Abstract
Introduction
Many patients with glioma experience surgery-related language impairment. This study developed a classification system to predict postoperative language prognosis.
Methods
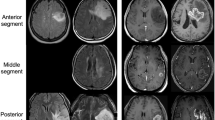
Sixty-eight patients were retrospectively reviewed. Based on their location, tumors were subtyped as follows: (I) inferior frontal lobe or precentral gyrus; (II) posterior central gyrus or supramarginal gyrus (above the lateral fissure level); (III) posterior region of the superior or middle temporal gyri or supramarginal gyrus (below the lateral fissure level); and (IV) insular lobe. The distance from the tumor to the superior longitudinal fasciculus/arcuate fasciculus was calculated. The recovery of language function was assessed using the Western Aphasia Battery before surgery, and a comprehensive language test was conducted on the day of surgery; 3, 7, and 14 days after surgery. Our follow-up information of was the comprehensive language test from telephone interviews in 3 months after surgery.
Results
Thirty-three patients experienced transient language impairment within 1 week of surgery. Fourteen patients had permanent language impairment. Type II tumors, shorter distance from the tumor to the posterior superior longitudinal fasciculus/arcuate fasciculus, and isocitrate dehydrogenase mutations were risk factors for surgery-related language impairment. Regarding the presence or absence of permanent surgery-related language impairments, the cut-off distance between the tumor and posterior superior longitudinal fasciculus/arcuate fasciculus was 2.75 mm.
Conclusions
According to our classification, patients with type II tumors had the worst language prognosis and longest recovery time. Our classification, based on tumor location, can reliably predict postoperative language status and may be used to guide tumor resection.



Similar content being viewed by others
Data availability
Anonymized data will be made available on request.
Change history
12 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11060-021-03871-y
References
Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2017) CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19:v1–v88. https://doi.org/10.1093/neuonc/nox158
Jiang T, Nam DH, Ram Z, Poon WS, Wang J, Boldbaatar D, Mao Y, Ma W, Mao Q, You Y, Jiang C, Yang X, Kang C, Qiu X, Li W, Li S, Chen L, Li X, Liu Z, Wang W, Bai H, Yao Y, Li S, Wu A, Sai K, Li G, Yao K, Wei X, Liu X, Zhang Z, Dai Y, Lv S, Wang L, Lin Z, Dong J, Xu G, Ma X, Zhang W, Zhang C, Chen B, You G, Wang Y, Wang Y, Bao Z, Yang P, Fan X, Liu X, Zhao Z, Wang Z, Li Y, Wang Z, Li G, Fang S, Li L, Liu Y, Liu S, Shan X, Liu Y, Chai R, Hu H, Chen J, Yan W, Cai J, Wang H, Chen L, Yang Y, Wang Y, Han L, Wang Q, Chinese Glioma Cooperative G, Society for Neuro-Oncology of C, Chinese Brain Cancer A, Chinese Glioma Genome A, Asian Glioma Genome Atlas n (2020) Clinical practice guidelines for the management of adult diffuse gliomas. Cancer Lett. https://doi.org/10.1016/j.canlet.2020.10.050
Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgard G, Solheim O (2012) Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA 308:1881–1888. https://doi.org/10.1001/jama.2012.12807
McGirt MJ, Chaichana KL, Attenello FJ, Weingart JD, Than K, Burger PC, Olivi A, Brem H, Quinones-Hinojosa A (2008) Extent of surgical resection is independently associated with survival in patients with hemispheric infiltrating low-grade gliomas. Neurosurgery 63:700–707; author reply 707–708. https://doi.org/10.1227/01.NEU.0000325729.41085.73
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S, Tihan T, Vandenberg S, McDermott MW, Berger MS (2008) Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol 26:1338–1345. https://doi.org/10.1200/JCO.2007.13.9337
Eseonu CI, Rincon-Torroella J, ReFaey K, Lee YM, Nangiana J, Vivas-Buitrago T, Quinones-Hinojosa A (2017) Awake craniotomy vs craniotomy under general anesthesia for perirolandic gliomas: evaluating perioperative complications and extent of resection. Neurosurgery 81:481–489. https://doi.org/10.1093/neuros/nyx023
Fang S, Bai HX, Fan X, Li S, Zhang Z, Jiang T, Wang Y (2020) A novel sequence: ZOOMit-blood oxygen level-dependent for motor-cortex localization. Neurosurgery 86:E124–E132. https://doi.org/10.1093/neuros/nyz441
