Abstract
Purpose
As sphenoid wing meningiomas (SWMs) are associated with varying degrees of bony involvement, we sought to understand potential relationships between genomic subgroup and this feature.
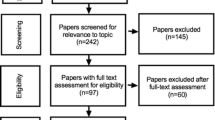
Methods
Patients treated at Yale-New Haven Hospital for SWM were reviewed. Genomic subgroup was determined via whole exome sequencing, while the extent of bony involvement was radiographically classified as no bone invasion (Type I), hyperostosis only (Type II), tumor invasion only (Type III), or both hyperostosis and tumor invasion (Type IV). Among additional clinical variables collected, a subset of tumors was identified as spheno-orbital meningiomas (SOMs). Machine-learning approaches were used to predict genomic subgroups based on pre-operative clinical features.
Results
Among 64 SWMs, 53% had Type-II, 9% had Type-III, and 14% had Type-IV bone involvement; nine SOMs were identified. Tumors with invasion (i.e., Type III or IV) were more likely to be WHO grade II (p: 0.028). Additionally, tumors with invasion were nearly 30 times more likely to harbor NF2 mutations (OR 27.6; p: 0.004), while hyperostosis only were over 4 times more likely to have a TRAF7 mutation (OR 4.5; p: 0.023). SOMs were a significant predictor of underlying TRAF7 mutation (OR 10.21; p: 0.004).
Conclusions
SWMs with invasion into bone tend to be higher grade and are more likely to be NF2 mutated, while SOMs and those with hyperostosis are associated with TRAF7 variants. Pre-operative prediction of molecular subtypes based on radiographic bony characteristics may have significant biological and clinical implications based on known recurrence patterns associated with genomic drivers and grade.



Similar content being viewed by others
Data availability
The data generated and analyzed in this study are provided in the text and the figures, tables, and supplementary tables. Any additional data needed may be requested from the corresponding author.
Code availability
Code is available upon request.
References
Güdük M, Özduman K, Pamir MN (2019) Sphenoid wing meningiomas: surgical outcomes in a series of 141 cases and proposal of a scoring system predicting extent of resection. World Neurosurg 125:e48–e59
Simon M, Schramm J (2010) Sphenoid wing meningiomas. In: Meningiomas: A Comprehensive Text. Pamir N, Black P, Fahlbusch R. Elsevier, pp 427–443
Terrier L-M et al (2018) Spheno-orbital meningiomas surgery: multicenter management study for complex extensive tumors. World Neurosurg 112:e145–e156
Bikmaz K, Mrak R, Al-Mefty O (2007) Management of bone-invasive, hyperostotic sphenoid wing meningiomas. J Neurosurg 107(5):905–912
Collins JM, Christoforidis GA (2016) Chap. 44—Meningeal tumors. Handbook of neuro-oncology neuroimaging, 2nd edn. Newton HB. Elsevier, pp 519–542
Lau BL et al (2019) Does putting back hyperostotic bone flap in meningioma surgery cause tumor recurrence? An observational prospective study. World Neurosurg 127:e497–e502
Clark VE et al (2013) Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339(6123):1077–1080
Clark VE et al (2016) Recurrent somatic mutations in POLR2A define a distinct subset of meningiomas. Nat Genet 48(10):1253–1259
Brastianos PK et al (2013) Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat Genet 45(3):285–289
Youngblood MW et al (2019) Correlations between genomic subgroup and clinical features in a cohort of more than 3000 meningiomas. J Neurosurg 133(5):1345–1354
Youngblood MW et al (2020) Associations of meningioma molecular subgroup and tumor recurrence. Neuro-Oncology 23(5):783–794
Karsy M et al (2018) Clinical potential of meningioma genomic insights: a practical review for neurosurgeons. Neurosurg Focus FOC 44(6):E10
Gonen L et al (2018) Sphenoorbital meningioma: surgical series and design of an intraoperative management algorithm. Neurosurg Rev 41(1):291–301
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20(1):22
