Abstract
Purpose
Seizures are a common clinical occurrence in high-grade glioma (HGG). While many studies have explored seizure incidence and prevalence in HGG, limited studies have examined the prognostic effect of seizures occurring in the post-diagnosis setting. This study aims to assess the impact of seizure presentation on HGG survival outcomes.
Methods
Single-center retrospective review identified 950 patients with histologically-confirmed high-grade glioma. Seizure presentation was determined by clinical history and classified as early onset (occurring within 30 days of HGG presentation) or late onset (first seizure occurring after beginning HGG treatment). The primary outcome, hazard ratios for overall survival and progression-free survival, was assessed with multivariable Cox proportional-hazards models. IDH1 mutation status (assessed through immunohistochemistry) was only consistently available beginning in 2015; subgroup analyses were performed in the subset of patients with known IDH1 status.
Results
Epileptic activity before (HR = 0.81, 95% CI = 0.68–0.96, P = 0.017) or after (HR = 0.74, 95% CI = 0.60–0.91, P = 0.005) HGG diagnosis associated with improved overall survival. Additionally, late seizure onset significantly associated with lower odds of achieving partial (OR = 0.25, 95% CI = 0.12–0.53, P = < 0.001) or complete (OR = 0.30, 95% CI = 0.18–0.50, P < 0.001) seizure control than patients with early seizure onset.
Conclusions
Clinical seizures both at the time of diagnosis and later during the HGG treatment course are associated with improved overall survival. This association potentially persists for both IDH1-wildtype and IDH1-mutant patients, but further study is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-grade gliomas (HGG), a group of infiltrative neoplasms including Grade IV IDH-wildtype astrocytoma (formerly glioblastoma multiforme; GBM), currently affect between 0.59 and 5 individuals per 100,000 population per year [1]. In 2021, the World Health Organization (WHO) amended its definition of GBM to follow genetic guidelines in addition to histological guidelines, requiring a diagnosis of GBM to lack isocitrate-dehydrogenase 1 and 2 mutations (IDH-wildtype); IDH-mutant grade IV gliomas are now termed IDH-mutant astrocytomas [2].
Seizures are a common clinical occurrence throughout the disease course in HGG, estimated to affect 30–60% of patients with HGG [3, 4]. While many studies have explored the impact of surgical and medical HGG treatment on seizure incidence and prevalence, limited studies have assessed the prognostic effect of seizures occurring in the post-treatment setting [5, 6].
Recently, a positive seizure history at initial HGG presentation has been shown to associate with improved overall survival: a 2017 meta-analysis of 1,836 GBM patients found reduced mortality with positive seizure history (HR = 0.71, P = < 0.00001); a 2018 meta-analysis of 2,088 patients showed increased mortality with negative seizure history (HR = 1.73, P = < 0.001) [7, 8]. Current theories for the underlying mechanism behind a possible protective effect of seizures in HGG include both cellular theories (such as an association with IDH1 mutation) and clinical theories (such as early detection of HGG through seizure work-up) [7].
In this study, we aimed to retrospectively assess the effects of tumor-related epilepsy in patients with HGG on overall and progression-free survival. Further, we sought to better delineate the temporal relationship between seizure onset and HGG survival to understand whether early or late seizures carry distinct prognoses in tumor-related epilepsy. Given the substantial recent history of including IDH-mutant disease in the umbrella of GBM as well as the uncertainty regarding IDH1 status’s impact, our paper additionally incorporates both IDH-wildtype GBM and IDH-mutant grade IV astrocytomas.
Materials and methods
Participants
We retrospectively reviewed all patients diagnosed with HGG (defined as WHO Grade IV glioma), histologically confirmed by board-certified neuropathologists, at the Cleveland Clinic between 1999 and 2022. For seizure control analyses, only patients with clinically diagnosed epileptic activity (defined based on neurologist-obtained history or direct observation during hospitalization) were included. Electroencephalogram (EEG) data was not included as it was not collected as part of the standard of care for all patients [3].
