Abstract
Introduction
Glioblastoma (GBM) is the most common central nervous system malignancy in adults. Despite decades of developments in surgical management, radiation treatment, chemotherapy, and tumor treating field therapy, GBM remains an ultimately fatal disease. There is currently no definitive standard of care for patients with recurrent glioblastoma (rGBM) following failure of initial management.
Objective
In this retrospective cohort study, we set out to examine the relative effects of bevacizumab and Gamma Knife radiosurgery on progression-free survival (PFS) and overall survival (OS) in patients with GBM at first-recurrence.
Methods
We conducted a retrospective review of all patients with rGBM who underwent treatment with bevacizumab and/or Gamma Knife radiosurgery at Roswell Park Comprehensive Cancer Center between 2012 and 2022. Mean PFS and OS were determined for each of our three treatment groups: Bevacizumab Only, Bevacizumab Plus Gamma Knife, and Gamma Knife Only.
Results
Patients in the combined treatment group demonstrated longer post-recurrence median PFS (7.7 months) and median OS (11.5 months) compared to glioblastoma patients previously reported in the literature, and showed improvements in total PFS (p=0.015), total OS (p=0.0050), post-recurrence PFS (p=0.018), and post-recurrence OS (p=0.0082) compared to patients who received either bevacizumab or Gamma Knife as monotherapy.
Conclusion
This study demonstrates that the combined use of bevacizumab with concurrent stereotactic radiosurgery can have improve survival in patients with rGBM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common malignant brain cancer in adults and accounts for 25–30% of all primary central nervous system (CNS) tumors [1]. Despite developments in various treatment modalities over the past three decades, the prognosis for extended survival remains poor, with various studies showing median progression-free survival (PFS) and overall survival (OS) ranging from 6.2–7.5 months and 14.6–16.7 months, respectively, from time of initial diagnosis [2]. Standard-of-care treatment of GBM commonly consists of maximal safe surgical resection and radiotherapy followed by chemotherapy with temozolomide [3]. Other forms of treatment including tumor treating fields, carmustine wafers, and bevacizumab are also commonly used as adjuvants to primary therapy [4, 5]. However, tumor recurrence usually develops within 6 months following initial treatment [6, 7], most often within 2 cm of the surgical cavity [1, 8].
There are currently no established standard therapies for recurrent GBM consistently showing improvements in OS. Joint recommendations from the American Association of Neurological Surgeons and Congress of Neurological Surgeons support re-resection (Level II) [9], re-irradiation (Level III) [10], and revised temozolomide dosing (Level III) [11]. The use of nitrosoureas, platinum agents, topoisomerase inhibitors, tumor treating field therapy, and viral therapy are either not recommended or have insufficient evidence for recommendation (Level III) [11]. Bevacizumab has been shown to improve PFS in this setting, but there is currently insufficient evidence to show advantages in PFS or OS when it is used in combination with cytotoxic chemotherapeutic agents (Level III) [12]. Despite aggressive treatment, patients with rGBM have an estimated median PFS of 9 weeks and median OS of 25 weeks following tumor recurrence [13].
We performed a single-institution, retrospective analysis of all patients treated for rGBM over a 10-year period between 2012 and 2022. Treatment of these first-recurrence GBM patients (who failed initial Stupp protocol management) included administration of bevacizumab and/or treatment with Gamma Knife radiosurgery.
Methods
Following Institutional Review Board (IRB) approval, we conducted a retrospective review of all patients diagnosed with recurrent GBM who were treated with bevacizumab and/or Gamma Knife radiosurgery at the Roswell Park Comprehensive Cancer Center between September 1, 2012, and April 30, 2022. All diagnoses of GBM were made upon histopathological analysis of tissue samples obtained during biopsy or surgical resection, consistent with World Health Organization diagnostic criteria at the time of tissue resection [14, 15]. Patients were retrospectively assigned to one of three treatment groups depending upon whether they had received bevacizumab monotherapy (“BEV Only”), Gamma Knife monotherapy (“GK Only”), or a combination of the two (“BEV + GK”). Patients were excluded from further data collection and analysis if they had incomplete records or no available post-treatment magnetic resonance imaging (MRI), were participating in a clinical trial, did not complete Stupp protocol treatment, or had evidence of leptomeningeal disease at the time of diagnosis or recurrence. Patients who were reported to be alive at the time of data collection were also excluded due to the inability to definitively calculate PFS and OS for these patients.
