Abstract
Purpose
Iatrogenic neurologic deficits adversely affect patient outcomes following brain tumor resection. Motor evoked potential (MEP) monitoring allows surgeons to assess the integrity of motor-eloquent areas in real-time during tumor resection to lessen the risk of iatrogenic insult. We retrospectively associate intraoperative transcranial and direct cortical MEPs (TC-MEPs, DC-MEPs) to early and late post-operative motor function to prognosticate short- and long-term motor recovery in brain tumor patients undergoing surgical resection in peri-eloquent regions.
Methods
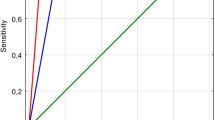
We reviewed 121 brain tumor patients undergoing craniotomies with DC-MEP and/or TC-MEP monitoring. Motor function scores were recorded at multiple time-points up to 1 year postoperatively. Sensitivity, specificity, and positive and negative predictive values (PPV, NPV) were calculated at each time point.
Results
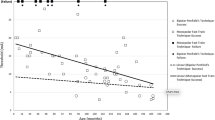
The sensitivity, specificity, PPV, and NPV of TC-MEP in the immediate postoperative period was 17.5%, 100%, 100%, and 69.4%, respectively. For DC-MEP monitoring, the respective values were 25.0%, 100%, 100%, and 68.8%. By discharge, sensitivity had increased for both TC-MEP and DC MEPs to 43.8%, and 50.0% respectively. Subset analysis on patients without tumor recurrence/progression at long term follow-up (n = 62 pts, 51.2%) found that all patients with stable monitoring maintained or improved from preoperative status. One patient with transient intraoperative TC-MEP loss and permanent DC-MEP loss suffered a permanent deficit.
Conclusion
Brain tumor patients who undergo surgery with intact MEP monitoring and experience new postoperative deficits likely suffer transient deficits that will improve over the postoperative course in the absence of disease progression.
Similar content being viewed by others
References
Giampiccolo D, Parisi C, Meneghelli P et al (2021) Long-term motor deficit in brain tumour surgery with preserved intra-operative motor-evoked potentials. Brain Commun. 3(1):fcaa226. https://doi.org/10.1093/braincomms/fcaa226
Zhang N, Yu Z, Hameed NUF et al (2018) Long-term functional and oncologic outcomes of glioma surgery with and without intraoperative neurophysiologic monitoring: a retrospective cohort study in a single center. World Neurosurg 119:e94–e105. https://doi.org/10.1016/j.wneu.2018.07.051
Duffau H, Capelle L, Denvil D et al (2003) Usefulness of intraoperative electrical subcortical mapping during surgery for low-grade gliomas located within eloquent brain regions: functional results in a consecutive series of 103 patients. J Neurosurg 98(4):764–778. https://doi.org/10.3171/jns.2003.98.4.0764
Taniguchi M, Cedzich C, Schramm J (1993) Modification of cortical stimulation for motor evoked potentials under general anesthesia: technical description. Neurosurgery 32(2):219–226. https://doi.org/10.1227/00006123-199302000-00011
Kombos T, Suess O, Ciklatekerlio O, Brock M (2001) Monitoring of intraoperative motor evoked potentials to increase the safety of surgery in and around the motor cortex. J Neurosurg 95(4):608–614. https://doi.org/10.3171/jns.2001.95.4.0608
Kombos T, Suss O, Vajkoczy P (2009) Subcortical mapping and monitoring during insular tumor surgery. Neurosurg Focus 27(4):E5. https://doi.org/10.3171/2009.8.FOCUS09140
Duffau H, Lopes M, Arthuis F et al (2005) Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985–96) and with (1996–2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry 76(6):845–851. https://doi.org/10.1136/jnnp.2004.048520
Pan SY, Chen JP, Cheng WY, Lee HT, Shen CC (2020) The role of tailored intraoperative neurophysiological monitoring in glioma surgery: a single institute experience. J Neurooncol 146(3):459–467. https://doi.org/10.1007/s11060-019-03347-0