Walker JA, Quinones-Hinojosa A, Berger MS (2004) Intraoperative speech mapping in 17 bilingual patients undergoing resection of a mass lesion. Neurosurgery 54:113–117. https://doi.org/10.1227/01.neu.0000097270.95721.3b (discussion 118)
Trinh VT, Fahim DK, Maldaun MV, Shah K, McCutcheon IE, Rao G, Lang F, Weinberg J, Sawaya R, Suki D, Prabhu SS (2014) Impact of preoperative functional magnetic resonance imaging during awake craniotomy procedures for intraoperative guidance and complication avoidance. Stereotact Funct Neurosurg 92:315–322. https://doi.org/10.1159/000365224
Ille S, Sollmann N, Hauck T, Maurer S, Tanigawa N, Obermueller T, Negwer C, Droese D, Zimmer C, Meyer B, Ringel F, Krieg SM (2015) Combined noninvasive language mapping by navigated transcranial magnetic stimulation and functional MRI and its comparison with direct cortical stimulation. J Neurosurg 123:212–225. https://doi.org/10.3171/2014.9.JNS14929
Duffau H, Moritz-Gasser S, Gatignol P (2009) Functional outcome after language mapping for insular World Health Organization Grade II gliomas in the dominant hemisphere: experience with 24 patients. Neurosurg Focus 27:E7. https://doi.org/10.3171/2009.5.FOCUS0938
Bu LH, Zhang J, Lu JF, Wu JS (2020) Glioma surgery with awake language mapping versus generalized anesthesia: a systematic review. Neurosurg Rev. https://doi.org/10.1007/s10143-020-01418-9
Zelitzki R, Korn A, Arial E, Ben-Harosh C, Ram Z, Grossman R (2019) Comparison of motor outcome in patients undergoing awake vs general anesthesia surgery for brain tumors located within or adjacent to the motor pathways. Neurosurgery 85:E470–E476. https://doi.org/10.1093/neuros/nyz007
Tuominen J, Yrjana S, Ukkonen A, Koivukangas J (2013) Awake craniotomy may further improve neurological outcome of intraoperative MRI-guided brain tumor surgery. Acta Neurochir (Wien) 155:1805–1812. https://doi.org/10.1007/s00701-013-1837-3
Sacko O, Lauwers-Cances V, Brauge D, Sesay M, Brenner A, Roux FE (2011) Awake craniotomy vs surgery under general anesthesia for resection of supratentorial lesions. Neurosurgery 68:1192–1198. https://doi.org/10.1227/NEU.0b013e31820c02a3 (discussion 1198-1199)
Pichierri A, Bradley M, Iyer V (2019) Intraoperative magnetic resonance imaging-guided glioma resections in awake or asleep settings and feasibility in the context of a public health system. World Neurosurg X 3:100022. https://doi.org/10.1016/j.wnsx.2019.100022
Peraud A, Ilmberger J, Reulen HJ (2004) Surgical resection of gliomas WHO grade II and III located in the opercular region. Acta Neurochir (Wien) 146:9–17. https://doi.org/10.1007/s00701-003-0165-4 (discussion 17-18)
Martino J, Gomez E, Bilbao JL, Duenas JC, Vazquez-Barquero A (2013) Cost-utility of maximal safe resection of WHO grade II gliomas within eloquent areas. Acta Neurochir (Wien) 155:41–50. https://doi.org/10.1007/s00701-012-1541-8
Gupta DK, Chandra PS, Ojha BK, Sharma BS, Mahapatra AK, Mehta VS (2007) Awake craniotomy versus surgery under general anesthesia for resection of intrinsic lesions of eloquent cortex–a prospective randomised study. Clin Neurol Neurosurg 109:335–343. https://doi.org/10.1016/j.clineuro.2007.01.008
Duffau H, Lopes M, Arthuis F, Bitar A, Sichez JP, Van Effenterre R, Capelle L (2005) Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985–96) and with (1996–2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry 76:845–851. https://doi.org/10.1136/jnnp.2004.048520
Fang S, Li Y, Wang Y, Zhang Z, Jiang T (2020) Awake craniotomy for gliomas involving motor-related areas: classification and function recovery. J Neurooncol 148:317–325. https://doi.org/10.1007/s11060-020-03520-w
Jehna M, Becker J, Zaar K, von Campe G, Mahdy Ali K, Reishofer G, Payer F, Synowitz M, Fazekas F, Enzinger C, Deutschmann H (2017) Symmetry of the arcuate fasciculus and its impact on language performance of patients with brain tumors in the language-dominant hemisphere. J Neurosurg 127:1407–1416. https://doi.org/10.3171/2016.9.JNS161281
Negwer C, Sollmann N, Ille S, Hauck T, Maurer S, Kirschke JS, Ringel F, Meyer B, Krieg SM (2017) Language pathway tracking: comparing nTMS-based DTI fiber tracking with a cubic ROIs-based protocol. J Neurosurg 126:1006–1014. https://doi.org/10.3171/2016.2.JNS152382
