Task for Visual Neglect Assessment: a pilot study. Frontiers in Human Neuroscience, 14, 180. https://doi.org/10.3389/fnhum.2020.00180.
Kocanaogullari, D., Mak, J., Kersey, J., Khalaf, A., Ostadabbas, S., Wittenberg, G. (2020). EEG-based Neglect Detection for Stroke Patients. In 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC) (pp. 264–267). Presented at the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) in conjunction with the 43rd Annual Conference of the Canadian Medical and Biological Engineering Society, Montreal, QC, Canada: IEEE. https://doi.org/10.1109/EMBC44109.2020.9176378
Kourtesis,., Korre, D., Collina, S., Doumas, L. A. A., & MacPherson, S. E. (2020). Guidelines for the development of immersive virtual reality Software for Cognitive Neuroscience and Neuropsychology: the development of virtual reality Everyday Assessment Lab (VR-EAL), a neuropsychological test battery in immersive virtual reality. Frontiers in Computer Science, 1, 12. https://doi.org/10.3389/fcomp.2019.00012.
Kourtesis, P., Collina, S., Doumas, L. A. A., & MacPherson, S. E. (2019a). Technological competence is a pre-condition for effective implementation of virtual reality head mounted Displays in Human Neuroscience: a Technological Review and Meta-Analysis. Frontiers in Human Neuroscience, 13, 342. https://doi.org/10.3389/fnhum.2019.00342.
Kourtesis, P., Collina, S., Doumas, L. A. A., & MacPherson, S. E. (2019b). Validation of the virtual reality Neuroscience Questionnaire: Maximum Duration of Immersive virtual reality Sessions without the Presence of Pertinent adverse symptomatology. Frontiers in Human Neuroscience, 13, 417. https://doi.org/10.3389/fnhum.2019.00417.
Kourtesis, P., & MacPherson, S. E. (2021). How immersive virtual reality methods may meet the criteria of the National Academy of Neuropsychology and American Academy of Clinical Neuropsychology: A software review of the virtual reality Everyday Assessment Lab (VR-EAL). Computers in Human Behavior Reports, 4, 100151. https://doi.org/10.1016/j.chbr.2021.100151.
Làdavas, E. (1990). Selective spatial attention in patients with visual extinction. Brain, 113(5), 1527–1538. https://doi.org/10.1093/brain/113.5.1527.
Lee, B. H., Kang, S. J., Park, J. M., Son, Y., Lee, K. H., Adair, J. C., et al. (2004). The character-line Bisection Task: a new test for hemispatial neglect. Neuropsychologia, 42(12), 1715–1724. https://doi.org/10.1016/j.neuropsychologia.2004.02.015.
Levine, D. N., Warach, J. D., Benowitz, L., & Calvanio, R. (1986). Left spatial neglect: Effects of lesion size and premorbid brain atrophy on severity and recovery following right cerebral infarction. Neurology, 36(3), 362–362. https://doi.org/10.1212/WNL.36.3.362.
Lezak, M. D., Howieson, D. B., Bigler, E., & Tranel, D. (1995). Neuropsychological assessment (5th ed.). 9780195395525?cc=it〈=en&: Oxford University Press. https://global.oup.com/academic/product/neuropsychological-assessment.
Liang, Y., Guest, R. M., Fairhurst, M. C., & Potter, J. M. (2010). A computer-based quantitative assessment of visuo-spatial neglect using regression and data transformation.Pattern Analysis and Applications, 13(4),409–422. https://doi.org/10.1007/s10044-009-0172-z
Machner, B., Könemund, I., von der Gablentz, J., Bays, P. M., & Sprenger, A. (2018). The ipsilesional attention bias in right-hemisphere stroke patients as revealed by a realistic visual search task: neuroanatomical correlates and functional relevance. Neuropsychology, 32(7), 850–865. https://doi.org/10.1037/neu0000493.
Mainetti, R., Sedda, A., Ronchetti, M., Bottini, G., & Borghese, N. A. (2013). Duckneglect: video-games based neglect rehabilitation. Technology and Health Care, 21(2), 97–111. https://doi.org/10.3233/THC-120712.