Wilder P, Boldrey E (1937) Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain 60(4):389–443. https://doi.org/10.1093/brain/60.4.389
Silverstein JW, Rosenthal A, Ellis JA (2018) Direct cortical motor evoked potentials versus transcranial motor evoked potentials for the detection of cortical ischemia during supratentorial craniotomy: case report. Cureus. 10(12):e3771. https://doi.org/10.7759/cureus.3771
Jones SJ, Harrison R, Koh KF, Mendoza N, Crockard HA (1996) Motor evoked potential monitoring during spinal surgery: responses of distal limb muscles to transcranial cortical stimulation with pulse trains. Electroencephalogr Clin Neurophysiol 100(5):375–383
Pechstein U, Cedzich C, Nadstawek J, Schramm J (1996) Transcranial high-frequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 39(2):335–343. https://doi.org/10.1097/00006123-199608000-00020
Rodi Z, Deletis V, Morota N, Vodusek DB (1996) Motor evoked potentials during brain surgery. Pflugers Arch 431(6 Suppl 2):R291–R292. https://doi.org/10.1007/BF02346383
Do HJ, Seo HG, Oh BM et al (2018) Limitation of intraoperative transcranial electrical stimulation-motor evoked potential monitoring during brain tumor resection adjacent to the primary motor cortex. Ann Rehabil Med 42(5):767–772. https://doi.org/10.5535/arm.2018.42.5.767
Neuloh G, Schramm J (2009) Are there false-negative results of motor evoked potential monitoring in brain surgery? Cent Eur Neurosurg 70(4):171–175. https://doi.org/10.1055/s-0029-1225651
Szelenyi A, Langer D, Beck J et al (2007) Transcranial and direct cortical stimulation for motor evoked potential monitoring in intracerebral aneurysm surgery. Neurophysiol Clin 37(6):391–398. https://doi.org/10.1016/j.neucli.2007.09.006
Li F, Deshaies EM, Allott G, Canute G, Gorji R (2011) Direct cortical stimulation but not transcranial electrical stimulation motor evoked potentials detect brain ischemia during brain tumor resection. Am J Electroneurodiagnostic Technol 51(3):191–197
Motoyama Y, Kawaguchi M, Yamada S et al (2011) Evaluation of combined use of transcranial and direct cortical motor evoked potential monitoring during unruptured aneurysm surgery. Neurol Med Chir (Tokyo) 51(1):15–22. https://doi.org/10.2176/nmc.51.15
Umemura T, Nishizawa S, Nakano Y et al (2018) Intraoperative monitoring of motor-evoked potential for parenchymal brain tumor removal: an analysis of false-negative cases. J Clin Neurosci 57:105–110. https://doi.org/10.1016/j.jocn.2018.08.019
Legatt AD, Emerson RG, Epstein CM et al (2016) ACNS guideline: transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol 33(1):42–50. https://doi.org/10.1097/WNP.0000000000000253
Krammer MJ, Wolf S, Schul DB, Gerstner W, Lumenta CB (2009) Significance of intraoperative motor function monitoring using transcranial electrical motor evoked potentials (MEP) in patients with spinal and cranial lesions near the motor pathways. Br J Neurosurg 23(1):48–55. https://doi.org/10.1080/02688690802563349
Lee S, Kim DY, Kim SB et al (2019) Predictive value of neurophysiologic monitoring during neurovascular intervention for postoperative new neurologic deficits. Neuroradiology 61(2):207–215. https://doi.org/10.1007/s00234-018-2115-0
Neuloh G, Pechstein U, Cedzich C, Schramm J (2004) Motor evoked potential monitoring with supratentorial surgery. Neurosurgery 54(5):1061–1072
Plans G, Fernandez-Conejero I, Rifa-Ros X, Fernandez-Coello A, Rossello A, Gabarros A (2017) Evaluation of the high-frequency monopolar stimulation technique for mapping and monitoring the corticospinal tract in patients with supratentorial gliomas. A proposal for intraoperative management based on neurophysiological data analysis in a series of 92 patients. Neurosurgery 81(4):585–594. https://doi.org/10.1093/neuros/nyw087