Tunc B, Ingalhalikar M, Parker D, Lecoeur J, Singh N, Wolf RL, Macyszyn L, Brem S, Verma R (2016) Individualized map of white matter pathways: connectivity-based paradigm for neurosurgical planning. Neurosurgery 79:568–577. https://doi.org/10.1227/NEU.0000000000001183
Zemmoura I, Fournier E, El-Hage W, Jolly V, Destrieux C, Velut S (2016) Hypnosis for awake surgery of low-grade gliomas: description of the method and psychological assessment. Neurosurgery 78:53–61. https://doi.org/10.1227/NEU.0000000000000993
Hervey-Jumper SL, Li J, Lau D, Molinaro AM, Perry DW, Meng L, Berger MS (2015) Awake craniotomy to maximize glioma resection: methods and technical nuances over a 27-year period. J Neurosurg 123:325–339. https://doi.org/10.3171/2014.10.JNS141520
Carrabba G, Fava E, Giussani C, Acerbi F, Portaluri F, Songa V, Stocchetti N, Branca V, Gaini SM, Bello L (2007) Cortical and subcortical motor mapping in rolandic and perirolandic glioma surgery: impact on postoperative morbidity and extent of resection. J Neurosurg Sci 51:45–51
Khan SA, Nathani KR, Ujjan BU, Barakzai MD, Enam SA, Shafiq F (2016) Awake craniotomy for brain tumours in Pakistan: An initial case series from a developing country. J Pak Med Assoc 66(Suppl 3):S68–S71
Wong JM, Panchmatia JR, Ziewacz JE, Bader AM, Dunn IF, Laws ER, Gawande AA (2012) Patterns in neurosurgical adverse events: intracranial neoplasm surgery. Neurosurg Focus 33:E16. https://doi.org/10.3171/2012.7.FOCUS12183
Magill ST, Han SJ, Li J, Berger MS (2017) Resection of primary motor cortex tumors: feasibility and surgical outcomes. J Neurosurg. https://doi.org/10.3171/2017.5.JNS163045
ReFaey K, Tripathi S, Bhargav AG, Grewal SS, Middlebrooks EH, Sabsevitz DS, Jentoft M, Brunner P, Wu A, Tatum WO, Ritaccio A, Chaichana KL, Quinones-Hinojosa A (2020) Potential differences between monolingual and bilingual patients in approach and outcome after awake brain surgery. J Neurooncol 148:587–598. https://doi.org/10.1007/s11060-020-03554-0
Jacquin-Courtois S, Bays PM, Salemme R, Leff AP, Husain M (2013) Rapid compensation of visual search strategy in patients with chronic visual field defects. Cortex 49:994–1000. https://doi.org/10.1016/j.cortex.2012.03.025
Herbet G, Maheu M, Costi E, Lafargue G, Duffau H (2016) Mapping neuroplastic potential in brain-damaged patients. Brain 139:829–844. https://doi.org/10.1093/brain/awv394
van Geemen K, Herbet G, Moritz-Gasser S, Duffau H (2014) Limited plastic potential of the left ventral premotor cortex in speech articulation: evidence from intraoperative awake mapping in glioma patients. Hum Brain Mapp 35:1587–1596. https://doi.org/10.1002/hbm.22275
Plaza M, Gatignol P, Leroy M, Duffau H (2009) Speaking without Broca’s area after tumor resection. Neurocase 15:294–310. https://doi.org/10.1080/13554790902729473
Duffau H, Capelle L, Sichez N, Denvil D, Lopes M, Sichez JP, Bitar A, Fohanno D (2002) Intraoperative mapping of the subcortical language pathways using direct stimulations. An anatomo-functional study. Brain 125:199–214. https://doi.org/10.1093/brain/awf016
Henry RG, Berman JI, Nagarajan SS, Mukherjee P, Berger MS (2004) Subcortical pathways serving cortical language sites: initial experience with diffusion tensor imaging fiber tracking combined with intraoperative language mapping. Neuroimage 21:616–622. https://doi.org/10.1016/j.neuroimage.2003.09.047
Sarubbo S, De Benedictis A, Merler S, Mandonnet E, Barbareschi M, Dallabona M, Chioffi F, Duffau H (2016) Structural and functional integration between dorsal and ventral language streams as revealed by blunt dissection and direct electrical stimulation. Hum Brain Mapp 37:3858–3872. https://doi.org/10.1002/hbm.23281
Chang EF, Raygor KP, Berger MS (2015) Contemporary model of language organization: an overview for neurosurgeons. J Neurosurg 122:250–261. https://doi.org/10.3171/2014.10.JNS132647
Gogos AJ, Young JS, Morshed RA, Avalos LN, Noss RS, Villanueva-Meyer JE, Hervey-Jumper SL, Berger MS (2020) Triple motor mapping: transcranial, bipolar, and monopolar mapping for supratentorial glioma resection adjacent to motor pathways. J Neurosurg. https://doi.org/10.3171/2020.3.JNS193434