Maister, L., Slater, M., Sanchez-Vives, M. V., & Tsakiris, M. (2015). Changing bodies changes minds: owning another body affects social cognition. Trends in Cognitive Sciences, 19(1), 6–12. https://doi.org/10.1016/j.tics.2014.11.001.
Mancuso, M., Rosadoni, S., Capitani, D., Bickerton, W. L., Humphreys, G. W., De Tanti, A., et al. (2015). Italian standardization of the Apples Cancellation Test. Neurological Sciences, 36(7), 1233–1240. https://doi.org/10.1007/s10072-015-2088-2.
Massironi, M., Antonucci, G., Pizzamiglio, L., Vitale, M. V., & Zoccolotti, P. (1988). The Wundt-Jastrow illusion in the study of spatial hemi-inattention. Neuropsychologia, 26(1), 161–166. https://doi.org/10.1016/0028-3932(88)90039-5.
McIntosh, R. D., Brodie, E. E., Beschin, N., & Robertson, I. H. (2000). Improving the clinical diagnosis of personal neglect: a reformulated comb and Razor Test. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 36(2), 289–292. https://doi.org/10.1016/S0010-9452(08)70530-6.
Meador, K. J., Loring, D. W., Bowers, D., & Heilman, K. M. (1987). Remote memory and neglect syndrome. Neurology, 37(3), 522–522. https://doi.org/10.1212/WNL.37.3.522.
Menon, A., & Korner-Bitensky, N. (2004). Evaluating unilateral spatial neglect Post Stroke: working your way through the maze of Assessment Choices. Topics in Stroke Rehabilitation, 11(3), 41–66. https://doi.org/10.1310/KQWL-3HQL-4KNM-5F4U.
Mesa-Gresa, P., Lozano, J. A., Llórens, R., Alcañiz, M., Navarro, M. D., & Noé, E. (2011). Clinical validation of a virtual environment test for safe street crossing in the assessment of acquired brain injury patients with and without neglect (pp. 44–51). Presented at the IFIP Conference on Human-Computer Interaction, Springer.
Milner, A. D., Harvey, M., Roberts, R. C., & Forster, S. V. (1993). Line bisection errors in visual neglect: misguided action or size distortion? Neuropsychologia, 31(1), 39–49. https://doi.org/10.1016/0028-3932(93)90079-F.
Mizuno, K., Kato, K., Tsuji, T., Shindo, K., Kobayashi, Y., & Liu, M. (2016). Spatial and temporal dynamics of visual search tasks distinguish subtypes of unilateral spatial neglect: comparison of two cases with viewer-centered and stimulus-centered neglect. Neuropsychological Rehabilitation, 26(4), 610–634. https://doi.org/10.1080/09602011.2015.1051547.
Montedoro, V., Alsamour, M., Dehem, S., Lejeune, T., Dehez, B., & Edwards, M. G. (2019). Robot diagnosis test for egocentric and allocentric hemineglect. Archives of Clinical Neuropsychology, 34(4), 481–494. https://doi.org/10.1093/arclin/acy062.
Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18, 1–7.
Murphy, T. H., & Corbett, D. (2009). Plasticity during stroke recovery: from synapse to behaviour. Nature Reviews Neuroscience, 10(12), 861–872. https://doi.org/10.1038/nrn2735.
Neguț, A., Matu, S. A., Sava, F. A., & David, D. (2016). Virtual reality measures in neuropsychological assessment: a meta-analytic review. The Clinical Neuropsychologist, 30(2), 165–184. https://doi.org/10.1080/13854046.2016.1144793.
Niedeggen, M., & Jörgens, S. (2005). Visuelle Wahrnehmungsstörungen (5 vol.). Hogrefe Verlag.
Nijboer, T., van de Port, I., Schepers, V., Post, M., & Visser-Meily, A. (2013). Predicting Functional Outcome after Stroke: the influence of neglect on Basic Activities in Daily Living. Frontiers in Human Neuroscience, 7. https://doi.org/10.3389/fnhum.2013.00182.
Ogden, J. A. (1985). Contralesional neglect of constructed visual images in right and left brain-damaged patients. Neuropsychologia, 23(2), 273–277. https://doi.org/10.1016/0028-3932(85)90112-5.