Krieg SM, Shiban E, Droese D et al (2012) Predictive value and safety of intraoperative neurophysiological monitoring with motor evoked potentials in glioma surgery. Neurosurgery 70(5):1060–1070. https://doi.org/10.1227/NEU.0b013e31823f5ade
Boex C, Haemmerli J, Momjian S, Schaller K (2016) Prognostic values of motor evoked potentials in insular, precental, or postcentral resections. J Clin Neurophysiol 33(1):51–59. https://doi.org/10.1097/WNP.0000000000000227
Macdonald DB (2006) Intraoperative motor evoked potential monitoring: overview and update. J Clin Monit Comput 20(5):347–377. https://doi.org/10.1007/s10877-006-9033-0
Obermueller T, Schaeffner M, Shiban E et al (2015) Intraoperative neuromonitoring for function-guided resection differs for supratentorial motor eloquent gliomas and metastases. BMC Neurol 15:211. https://doi.org/10.1186/s12883-015-0476-0
Vigano L, Callipo V, Lamperti M et al (2022) Transcranial versus direct electrical stimulation for intraoperative motor-evoked potential monitoring: prognostic value comparison in asleep brain tumor surgery. Front Oncol 12:963669. https://doi.org/10.3389/fonc.2022.963669
Zetterling M, Elf K, Semnic R, Latini F, Engstrom ER (2020) Time course of neurological deficits after surgery for primary brain tumours. Acta Neurochir (Wien) 162(12):3005–3018. https://doi.org/10.1007/s00701-020-04425-3
Kim YH, Kim CH, Kim JS et al (2013) Risk factor analysis of the development of new neurological deficits following supplementary motor area resection. J Neurosurg 119(1):7–14. https://doi.org/10.3171/2013.3.JNS121492
Palmisciano P, Haider AS, Balasubramanian K et al (2022) Supplementary motor area syndrome after brain tumor surgery: a systematic review. World Neurosurg. 165:160-171e2. https://doi.org/10.1016/j.wneu.2022.06.080
Dadario NB, Tabor JK, Silverstein J, Sun XR (2021) Postoperative focal lower extremity supplementary motor area syndrome: case report and review of the literature. Neurodiagn J. 61(4):169–185. https://doi.org/10.1080/21646821.2021.1991716
Gogos AJ, Young JS, Morshed RA et al (2020) Triple motor mapping: transcranial, bipolar, and monopolar mapping for supratentorial glioma resection adjacent to motor pathways. J Neurosurg 134(6):1728–1737. https://doi.org/10.3171/2020.3.JNS193434
MacDonald DB (2017) Overview on criteria for MEP monitoring. J Clin Neurophysiol 34(1):4–11. https://doi.org/10.1097/WNP.0000000000000302
Macdonald DB, Skinner S, Shils J, Yingling C, American Society of Neurophysiological M (2013) Intraoperative motor evoked potential monitoring—a position statement by the American Society of neurophysiological monitoring. Clin Neurophysiol 124(12):2291–2316. https://doi.org/10.1016/j.clinph.2013.07.025
Acknowledgements
Not applicable.
Funding
The authors declare no financial support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design and conception of the study. Data collection and analysis were conducted by JS, HS, PU, and SV. The first draft of the manuscript was prepared by JS, HS, PU and RD. All authors commented on and critically revised previous drafts of the manuscript and approved of the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no competing financial and/or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Silverstein, J.W., Shah, H.A., Unadkat, P. et al. Short and long-term prognostic value of intraoperative motor evoked potentials in brain tumor patients: a case series of 121 brain tumor patients. J Neurooncol 161, 127–133 (2023). https://doi.org/10.1007/s11060-022-04229-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04229-8