Bello L, Gallucci M, Fava M, Carrabba G, Giussani C, Acerbi F, Baratta P, Songa V, Conte V, Branca V, Stocchetti N, Papagno C, Gaini SM (2007) Intraoperative subcortical language tract mapping guides surgical removal of gliomas involving speech areas. Neurosurgery 60:67–80. https://doi.org/10.1227/01.NEU.0000249206.58601.DE (discussion 80-62)
Magill ST, Han SJ, Li J, Berger MS (2018) Resection of primary motor cortex tumors: feasibility and surgical outcomes. J Neurosurg 129:961–972. https://doi.org/10.3171/2017.5.JNS163045
Beiko J, Suki D, Hess KR, Fox BD, Cheung V, Cabral M, Shonka N, Gilbert MR, Sawaya R, Prabhu SS, Weinberg J, Lang FF, Aldape KD, Sulman EP, Rao G, McCutcheon IE, Cahill DP (2014) IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro Oncol 16:81–91. https://doi.org/10.1093/neuonc/not159
Navarria P, Pessina F, Clerici E, Rossini Z, Franceschini D, D’Agostino G, Franzese C, Comito T, Loi M, Simonelli M, Lorenzi E, Persico P, Politi LS, Grimaldi M, Bello L, Santoro A, Fornari M, Servadei F, Scorsetti M (2020) Is IDH status the only factor predicting prognosis in newly diagnosed anaplastic glioma patients? Outcome evaluation and prognostic factor analysis in a single-institution large series. J Neurosurg. https://doi.org/10.3171/2020.5.JNS201116
Delev D, Heiland DH, Franco P, Reinacher P, Mader I, Staszewski O, Lassmann S, Grau S, Schnell O (2019) Surgical management of lower-grade glioma in the spotlight of the 2016 WHO classification system. J Neurooncol 141:223–233. https://doi.org/10.1007/s11060-018-03030-w
Kawaguchi T, Sonoda Y, Shibahara I, Saito R, Kanamori M, Kumabe T, Tominaga T (2016) Impact of gross total resection in patients with WHO grade III glioma harboring the IDH 1/2 mutation without the 1p/19q co-deletion. J Neurooncol 129:505–514. https://doi.org/10.1007/s11060-016-2201-2
Hameed NUF, Qiu T, Zhuang D, Lu J, Yu Z, Wu S, Wu B, Zhu F, Song Y, Chen H, Wu J (2018) Transcortical insular glioma resection: clinical outcome and predictors. J Neurosurg 131:706–716. https://doi.org/10.3171/2018.4.JNS18424
Hervey-Jumper SL, Berger MS (2019) Insular glioma surgery: an evolution of thought and practice. J Neurosurg 130:9–16. https://doi.org/10.3171/2018.10.JNS181519
Gil-Robles S, Duffau H (2010) Surgical management of World Health Organization Grade II gliomas in eloquent areas: the necessity of preserving a margin around functional structures. Neurosurg Focus 28:E8. https://doi.org/10.3171/2009.12.FOCUS09236
Duffau H (2012) The challenge to remove diffuse low-grade gliomas while preserving brain functions. Acta Neurochir (Wien) 154:569–574. https://doi.org/10.1007/s00701-012-1275-7
Acknowledgements
We would like to thank Dr. Lanxi Meng for imaging data acquisition for this study.
Funding
This study was supported by funds from Public Welfare Development and Reform Pilot Project of Beijing Medical Research Institute (PXM2019_026280_000008), Beijing Municipal Natural Science Foundation (No. 7202021), National Natural Science Foundation of China (No. 82001777), and Brain Tumor Precision Diagnosis and Treatment and Translational Medicine Innovation Unit, Chinese Academy of Medical Sciences (2019-I2M-5-021).
Author information
Authors and Affiliations
Contributions
Study concept and design: SF, YL, and LL. Data acquisition and analysis: SF, YL, and LL. Statistical analyses/verified the analytical method: SF, YL, and YW. Writing the first draft: SF, XF, and YW. Supervision study: XF, YW, and TJ. Read and approved final version: All authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
This study was approved by the IRB of Beijing Tiantan Hospital.
Informed consent
All participants provided informed written consent before data acquisition.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article has been revised: The corresponding authorship has been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fang, S., Liang, Y., Li, L. et al. Tumor location-based classification of surgery-related language impairments in patients with glioma. J Neurooncol 155, 143–152 (2021). https://doi.org/10.1007/s11060-021-03858-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03858-9