Ogourtsova, T., Archambault, P. S., & Lamontagne, A. (2018a). Post-stroke unilateral spatial neglect: virtual reality-based navigation and detection tasks reveal lateralized and non-lateralized deficits in tasks of varying perceptual and cognitive demands. Journal of NeuroEngineering and Rehabilitation, 15(1), 34. https://doi.org/10.1186/s12984-018-0374-y.
Ogourtsova, T., Archambault, P. S., Sangani, S., & Lamontagne, A. (2018b). Ecological virtual reality evaluation of neglect symptoms (EVENS): Effects of virtual scene complexity in the Assessment of Poststroke unilateral spatial neglect. Neurorehabilitation and Neural Repair, 32(1), 46–61. https://doi.org/10.1177/1545968317751677.
Ogourtsova, T., Souza Silva, W., Archambault, P. S., & Lamontagne, A. (2017). Virtual reality treatment and assessments for post-stroke unilateral spatial neglect: a systematic literature review. Neuropsychological Rehabilitation, 27(3), 409–454. https://doi.org/10.1080/09602011.2015.1113187.
Ota, H., Fujii, T., Suzuki, K., Fukatsu, R., & Yamadori, A. (2001). Dissociation of body-centered and stimulus-centered representations in unilateral neglect. Neurology, 57(11), 2064–2069. https://doi.org/10.1212/WNL.57.11.2064.
Ota, H., Fujii, T., Tabuchi, M., Sato, K., Saito, J., & Yamadori, A. (2003). Different spatial processing for stimulus-centered and body-centered representations. Neurology, 60(11), 1846–1848. https://doi.org/10.1212/01.WNL.0000065899.22903.07.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4.
Pallavicini, F., Pedroli, E., Serino, S., Dell’Isola, A., Cipresso, P., Cisari, C., & Riva, G. (2015). Assessing unilateral spatial neglect using advanced technologies: the potentiality of mobile virtual reality. Technology and Health Care, 23(6), 795–807. https://doi.org/10.3233/THC-151039.
Parsons, T. D. (2015). Virtual reality for enhanced ecological validity and experimental control in the Clinical, Affective and Social Neurosciences. Frontiers in Human Neuroscience, 9. https://doi.org/10.3389/fnhum.2015.00660.
Paterson, A., & Zangwill, O. L. (1944). Disorders of visual space perception associated with lesions of the right cerebral hemisphere. Brain, 67(4), 331–358.
Pedroli, E., Serino, S., Cipresso, P., Pallavicini, F., & Riva, G. (2015). Assessment and rehabilitation of neglect using virtual reality: a systematic review. Frontiers in Behavioral Neuroscience, 9. https://doi.org/10.3389/fnbeh.2015.00226.
Peru, A., Bollini, A., Costanzo, S., Dainelli, M., Landucci, L., Pezzatini, D., et al. (2017). Towards a dynamic Assessment of unilateral spatial neglect. The Open Psychology Journal, 10(1), 71–80. https://doi.org/10.2174/1874350101710010071.
Peskine, A., Rosso, C., Box, N., Galland, A., Caron, E., Rautureau, G., et al. (2011). Virtual reality assessment for visuospatial neglect: importance of a dynamic task. Journal of Neurology Neurosurgery & Psychiatry, 82(12), 1407–1409. https://doi.org/10.1136/jnnp.2010.217513.
Pierce, J. E., Ronchi, R., Thomasson, M., Rossi, I., Casati, C., Saj, A., et al. (2021). A novel computerized assessment of manual spatial exploration in unilateral spatial neglect. Neuropsychological Rehabilitation, 1–22. https://doi.org/10.1080/09602011.2021.1875850.
Pizzamiglio, L., Judica, A., Razzano, C., & Zoccolotti, P. (1989). Toward a comprehensive diagnosis of visual-spatial disorders in unilateral brain damaged patients. Evaluación Psicológica.
Ptak, R., & Schnider, A. (2011). The attention network of the human brain: relating structural damage associated with spatial neglect to functional imaging correlates of spatial attention. Neuropsychologia, 49(11), 3063–3070. https://doi.org/10.1016/j.neuropsychologia.2011.07.008.