Gamma Knife stereotactic radiosurgery (SRS) was performed using the Leksell Gamma Knife Perfexion and Icon (Elekta Inc) systems. Treatment planning was carried out using pretreatment MRIs imported into Leksell Gamma Plan (Version 11.0.2) and dosing (ranging from 0–30 Gy in 1–5 fractions) was calculated for each patient specifically based on tumor size and location. No margins were added to the gross tumor volume in order to determine the clinical or planned tumor volumes. Tumor volumes were calculated from manual segmentation of pre-treatment and post-treatment MRIs using Brainlab (Version 1.6.2.54) and Eclipse External Beam Planning (Varian, Version 15.6) software programs.
Data analysis was carried out using Microsoft Excel (Microsoft Office, Version 16.0.5278.1000) and IBM SPSS Statistics (Version 29.0.0.0). Patient demographic and clinical variables were compared across treatment groups using one-way analysis of variance (ANOVA), Mann–Whitney, Kruskal–Wallis, and chi-square testing. Univariate and multivariate Cox proportional hazards regression models were used to evaluate the association between survival outcomes and treatment groups while accounting for potential confounders: age, gender, single vs. multifocal lesions, recurrence tumor volume, IDH and MGMT statuses, post-surgical KPS, number of bevacizumab cycles, steroid use, number of surgical resections, and number of other chemotherapeutic agents administered to the patients during their treatment course.
Results
Patient Demographics
Two-hundred and forty-eight patients received treatment for rGBM at the Roswell Park Comprehensive Cancer Center between September 1, 2012, and April 30, 2022. Of those patients, 153 were excluded for the following reasons: 90 patients had incomplete treatment records, 24 patients were alive at the time of data collection, 17 patients were participants in a clinical trial, 15 patients had refused or been unable to complete standard of care management, five patients had diffuse leptomeningeal disease at the time of diagnosis, one patient had received more than three craniotomies in the past for treatment of astrocytoma, and one patient had been receiving chronic bevacizumab for low-grade glioma prior to starting treatment for GBM.
Patient demographics and tumor characteristics are presented in Table 1. Of the 95 rGBM patients included in our study, 19 patients were treated with bevacizumab only (BEV Only), 57 patients were treated with both bevacizumab and Gamma Knife (BEV + GK), and 19 patients received Gamma Knife SRS only (GK Only). The mean age at diagnosis was 56.8 ± 11.3 years, with no significant differences in patient ages among treatment groups (p = 0.23). The median number of surgical resections was higher in the BEV + GK group compared to BEV Only and GK Only patients (2 vs. 1 vs. 1, p = 0.012, respectively). The number of bevacizumab cycles received by patients in the BEV Only and BEV + GK groups did not significantly differ (BEV Only vs. BEV + GK: 5 vs. 5, p = 0.27), and the use of steroids (p = 0.34) and number of other chemotherapeutic agents received during treatment for rGBM (p = 0.28) were also similar across all treatment groups. The median decline in KPS from post-surgical functioning to the last recorded KPS found in each patient’s note was 20 for all patients, with no significantly increased or decreased declines noted for any particular treatment group (p = 0.79).
The majority of GBMs were right-hemispheric (n = 53, 55.8%). Three patients had multifocal lesions involving both left and right hemispheres. Single focus lesions were present in 56.8% (n = 54) of study patients, while 43.2% (n = 41) of patients had multifocal lesions. The majority of lesions occurred in the temporal lobe (n = 41, 43.2%), followed by the frontal lobe (n = 33, 34.7%), parietal lobe (n = 22, 23.2%), and occipital lobe (n = 4, 4.2%). Five tumors involved the lateral ventricle, corpus callosum, insular cortex, thalamus, and pons. There were no significant differences in the distribution of GBM locations among the three treatment groups.