Data collection
Electronic medical records were queried for relevant clinical factors including: age, sex, extent of surgical resection (defined as gross total resection versus all other surgical procedures), laterality, primary tumor location (defined as frontal lobe, parietal lobe, temporal lobe, occipital lobe, or other location), Karnofsky Performance Score (KPS) at diagnosis, radiation therapy, chemotherapy (cytotoxic), chemotherapy (biological target), IDH1 mutation status, survival duration (progression-free (PFS) and overall (OS)), and presence of epileptic activity. Epileptic activity was classified into three groups: None (no history of epileptic activity), Early Seizure (defined as first seizure occurring within 30 days prior to HGG diagnosis), and Late Seizure (defined as first seizure occurring after HGG diagnosis). “Diagnosis” timepoint was defined as the date of first surgery which provided the tissue sample for histologic confirmation of disease. PFS duration was defined as the time from diagnosis until first progression or recurrence of disease as measured by the Response Assessment in Neuro-Oncology (RANO) criteria [9]; OS was defined as the time from diagnosis until death. Seizure control was classified into three groups: None (never achieved six consecutive seizure-free months), Partial (achieved at least six consecutive seizure-free months, but later relapsed), and Complete (achieved permanent seizure control of at least six consecutive months). Consistent immunohistochemistry for IDH1 mutations was not available until 2015; IDH1 mutation status prior to 2015 was sporadic.
Statistical analysis
Descriptive statistics summarized the patient sample, overall and stratified by seizure status (None, Early Seizure, Late Seizure). Mean with standard deviation or median with interquartile range was used for continuous variables and frequency with percentage was used for categorical variables. Group comparisons were made using one-way analysis of variance (ANOVA) or Kruskal-Wallis test for continuous variables and chi-square or Fisher’s exact test for categorical variables.
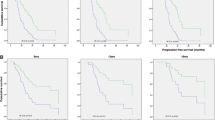
Kaplan-Meier curves were constructed for the overall sample to estimate survival and progression-free survival. To determine if timing and severity of initial seizure presentation, as well as seizure control, were associated with survival and progression-free survival, we fit multivariable Cox proportional hazards models. Surviving patients were censored at their date of last follow-up. Separate models were fit for each outcome (survival and progression-free survival) and for each independent variable of interest (seizure presence, timing of initial seizure [None, Early Seizure, Late Seizure], severity of epileptic disease initial seizure presentation [0, 1, 2 + seizures/month], and seizure control [None, Partial, Complete]). In all models, we adjusted for the following covariates: age, sex, gross total resection (vs. subtotal resection or biopsy), laterality (bilateral vs. right/left), frontal lobe, parietal lobe, temporal lobe, occipital lobe, other location, KPS at diagnosis, radiation therapy, chemotherapy (cytotoxic), and chemotherapy (biological target). We used variance inflation factors (VIFs) to assess for multicollinearity with VIF > 5 indicating multicollinearity.
In order to reduce a potential persistence bias for seizure occurring after diagnosis in patients with long survival duration, we performed an analysis restricting the Late Seizure group to those patients with their first seizure within the 14 months following diagnosis. 14 months was chosen as a cutoff to represent the median survival time in IDH-wildtype HGG, the most common type of HGG [1].
We further examined these models in the subset with known IDH1 wildtype status. Subgroup analysis focusing on seizure control was performed on those patients who had seizures. Seizure control was defined as a categorical variable with three groups: None (never achieved six consecutive seizure-free months), Partial (achieved at least six consecutive seizure-free months, but later relapsed prior to death), and Complete (achieved permanent seizure control of at least six consecutive months). Six months of seizure absence was chosen as the definition for seizure remission. Six months is a commonly-selected window in prior studies of epileptic remission, as well as the most common window required to reattain driving eligibility across US states [10,11,12].
To assess whether seizure timing (Early Seizure vs. Late Seizure) and initial seizure frequency (0, 1, 2 + seizures) were associated with seizure control, we fit two multivariable multinomial logistic regression models where seizure control was the dependent variable.
Results
950 patients with a histologically confirmed diagnosis of HGG treated at the Cleveland Clinic Foundation from 1999 to 2022 meeting inclusion criteria were identified. 414 patients (43.6%) had seizures; of these, 261 (63.0%) had their initial seizure before glioma diagnosis, and 153 (37.0%) had their initial seizure following initiation of glioma treatment. Table 1 shows descriptive statistics of patient and clinical characteristics, stratified by seizure status; patients with no history of seizures were significantly older (P = < 0.001) and less likely to have received chemotherapy (P = < 0.001) than patients with Early or Late seizures, but no significant differences between groups were observed for sex (P = 0.444). Additional demographic and clinical characteristics are provided in Supplementary Table 1. Further, Supplementary Table 2 classifies all included anticancer therapies as cytotoxic chemotherapy, targeted chemotherapy, or immunotherapy. Figure 1 shows overall survival and progression-free survival for the entire sample. Median overall survival time was 13.4 months (95% CI = 12.4–14.3 months). Median progression-free survival was 5.5 months (95% CI = 5.1–6.1 months).
