Abstract
Introduction
Meningiomas with bone involvement account for 4.5–17% of all intracranial meningiomas. Little is known about whether these meningiomas (WHO grade I) behave differently than meningiomas without bone involvement. We sought to study the relatively uncommon imaging manifestations of meningioma and to evaluate their clinical significance.
Methods
A single-institution retrospective cohort study of surgically treated superficial meningioma patients between 2011 and 2022 was conducted. Age, sex, preoperative imaging, operative data, and surgical outcomes were reviewed. Imaging variables and outcomes were reported for patients with bone-invading meningiomas and compared with those with nonbone-invading meningiomas. Univariate analyses were also conducted.
Results
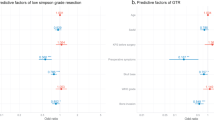
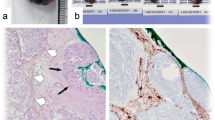
Of 577 total superficial meningiomas treated surgically, 47 (8.1%) exhibited bone invasion. Most bone-invading meningiomas were parasagittal (n = 29, 61.7%). A total of 12.7% (n = 6) of patients with bone-invading meningioma had recurrence, whereas 9.1% (n = 48) of patients with non-bone-invading meningioma had recurrence (p = 0.426). No significant difference in the median time to recurrence was observed between patients with bone-invading meningiomas and patients with nonbone-invading meningiomas (69.8 months, Q1:53.1; Q3:81.4 months vs. 69.7 months, Q1:47.5; Q3:96.7; p = 0.638).
Conclusions
Superficial meningioma with bone involvement had similar outcomes compared to those of superficial meningioma without bone involvement. Hyperostosis in meningioma (WHO grade I) may not be a surrogate for aggressive meningioma behavior.



Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Ottenhausen M, Rumalla K, Younus I, Minkowitz S, Tsiouris AJ, Schwartz TH (2018) Predictors of postoperative motor function in rolandic meningiomas. J Neurosurg 130:1283–1288. https://doi.org/10.3171/2017.12.JNS172423
Marbacher S, Coluccia D, Fathi AR, Andereggen L, Beck J, Fandino J (2013) Intraoperative patient-specific reconstruction of partial bone flap defects after convexity meningioma resection. World Neurosurg 79:124–130. https://doi.org/10.1016/j.wneu.2011.05.057
Jin L, Youngblood MW, Gupte TP et al (2021) Type of bony involvement predicts genomic subgroup in sphenoid wing meningiomas. J Neurooncol 154:237–246. https://doi.org/10.1007/s11060-021-03819-2
Kalasauskas D, Tanyildizi Y, Renovanz M, Brockmann MA, Sommer CJ, Ringel F, Keric N (2021) Evaluation of resection margin after image-guided dural tail resection in Convexity meningiomas. J Clin Med 10:1177. https://doi.org/10.3390/jcm10061177
Fathalla H, Tawab MGA, El-Fiki A (2020) Extent of gyperostotic bone resection in convexity meningioma to achieve pathologically free margins. J Korean Neurosurg Soc 63:821–826. https://doi.org/10.3340/jkns.2020.0020
Goyal N, Kakkar A, Sarkar C, Agrawal D (2012) Does bony hyperostosis in intracranial meningioma signify tumor invasion? A radio-pathologic study. Neurol India 60:50–54. https://doi.org/10.4103/0028-3886.93589
Pieper DR, Al-Mefty O, Hanada Y, Buechner D (1999) Hyperostosis associated with meningioma of the cranial base: secondary changes or tumor invasion. Neurosurgery 44:742–747. https://doi.org/10.1097/00006123-199904000-00028
Gabeau-Lacet D, Aghi M, Betensky RA, Barker FG, Loeffler JS, Louis DN (2009) Bone involvement predicts poor outcome in atypical meningioma. J Neurosurg 111:464–471. https://doi.org/10.3171/2009.2.JNS08877
Di Cristofori A, Del Bene M, Locatelli M, Boggio F, Ercoli G, Ferrero S, Del Gobbo A (2018) Meningioma and bone hyperostosis: expression of bone stimulating factors and review of the literature. World Neurosurg 115:e774–e781. https://doi.org/10.1016/j.wneu.2018.04.176
Kim KS, Rogers LF, Goldblatt D (1987) CT features of hyperostosing meningioma en plaque. AJR Am J Roentgenol 149:1017–1023. https://doi.org/10.2214/ajr.149.5.1017
Salehi F, Jalali S, Alkins R, Lee JI, Lwu S, Burrell K, Gentili F, Croul S, Zadeh G (2013) Proteins involved in regulating bone invasion in skull base meningiomas. Acta Neurochir (Wien) 155:421–427. https://doi.org/10.1007/s00701-012-1577-9
Sauvigny T, Giese H, Höhne J et al (2021) A multicenter cohort study of early complications after cranioplasty: results of the German Cranial Reconstruction Registry. J Neurosurg 137:591–598. https://doi.org/10.3171/2021.9.JNS211549
Eaton JC, Greil ME, Nistal D, Caldwell DJ, Robinson E, Aljuboori Z, Temkin N, Bonow RH, Chesnut RM (2022) Complications associated with early cranioplasty for patients with traumatic brain injury: a 25-year single-center analysis. J Neurosurg 137:776–781. https://doi.org/10.3171/2021.11.JNS211557
Traylor JI, Plitt AR, Hicks WH, Mian TM, Mickey BE, Barnett SL (2023) Evaluating risk of recurrence in patients with meningioma. J Neurosurg 138:621–628. https://doi.org/10.3171/2022.6.JNS221162
Tang AR, Chotai S, Guidry BS, Sun L, Ye F, Kelly PD, McDermott JR, Grisham CJ, Morone PJ, Thompson RC, Chambless LB (2023) Conditional recurrence-free Survival after Surgical Resection of Meningioma. Neurosurgery 93:339–347. https://doi.org/10.1227/neu.0000000000002416
Acknowledgements
We thank Journal Experts for assisting in the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
GL: Conceptualization, Methodology. QT: Writing—original draft. SW: Visualization, Investigation. KL: Visualization, Investigation. YZ: Supervision. QC: Writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, G., Tian, Q., Wang, S. et al. Superficial meningioma with bone involvement: surgical strategies and clinical outcomes. J Neurooncol 168, 27–33 (2024). https://doi.org/10.1007/s11060-024-04604-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-024-04604-7