The mean initial tumor and post-surgical volumes were 28.8 ± 24.3 cm3 and 3.2 ± 3.3 cm3. Patients in the BEV + GK treatment group had the lowest mean post-surgical, recurrence, and first post-treatment tumor volumes (p = 0.021, 0.030, and 0.024, respectively), but no significant differences in second, third, or last recorded tumor volumes were noted. In total, 213 target lesions were treated with Gamma Knife radiosurgery. No patients received a third GK treatment, and statistical testing for differences in “Third Post-Treatment Tumor Volumes” was therefore only performed between the BEV Only and BEV + GK groups.
Only 71 of 95 (74.7%) included patients had both IDH and MGMT statuses available. Forty-nine patients (69.0%) were IDH-wild type, MGMT-unmethylated; 16 patients (22.5%) were IDH-wild type, MGMT-methylated; four patients (5.6%) were IDH-mutated, MGMT-unmethylated; and two patients (2.8%) were IDH-mutated, MGMT-methylated. No significant differences in the distribution of these patients throughout the three treatment groups were found.
Univariate and Multivariate Survival Outcomes
The median PFS and OS for our study population were 14.1 months and 17.1 months, respectively. Patients in the BEV + GK group had the highest median PFS (BEV Only vs. BEV + GK vs. GK Only: 11.8 vs. 15.6 vs. 12.0 months, p = 0.015) and OS (BEV Only vs. BEV + GK vs. GK Only: 14.3 vs. 18.6 vs. 15.0 months, p = 0.0050) among treatment groups. Patients in the combination treatment group also showed significantly improved post-tumor recurrence PFS and OS compared to patients in the individual treatment groups (Post-Recurrence PFS, BEV Only vs. BEV + GK vs. GK Only: 5.0 vs. 7.7 vs. 4.9 months, p = 0.018; Post-Recurrence OS, BEV Only vs. BEV + GK vs. GK Only: 6.5 vs. 11.5 vs. 7.9 months, p = 0.0082).
Patients were also stratified by IDH and MGMT statuses vs. treatment group, with the highest PFS and OS found for the “IDH-WT, MGMT-Methylated” genotype (PFS: 17.0 months, OS: 21.2 months) among all patients included in this study. Patients with “IDH-WT, MGMT-Unmethylated” did not show differences in PFS or OS when stratified by treatment group, and statistical analysis of patients with other IDH/MGMT combination genotypes were not able to be performed due to small subgroup sizes. These results are presented in Table 2.
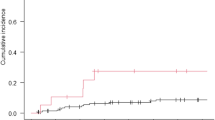
Kaplan–Meier plots (Fig. 1) were constructed to compare cumulative survival functions for post-recurrence PFS and OS between the three treatment groups. Only the comparison between BEV Only and BEV + GK groups showed significant differences in post-recurrence PFS (p = 0.002) and OS (p = 0.001).
Post-Recurrence Survival Plots. Kaplan–Meier survival plots as a function of post-recurrence PFS or OS compared between treatment groups. The x-axis represents post-recurrence PFS or OS durations in months. The y-axis represents the cumulative survival probability. BEV bevacizumab; GK Gamma Knife; OS overall survival; PFS progression-free survival; Tx treatment
Univariate regression analysis was performed for PFS, OS, post-recurrence PFS, and post-recurrence OS with respect to a number of our study demographic and clinical variables, including age, gender, GBM location, single vs. multifocal lesion, IDH and MGMT statuses, tumor volumes at various timepoints, administered medications, number of surgical resections, and KPS (Table 3). None of the tested variables were associated with consistent increases or decreases in risk of disease progression or patient death. However, patient age was associated with significantly increased risk of early progression (PFS: HR = 1.07, p = 0.003) and patient death (OS: HR = 1.05, p = 0.009; Post-Recurrence OS: HR = 1.05, p = 0.025) for three of our four survival metrics, while a greater number of surgical resections was associated with significantly decreased risk of progression (PFS: HR = 0.44, p = 0.002; Post-Recurrence PFS: HR = 0.46, p = 0.015) and patient death (OS: HR = 0.40, p < 0.001) for three of our four survival metrics.