The impact of seizures on overall and progression-free survival
In the full patient cohort (N = 950), seizure timing was associated with prolonged overall survival but not with prolonged progression-free survival (Table 2). Compared to patients who did not have any seizures, patients with seizures had lower risk of death whether they experienced seizures before (HR = 0.81, 95% CI = 0.68–0.96, P = 0.017) or after (HR = 0.74, 95% CI = 0.60–0.91, P = 0.005) glioma diagnosis. Initial seizure frequency was not associated with overall survival (omnibus p-value = 0.968) or progression-free survival (omnibus p-value = 0.548).
Of the 153 patients who had their first seizure post-glioma diagnosis, 120 (78.4%) had their first seizure within 14 months after glioma diagnosis. When restricting the Late Seizure group to these 120 patients, patients in the Early Seizure group still had lower risk of death than patients who never had seizures (HR = 0.80, 95% CI = 0.67–0.95, P = 0.011); however, the Late Seizure group did not have significantly different risk of death than the no-seizure group (HR = 0.89, 95% CI = 0.72–1.12, P = 0.324) (Table 2).
Patients who had any seizures displayed significantly reduced risk of death compared to those who never had seizures (Table 2). This association was seen when analyzing all patients (HR = 0.78, 95% CI = 0.67–0.91, P = 0.002) and when excluding patients whose post-glioma seizure diagnosis was greater than 14 months from diagnosis (HR = 0.83, 95% CI = 0.71–0.97, P = 0.017). Further, patients with seizures had significantly lower risk of progression when considering all patients (HR = 0.84, 95% CI = 0.73–0.97, P = 0.020) but not when excluding patients with post-glioma seizures beginning more than 14 months following glioma diagnosis (HR = 0.90, 95% CI = 0.78–1.04, P = 0.166) (Table 2). A separate analysis was run including only patients who received anticancer therapy (n = 829), yielding similar findings (Supplementary Table 3).
We next examined patients with known IDH1-wildtypestatus (N = 563) [13, 14]. Among these patients,, neither seizure timing (omnibus p-value = 0.204 for OS; 0.384 for PFS) nor initial seizure severity (omnibus p-value = 0.431 for OS; 0.320 for PFS) displayed significant associations with overall survival or progression-free survival (Table 2). When classifying patient seizure status as a binary variable (“any timing of seizures” vs. “no seizures”) seizure presence did not display significant associations with overall survival (HR = 0.83, 95% CI = 0.68, 1.02, P = 0.075) or progression-free survival (HR = 0.91, 95% CI = 0.75–1.10, P = 0.332) (Table 2). In all models, there was no evidence of multicollinearity (all VIFs < 3).
Epileptic presentation and severity association with glioma-related seizure control
Both seizure timing and frequency were independently associated with likelihood of achieving seizure control (Table 3). Compared to patients in the Early Seizure group, patients in the Late Seizure group were less likely to achieve partial (OR = 0.25, 95% CI = 0.12–0.53, P < 0.001) or complete (OR = 0.30, 95% CI = 0.18–0.50, P < 0.001) seizure control. Patients with one seizure in the 30 days before their HGG diagnosis had greater odds of achieving partial (OR = 2.88, 95% CI = 1.28–6.49, P = 0.011) and complete (OR = 3.04, 95% CI = 1.75–5.30, P < 0.001) seizure control compared to patients with no seizures at presentation. For patients with more than one seizure in the 30 days before their diagnosis, odds of achieving partial seizure control (OR = 4.44, 95% CI = 1.81–10.89, P = 0.001) and complete seizure control (OR = 2.65, 95% CI = 1.36–5.16, P = 0.004) were also higher than those without seizures at presentation.
