Abstract
Objective
To compare the clinical outcomes of large or giant vestibular schwannomas (VSs) between older patients and younger patients who underwent microsurgery and to explore whether the incidence of postoperative complications increased and whether the postoperative hospital stay was prolonged.
Methods
We conducted a retrospective matched cohort study based on the surgical approach, maximum tumor diameter and extent of resection. Older patients (≥ 60 years) and a matched group (<60 years) who had undergone microsurgery for VSs between January 2015 and December 2021 were included. Clinical data, surgical outcomes and postoperative complications were analyzed statistically.
Results
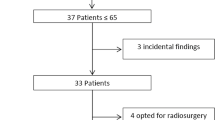
Forty-two older patients (≥ 60 years, 66.0 ± 3.8 years) were identified and matched to younger patients (<60 years, 43.9 ± 11.2 years), and they all underwent microsurgery through a retrosigmoid approach. There were twenty-nine patients with 3–4 cm VSs and thirteen patients with > 4 cm VSs in both groups. The older patients had a higher proportion of imbalance (P = 0.016) and lower American Society of Anesthesiology scores (P = 0.003) before surgery than the younger patients. There was no significant difference in facial nerve function one week (p = 0.851) and one year (p = 0.756) after surgery and no difference in the postoperative complication incidence (40.5% vs. 23.8%, p = 0.102) between the older patients and controls. Furthermore, the older patients had longer postoperative hospital stays than the younger patients (p = 0.043). In the older group, six patients with near total resection and five with subtotal resection were administered stereotactic radiotherapy, and one had recurrence three years after surgery and received conservative treatment. The postoperative follow-up time ranged from 1 to 83 months, with an average of 33.5 ± 21.1 months.
Conclusions
For older patients (≥ 60 years) with symptomatic, large or giant -VSs, microsurgery is the only effective method to prolong lifespan, alleviate clinical symptoms and cure the tumor. However, radical resection of VSs may result in a decreased preservation rate of facial-acoustic nerve function and an increased postoperative complication incidence. Therefore, subtotal resection followed by stereotactic radiotherapy should be recommended.


Similar content being viewed by others
Change history
29 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11060-023-04423-2
Abbreviations
- nASA:
-
American Society of Anesthesiology
- nGTR:
-
Gross total resection
- nHB:
-
House Brackmann
- nLOS:
-
Length of stay
- nNTR:
-
Near total resection
- nSTR:
-
Subtotal resection
- VSs:
-
Vestibular schwannomas
References
Carlson ML, Link MJ (2021) Vestibular Schwannomas. N Engl J Med 384:1335–1348. https://doi.org/10.1056/NEJMra2020394
Carlson ML et al (2015) Long-term quality of life in patients with vestibular schwannoma: an international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery, observation, and nontumor controls. J Neurosurg 122:833–842. https://doi.org/10.3171/2014.11.JNS14594
Whitmore RG et al (2011) Decision analysis of treatment options for vestibular schwannoma. J Neurosurg 114:400–413. https://doi.org/10.3171/2010.3.JNS091802
Liu W et al (2015) How to address small- and medium-sized acoustic neuromas with hearing: a systematic review and decision analysis. World Neurosurg 84:283–291e281. https://doi.org/10.1016/j.wneu.2015.03.013
Gauden A, Weir P, Hawthorne G, Kaye A (2011) Systematic review of quality of life in the management of vestibular schwannoma. J Clin Neurosci 18:1573–1584. https://doi.org/10.1016/j.jocn.2011.05.009
Muzevic D, Legcevic J, Splavski B (2014) Caye-Thomasen, P. Stereotactic radiotherapy for vestibular schwannoma. Cochrane Database Syst Rev CD009897. https://doi.org/10.1002/14651858.CD009897.pub2
Boublata L et al (2017) Facial nerve function and quality of Resection in large and giant vestibular schwannomas surgery operated by Retrosigmoid Transmeatal Approach in semi-sitting position with intraoperative facial nerve monitoring. World Neurosurg 103:231–240. https://doi.org/10.1016/j.wneu.2017.02.053
Huang X et al (2017) Functional outcome and complications after the microsurgical removal of giant vestibular schwannomas via the retrosigmoid approach: a retrospective review of 16-year experience in a single hospital. BMC Neurol 17:18. https://doi.org/10.1186/s12883-017-0805-6
Van Abel KM, Carlson ML, Driscoll CL, Neff BA, Link MJ (2014) Vestibular schwannoma surgery in the elderly: a matched cohort study. J Neurosurg 120:207–217. https://doi.org/10.3171/2013.6.JNS122433
Bowers CA et al (2016) Surgical treatment of vestibular Schwannoma: does Age Matter? World Neurosurg 96:58–65. https://doi.org/10.1016/j.wneu.2016.08.054
