Abstract
Purpose
Brain tumor patients report an overwhelming sense of uncertainty when navigating the course of their terminal disease. Historically, organizational experts and/or treating physicians have established neuro-oncology programs. However, given the disease burden and incurable nature of current medical treatments, patient-centric care should be prioritized alongside institutional and academic objectives. Integrating patient perspectives into interdisciplinary programmatic development can improve comprehensive care and empower patients to advocate for their own quality healthcare needs.
Methods
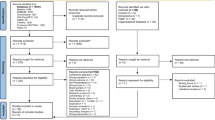
Data was derived from four focus groups with adult brain tumor patients (N = 15; Mage = 46 years, 53% female). A trained moderator led each 90-min group and posed semi-structured questions regarding patients’ care needs throughout their neuro-oncological disease trajectory. Emphasis was placed on quality of life and psychological distress reduction for both patients and their loved ones. Common themes were identified via thematic content analysis using NVivo software. A high inter-rater reliability (Mkappa = 0.92, range= 0.85–0.93) was achieved.
Results
Six distinct themes emerged, where the frequency of each theme ranged from 12.5 to 23.3%. Specifically, patients discussed relational concerns, navigation of interdisciplinary care, neurobehavioral impacts, emotional responses to stressors, existential concerns, and caregiver support. A discussion of themes follows.
Conclusions
It is imperative that we include the patient perspective in the development of neuro-oncology programs; considering the quality of survival in addition to quantity. Neuro-oncology quality care themes identified were relational concerns, navigating interdisciplinary care, neurobehavioral impact, emotional response to stressors, existential concerns, and caregiver support. A paramount concentration for comprehensive neuro-oncology programs must include patients’ quality needs.

Similar content being viewed by others
References
Ae SB, Ae PRS, Donovan HS et al (2007) I could lose everything: understanding the cost of a brain tumor. J Neuro-Oncol. https://doi.org/10.1007/s11060-007-9425-0
Salander P, Bergenheim AT, Henriksson R (2000) How was life after treatment of a malignant brain tumour? Soc Sci Med 51(4):589–598. https://doi.org/10.1016/S0277-9536(00)00002-2
Loughan AR, Aslanzadeh FJ, Brechbiel J et al (2020) Death-related distress in adult primary brain tumor patients. Neuro-oncol Pract 7(5):498–506. https://doi.org/10.1093/NOP/NPAA015
Loughan AR, Husain M, Ravyts SG et al (2021) Death anxiety in patients with primary brain tumor: measurement, prevalence, and determinants. Palliat Support Care 19(6):672–680. https://doi.org/10.1017/S1478951521000808
Braun SE, Aslanzadeh FJ, Thacker L, Loughan AR (2021) Examining fear of cancer recurrence in primary brain tumor patients and their caregivers using the actor-partner interdependence model. Psycho‐Oncology 30(7):1120–1128. https://doi.org/10.1002/PON.5659
Huang J, Zeng C, Xiao J et al (2017) Association between depression and brain tumor: a systematic review and meta-analysis. Oncotarget 8(55):94932–94943. https://doi.org/10.18632/ONCOTARGET.19843
Boele FW, Douw L, Reijneveld JC et al (2015) Health-related quality of life in stable, long-term survivors of low-grade glioma. J Clin Oncol 33(9):1023–1029. https://doi.org/10.1200/JCO.2014.56.9079
Meyers CA, Rock EP, Fine HA (2012) Methods and clinical tools for outcome assessments refining endpoints in brain tumor clinical trials. J Neuro-Oncol. https://doi.org/10.1007/s11060-012-0813-8
Armstrong TS, Gilbert MR (2014) Patient reported endpoints for measuring clinical benefit in (high grade glioma) primary brain tumor patients. Curr Treat Options Oncol 15(4):519–528. https://doi.org/10.1007/S11864-014-0302-8/FIGURES/1
Rosenblum ML, Mikkelsen T (2004) Developing a brain tumor center. J Neuro-Oncol 69(1):169–180
Leeper H, Milbury K (2018) Survivorship care planning and implementation in neuro-oncology. Neuro Oncol 20((suppl_7)):VII40–VII46. https://doi.org/10.1093/NEUONC/NOY110
Fong TG, Fearing MA, Jones RND et al (2009) The telephone interview for cognitive status: creating a crosswalk with the mini-mental state exam. Alzheimers Dement 5(6):492–497. https://doi.org/10.1016/j.jalz.2009.02.007
Saunders B, Sim J, Kingstone T et al (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 52:1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/J.JBI.2008.08.010
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706QP063OA
QSR International Pty Ltd. NVivo (2020)
IBM Corp. IBM SPSS Statistics for Windows (2020)