Hao S et al (2019) Non-NF2 mutations have a key effect on inhibitory immune checkpoints and tumor pathogenesis in skull base meningiomas. J Neuro-oncol 144(1):11–20
Bi WL et al (2017) Radiographic prediction of meningioma grade and genomic profile. J Neurol Surg Part B Skull Base 78:01
Birzu C, Peyre M, Sahm F (2020) Molecular alterations in meningioma: prognostic and therapeutic perspectives. Curr Opin Oncol 32(6):613–622
Yuzawa S, Nishihara H, Tanaka S (2016) Genetic landscape of meningioma. Brain Tumor Pathol 33(4):237–247
Harmancı AS et al (2017) Integrated genomic analyses of de novo pathways underlying atypical meningiomas. Nat Commun 8(1):1–14
Goutagny S et al (2014) High incidence of activating TERT promoter mutations in meningiomas undergoing malignant progression. Brain Pathol 24(2):184–189
Mariniello G et al (2013) Management of the optic canal invasion and visual outcome in spheno-orbital meningiomas. Clin Neurol Neurosurg 115(9):1615–1620
Ringel F, Cedzich C, Schramm J (2007) Microsurgical technique and results of a series of 63 spheno-orbital meningiomas. Oper Neurosurg 60(suppl_4):ONS-214–ONS-222
Kissil JL et al (2003) Merlin, the product of the Nf2 tumor suppressor gene, is an inhibitor of the p21-activated kinase, Pak1. Mol Cell 12(4):841–849
Striedinger K et al (2008) The neurofibromatosis 2 tumor suppressor gene product, merlin, regulates human meningioma cell growth by signaling through YAP. Neoplasia 10(11):1204–1212
Morice S et al (2020) Hippo/YAP signaling pathway: a promising therapeutic target in bone paediatric cancers? Cancers (Basel) 12(3):645
Zotti T, Vito P, Stilo R (2012) The seventh ring: exploring TRAF7 functions. J Cell Physiol 227(3):1280–1284
Whyte MP (2006) Paget’s disease of bone and genetic disorders of RANKL/OPG/RANK/NF-kappaB signaling. Ann NY Acad Sci 1068:143–164
Han J et al (2007) Concerted action of Msx1 and Msx2 in regulating cranial neural crest cell differentiation during frontal bone development. Mech Dev 124(9–10):729–745
Alappat S, Zhang ZY, Chen YP (2003) Msx homeobox gene family and craniofacial development. Cell Res 13(6):429–442
Tokita MJ et al (2018) De novo missense variants in TRAF7 cause developmental delay, congenital anomalies, and dysmorphic features. Am J Hum Genet 103(1):154–162
Castilla-Vallmanya L et al (2020) Phenotypic spectrum and transcriptomic profile associated with germline variants in TRAF7. Genet Sci 22(7):1215–1226
Pieper DR et al (1999) Hyperostosis associated with meningioma of the cranial base: secondary changes or tumor invasion. Neurosurgery 44(4):742–746
Acknowledgements
We are grateful to the patients who contributed to this study. This study was supported by the Gregory M. Kiez and Mehmet Kutman Foundation and the Connecticut Brain Tumor Alliance.
Funding
This study was funded by Connecticut Brain Tumor Alliance.
Author information
Authors and Affiliations
Contributions
Study Design: LJ, MWY, RKF, and JM. Data Collection: TG, SV, AN, TB, ZE-O, KY, KM-G, SMA, and SBO. Data Analysis: LJ and MWY. Manuscript Drafting: LJ, MWY, SV, AN, and JM. Genomics Expertise: ZE-O, MG, and JM. Supervision of Clinical Correlations: JM. Radiology Imaging Expertise: MA and RKF. Histology Expertise: DM. Clinical providers: SBO, NB, RPL, BLJ, MA.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Ethical approval
IRB approval from Yale University for this study’s methods was obtained.
Consent to participate
Written informed consent was obtained from the parents.
Consent to publication
The tables and figures contain non-identifiable patient data. Written informed consent was obtained from the parents.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jin, L., Youngblood, M.W., Gupte, T.P. et al. Type of bony involvement predicts genomic subgroup in sphenoid wing meningiomas. J Neurooncol 154, 237–246 (2021). https://doi.org/10.1007/s11060-021-03819-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03819-2