Cox multivariate regression models (Table 4) were constructed to compare survival outcomes between the BEV Only, BEV + GK, and GK Only treatment groups while controlling for intergroup differences in age, gender, single vs. multifocal lesion, recurrence tumor volume, IDH and MGMT statuses, post-surgical KPS, number of bevacizumab cycles, steroid use, number of surgical resections, and number of other chemotherapeutic agents administered to the patients during their treatment course. Patients in the combination treatment group showed significant benefits in post-recurrence PFS and OS in comparison to the BEV Only group (BEV + GK vs. BEV Only, Post-Recurrence PFS: HR = 0.44, p = 0.028; BEV + GK vs. BEV Only, Post-Recurrence OS: HR = 0.32, p = 0.004), but not in comparison to the GK Only group (BEV + GK vs. GK Only, Post-Recurrence PFS: HR = 1.45, p = 0.37; BEV + GK vs. GK Only, Post-Recurrence OS: HR = 1.27, p = 0.58). The GK Only also showed significant improvements in Post-Recurrence PFS and OS in comparison to the BEV Only group on multivariate analysis (BEV Only vs. GK Only, Post-Recurrence PFS: HR = 8.19, p = 0.0080; BEV Only vs. GK Only, Post-Recurrence OS: HR = 5.58, p = 0.032).
Discussion
Few studies have examined the combined use of bevacizumab and stereotactic radiosurgery in the treatment of recurrent GBM. Case series suggest promising but inconclusive results due to their small sample sizes and insufficient controls for demographic and treatment variability [16, 17]. A recent study by Morris et al. reported improvements in PFS and OS in rGBM patients treated with bevacizumab and Gamma Knife versus Gamma Knife alone when combining their results with other published studies [18]. However, a formal meta-analysis was not performed to reach this conclusion and significant variability existed between the study populations, as was stated by the authors. In our study, we examined whether bevacizumab and Gamma Knife SRS together, or as separate treatments, result in improved survival in rGBM by accounting for intergroup differences in patient demographics, tumor characteristics, number of surgical resections, functional scores, and other concurrently administered steroid and chemotherapeutic medications. Our results showed that patients treated with both bevacizumab and Gamma Knife had improved total and post-recurrence PFS and OS compared to patients previously reported in the literature [2], and was associated with superior survival outcomes compared to patients treated with bevacizumab or Gamma Knife alone.
Glioblastoma cells have been shown to produce high levels of VEGF which support angiogenesis, neovascularization, and tumor growth. In addition to being associated with higher recurrence rates and poorer patient prognosis [19, 20], increased levels of VEGF signaling promote the proliferation and tumorigenic properties of glioma stem cells, which are highly resistant to chemotherapy and radiation [21, 22]. Therefore, anti-VEGF agents such as bevacizumab could be included in standard treatment regimens for GBM in order to inhibit angiogenesis and slow tumor growth, while also controlling the development of abnormal peritumoral blood vessels to increase the delivery of systemic chemotherapeutic drugs [23,24,25]. Bevacizumab has been utilized as an antiangiogenic agent in the treatment of other forms of cancer and its use is associated with significant improvements in OS and PFS in advanced colorectal cancer [26], ovarian cancer [27], non-small cell lung cancer [28], and cervical cancer [29]. The effectiveness of bevacizumab in the treatment of GBM, on the other hand, is more controversial, and major Phase III trials have previously only shown improvements in PFS without any effects on OS [30,31,32]. However, a recent Cochrane review which included 11 randomized, controlled trials studying the use of antiangiogenic agents in the treatment of both newly-diagnosed and recurrent high-grade glioma, found a PFS benefit as well as modest improvements in OS for both disease groups when antiangiogenic agents were given in combination with chemotherapy (reported as HR = 0.92, p = 0.05) [33].