Quinn, T. J., Livingstone, I., Weir, A., Shaw, R., Breckenridge, A., McAlpine, C., & Tarbert, C. M. (2018). Accuracy and feasibility of an android-based Digital Assessment Tool for Post Stroke Visual Disorders—The StrokeVision App. Frontiers in Neurology, 9, 146. https://doi.org/10.3389/fneur.2018.00146.
Rabuffetti, M., Farina, E., Alberoni, M., Pellegatta, D., Appollonio, I., Affanni, P., et al. (2012). Spatio-temporal features of Visual Exploration in unilaterally brain-damaged subjects with or without neglect: results from a touchscreen test. Plos One, 7(2), e31511. https://doi.org/10.1371/journal.pone.0031511.
Rabuffetti, M., Ferrarin, M., Spadone, R., Pellegatta, D., Gentileschi, V., Vallar, G., & Pedotti, A. (2002). Touch-screen system for assessing visuo-motor exploratory skills in neuropsychological disorders of spatial cognition. Medical & Biological Engineering & Computing, 40(6), 675–686. https://doi.org/10.1007/BF02345306.
Rand, D., Kizony, R., & Weiss, P. T. L. (2008). The Sony PlayStation II EyeToy: low-cost virtual reality for use in rehabilitation. Journal of neurologic physical therapy, 32(4), 155–163.
Rehme, A. K., Eickhoff, S. B., Rottschy, C., Fink, G. R., & Grefkes, C. (2012). Activation likelihood estimation meta-analysis of motor-related neural activity after stroke. Neuroimage, 59(3), 2771–2782. https://doi.org/10.1016/j.neuroimage.2011.10.023.
Reinhart, S., Leonhard, E., & Kerkhoff, G. (2016). Sensitive neglect test (SNT) single and dual task. Saarbrücken: Saarland University.
Ringman, J. M., Saver, J. L., Woolson, R. F., Clarke, W. R., & Adams, H. P. (2004). Frequency, risk factors, anatomy, and course of unilateral neglect in an acute stroke cohort. Neurology, 63(3), 468–474. https://doi.org/10.1212/01.WNL.0000133011.10689.CE.
Rizzo, A. A., Schultheis, M., Kerns, K. A., & Mateer, C. (2004). Analysis of assets for virtual reality applications in neuropsychology. Neuropsychological Rehabilitation, 14(1–2), 207–239. https://doi.org/10.1080/09602010343000183.
Robey, R. R., Schultz, M. C., Crawford, A. B., & Sinner, C. A. (1999). Single-subject clinical-outcome research: designs, data, effect sizes, and analyses. Aphasiology, 13(6), 445–473.
Rode, G., Michel, C., Rossetti, Y., Boisson, D., & Vallar, G. (2006). Left size distortion (hyperschematia) after right brain damage. Neurology, 67(10), 1801–1808. https://doi.org/10.1212/01.wnl.0000244432.91915.d0.
Rode, G., Perenin, M. T., & Boisson, D. (1995). Neglect of the representational space: demonstration by mental evocation of the map of France. Revue neurologique, 151(3), 161–164.
Ronchi, R., Algeri, L., Chiapella, L., Gallucci, M., Spada, M. S., & Vallar, G. (2016). Left neglect dyslexia: perseveration and reading error types. Neuropsychologia, 89, 453–464. https://doi.org/10.1016/j.neuropsychologia.2016.07.023.
Ronchi, R., Algeri, L., Chiapella, L., Spada, M. S., & Vallar, G. (2012). Spatial neglect and perseveration in visuomotor exploration. Neuropsychology, 26(5), 588–603. https://doi.org/10.1037/a0029216.
Ronchi, R., Posteraro, L., Fortis, P., Bricolo, E., & Vallar, G. (2009). Perseveration in left spatial neglect: drawing and cancellation tasks. Cortex; A Journal Devoted To The Study Of The Nervous System And Behavior, 45(3), 300–312. https://doi.org/10.1016/j.cortex.2008.03.012.
Rorden, C., & Karnath, H. O. (2010). A simple measure of neglect severity. Neuropsychologia, 48(9), 2758–2763. https://doi.org/10.1016/j.neuropsychologia.2010.04.018.