Jiang N et al (2017) Microsurgical outcomes after gross total resection on vestibular Schwannoma in Elderly Patients: a matched cohort study. World Neurosurg 101:457–465. https://doi.org/10.1016/j.wneu.2017.01.120
Mak PH, Campbell RC, Irwin MG (2002) American society of, a. The ASA Physical Status Classification: inter-observer consistency. American Society of Anesthesiologists. Anaesth Intensive Care 30:633–640. https://doi.org/10.1177/0310057X0203000516
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93:146–147. https://doi.org/10.1177/019459988509300202
Committee on Hearing and Equilibrium guidelines for the (1995) Evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). American Academy of Otolaryngology-Head and Neck surgery Foundation, INC. Otolaryngol Head Neck Surg 113:179–180. https://doi.org/10.1016/S0194-5998(95)70101-X
Gurgel RK, Dogru S, Amdur RL, Monfared A (2012) Facial nerve outcomes after surgery for large vestibular schwannomas: do surgical approach and extent of resection matter? Neurosurg Focus 33:E16. https://doi.org/10.3171/2012.7.FOCUS12199
Glasscock ME 3 et al (1997) Management of acoustic neuroma in the elderly population. Am J Otol 18:236–241 discussion 241 – 232
Perry BP, Gantz BJ, Rubinstein JT (2001) Acoustic neuromas in the elderly. Otol Neurotol 22:389–391. https://doi.org/10.1097/00129492-200105000-00020
Piazza F, Frisina A, Gandolfi A, Quaranta N, Zini C (2003) Management of acoustic neuromas in the elderly: retrospective study. Ear Nose Throat J 82:374–378
Persson O et al (2017) Stereotactic radiosurgery vs. fractionated radiotherapy for tumor control in vestibular schwannoma patients: a systematic review. Acta Neurochir (Wien) 159:1013–1021. https://doi.org/10.1007/s00701-017-3164-6
Golfinos JG et al (2016) A matched cohort comparison of clinical outcomes following microsurgical resection or stereotactic radiosurgery for patients with small- and medium-sized vestibular schwannomas. J Neurosurg 125:1472–1482. https://doi.org/10.3171/2015.12.JNS151857
Bailo M et al (2016) Gamma Knife Radiosurgery as Primary Treatment for large vestibular Schwannomas: clinical results at Long-Term Follow-Up in a series of 59 patients. World Neurosurg 95:487–501. https://doi.org/10.1016/j.wneu.2016.07.117
Roehm PC, Gantz BJ (2007) Management of acoustic neuromas in patients 65 years or older. Otol Neurotol 28:708–714. https://doi.org/10.1097/01.mao.0000281805.44197.ec
Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB (2009) Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med 169:938–944. https://doi.org/10.1001/archinternmed.2009.66
Bretonnier M et al (2020) Functional sparing surgery policy for giant vestibular schwannomas. Clin Otolaryngol 45:762–767. https://doi.org/10.1111/coa.13588
Haque R et al (2011) Efficacy of facial nerve-sparing approach in patients with vestibular schwannomas. J Neurosurg 115:917–923. https://doi.org/10.3171/2011.7.JNS101921
Brokinkel B et al (2014) Gamma Knife radiosurgery following subtotal resection of vestibular schwannoma. J Clin Neurosci 21:2077–2082. https://doi.org/10.1016/j.jocn.2014.03.037
Radwan H et al (2021) Subtotal Resection followed by adjuvant radiosurgery for large vestibular Schwannomas: outcomes with regard to the timing and regimen of irradiation. Acta Neurochir Suppl 128:1–5. https://doi.org/10.1007/978-3-030-69217-9_1
van de Langenberg R et al (2011) Management of large vestibular schwannoma. Part I. Planned subtotal resection followed by Gamma Knife surgery: radiological and clinical aspects. J Neurosurg 115:875–884. https://doi.org/10.3171/2011.6.JNS101958
Starnoni D et al (2018) Systematic review and meta-analysis of the technique of subtotal resection and stereotactic radiosurgery for large vestibular schwannomas: a “nerve-centered” approach. Neurosurg Focus 44:E4. https://doi.org/10.3171/2017.12.FOCUS17669
Author information
Authors and Affiliations
Contributions
QY and ZTZ: chief surgeon, writing—review and editing. WYX, CQ, and ZM: writing—original draft preparation. XYF: data collection and arrangement. LJT: statistical analysis. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest, no financial relationship with any organization that might have an interest in the submitted work in the previous three years.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tianzhi Zhao is the first corresponding author.
Yingxi Wu, Qing Cai and Min Zheng have contributed equally to this work.
The original version of this article has been revised: The copyright holder name has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Y., Cai, Q., Zheng, M. et al. Clinical outcomes and safety of large or giant vestibular schwannoma in older patients undergoing microsurgery: a matched cohort study. J Neurooncol 163, 429–437 (2023). https://doi.org/10.1007/s11060-023-04330-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04330-6