Abstract
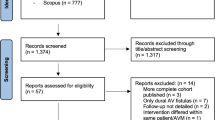
Preclinical evidence suggests angiotensin blockade therapy (ABT) decreases late radiation toxicities. This study aims to investigate the association between ABT and symptomatic radiation necrosis (SRN) following stereotactic radiosurgery (SRS). Resected brain metastases (rBM) and arteriovenous malformation (AVM) patients treated with SRS from 2002 to 2015 were identified. Patients in the ABT cohort were on therapy during SRS and at 1-month follow up. Kaplan Meier method and cumulative incidence model were used to analyze overall survival (OS) and intracranial outcomes. 228 consecutive patients were treated with SRS: 111 with rBM and 117 with AVM. Overall, 51 (22.4%) patients were in the ABT group: 32 (28.8%) in the rBM and 19 (16.2%) in AVM cohorts. Baseline characteristics were similar, except for higher Graded Prognostic Analysis (3–4) in the rBM (ABT: 25.0% vs. non-ABT: 49.0%, p = 0.033) and median age in the AVM (ABT: 51.4 vs. non-ABT: 35.4, p < 0.001) cohorts. In both populations, OS and intracranial efficacy (rBM—local control; AVM—obliteration rates) were statistically similar between the cohorts. ABT was associated with lower 1-year SRN rates in both populations: rBM, 3.1 versus 25.3% (p = 0.003); AVM, 6.7 vs. 14.6% (p = 0.063). On multivariate analysis, ABT was a significant predictive factor for rBM (HR: 0.17; 95% CI 0.03–0.88, p = 0.035), but did not reach statistical significance for AVM (HR: 0.36; 95% CI 0.09–1.52, p = 0.165). ABT use appears to be associated with a reduced risk of SRN following SRS, without detriment to OS or intracranial efficacy. A prospective trial to validate these findings is warranted.



Similar content being viewed by others
References
Patel KR, Burri SH, Asher AL et al (2016) Comparing preoperative with postoperative stereotactic radiosurgery for resectable brain metastases: a multi-institutional analysis. Neurosurgery 79:279–285
Patel KR, Lawson DH, Kudchadkar RR et al (2015) Two heads better than one? Ipilimumab immunotherapy and radiation therapy for melanoma brain metastases. Neuro Oncol 17:1312–1321
Chao ST, Ahluwalia MS, Barnett GH et al (2013) Challenges with the diagnosis and treatment of cerebral radiation necrosis. Int J Radiat Oncol Biol Phys 87:449–457
Ebner D, Rava P, Gorovets D et al (2015) Stereotactic radiosurgery for large brain metastases. J Clin Neurosci 22:1650–1654
Prabhu R, Shu HK, Hadjipanayis C et al (2012) Current dosing paradigm for stereotactic radiosurgery alone after surgical resection of brain metastases needs to be optimized for improved local control. Int J Radiat Oncol Biol Phys 83:e61-6
Stockham AL, Ahluwalia M, Reddy CA et al (2013) Results of a questionnaire regarding practice patterns for the diagnosis and treatment of intracranial radiation necrosis after SRS. J Neurooncol 115:469–475
Re RN (2004) Mechanisms of disease: local renin-angiotensin-aldosterone systems and the pathogenesis and treatment of cardiovascular disease. Nat Clin Pract Cardiovasc Med 1:42–47
Escobar E, Rodriguez-Reyna TS, Arrieta O et al (2004) Angiotensin II, cell proliferation and angiogenesis regulator: biologic and therapeutic implications in cancer. Curr Vasc Pharmacol 2:385–399
Zhuang S, Li J, Wang X et al (2016) Renin-angiotensin system-targeting antihypertensive drugs and risk of vascular cognitive impairment: A meta-analysis. Neurosci Lett 615:1–8
Nordal RA, Nagy A, Pintilie M et al (2004) Hypoxia and hypoxia-inducible factor-1 target genes in central nervous system radiation injury: a role for vascular endothelial growth factor. Clin Cancer Res 10:3342–3353
Vujaskovic Z, Marks LB, Anscher MS (2000) The physical parameters and molecular events associated with radiation-induced lung toxicity. Semin Radiat Oncol 10:296–307
Starke RM, Yen CP, Ding D et al (2013) A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: analysis of 1012 treated patients. J Neurosurg 119:981–987