Rossa, T., Pompidor, P., Rodriguez, N., Sallaberry, A., Poncelet, P., Urbanski, M. (2019). Experimental web service and eye-tracking setup for unilateral spatial neglect assessment (pp. 141–155). Presented at the International Conference on Human-Computer Interaction, Springer.
Rusconi, M. L., Maravita, A., Bottini, G., & Vallar, G. (2002). Is the intact side really intact? Perseverative responses in patients with unilateral neglect: a productive manifestation. Neuropsychologia, 40(6), 594–604. https://doi.org/10.1016/S0028-3932(01)00160-9.
Schendel, K. L., & Robertson, L. C. (2002). Using reaction time to assess patients with unilateral neglect and extinction. Journal of Clinical and Experimental Neuropsychology, 24(7), 941–950. https://doi.org/10.1076/jcen.24.7.941.8390.
Schenkenberg, T., Bradford, D. C., & Ajax, E. T. (1980). Line bisection and unilateral visual neglect in patients with neurologic impairment. Neurology, 30(5), 509–509. https://doi.org/10.1212/WNL.30.5.509.
Schwartz, M. F., Segal, M., Veramonti, T., Ferraro, M., & Buxbaum, L. J. (2002). The naturalistic action test: a standardised assessment for everyday action impairment. Neuropsychological Rehabilitation, 12(4), 311–339. https://doi.org/10.1080/09602010244000084.
Sedda, A., Borghese, N. A., Ronchetti, M., Mainetti, R., Pasotti, F., Beretta, G., & Bottini, G. (2013). Using virtual reality to rehabilitate neglect. Behavioural Neurology, 26(3), 183–185. https://doi.org/10.1155/2013/810279.
Siéroff, E. (2017). Acquired spatial dyslexia. Annals of Physical and Rehabilitation Medicine, 60(3), 155–159. https://doi.org/10.1016/j.rehab.2015.07.004.
Slater, M. (2009). Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philosophical Transactions of the Royal Society B: Biological Sciences, 364(1535), 3549–3557. https://doi.org/10.1098/rstb.2009.0138.
Slater, M. (2018). Immersion and the illusion of presence in virtual reality. British Journal of Psychology, 109(3), 431–433. https://doi.org/10.1111/bjop.12305.
Smit, M., Van der Stigchel, S., Visser-Meily, J. M. A., Kouwenhoven, M., Eijsackers, A. L. H., & Nijboer, T. C. W. (2013). The feasibility of computer-based prism adaptation to ameliorate neglect in Sub-Acute Stroke Patients admitted to a Rehabilitation Center. Frontiers in Human Neuroscience, 7. https://doi.org/10.3389/fnhum.2013.00353.
Sotokawa, T., Murayama, T., Noguchi, J., Sakimura, Y., & Itoh, M. (2015). Driving evaluation of mild unilateral spatial neglect patients–three high-risk cases undetected by BIT after Recovery. In S. Yamamoto (Ed.), Human interface and the management of information. Information and knowledge in Context (9173 vol., pp. 253–261). Cham: Springer International Publishing. https://doi.org/10.1007/978-3-319-20618-9_25.
Sportillo, D., Paljic, A., Boukhris, M., Fuchs, P., Ojeda, L., & Roussarie, V. (2017). An Immersive Virtual Reality System for Semi-autonomous Driving Simulation: A Comparison between Realistic and 6-DoF Controller-based Interaction. In Proceedings of the 9th International Conference on Computer and Automation Engineering - ICCAE ’17 (pp. 6–10). Presented at the the 9th International Conference, Sydney, Australia: ACM Press. https://doi.org/10.1145/3057039.3057079
Spreij, L. A., Brink, T., Visser-Meily, A. F., J. M. A., & Nijboer, T. C. W. (2020). Simulated driving: the added value of dynamic testing in the assessment of visuo‐spatial neglect after stroke. Journal of Neuropsychology, 14(1), 28–45. https://doi.org/10.1111/jnp.12172.
