Abstract
Background
Breast cancer (BC) is the second most common etiology of brain metastases (BrM). We aimed to examine the incidence of BrM among all BC patients presenting to a large tertiary cancer centre over one decade.
Methods
We included all BC patients presenting consecutively between 2009 and 2019 and cross referenced that cohort to a radiotherapy database, identifying patients treated for BrM at any time following their initial presentation. Cumulative incidences (CI) of BrM diagnoses were calculated using death as a competing risk and compared using the Fine-Gray method. Overall survival was estimated using the Kaplan Meier method.
Results
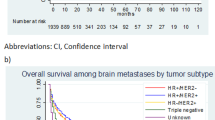
We identified 12,995 unique patients. The CI of BrM in patients who initially presented with Stage 0–4 disease was 2.1%, 3.7%, 9.4%, 10.6%, and 28.7%, respectively at 10 years. For 8,951 patients with available molecular subtype data, 6,470 (72%), 961 (11%), 1,023 (11%), and 497 (6%) had hormone-receptor (HR)-positive/ERBB2-, HR-negative/ERBB2-, HR-positive/ERBB2 + , and HR-negative/ERBB2 + disease, respectively; the CI of BrM in each was 7.6%, 25.3%, 24.1%, and 26.6%, at 10 years following BC diagnosis, respectively. Median overall survival (OS) following BC diagnosis and BrM diagnosis was 28 years 95% CI [25, 32] and 10 months 95% CI [9, 12], respectively.
Conclusions
From a large, registry-based study, we observed that patients with ERBB2 + and triple negative BC have the highest incidence of BrM. Our data supports prospective surveillance brain MRI studies. Given advancements in BrM treatment, clinicians should have a low threshold for brain imaging in BC patients with high risk subtypes.



Similar content being viewed by others
Data availability
Data available on request due to privacy/ethical considerations.
References
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto W, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, Yu J, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Beyond an updated graded prognostic assessment (breast GPA): a prognostic index and trends in treatment and survival in breast cancer brain metastases from 1985 to today. Int J Radiat Oncol Biol Phys 107(2):334–343. https://doi.org/10.1016/j.ijrobp.2020.01.051. Erratum in: Int J Radiat Oncol Biol Phys. 2021;109(1):303
Martin AM, Cagney DN, Catalano PJ, Warren LE, Bellon JR, Punglia RS, Claus EB, Lee EQ, Wen PY, Haas-Kogan DA, Alexander BM, Lin NU, Aizer AA (2017) Brain metastases in newly diagnosed breast cancer: a population-based study. JAMA Oncol 3(8):1069–1077. https://doi.org/10.1001/jamaoncol.2017.0001
Gabos Z, Sinha R, Hanson J, Chauhan N, Hugh J, Mackey JR, Abdulkarim B (2006) Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol 24(36):5658–5663. https://doi.org/10.1200/JCO.2006.07.0250
Wang XY, Rosen MN, Chehade R, Sahgal A, Das S, Warner E, Saskin R, Zhang B, Soliman H, Chan KKW, Jerzak KJ (2022) Analysis of rates of brain metastases and association with breast cancer subtypes in Ontario, Canada. JAMA Netw Open 5(8):e2225424. https://doi.org/10.1001/jamanetworkopen.2022.25424
Kuksis M, Gao Y, Tran W, Hoey C, Kiss A, Komorowski AS, Dhaliwal AJ, Sahgal A, Das S, Chan KK, Jerzak KJ (2021) The incidence of brain metastases among patients with metastatic breast cancer: a systematic review and meta-analysis. Neuro Oncol 23(6):894–904. https://doi.org/10.1093/neuonc/noaa285
Pasquier D, Darlix A, Louvel G, Fraisse J, Jacot W, Brain E, Petit A, Mouret-Reynier MA, Goncalves A, Dalenc F, Deluche E, Fresnel JS, Augereau P, Ferrero JM, Geffrelot J, Fumet JD, Lecouillard I, Cottu P, Petit T, Uwer L, Jouannaud C, Leheurteur M, Dieras V, Robain M, Mouttet-Audouard R, Bachelot T, Courtinard C (2020) Treatment and outcomes in patients with central nervous system metastases from breast cancer in the real-life ESME MBC cohort. Eur J Cancer 125:22–30. https://doi.org/10.1016/j.ejca.2019.11.001