Compared to patients who did not achieve seizure control, risk of progression was lower in patients with partial (HR = 0.45, 95% CI = 0.32–0.62, P = < 0.001) or complete (HR = 0.54, 95% CI = 0.43–0.69, P = < 0.001) seizure control. Risk of death was also lower in patients with partial (HR = 0.30, 95% CI = 0.21–0.43, P = < 0.001) or complete (HR = 0.43, 95% CI = 0.33–0.55, P = < 0.001) seizure control compared to those who did not achieve any seizure control.
The IDH1 wildtype subanalysis demonstrated a significant association of seizure timing with likelihood of seizure control: the Late Seizure group was less likely than the Early Seizure group to achieve partial (OR = 0.16, 95% CI = 0.06–0.45, P = < 0.001) or complete (OR = 0.23, 95% CI = 0.12–0.46, P = < 0.001) seizure control (Table 3). For patients with a pathogenic variant in IDH1, timing of first seizure and seizure frequency did not display significant associations with odds of attaining partial or complete seizure control (Table 4).
Discussion
We present a retrospective analysis of 950 patients with HGG and recorded seizure status, demonstrating an association with improved survival for both patients with seizure activity at baseline and patients who first developed seizure activity after their HGG diagnosis. Our approach allowed us to explore whether epilepsy itself associates with prolonged survival or whether the effect is confounded by a lead-time bias of earlier HGG diagnosis (extending survival only in patients who had epileptic activity prior to HGG diagnosis).
Consistent with prior studies, seizure presence at disease presentation was associated with improved overall survival, but not progression-free survival, within our full 950-patient cohort [8, 15]. A 2018 meta-analysis including 368 patients found an increase in progression-free survival among patients with epilepsy at initial glioma presentation; however, this sample included a mix of low-grade (LGG) and high-grade gliomas [7]. The incidence of seizure activity in LGG is higher than in HGG; our decision to focus exclusively on HGG may explain our different findings [6]. Additionally, PFS is influenced by inter-radiologist differences in scan interpretation as well as follow-up cadence; this subjectivity may contribute to differences in PFS conclusions between studies [16]. We believe that OS is a much more objective measure of disease-related longevity. Alternatively, it is possible that seizures associate with increased survival via cancer-independent mechanisms (e.g. more frequent follow-up with medical providers, potential unknown benefits of ASM use), thereby linking to OS but not affecting PFS.
A 2024 retrospective analysis by Pallud et al. of IDH1-wildtype GBM yielded similar findings regarding the prognostic impact of seizure presence at disease presentation; we add to this analysis by also reporting a previously undescribed significant increase in both overall and progression-free survival among patients whose first seizure occurred after histologically-confirmed diagnosis of HGG (our “Late Seizure” group) [15]. To our knowledge, our analysis is one of the first and largest cohorts examining the prognostic value of seizures presenting after HGG diagnosis. By finding a significant association between seizures and survival in patients who experienced their first seizure after HGG diagnosis (even after accounting for exposure to anticancer therapy), our data suggests that the positive prognostic impact of epilepsy goes beyond the explanation of lead time bias proposed in prior studies [17, 18].
Neuronal hyperexcitability has recently been implicated as a potential driver for gliomagenesis and tumor progression [19]. Peritumoral glutamatergic neurons can synapse directly on tumor cells; hyperexcitation of glioma cells is theorized to facilitate tumor invasion, and direct in vivo optogenetic excitation of glioma cells has been shown to promote tumor proliferation [19,20,21]. While this finding appears contradictory to an association between seizure presence and improved prognosis in HGG, at least one study has demonstrated a possible association between the anti-seizure medication (ASM) lamotrigine and delayed tumor progression in optic pathway glioma [22]. We hypothesize that the suppressive effects of ASM use on neuronal excitability may underpin the prognostic benefit of a positive seizure history in HGG.
Several ASMs have also shown a cytotoxic effect towards glioblastoma cells in vitro. One clinical study of 249 patients with tumor-related epilepsy demonstrated better survival in patients receiving ASM therapy compared to patients not taking ASMs, though it is challenging to discern survival related to seizure control versus antiseizure medication effect [23, 24]. Further, we report an increase in overall and progression-free survival in patients who achieved partial or complete seizure control compared to patients who were unable to achieve six seizure-free months. The 2024 Pallud et al. retrospective analysis reported less epileptic control at the time of tumor progression; our study elaborates further by demonstrating a significant association between seizure control and both improved PFS and OS [15]. Additional studies, including comparison of outcomes between HGG patients receiving different ASMs, are needed to validate the hypothesis that ASMs reduce HGG tumor progression and understand if ASM therapy could be better leveraged to improve HGG outcomes.