Patel KR, Prabhu RS, Kandula S et al (2014) Intracranial control and radiographic changes with adjuvant radiation therapy for resected brain metastases: whole brain radiotherapy versus stereotactic radiosurgery alone. J Neurooncol 120:657–663
Eaton BR, LaRiviere MJ, Kim S et al (2015) Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol 123:103–111
Patel KR, Chowdhary M, Switchenko JM et al (2016) BRAF inhibitor and stereotactic radiosurgery is associated with an increased risk of radiation necrosis. Melanoma Res 26:387–394
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Amer Statistical Assoc 94:496–509
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29:134–141
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280:1485–1489
Brennan C, Yang TJ, Hilden P et al (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88:130–136
Brown PD, Ballman KV, Cerhan J et al (2016) N107C/CEC.3: a phase iii trial of post-operative stereotactic radiosurgery (SRS) compared with whole brain radiotherapy (WBRT) for resected metastatic brain disease. Int J Radiat Oncol Biol Phys 96:937
Chowdhary M, Patel KR, Danish HH et al (2016) BRAF inhibitors and radiotherapy for melanoma brain metastases: potential advantages and disadvantages of combination therapy. Onco Targets Ther 9:7149–7159
Al-Shahi Salman R, White PM, Counsell CE et al (2014) Outcome after conservative management or intervention for unruptured brain arteriovenous malformations. JAMA 311:1661–1669
Mohr JP, Parides MK, Stapf C et al (2014) Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 383:614–621
Small W Jr, James JL, Moore TD et al (2016) Utility of the ACE Inhibitor captopril in mitigating radiation-associated pulmonary toxicity in lung cancer: results from NRG Oncology RTOG 0123. Am J Clin Oncol. https://doi.org/10.1097/COC.0000000000000289
Kharofa J, Cohen EP, Tomic R et al (2012) Decreased risk of radiation pneumonitis with incidental concurrent use of angiotensin-converting enzyme inhibitors and thoracic radiation therapy. Int J Radiat Oncol Biol Phys 84:238–243
Wang H, Liao Z, Zhuang Y et al (2013) Do angiotensin-converting enzyme inhibitors reduce the risk of symptomatic radiation pneumonitis in patients with non-small cell lung cancer after definitive radiation therapy? Analysis of a single-institution database. Int J Radiat Oncol Biol Phys 87:1071–1077
Alite F, Balasubramanian N, Adams W et al (2016) Decreased risk of radiation pneumonitis with coincident concurrent use of angiotensin-converting enzyme inhibitors in patients receiving lung stereotactic body radiation therapy. Am J Clin Oncol. https://doi.org/10.1097/COC.0000000000000324
Alashkham A, Paterson C, Rauchhaus P et al (2016) Can angiotensin-converting enzyme inhibitors reduce the incidence, severity, and duration of radiation proctitis? Int J Radiat Oncol Biol Phys 94:93–101
Harder EM, Park HS, Nath SK et al (2015) Angiotensin-converting enzyme inhibitors decrease the risk of radiation pneumonitis after stereotactic body radiation therapy. Pract Radiat Oncol 5:e643-e649
Leask A (2015) Getting to the heart of the matter: new insights into cardiac fibrosis. Circ Res 116:1269–1276
Okwan-Duodu D, Landry J, Shen XZ et al (2013) Angiotensin-converting enzyme and the tumor microenvironment: mechanisms beyond angiogenesis. Am J Physiol Regul Integr Comp Physiol 305:R205-15
Medhora M, Gao F, Jacobs ER et al (2012) Radiation damage to the lung: mitigation by angiotensin-converting enzyme (ACE) inhibitors. Respirology 17:66–71
Acknowledgements
Research reported in this publication was supported in part by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and NIH/NCI under award number P30CA138292. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Chowdhary, M., Okwan-Duodu, D., Switchenko, J.M. et al. Angiotensin receptor blockade: a novel approach for symptomatic radiation necrosis after stereotactic radiosurgery. J Neurooncol 136, 289–298 (2018). https://doi.org/10.1007/s11060-017-2652-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2652-0