Mitri Z, Constantine T, O’Regan R (2012) The HER2 receptor in breast cancer: pathophysiology, clinical use, and new advances in therapy. Chemother Res Pract 2012:743193. https://doi.org/10.1155/2012/743193
Perera M, Ribot EJ, Percy DB et al (2012) In vivo magnetic resonance imaging for investigating the development and distribution of experimental brain metastases due to breast cancer. Transl Oncol 5(3):217–225
Palmieri D, Bronder JL, Herring JM et al (2007) Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res 67(9):4190–4198
Momeny M, Saunus JM, Marturana F, McCart Reed AE, Black D, Sala G, Iacobelli S, Holland JD, Yu D, Da Silva L, Simpson PT, Khanna KK, Chenevix-Trench G, Lakhani SR (2015) Heregulin-HER3-HER2 signaling promotes matrix metalloproteinase-dependent blood-brain-barrier transendothelial migration of human breast cancer cell lines. Oncotarget 6(6):3932–46. https://doi.org/10.18632/oncotarget.2846
Choy C, Ansari KI, Neman J, Hsu S, Duenas MJ, Li H, Vaidehi N, Jandial R (2017) Cooperation of neurotrophin receptor TrkB and Her2 in breast cancer cells facilitates brain metastases. Breast Cancer Res 19(1):51. https://doi.org/10.1186/s13058-017-0844-3
Pestalozzi BC, Brignoli S (2000) Herceptin(R) (trastuzumab) in cerebrospinal fluid (CSF). Eur J Cancer 36(suppl 5):S54-S
Stemmler J, Schmitt M, Willems A, Bernhard H, Harbeck N, Heinemann V (2006) Brain metastases in HER2-overexpressing metastatic breast cancer: comparative analysis of trastuzumab levels in serum and cerebrospinal fluid. J Clin Oncol 24(18):64S-S
Baculi RH, Suki S, Nisbett J et al (2001) Meningeal carcinomatosis from breast carcinoma responsive to trastuzumab. J Clin Oncol 19:3297–3298
Filho OM, Leone J, Li T, Tan-Wasielewski Z, Trippa L, Barry W, Younger J, Lawler E, Walker L, Freedman R et al (2020) Phase I dose-escalation trial of tucatinib in combination with trastuzumab in patients with HER2-positive breast cancer brain metastases. Ann Oncol 31:1231–1239. https://doi.org/10.1016/j.annonc.2020.05.014
Borges VF, Ferrario C, Aucoin N, Falkson C, Khan Q, Krop I, Welch S, Conlin A, Chaves J, Bedard PL et al (2018) Tucatinib combined with ado-trastuzumab emtansine in advanced ERBB2/HER2-positive metastatic breast cancer. JAMA Oncol 4:1214–1220. https://doi.org/10.1001/jamaoncol.2018.1812
Garcia-Alvarez A, Papakonstantinou A, Oliveira M (2021) Brain metastases in HER2-positive breast cancer: current and novel treatment strategies. Cancers (Basel) 13(12):2927. https://doi.org/10.3390/cancers13122927
Bartsch R, Berghoff AS, Furtner J, Marhold M, Bergen ES, Roider-Schur S, Starzer AM, Forstner H, Rottenmanner B, Dieckmann K, Bago-Horvath Z, Haslacher H, Widhalm G, Ilhan-Mutlu A, Minichsdorfer C, Fuereder T, Szekeres T, Oehler L, Gruenberger B, Singer CF, Weltermann A, Puhr R, Preusser M (2022) Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: a single-arm, phase 2 trial. Nat Med 28(9):1840–1847. https://doi.org/10.1038/s41591-022-01935-8
Pérez-García JM, Vaz Batista M, Cortez P, Ruiz-Borrego M, Cejalvo JM, de la Haba-Rodriguez J, Garrigós L, Racca F, Servitja S, Blanch S, Gion M, Nave M, Fernández-Abad M, Martinez-Bueno A, Llombart-Cussac A, Sampayo-Cordero M, Malfettone A, Cortés J, Braga S (2023) Trastuzumab deruxtecan in patients with central nervous system involvement from HER2-positive breast cancer: The DEBBRAH trial. Neuro Oncol 25(1):157–166. https://doi.org/10.1093/neuonc/noac144
