Abstract
Purpose
The aim of this study was to identify racial/ethnic disparities with regard to survival among patients with ependymoma.
Methods
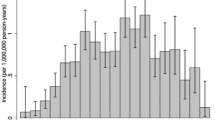
Data from the Surveillance, Epidemiology and End Results (SEER) registry between the years of 1973–2015 which included 4821 patients diagnosed with ependymoma were analyzed. Multivariable cox proportional hazard ratios were performed to examine overall survival across racial/ethnic groups of patients with ependymoma, mortality risks across specified age groups, and mortality during specified time intervals, all with corresponding 95% confidence intervals.
Results
Non-Hispanic black patients (n = 421) have higher risk of overall mortality when compared to non-Hispanic white patients (n = 3255) with ependymoma (HR 1.48, CI 1.17–1.87). Risk of mortality was highest when comparing non-Hispanic black children under the age of 3 to non-Hispanic white children of the same age group (HR 3.05, CI 1.55–5.99). Mortality risk has increased among pediatric non-Hispanic black patients compared to pediatric non-Hispanic white patients between the years of 2006–2015, from previous rates between the years 1973–2005 (HR 1.95, CI 1.15–3.33 and HR 2.35, CI 1.24–4.44). Hispanic patients under 3 years had an increased risk of mortality compared to non-Hispanic white patients of this age group (HR 2.49, CI 1.37–4.53). Asian/Pacific Islander patients (n = 282) had no significant difference in outcomes when compared to non-Hispanic white patients.
Conclusions
Our findings showed higher risk of mortality among non-Hispanic black patients compared to non-Hispanic white patients with ependymoma, with highest risk among pediatric patients. These results demonstrate significant need for research in survival outcomes for this disease.

Similar content being viewed by others
References
SEER Cancer Stat Facts. Brain and other nervous system cancer. National Cancer Institute. Bethesda. https://seer.cancer.gov/statfacts/html/brain.html
Villano JL, Parker CK, Dolecek TA (2013) Descriptive epidemiology of ependymal tumours in the United States. Br J Cancer 108:2367–2371
Khalid SI, Kelly R, Adogwa O et al (2018) Pediatric spinal ependymomas: an epidemiologic study. World Neurosurg 115:E119–E128
Ryu SM, Lee SH, Kim ES, Eoh W (2019) Predicting survival of patients with spinal ependymoma using machine learning algorithms with the SEER database. World Neurosurg 124:e331–e339
McGuire CS, Sainani KL, Fisher PG (2009) Both location and age predict survival in ependymomas: a SEER study. Pediatr Blood Cancer 52(1):65–69
Bates JE, Choi G, Milano MT (2016) Myxopapillary ependymoma: a SEER analysis of epidemiology and outcomes. J Neurooncol 129(2):251–258
Goldwein JW, Leahy JM, Packer RJ, et al (1990) Intracranial ependymomas in children. Int J Radiat Oncol Biol Phys 19(6):1497–1502
Lucchesi KM, Grant R, Kahle KT, Marks AM, DiLuna ML (2016) Primary spinal myxopapillary ependymoma in the pediatric population: a study from the Surveillance, Epidemiology, and End Results (SEER) database. J Neurooncol 130(1):133–140
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence—SEER 18 Regs Research Data, Nov 2017 Sub (1995–2015) <Katrina/Rita Population Adjustment>—Linked To County Attributes—Total U.S., 1969–2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2018, based on the November 2017 submission
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL (2018) Racial and ethnic disparities in cancer survival: the contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J Clin Oncol 36(1):25–33
Ward E, Jemal A, Cokkinides V et al (2008) Cancer disparities by race/ethnicity and socioeconomic status. Cancer 54(2):78–93
Kehm RD, Spector LG, Poynter JN, Vock DM, Altekruse SF (2018) Does socioeconomic status account for racial and ethnic disparities in childhood cancer survival? Cancer 124(20): 4090–4097
Jacobs AJ, Lindholm EB, Levy CF, Fish JD, Glick RD (2017) Racial and ethnic disparities in treatment and survival of pediatric sarcoma. J Surg Res 219:43–49
Friedrich P, Itriago E, Rodriguez-Galindo C, Ribeiro K (2017) Racial and ethnic disparities in the incidence of pediatric extracranial embryonal tumors. JNCI 109(10):djx050
Henderson TO, Bhatia S, Pinto N et al (2011) Racial and ethnic disparities in risk and survival in children with neuroblastoma: a Children's Oncology Group study. J Clin Oncol 29(1):76–82
Khanna V, Achey RL, Ostrom QT et al (2017) Incidence and survival trends for medulloblastomas in the United States from 2001 to 2013. J Neurooncol. 135(3):433–441
Pajtler KW, Mack SC, Ramaswamy V et al (2017) The current consensus on the clinical management of intracranial ependymoma and its distinct molecular variants. Acta Neuropathol 133(1):5–12
Hübner JM, Kool M, Pfister SM, Pajtler KW (2017) Epidemiology, molecular classification and WHO grading of ependymoma. J Neurosurg Sci 62(1):46–50
Gramatzki D, Witt H, Hentschel B et al (2017) Clinical and molecular subgroups of ependymoma in adulthood: an analysis of the German Glioma Network. J Clin Oncol 35(15):2038–2038
Nuno M, Yu JJ, Varshneya K, Alexander J, Mukherjee D, Black KL, Patil CG (2016) Treatment and survival of supratentorial and posterior fossa ependymomas in adults. J Clin Neurosci 28:24–30
Yeboa DN, Liao K, Guadagnolo BA, et al. National patterns of care in the management of World Health Organization Grade II and III Spinal Ependymomas.
Reni M, Gatta G, Mazza E, Vecht C (2007) Ependymoma. Crit Rev Oncol/Hematol 63(1):81–89
Snider CA, Yang K, Mack SC, Suh JH, Chao ST, Merchant TE, Murphy ES (2018) Impact of radiation therapy and extent of resection for ependymoma in young children: a population-based study. Pediatr Blood Cancer 65:e26880
Fukuoka K, Kanemura Y, Shofuda T, Fukushima S, Yamashita S, Narushima D et al (2018) Significance of molecular classification of ependymomas: C11orf95-RELA fusion negative supratentorial ependymomas are a heterogeneous group of tumors. Acta Neuropathol Commun 6:134
Lillard JC, Venable GT, Khan NR, Tatevossian RG, Dalton J, Vaughn BN, Klimo P (2018) Pediatric supratentorial ependymoma: surgical, clinical, and molecular analysis. Neurosurgery. https://doi.org/10.1093/neuros/nyy239/5039612
Acknowledgements
Data for this study were provided to the researchers from the Surveillance, Epidemiology, and End Results (SEER) Program.
Author information
Authors and Affiliations
Contributions
This research paper was written by Ashley Stenzel and Kirsten Moysich, with substantial input from Robert Fenstermaker and Laura Wiltsie.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research did not require an ethical board approval because it utilized data from the de-identified SEER database. As such, it does not contain animals or studies with humans performed by the authors.
Informed consent
Informed consent was not needed for individual participants included in the study, as the authors did not work with human subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stenzel, A.E., Fenstermaker, R.A., Wiltsie, L.M. et al. Disparities among racial/ethnic groups of patients diagnosed with ependymoma: analyses from the Surveillance, Epidemiology and End Results (SEER) registry. J Neurooncol 144, 43–51 (2019). https://doi.org/10.1007/s11060-019-03214-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03214-y