When analyzing only known IDH1-wildtype patients, the significant associations observed in our full 950 patient analyses were lost. However, the directionality and approximate magnitude of hazard ratios in the 563-patient IDH1-wildtype analyses mimicked those seen in the 950-patient analyses, a finding we propose may speak to a loss in statistical power with reduced sample size [25]. Further, a 2024 retrospective analysis looking exclusively at IDH-wildtype cases also demonstrated prolonged survival with seizure presence at diagnosis [15]. Alternatively, these findings may be influenced by changing treatment practices over time– IDH1 testing primarily occurred after 2015. When plotting anticancer treatments received over time, no obvious temporal shifts are seen, although more subtle variation in specific medications or dosing could be possible (Supplementary Fig. 3).
A limitation of this study is its retrospective nature, which allows for the introduction of recall bias. While we extracted data from a prospectively collected clinical database for the study of CNS tumors, all variables related to tumor-related epilepsy were collected retrospectively. For example, EEG collection is not part of the standard of care for HGG-associated epilepsy in most cases; we relied on clinical documentation of seizure activity. Our large sample size, however, does help to reduce this bias. Additionally, our study was conducted without access to tumor volume data; determining whether seizure activity correlates with tumor volume would be a prudent future research direction to clarify whether patients with seizures are diagnosed with smaller tumors.
Our investigation should serve as retrospective evidence that the positive prognostic value of epileptic activity in patients with HGG goes beyond the early-diagnosis theory. Future exploration of molecular alterations in HGG to assess their potential impact on seizure incidence and management, as well as disease course, is warranted. Despite the potential positive prognostic value of epileptic activity in HGG survival, seizures nonetheless can have a serious detrimental impact on quality of life, and our findings demonstrate a need for greater understanding of late-onset epileptic activity and better approaches to management. Seizure presence associates with improved overall survival, but seizure control is affected by many factors including the selection of ASMs, and additional study is needed to understand how the clinical approach to treating HGG-associated epilepsy affects HGG disease course and survival.
Data availability
No datasets were generated or analysed during the current study.
Figures
Study figures were generated using R.
References
Grech N, Dalli T, Mizzi S et al (2020) Rising incidence of Glioblastoma Multiforme in a well-defined Population. Cureus 12:e8195. https://doi.org/10.7759/cureus.8195
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO classification of tumors of the Central Nervous System: a summary. Neuro Oncol 23:1231–1251. https://doi.org/10.1093/neuonc/noab106
Armstrong TS, Grant R, Gilbert MR et al (2016) Epilepsy in glioma patients: mechanisms, management, and impact of anticonvulsant therapy. Neuro Oncol 18:779–789. https://doi.org/10.1093/neuonc/nov269
Kerkhof M, Vecht CJ (2013) Seizure characteristics and prognostic factors of gliomas. Epilepsia 54 Suppl 9:12–17. https://doi.org/10.1111/epi.12437
Iuchi T, Hasegawa Y, Kawasaki K, Sakaida T (2015) Epilepsy in patients with gliomas: incidence and control of seizures. J Clin Neurosci 22:87–91. https://doi.org/10.1016/j.jocn.2014.05.036
Samudra N, Zacharias T, Plitt A et al (2019) Seizures in glioma patients: an overview of incidence, etiology, and therapies. J Neurol Sci 404:80–85. https://doi.org/10.1016/j.jns.2019.07.026
Fan X, Li Y, Shan X et al (2018) Seizures at presentation are correlated with better survival outcomes in adult diffuse glioma: a systematic review and meta-analysis. Seizure 59:16–23. https://doi.org/10.1016/j.seizure.2018.04.018
