Abstract
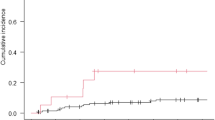
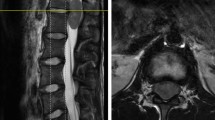
Primary spinal cord tumors constitute 2–4% of all primary central nervous system malignancies in adults of which less than 5% are glioblastoma. A retrospective evaluation to determine toxicity and response to bevacizumab in patients with recurrent spinal cord glioblastoma. Six patients (4 males; 2 females: median age 34 years) with recurrent spinal cord glioblastoma were treated with bevacizumab (10 mg/kg given once every 2 weeks wherein 2 treatments constituted a cycle of therapy). All patients had failed surgery and temozolomide-based chemoradiotherapy and post-radiotherapy temozolomide. Blood counts, chemistry panel, urine protein to creatinine ratio and neurologic examination were obtained bi-weekly. Contrast-enhanced spine MRI was performed after one cycle of therapy and thereafter following every two cycles of bevacizumab. Treatment-related complications included fatigue in six patients, constipation in 4, hypertension in 2, venous thrombosis in 2, and infection without neutropenia in 2. There were three grade 3 toxicities (1 each fatigue, leukopenia and venous thrombosis). There were no treatment-related deaths. After one cycle of bevacizumab, one patient (17%) demonstrated progressive disease, 2 (34%) partial responses and three (51%) stable disease. Overall median response or stable disease duration (disease free progression) was 7 months (range 3–11 months). Overall median survival was 9 months (range of 5–13 months). Bevacizumab is well tolerated, has tolerable toxicity and apparent activity in this small cohort of adults with recurrent spinal cord glioblastoma.

Similar content being viewed by others
References
Campello C LFA, Parker F et al (2009) Neuroepithelial intramedullary spinal cord tumors in adults: study of 70 cases. Neurology 72(11, Suppl 3):A33
Raco A, Esposito V, Lenzi J et al (2005) Long-term follow-up of intramedullary spinal cord tumors: a series of 202 cases. Neurosurgery 56(5):972–981 discussion 972–981
Helseth A, Mork SJ (1989) Primary intraspinal neoplasms in Norway, 1955 to 1986. A population-based survey of 467 patients. J Neurosurg 71(6):842–845
Rodrigues GB, Waldron JN, Wong CS, Laperriere NJ (2000) A retrospective analysis of 52 cases of spinal cord glioma managed with radiation therapy. Int J Radiat Oncol Biol Phys 48(3):837–842
Minehan KJ, Brown PD, Scheithauer BW, Krauss WE, Wright MP (2009) Prognosis and treatment of spinal cord astrocytoma. Int J Radiat Oncol Biol Phys 73(3):727–733
Kim MS, Chung CK, Choe G, Kim IH, Kim HJ (2001) Intramedullary spinal cord astrocytoma in adults: postoperative outcome. J Neurooncol 52(1):85–94
Innocenzi G, Salvati M, Cervoni L, Delfini R, Cantore G (1997) Prognostic factors in intramedullary astrocytomas. Clin Neurol Neurosurg 99(1):1–5
Isaacson SR (2000) Radiation therapy and the management of intramedullary spinal cord tumors. J Neurooncol 47(3):231–238
MacDonald DR, Cascino TL, Schold SC et al (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:1277–1280
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Eng J Med 352:987–996
Chamberlain MC (2008) Temozolomide for recurrent low-grade spinal cord gliomas in adults. Cancer 113(5):1019–1024
Kaley T M-CI, Abrey L (2009) Temozolomide for spinal cord high-grade gliomas. Neurology 72(11, Suppl 3):A33
Allen JC, Aviner S, Yates AJ et al (1998) Treatment of high-grade spinal cord astrocytoma of childhood with “8-in-1” chemotherapy, radiotherapy: a pilot study of CCG-945. Children’s Cancer Group. J Neurosurg 88(2):215–220
Kreisl TN, Kim L, Moore K et al (2009) Phase II trial of single agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27:1–10
Friedman HS, Prados MD, Wen PY et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27:4733–4740
Wen P, Macdonald DR, Reardon DA et al (2010) Proposal for an updated response assessment criteria for high-grade gliomas: radiology assessment for neuro-oncology: working group. J Clin Oncol 28:1963–1972
Wick W, Weller M, van den bent M, Stupp R (2010) Bevacizumab and recurrent glioma: a European perspective. J Clin Oncol 28:e188–e189
Chamberlain MC, Glantz MJ, Chalmers L, Sloan A (2007) Early necrosis following Temodar and radiotherapy in patients with glioblastoma. J Neurooncol 82(1):81–83
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chamberlain, M.C., Johnston, S.K. Recurrent spinal cord glioblastoma: salvage therapy with bevacizumab. J Neurooncol 102, 427–432 (2011). https://doi.org/10.1007/s11060-010-0330-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0330-6