Stefaniak, J. D., Halai, A. D., & Lambon Ralph, M. A. (2020). The neural and neurocomputational bases of recovery from post-stroke aphasia. Nature Reviews Neurology, 16(1), 43–55. https://doi.org/10.1038/s41582-019-0282-1.
Stinear, C. M. (2017). Prediction of motor recovery after stroke: advances in biomarkers. The Lancet Neurology, 16(10), 826–836. https://doi.org/10.1016/S1474-4422(17)30283-1.
Stone, S. P., Wilson, B., Wroot, A., Halligan, P. W., Lange, L. S., Marshall, J. C., & Greenwood, R. J. (1991). The assessment of visuo-spatial neglect after acute stroke. Journal of Neurology Neurosurgery & Psychiatry, 54(4), 345–350.
Strauss, M. E., & Smith, G. T. (2009). Construct validity: advances in theory and methodology. Annual Review of Clinical Psychology, 5(1), 1–25. https://doi.org/10.1146/annurev.clinpsy.032408.153639.
Sugarman, H., Weisel-Eichler, A., Burstin, A., & Brown, R. (2011). Use of novel virtual reality system for the assessment and treatment of unilateral spatial neglect: A feasibility study (pp. 1–2). Presented at the 2011 International Conference on Virtual Rehabilitation, IEEE.
Swift, A., Heale, R., & Twycross, A. (2020). What are sensitivity and specificity? Evidence Based Nursing, 23(1), 2–4. https://doi.org/10.1136/ebnurs-2019-103225.
Tanaka, T. (2010). Clinical application for assistive engineering-mixed reality rehabilitation. Journal of Medical and Biological Engineering, 31(4), 277–282.
Teuber, H. L. (1955). Physiological psychology. Annual review of psychology, 6(1), 267–296.
Tham, K. (1996). The Baking Tray Task: a test of spatial neglect. Neuropsychological Rehabilitation, 6(1), 19–26. https://doi.org/10.1080/713755496.
Toraldo, A., Romaniello, C., & Sommaruga, P. (2017). Measuring and diagnosing unilateral neglect: a standardized statistical procedure. The Clinical Neuropsychologist, 31(6–7), 1248–1267. https://doi.org/10.1080/13854046.2017.1349181.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850.
Tsirlin, I., Dupierrix, E., Chokron, S., Coquillart, S., & Ohlmann, T. (2009). Uses of virtual reality for diagnosis, Rehabilitation and Study of unilateral spatial neglect: review and analysis. CyberPsychology & Behavior, 12(2), 175–181. https://doi.org/10.1089/cpb.2008.0208.
Ulm, L., Wohlrapp, D., Meinzer, M., Steinicke, R., Schatz, A., Denzler, P., et al. (2013). A Circle-Monitor for Computerised Assessment of Visual Neglect in Peripersonal Space. Plos One, 8(12), e82892. https://doi.org/10.1371/journal.pone.0082892.
Vaes, N., Lafosse, C., Nys, G., Schevernels, H., Dereymaeker, L., Oostra, K., et al. (2015). Capturing peripersonal spatial neglect: an electronic method to quantify visuospatial processes. Behavior Research Methods, 47(1), 27–44. https://doi.org/10.3758/s13428-014-0448-0.
Vallar, G. (1998). Spatial hemineglect in humans. Trends in Cognitive Sciences, 2(3), 87–97. https://doi.org/10.1016/S1364-6613(98)01145-0.
Vallar, G. (2000). The methodological foundations of human neuropsychology; studies in brain damaged patients. In F. Boller, J. Grafman, & G. Rizzolatti (Eds.), Handbook of Neuropsychology (1 vol., pp. 305–344). Amsterdam, The Netherlands: Elsevier.
Vallar, G., & Bolognini, N. (2014). Unilateral Spatial Neglect. (A. C. Nobre & S. Kastner, Eds.) (Vol. 1). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199675111.013.012
Vallar, G., Bottini, G., Sterzi, R., Passerini, D., & Rusconi, M. L. (1991a). Hemianesthesia, sensory neglect, and defective access to conscious experience. Neurology, 41(5), 650–652. https://doi.org/10.1212/WNL.41.5.650.