Lu VM, Jue TR, Phan K, McDonald KL (2018) Quantifying the prognostic significance in glioblastoma of seizure history at initial presentation: a systematic review and meta-analysis. Clin Neurol Neurosurg 164:75–80. https://doi.org/10.1016/j.clineuro.2017.11.015
van den Bent MJ, Wefel JS, Schiff D et al (2011) Response assessment in neuro-oncology (a report of the RANO group): assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12:583–593. https://doi.org/10.1016/S1470-2045(11)70057-2
Driving Laws In: Epilepsy Foundation. https://www.epilepsy.com/lifestyle/driving-and-transportation/laws. Accessed 17 Dec 2023
Nevitt SJ, Sudell M, Cividini S et al (2022) Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. Cochrane Database Syst Rev 2022:CD011412. https://doi.org/10.1002/14651858.CD011412.pub4
Callaghan BC, Anand K, Hesdorffer D et al (2007) Likelihood of seizure remission in an adult population with refractory epilepsy. Ann Neurol 62:382–389. https://doi.org/10.1002/ana.21166
Yan H, Parsons DW, Jin G et al (2009) IDH1 and IDH2 mutations in Gliomas. N Engl J Med 360:765–773. https://doi.org/10.1056/NEJMoa0808710
Chen H, Judkins J, Thomas C et al (2017) Mutant IDH1 and seizures in patients with glioma. Neurology 88:1805–1813. https://doi.org/10.1212/WNL.0000000000003911
Pallud J, Roux A, Moiraghi A et al (2024) Characteristics and prognosis of Tumor-Related Epilepsy during Tumor Evolution in patients with IDH Wild-Type Glioblastoma. Neurology 102:e207902. https://doi.org/10.1212/WNL.0000000000207902
Korn RL, Crowley JJ (2013) Overview: progression-free survival as an endpoint in clinical trials with solid tumors. Clin Cancer Res 19:2607–2612. https://doi.org/10.1158/1078-0432.CCR-12-2934
Mastall M, Wolpert F, Gramatzki D et al (2021) Survival of brain tumour patients with epilepsy. Brain 144:3322–3327. https://doi.org/10.1093/brain/awab188
Lee JW, Norden AD, Ligon KL et al (2014) Tumor associated seizures in glioblastomas are influenced by survival gene expression in a region-specific manner: a gene expression imaging study. Epilepsy Res 108:843–852. https://doi.org/10.1016/j.eplepsyres.2014.02.021
Goethe EA, Deneen B, Noebels J, Rao G (2023) The role of hyperexcitability in Gliomagenesis. Int J Mol Sci 24:749. https://doi.org/10.3390/ijms24010749
Venkatesh HS, Morishita W, Geraghty AC et al (2019) Electrical and synaptic integration of glioma into neural circuits. Nature 573:539–545. https://doi.org/10.1038/s41586-019-1563-y
Venkataramani V, Tanev DI, Strahle C et al (2019) Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature 573:532–538. https://doi.org/10.1038/s41586-019-1564-x
Anastasaki C, Mo J, Chen J-K et al (2022) Neuronal hyperexcitability drives central and peripheral nervous system tumor progression in models of neurofibromatosis-1. Nat Commun 13:2785. https://doi.org/10.1038/s41467-022-30466-6
Yagi C, Tatsuoka J, Sano E et al (2022) Anti–tumor effects of anti–epileptic drugs in malignant glioma cells. Oncol Rep 48:1–12. https://doi.org/10.3892/or.2022.8431
Cacho-Diaz B, San-Juan D, Salmeron K et al (2018) Choice of antiepileptic drugs affects the outcome in cancer patients with seizures. Clin Transl Oncol 20:1571–1576. https://doi.org/10.1007/s12094-018-1892-6
Serdar CC, Cihan M, Yücel D, Serdar MA (2021) Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem Med (Zagreb) 31:010502. https://doi.org/10.11613/BM.2021.010502
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection was performed by Ryan G. Rilinger, Lydia Guo, and Josephine Volovetz. Data analysis and figure generation were performed by Nicolas R. Thompson. The first draft of the manuscript was written by Ryan G. Rilinger, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Preliminary results associated with the findings in this manuscript were presented as a poster abstract at the 2023 Society for Neuro-Oncology / American Society of Clinical Oncology Central Nervous System Conference in San Francisco, CA.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rilinger, R.G., Guo, L., Sharma, A. et al. Tumor-related epilepsy in high-grade glioma: a large series survival analysis. J Neurooncol (2024). https://doi.org/10.1007/s11060-024-04787-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11060-024-04787-z