Ownsworth T, Chambers S, Hawkes A, Walker DG, Shum D (2010) Making sense of brain tumour: a qualitative investigation of personal and social processes of adjustment. Neuropsychol Rehabil 21(1):117–137. https://doi.org/10.1080/09602011.2010.537073
Goebel S, Von Harscher M, Mehdorn HM (2011) Comorbid mental disorders and psychosocial distress in patients with brain tumours and their spouses in the early treatment phase. Support Care Cancer. https://doi.org/10.1007/s00520-010-1021-8
Voß H, Scholz-Kreisel P, Richter C, Ringel F, Singer S (2021) Development of screening questions for doctor-patient consultation assessing the quality of life and psychosocial burden of glioma patients: an explorative study. Qual Life Res 30:1513–1522. https://doi.org/10.1007/s11136-021-02756-x
Cubis L, Ownsworth T, Pinkham MB, Foote M, Legg M, Chambers S (2019) The importance of staying connected: mediating and moderating effects of social group memberships on psychological well-being after brain tumor. Psychooncology 28:1537–1543. https://doi.org/10.1002/pon.5125
Ownsworth T, Chambers S, Damborg E, Casey L, Walker DG, Shum DHK (2014) Evaluation of the making sense of brain tumor program: a randomized controlled trial of a home-based psychosocial intervention. Psychooncology. https://doi.org/10.1002/pon.3687
Reblin M, Ketcher D, Forsyth P et al (2018) Outcomes of an electronic social network intervention with neuro-oncology patient family caregivers. J Neuro-Oncol 139(3):643–649. https://doi.org/10.1007/S11060-018-2909-2
Raj VS, Pugh TM, Yaguda SI, Mitchell CH, Mullan SS, Garces NS (2020) The who, what, why, when, where, and how of team-based interdisciplinary cancer rehabilitation. Semin Oncol Nurs 36(1):150974. https://doi.org/10.1016/J.SONCN.2019.150974
Gilbert J, Veazie S, Joines K et al (2018) Patient navigation models for. Lung Cancer. https://doi.org/10.23970/AHRQEPCRAPIDLUNG
Daniels J, Kissane DW (2008) Psychosocial interventions for cancer patients. Curr Opin Oncol 20(4):367–371. https://doi.org/10.1097/CCO.0B013E3283021658
Johannsen M, Farver I, Beck N, Zachariae R (2013) The efficacy of psychosocial intervention for pain in breast cancer patients and survivors: a systematic review and meta-analysis. Breast Cancer Res Treat 138:675–690. https://doi.org/10.1007/s10549-013-2503-4
Papadakos J, Barnsley J, Berta W, Rowlands G, Samoil D, Howell D (2022) The association of self-efficacy and health literacy to chemotherapy self-management behaviors and health service utilization. Suppor Care Cancer. 1:3. https://doi.org/10.1007/s00520-021-06466-5
Temkin SM, Reich R, Krok-Schoen JL, Oliveri JM, Paskett ED (2016) Cancer care delivery and women’s health: the role of patient navigation. Front Oncol 6:1. https://doi.org/10.3389/fonc.2016.00002
Randazzo D, Peters KB (2016) Psychosocial distress and its effects on the health-related quality of life of primary brain tumor patients. CNS Oncol 5(4):241–249. https://doi.org/10.2217/cns-2016-0010
Armstrong TS, Vera-Bolanos E, Acquaye AA, Gilbert MR, Ladha H, Mendoza T (2015) The symptom burden of primary brain tumors: evidence for a core set of tumor-and treatment-related symptoms. Neuro Oncol. https://doi.org/10.1093/neuonc/nov166
Kvale EA, Murthy R, Taylor R, Lee JY, Nabors LB (2009) Distress and quality of life in primary high-grade brain tumor patients. Support Care Cancer. https://doi.org/10.1007/s00520-008-0551-9
Salans M, Tibbs MD, Huynh-Le MP et al (2021) Quality of life is independently associated with neurocognitive function in patients with brain tumors: analysis of a prospective clinical trial. Int J Radiat Oncol Biol Phys 111(3):754–763. https://doi.org/10.1016/J.IJROBP.2021.05.134
Johnson DR, Sawyer AM, Meyers CA, Patrick O’neill B, Wefel JS (2012) Early measures of cognitive function predict survival in patients with newly diagnosed glioblastoma. Neuro Oncol. https://doi.org/10.1093/neuonc/nos082
Sato I, Higuchi A, Yanagisawa T et al (2018) Employment status and termination among survivors of pediatric brain tumors: a cross-sectional survey. Int J Clin Oncol 23(3):801–811. https://doi.org/10.1007/s10147-018-1279-2
Scholtes C, Baust K, Weinhold L et al (2019) Health status, health-related quality of life, and socioeconomic outcome in childhood brain tumor survivors: a German cohort study. Hann Med Sch 21(8):1069–1081. https://doi.org/10.1093/neuonc/noz044
Litofsky NS, Farace E, Anderson F, Meyers CA, Huang W, Laws ER (2004) Depression in patients with high-grade glioma: results of the glioma outcomes project. Neurosurgery 54(2):358–367. https://doi.org/10.1227/01.NEU.0000103450.94724.A2
Götze H, Brähler E, Gansera L, Polze N, Köhler N (2014) Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer 22(10):2775–2782. https://doi.org/10.1007/S00520-014-2257-5/TABLES/4