Cortes J, Rugo HS, Cescon DW, Im SA, Yusof MM, Gallardo C, Lipatov O, Barrios CH, Perez-Garcia J, Iwata H, Masuda N, Torregroza Otero M, Gokmen E, Loi S, Guo Z, Zhou X, Karantza V, Pan W, Schmid P; KEYNOTE-355 Investigators (2022) Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N Engl J Med 387(3):217–226. https://doi.org/10.1056/NEJMoa2202809
Chehade R, Qazi MA, Ennis M, Sahgal A, Das S, Nofech-Mozes S, Jerzak KJ (2022) PD-L1 expression in breast cancer brain metastases. Neurooncol Adv 4(1):vdac154. https://doi.org/10.1093/noajnl/vdac154
Rostami R, Mittal S, Rostami P, Tavassoli F, Jabbari B (2016) Brain metastasis in breast cancer: a comprehensive literature review. J Neurooncol 127(3):407–414. https://doi.org/10.1007/s11060-016-2075-3
Yan M, Lü HM, Liu ZZ, Liu H, Zhang MW, Sun XB, Cui SD (2013) High risk factors of brain metastases in 295 patients with advanced breast cancer. Chin Med J (Engl) 126(7):1269–1275
Katarzyna J Jerzak, Arjun Sahgal, Gregory Pond, Priscilla K Brastianos, Orit Freedman, Gregory Stanisz, Ellen Warner (2022) Abstract OT1-07-01: MRI screening versus symptom-directed surveillance for brain metastases among patients with triple negative or HER2+ metastatic breast cancer: A pilot study (nct03881605). Cancer Res 82 (4_Supplement): OT1–07–01. https://doi.org/10.1158/1538-7445.SABCS21-OT1-07-01
National Comprehensive Cancer Network NCCN Guidelines—Breast Cancer, Version 4.2023. BINV-18. www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed Oct 2023
Ramakrishna N, Anders CK, Lin NU, Morikawa A, Temin S, Chandarlapaty S, Crews JR, Davidson NE, Maria AB, Franzoi JJ, Kirshner IE, Krop DA, Patt JP, Giordano SH (2022) Management of advanced human epidermal growth factor receptor 2–positive breast cancer and brain metastases: ASCO guideline update. J Clin Oncol 40(23):2636–2655
Gennari A, André F, Barrios CH et al (2021) ESMO clinical practice guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann Oncol 32:1475–1495
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
C.P. Conceptualization-Equal, Data curation-Equal, Methodology-Equal, Project administration-Equal, Software-Equal, Supervision-Equal, Writing – original draft-Equal, Writing – review & editing-Equal B.A. Data curation-Equal, Software-Equal A.S. Formal analysis-Equal, Methodology-Equal, Validation-Equal, Validation-Equal M.Y. Conceptualization-Equal, Writing – review & editing-Equal T.C. Conceptualization-Equal, Writing – review & editing-Equal K.J. Writing – review & editing-Equal D.S. Conceptualization-Equal, Data curation-Equal, Investigation-Equal, Methodology-Equal, Project administration-Equal, Resources-Equal, Supervision-Equal, Writing – original draft-Equal, Writing – review & editing-Equal.
Corresponding author
Ethics declarations
Ethics
All study procedures are performed in accordance with protocols approved by the research ethics board at the University Health Network. A exemption was granted by the ethics committee regarding written informed consent due to the anonymized retrospective nature of the data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Précis: From a large, registry-based study, we observed that patients with ERBB2 + and triple negative BC have the highest incidence of BrM. Clinicians should have a low threshold to image the brain of patients with a history of BC who experience symptoms suggestive of BrM, especially in ERBB2 + and triple negative BC.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Poletes, C., Amanirad, B., Santiago, A.T. et al. The incidence of brain metastases in breast cancer according to molecular subtype and stage: a 10-year single institution analysis. J Neurooncol (2024). https://doi.org/10.1007/s11060-024-04707-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11060-024-04707-1