Vallar, G., Burani, C., & Arduino, L. S. (2010). Neglect dyslexia: a review of the neuropsychological literature. Experimental Brain Research, 206(2), 219–235. https://doi.org/10.1007/s00221-010-2386-0.
Vallar, G., & Calzolari, E. (2018). Unilateral spatial neglect after posterior parietal damage. In Handbook of Clinical Neurology (Vol. 151, pp. 287–312). Elsevier. https://doi.org/10.1016/B978-0-444-63622-5.00014-0
Vallar, G., & Caputi, N. (2021). The History of Human Neuropsychology. In S. Della Sala (Ed.), Encyclopedia of Behavioral Neuroscience (Vol. 1, pp. 14–39). Elsevier. https://doi.org/10.1016/b978-0-12-809324-5.23914-x
Vallar, G., Daini, R., & Antonucci, G. (2000). Processing of illusion of length in spatial hemineglect: a study of line bisection. Neuropsychologia, 38(7), 1087–1097. https://doi.org/10.1016/S0028-3932(99)00139-6.
Vallar, G., & Maravita, A. (2009). Personal and extrapersonal spatial perception. In G. G. Berntson, & J. T. Cacioppo (Eds.), Handbook of Neuroscience for the behavioral Sciences (p. neubb001016). Hoboken, NJ, USA: John Wiley & Sons, Inc. https://doi.org/10.1002/9780470478509.neubb001016.
Vallar, G., & Perani, D. (1986). The anatomy of unilateral neglect after right-hemisphere stroke lesions. A clinical/CT-scan correlation study in man. Neuropsychologia, 24(5), 609–622. https://doi.org/10.1016/0028-3932(86)90001-1.
Vallar, G., & Ronchi, R. (2009). Somatoparaphrenia: a body delusion. A review of the neuropsychological literature. Experimental Brain Research, 192(3), 533–551. https://doi.org/10.1007/s00221-008-1562-y.
Vallar, G., Rusconi, M. L., Fontana, S., & Musicco, M. (1994). Tre test di esplorazione visuo-spaziale: taratura su 212 soggetti normali. Archivio di Psicologia, Neurologia e Psichiatria.
Vallar, G., Sandroni, P., Rusconi, M. L., & Barbieri, S. (1991b). Hemianopia, hemianesthesia, and spatial neglect: a study with evoked potentials. Neurology, 41(12), 1918–1918. https://doi.org/10.1212/WNL.41.12.1918.
Van der Stigchel, S., & Nijboer, T. C. W. (2010). The imbalance of oculomotor capture in unilateral visual neglect. Consciousness and Cognition, 19(1), 186–197. https://doi.org/10.1016/j.concog.2009.11.003.
Van der Stoep, N., Visser-Meily, J. M. A., Kappelle, L. J., de Kort, P. L. M., Huisman, K. D., Eijsackers, A. L. H., et al. (2013). Exploring near and far regions of space: Distance-specific visuospatial neglect after stroke. Journal of Clinical and Experimental Neuropsychology, 35(8), 799–811. https://doi.org/10.1080/13803395.2013.824555.
Villarreal, S., Linnavuo, M., Sepponen, R., Vuori, O., Bonato, M., Jokinen, H., & Hietanen, M. (2021). Unilateral stroke: computer-based Assessment uncovers non-lateralized and Contralesional Visuoattentive deficits. Journal of the International Neuropsychological Society, 1–11. https://doi.org/10.1017/S1355617720001393.
Villarreal, S., Linnavuo, M., Sepponen, R., Vuori, O., Bonato, M., Jokinen, H., & Hietanen, M. (2022). Computer-based Assessment: Dual-Task outperforms large-screen Cancellation Task in detecting Contralesional Omissions. Frontiers in Psychology, 12, 790438. https://doi.org/10.3389/fpsyg.2021.790438.
Villarreal, S., Linnavuo, M., Sepponen, R., Vuori, O., Jokinen, H., & Hietanen, M. (2020). Dual-Task in large Perceptual Space reveals subclinical hemispatial neglect. Journal of the International Neuropsychological Society, 26(10), 993–1005. https://doi.org/10.1017/S1355617720000508.
Walker, R. (1995). Spatial and object-based neglect. Neurocase, 1(4), 371–383. https://doi.org/10.1080/13554799508402381.