Kroenke K, Theobald D, Wu J, Loza JK, Carpenter JS, Tu W (2010) The association of depression and pain with health-related quality of life, disability, and health care use in cancer patients. J Pain Symptom Manag 40(3):327–341. https://doi.org/10.1016/J.JPAINSYMMAN.2009.12.023
Ng CG, Mohamed S, See MH et al (2015) Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: a 1-year prospective study. Health Qual Life Outcomes. https://doi.org/10.1186/S12955-015-0401-7
Ayres A, Hoon PW, Franzoni JB, Matheny KB, Cotanch PH, Takayanagi S (1994) Influence of mood and adjustment to cancer on compliance with chemotherapy among breast cancer patients. J Psychosom Res 38(5):393–402. https://doi.org/10.1016/0022-3999(94)90100-7
Holland JC (2018) Psycho-oncology: overview, obstacles and opportunities. Psycho‐Oncology 27(5):1364–1376. https://doi.org/10.1002/PON.4692
Min JA, Yoon S, Lee CU et al (2013) Psychological resilience contributes to low emotional distress in cancer patients. Support Care Cancer 21(9):2469–2476. https://doi.org/10.1007/S00520-013-1807-6
Dehghan M, Jazinizade M, Malakoutikhah A et al (2020) Stress and quality of life of patients with cancer: the mediating role of mindfulness. J Oncol. https://doi.org/10.1155/2020/3289521
Vehling S, Kissane DW (2018) Existential distress in cancer: alleviating suffering from fundamental loss and change. Psycho‐Oncology 27(11):2525–2530. https://doi.org/10.1002/PON.4872
Ownsworth T, Nash K (2015) Existential well-being and meaning making in the context of primary brain tumor: conceptualization and implications for intervention. Front Oncol. https://doi.org/10.3389/FONC.2015.00096
Pelletier G, Verhoef MJ, Khatri N, Hagen N (2002) Quality of life in brain tumor patients: the relative contributions of depression, fatigue, emotional distress, and existential issues. J Neuro-Oncol 57:41–49
Randazzo DM, McSherry F, Herndon JE et al (2021) Spiritual well-being and its association with health-related quality of life in primary brain tumor patients. Neuro-Oncol Pract 8(3):299–309. https://doi.org/10.1093/NOP/NPAA084
Breitbart W, Poppito S, Rosenfeld B et al (2012) Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol 30:1304–1309. https://doi.org/10.1200/JCO.2011.36.2517
Rodin G, Lo C, Rydall A et al (2018) Journal of clinical oncology managing cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol 36:2422–2432. https://doi.org/10.1200/JCO
Kissane DW, Love A, Hatton A et al (2004) Effect of cognitive-existential group therapy on survival in early-stage breast cancer. J Clin Oncol 22(21):4255–4260. https://doi.org/10.1200/JCO.2004.12.129
Chen D, Zhu J, Xu Q et al (2021) The role of informal caregivers for patients with glioma: a systematic review and meta-synthesis of qualitative studies. Ann Transl Med 9(12):1020. https://doi.org/10.21037/atm-21-2761
Boele FW (2019) Interventions to help support caregivers of people with a brain or spinal cord tumour (review). Cochrane Libr Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012582.pub2
Keir ST (2007) Levels of stress and intervention preferences of caregivers of brain tumor patients. Cancer Nurs. https://doi.org/10.1097/01.NCC.0000300174.18584.F9
National Brain Tumor Society. Quick Brain Tumor Facts. https://braintumor.org/brain-tumor-information/brain-tumor-facts/
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/J.1525-1497.2001.016009606.X
Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/ARCHINTE.166.10.1092
Krause S, Rydall A, Hales S, Rodin G, Lo C (2015) Initial validation of the death and dying distress scale for the assessment of death anxiety in patients with advanced cancer. J Pain Symptom Manag 49(1):126–134. https://doi.org/10.1016/J.JPAINSYMMAN.2014.04.012
Humphris GM, Watson E, Sharpe M, Ozakinci G (2018) Unidimensional scales for fears of cancer recurrence and their psychometric properties: the FCR4 and FCR7. Health Qual Life Outcomes. https://doi.org/10.1186/S12955-018-0850-X
Acknowledgements
Thank you to our patients who shared their voice on quality care in neuro-oncology
Funding
Funding was provided by Massey Cancer Center.
Author information
Authors and Affiliations
Contributions
ARL initiated project conceptualization. ARL and RLB managed methodology. All authors contributed to study analysis. All authors contributed to original writing and ARL, MR, KDW, RLB completed final editing. All authors reviewed the manuscript. ARL secured project funding.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loughan, A.R., Reid, M., Willis, K.D. et al. The burden of a brain tumor: guiding patient centric care in neuro-oncology. J Neurooncol 157, 487–498 (2022). https://doi.org/10.1007/s11060-022-03993-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03993-x