The mechanism by which radiation treatment controls tumor growth is complex, but is thought to include to the production of free radicals which damage DNA and trigger apoptotic signaling pathways in proliferating cells [1]. SRS treatment also alters the microvasculature of tumors, resulting in decreased capillary density and stenosis of blood vessels in the affected area [34]. The efficacy of SRS is therefore in part related to the radiosensitivity of endothelial cells which comprise the tumor vasculature [35]. Tumor cells are capable of developing radioresistance through the production of cytokines that have protective and proliferative effects on endothelial cells [36]. In particular, radiation exposure has been shown to greatly increase the expression of HIF-1 with downstream induction of VEGF production by tumor cells, triggering the formation of new peritumoral vasculature to replace damaged and narrowed vessels [36]. Therefore, mechanistically, we thought pairing bevacizumab with SRS would constitute a logical therapeutic paradigm. A meta-analysis by Larson et al. of 9 studies from 2005 to 2013 found that median OS in rGBM was significantly higher (range 16.7 to 33.3 months) in the group treated with adjunct Gamma Knife radiosurgery, with the greatest survival benefit observed in the subgroup of patients who received re-resection or bevacizumab along with Gamma Knife [6].
Bevacizumab has previously been used as an adjunct to radiation treatment in order to ameliorate symptoms caused by cerebral edema through the “normalization” of weak, highly permeable vessels in the irradiated area. This hypothetically would allow for higher and better tolerated radiation doses, which has been suggested could improve PFS and OS [16, 20, 37]. Our study presents the largest sample population to date of patients treated with this combined regimen for rGBM. Patients in the BEV + GK and GK Only groups showed improved PFS and OS compared to other GBM patients reported in the literature, with significant improvements in survival outcome associated with the combination treatment group. Consistent with previous reports, we also found that patients who received only bevacizumab showed improvements in PFS but not in OS.
While post-recurrence survival outcomes in the GK Only group showed significant improvements over the BEV Only group on multivariate analysis, our population results showed that maximal survival benefits were observed in the group in which Gamma Knife administration is combined with bevacizumab use, as we had proposed mechanistically above. Patient age and number of surgical resections had significant effects on disease progression and patient death on univariate analysis, but improvements in post-recurrence PFS and OS attributed to differences in treatment were demonstrably robust on multivariate analysis when these differences in patient demographics and clinical variables were controlled between groups. Tumor volumes at the post-surgical, recurrence, and first post-treatment timepoints were also found to be significantly lower for the combination treatment group compared to the monotherapy groups on aggregate analysis. These findings reflect previous studies showing that control of tumor size does have an effect on the overall patient survival, though, ultimately, these initially observed differences lose significance over time (at Second Post-Treatment, Third Post-Treatment, and Last Recorded Tumor Volumes), suggesting that bevacizumab administration following Gamma Knife treatment has a more prominent role in sustaining long-term survival than short-term benefits gained from reresection.
Limitations of our study include a high proportion of excluded patients and its retrospective nature potentially leading to selection bias, in addition to possible confounds related to volumetric-based data collection. Contrast enhancement has been known to be influenced by factors such as corticosteroid use, postsurgical inflammation, and radiation necrosis [20], and tumor volume measurements are also complicated by operator variability, difficulty including nonenhancing portions of the tumor, and enhancement of the surgical resection cavity [38]. Decreases in tumor enhancement observed following initiation of bevacizumab therapy may be caused by improved control of peritumoral edema, rather than reductions in the actual size of the tumor (referred to as “pseudoresponse”) [39]. Temporal bias regarding the timing of Gamma Knife before or after starting bevacizumab may also confound our calculations of changes in tumor volume, as bevacizumab use may have an effect on improving Gamma Knife planning by reducing nontumor-related enhancement. An analysis of the timing of Gamma Knife and bevacizumab administration and its effects on survival outcomes may require a larger study to fully articulate their benefits. Conversely, Bevacizumab may also make it more difficult to visualize previously enhancing as well as nonenhancing lesions and thereby confound determinations of PFS predicated on observing tumor progression on MRI. However, these radiological considerations would not impact OS, which would be enough to demonstrate a therapeutic advantage to using bevacizumab and SRS when compared with other regimens reported in the literature. Future studies may benefit from the inclusion of serial neurocognitive assessments in order to follow trends in patient functional status over time and provide a better measurement of PFS.