Wechsler, D. (2009). WMS-IV: Wechsler memory scale. Pearson.
Wechsler, D. (2012). November 12). Wechsler Adult Intelligence Scale–Fourth Edition. American Psychological Association. https://doi.org/10.1037/t15169-000.
Weintraub, S., & Mesulam, M. M. (1988). Visual hemispatial inattention: stimulus parameters and exploratory strategies. Journal of Neurology Neurosurgery & Psychiatry, 51(12), 1481–1488. https://doi.org/10.1136/jnnp.51.12.1481.
Weisenberg, T., & McBride, K. E. (1935). Aphasia: a clinical and psychological study. Aphasia: a clinical and psychological study. The Commonwealth Fund.
Willer, L., Pedersen, P. M., Forchhammer, H. B., & Christensen, H. (2016). Cognitive assessment at bedside for iPad: a preliminary validation of a novel cognitive test for stroke patients. European Stroke Journal, 1(4), 294–301. https://doi.org/10.1177/2396987316665233.
Wilson, B., Cockburn, J., & Halligan, P. W. (1987). Behavioural inattention test thames valley test company: Titchfield. Hampshire, UK.
Yesavage, J. A., & Sheikh, J. I. (1986). 9/Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist, 5(1–2), 165–173. https://doi.org/10.1300/J018v05n01_09.
Zhang, J., Yu, J., Bao, Y., Xie, Q., Xu, Y., Zhang, J., & Wang, P. (2017). Constraint-induced aphasia therapy in post-stroke aphasia rehabilitation: a systematic review and meta-analysis of randomized controlled trials. PLOS ONE, 12(8), e0183349. https://doi.org/10.1371/journal.pone.0183349.
Zimmermann, P., & Fimm, B. (2002). In P. Z. M. Leclercq (Ed.), A test battery for attentional performance. Theory, diagnosis and rehabilitation.
Zoccolotti, P., Antonucci, G., & Judica, A. (1992). Psychometric characteristics of two semi-structured scales for the functional evaluation of hemi-inattention in extrapersonal and personal space. Neuropsychological Rehabilitation, 2(3), 179–191. https://doi.org/10.1080/09602019208401407.
Zoccolotti, P., Antonucci, G., Judica, A., Montenero, P., Pizzamiglio, L., & Razzano, C. (1989). Incidence and evolution of the Hemineglect disorder in chronic patients with unilateral right brain damage. International Journal of Neuroscience, 47(3–4), 209–216. https://doi.org/10.3109/00207458908987435.
Zoccolotti, P., & Judica, A. (1991). Functional evaluation of hemineglect by means of a semistructured scale: personal extrapersonal differentiation. Neuropsychological Rehabilitation, 1(1), 33–44. https://doi.org/10.1080/09602019108401378.
Funding
This research received funding to Giuseppe Vallar from the Fondo di Ateneo per la Ricerca of the University of Milano Bicocca and from the Fondi per la Ricerca Corrente by the IRCCS Istituto Auxologico Italiano. This research received also funding to Alberto Gallace from the Fondo di Ateneo per la Ricerca of the University of Milano Bicocca.
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Stefano Terruzzi: Methodology, Investigation, Visualization, Data curation, Writing - Original draft, Supervision. Federica Albini: Investigation, Visualization, Data curation, Writing - Original draft. Gemma Massetti: Investigation, Visualization, Data curation, Writing - Original draft. Roberta Etzi: Investigation, Visualization, Data curation, Writing - Review & Editing. Alberto Gallace: Conceptualization, Methodology, Writing - Review & Editing, Supervision, Funding acquisition. Giuseppe Vallar: Conceptualization, Methodology, Writing - Review & Editing, Supervision, Project administration, Funding acquisition.
Corresponding authors
Ethics declarations
Declaration of Interest
none.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Terruzzi, S., Albini, F., Massetti, G. et al. The Neuropsychological Assessment of Unilateral Spatial Neglect Through Computerized and Virtual Reality Tools: A Scoping Review. Neuropsychol Rev 34, 363–401 (2024). https://doi.org/10.1007/s11065-023-09586-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-023-09586-3