Our results demonstrate that the use of both bevacizumab and Gamma Knife SRS may improve survival for patients with first-recurrence GBM. They further suggest that combined, multimodal approaches are required for a disease as complex as GBM, and it is the hope of the authors that our study contributes to the further development of such treatment regimens in the future.
Conclusions
In this retrospective study, the combined use of bevacizumab and Gamma Knife in patients with recurrent glioblastoma improved progression-free and overall survival compared to patients who received only bevacizumab or Gamma Knife as monotherapy. Our findings support previous studies in the literature which suggested that a combined regimen of an antiangiogenic agent with stereotactic radiosurgery can improve survival in patients with recurrent disease, although a prospective randomized study would be required in the future to address this question more definitively.
Data availability
Data supporting the findings of this study will be made available by the corresponding author upon request.
Abbreviations
- ANOVA:
-
Analysis of variance
- BEV:
-
Bevacizumab
- CNS:
-
Central nervous system
- GBM:
-
Glioblastoma
- GK:
-
Gamma Knife
- Gy:
-
Gray
- HIF:
-
Hypoxia-inducible factor
- IDH:
-
Isocitrate dehydrogenase
- IQR:
-
Interquartile range
- IRB:
-
Institutional review board
- KPS:
-
Karnofsky performance scale
- MGMT:
-
O-6 methylguanine-DNA methyltransferase
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- SD:
-
Standard deviation
- SRS:
-
Stereotactic radiosurgery
- VEGF:
-
Vascular endothelial growth factor
- WT:
-
Wild-type
References
Crowley RW, Pouratian N, Sheehan JP (2006) Gamma knife surgery for glioblastoma multiforme. Neurosurg Focus. 20(4):E17. https://doi.org/10.3171/foc.2006.20.4.11
Stupp R, Taillibert S, Kanner A et al (2017) Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a randomized clinical trial. JAMA 318(23):2306–2316. https://doi.org/10.1001/jama.2017.18718
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. https://doi.org/10.1056/NEJMoa043330
Fabian D, Guillermo Prieto Eibl MDP, Alnahhas I et al (2019) Treatment of glioblastoma (GBM) with the addition of Tumor-Treating Fields (TTF): a review. Cancers (Basel). 11(2):174. https://doi.org/10.3390/cancers11020174
Holdhoff M, Grossman SA (2011) Controversies in the adjuvant therapy of high-grade gliomas. Oncologist 16(3):351–358. https://doi.org/10.1634/theoncologist.2010-0335
Larson EW, Peterson HE, Lamoreaux WT et al (2014) Clinical outcomes following salvage Gamma Knife radiosurgery for recurrent glioblastoma. World J Clin Oncol 5(2):142–148. https://doi.org/10.5306/wjco.v5.i2.142
Weller M, Cloughesy T, Perry JR, Wick W (2013) Standards of care for treatment of recurrent glioblastoma–are we there yet? Neuro Oncol 15(1):4–27. https://doi.org/10.1093/neuonc/nos273
Hochberg FH, Pruitt A (1980) Assumptions in the radiotherapy of glioblastoma. Neurology 30(9):907–911. https://doi.org/10.1212/wnl.30.9.907
Patrick HH, Sherman JH, Elder JB, Olson JJ (2022) Congress of neurological surgeons systematic review and evidence-based guidelines update on the role of cytoreductive surgery in the management of progressive glioblastoma in adults. J Neurooncol 158(2):167–177. https://doi.org/10.1007/s11060-021-03881-w
Ziu M, Goyal S, Olson JJ (2022) Congress of neurological surgeons systematic review and evidence-based guidelines update on the role of radiation therapy in the management of progressive and recurrent glioblastoma in adults. J Neurooncol 158(2):255–264. https://doi.org/10.1007/s11060-021-03857-w
Germano IM, Ziu M, Wen P, Ormond DR, Olson JJ (2022) Congress of neurological surgeons systematic review and evidence-based guidelines update on the role of cytotoxic chemotherapy and other cytotoxic therapies in the management of progressive glioblastoma in adults. J Neurooncol 158(2):225–253. https://doi.org/10.1007/s11060-021-03900-w
Winograd E, Germano I, Wen P, Olson JJ, Ormond DR (2022) Congress of Neurological Surgeons systematic review and evidence-based guidelines update on the role of targeted therapies and immunotherapies in the management of progressive glioblastoma. J Neurooncol 158(2):265–321. https://doi.org/10.1007/s11060-021-03876-7
Wong ET, Hess KR, Gleason MJ et al (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17(8):2572–2578. https://doi.org/10.1200/JCO.1999.17.8.2572
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23(8):1231–1251. https://doi.org/10.1093/neuonc/noab106
Louis DN, International Agency for Research on C. WHO classification of tumours of the central nervous system. rev. 4th ed. World Health Organization classification of tumours. International Agency for Research on Cancer; 2016.
Abbassy M, Missios S, Barnett GH et al (2018) Phase I trial of radiosurgery dose escalation plus bevacizumab in patients with recurrent/progressive glioblastoma. Neurosurg 83(3):385–392. https://doi.org/10.1093/neuros/nyx369
Park KJ, Kano H, Iyer A et al (2012) Salvage Gamma Knife stereotactic radiosurgery followed by bevacizumab for recurrent glioblastoma multiforme: a case-control study. J Neurooncol 107(2):323–333. https://doi.org/10.1007/s11060-011-0744-9
Morris SL, Zhu P, Rao M et al (2019) Gamma knife stereotactic radiosurgery in combination with bevacizumab for recurrent glioblastoma. World Neurosurg 127:e523–e533. https://doi.org/10.1016/j.wneu.2019.03.193
Wang R, Chadalavada K, Wilshire J et al (2010) Glioblastoma stem-like cells give rise to tumour endothelium. Nature 468(7325):829–833. https://doi.org/10.1038/nature09624
Sweet JA, Feinberg ML, Sherman JH (2012) The role of avastin in the management of recurrent glioblastoma. Neurosurg Clin N Am. 23(2):331–341. https://doi.org/10.1016/j.nec.2012.02.001
Xu C, Wu X, Zhu J (2013) VEGF promotes proliferation of human glioblastoma multiforme stem-like cells through VEGF receptor 2. ScientificWorldJournal 2013:417413. https://doi.org/10.1155/2013/417413
Bao S, Wu Q, Sathornsumetee S et al (2006) Stem cell-like glioma cells promote tumor angiogenesis through vascular endothelial growth factor. Cancer Res 66(16):7843–7848. https://doi.org/10.1158/0008-5472.CAN-06-1010
Dickson PV, Hamner JB, Sims TL et al (2007) Bevacizumab-induced transient remodeling of the vasculature in neuroblastoma xenografts results in improved delivery and efficacy of systemically administered chemotherapy. Clin Cancer Res 13(13):3942–3950. https://doi.org/10.1158/1078-0432.CCR-07-0278
Jain RK (2005) Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Sci 307(5706):58–62. https://doi.org/10.1126/science.1104819
Wong ET, Gautam S, Malchow C, Lun M, Pan E, Brem S (2011) Bevacizumab for recurrent glioblastoma multiforme: a meta-analysis. J Natl Compr Canc Netw 9(4):403–407. https://doi.org/10.6004/jnccn.2011.0037
Goey AK, Figg WD (2014) Potential novel role of bevacizumab in glioblastoma and cervical cancer. Cancer Biol Ther 15(10):1296–1298. https://doi.org/10.4161/cbt.29926
Perren TJ, Swart AM, Pfisterer J et al (2011) A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med 365(26):2484–2496. https://doi.org/10.1056/NEJMoa1103799
Johnson DH, Fehrenbacher L, Novotny WF et al (2004) Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 22(11):2184–2191. https://doi.org/10.1200/JCO.2004.11.022
Tewari KS, Sill MW, Penson RT et al (2017) Bevacizumab for advanced cervical cancer: final overall survival and adverse event analysis of a randomised, controlled, open-label, phase 3 trial (Gynecologic Oncology Group 240). Lancet 390(10103):1654–1663. https://doi.org/10.1016/S0140-6736(17)31607-0
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370(8):699–708. https://doi.org/10.1056/NEJMoa1308573
Chinot OL, Wick W, Mason W et al (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370(8):709–722. https://doi.org/10.1056/NEJMoa1308345
Wick W, Gorlia T, Bendszus M et al (2017) Lomustine and bevacizumab in progressive glioblastoma. N Engl J Med 377(20):1954–1963. https://doi.org/10.1056/NEJMoa1707358
Ameratunga M, Pavlakis N, Wheeler H, Grant R, Simes J, Khasraw M (2018) Anti-angiogenic therapy for high-grade glioma. Cochrane Database Syst Rev 11(11):CD008218. https://doi.org/10.1002/14651858.CD008218.pub4
Kamiryo T, Lopes MB, Kassell NF, Steiner L, Lee KS (2001) Radiosurgery-induced microvascular alterations precede necrosis of the brain neuropil. Neurosurg 49(2):409–415. https://doi.org/10.1097/00006123-200108000-00026
Garcia-Barros M, Paris F, Cordon-Cardo C et al (2003) Tumor response to radiotherapy regulated by endothelial cell apoptosis. Sci 300(5622):1155–1159. https://doi.org/10.1126/science.1082504
Moeller BJ, Cao Y, Li CY, Dewhirst MW (2004) Radiation activates HIF-1 to regulate vascular radiosensitivity in tumors: role of reoxygenation, free radicals, and stress granules. Cancer Cell 5(5):429–441. https://doi.org/10.1016/s1535-6108(04)00115-1
Zhuang H, Shi S, Yuan Z, Chang JY (2019) Bevacizumab treatment for radiation brain necrosis: mechanism, efficacy and issues. Mol Cancer 18(1):21. https://doi.org/10.1186/s12943-019-0950-1
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Kreisl TN, Kim L, Moore K et al (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27(5):740–745. https://doi.org/10.1200/JCO.2008.16.3055
Acknowledgements
None
Funding
The authors of this manuscript received no funding from any sources internal or external for any of the materials or findings related to this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: JFZ, JL, DP, RAF Data curation: JFZ, BO, AI, VG Formal analysis: JFZ Funding acquisition: N/A Investigation: All authors Methodology: All authors Project administration: DP, RAF Resources: N/A Supervision: DP, RAF Validation: All authors Writing—original draft: JFZ Writing—reviewing and editing: All authors.
Corresponding author
Ethics declarations
Conflict of interests
JFZ, BO, AI, VG, KA, JL, RMH, APA, DP, RAF: None.
Ethical approval
Written consent was obtained from all patients or their healthcare proxies before procedures were performed. This study was approved by the Roswell Park Comprehensive Cancer Center institutional review board, IRB ID: STUDY00001952 (BDR 159822).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J.F., Okai, B., Iovoli, A. et al. Bevacizumab and gamma knife radiosurgery for first-recurrence glioblastoma. J Neurooncol 166, 89–98 (2024). https://doi.org/10.1007/s11060-023-04524-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04524-y