Abstract
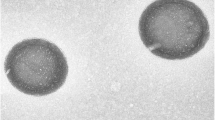
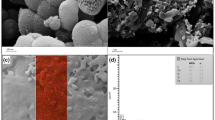
In recent decades, extensive research has been conducted on nano drug delivery systems for treating inflammation. Despite this, the lack of specificity in many carriers and materials has hindered their effectiveness in enhancing treatment efficiency. To address this challenge, among numerous candidate biomaterials, stimuli-responsive biopolymers have received significant interest for precisely delivering their payload to inflamed tissues. Herein, to overcome this deficiency, pH-responsive magnetic nanocarriers were fabricated. A cationic dextran was synthesized based on the oxidation of glucose ring and conjugation of spermine. Drug-loaded magnetic dextran-spermine nanoparticles (DS-NPs) were prepared by in situ drug loading via ionic gelation. Fabricated nanoparticles have smaller size (60–100 nm), with relatively narrow size distribution (pdI = 0.175–0.251), and a positive surface charge (+ 17.1 to + 29.0 mV). The in vitro release study in simulated normal and inflamed organ environments confirmed the pH sensitivity of the drug release with a slight burst effect in normal conditions and accelerated release in acidic pH (final release < 70% and < 50% of the total encapsulated drug for pH 7.4 and pH 5.0, respectively). Antibacterial study on Staphylococcus aureus showed no changes in the bactericidal activity of encapsulated vancomycin. Cytotoxicity studies on HUVEC cells confirmed that drug-free nanoparticles exhibited no toxicity, even up to 1 mg/mL. Furthermore, the cytotoxicity of encapsulated vancomycin against HUVEC cells was lower than that of free vancomycin in all incubation times (24 h, 48 h, 72 h).







Similar content being viewed by others
References
Zhu X et al (2014) Nanomedicine in the management of microbial infection–overview and perspectives. Nano Today 9(4):478–498
Craparo EF et al (2011) Nanoparticulate systems for drug delivery and targeting to the central nervous system. CNS neurosci Ther 17(6):670–677
Ghaeini-Hesaroeiye S, Boddohi S, Vasheghani-Farahani E (2020) Dual responsive chondroitin sulfate based nanogel for antimicrobial peptide delivery. Int J Bio Macromol 143:297–304
Nasrollahzadeh M et al (2022) Drug in adhesive transdermal patch containing antibiotic-loaded solid lipid nanoparticles. J Biosci Bioeng 134(5):471–476
Shao Q et al (2022) Protein corona mediated liposomal drug delivery for bacterial infection management. Asian J Pharm Sci 17(6):855–866
Xu H et al (2015) Amphiphilic poly (amino acid) based micelles applied to drug delivery: the in vitro and in vivo challenges and the corresponding potential strategies. J Control Release 199:84–97
Shaki H et al (2018) Self-assembled amphiphilic-dextran nanomicelles for delivery of rapamycin. J Drug Deliv Sci Technol 44:333–341
Jafarzadeh-Holagh S et al (2018) Self-assembled and pH-sensitive mixed micelles as an intracellular doxorubicin delivery system. J Colloid Inter Sci 523:179–190
Wang Y, Wang PG (2013) Polysaccharide-based systems in drug and gene delivery. Adv Drug Deliv Rev 65(9):1121–1122
Prasher P et al (2022) Advances and applications of dextran-based nanomaterials targeting inflammatory respiratory diseases. J Drug Deliv Sci Tech 74:103598
Yang J et al (2012) The biocompatibility of fatty acid modified dextran-agmatine bioconjugate gene delivery vector. Biomater 33(2):604–613
Yao X et al (2014) Intercellular pH-responsive histidine modified dextran-g-cholesterol micelle for anticancer drug delivery. Colloids Surf B: Biointerfaces 121:36–43
Tiryaki E et al (2020) Novel organic/inorganic hybrid nanoparticles as enzyme-triggered drug delivery systems: dextran and dextran aldehyde coated silica aerogels. J Drug Deliv Sci Tech 56:101517
Abeylath SC, Amiji MM (2011) ‘Click’synthesis of dextran macrostructures for combinatorial-designed self-assembled nanoparticles encapsulating diverse anticancer therapeutics. Bioorg Med Chem 19(21):6167–6173
Thomas JJ, Rekha M, Sharma CP (2010) Dextran–glycidyltrimethylammonium chloride conjugate/DNA nanoplex: a potential non-viral and haemocompatible gene delivery system. Int J Pharm 389(1–2):195–206
Shaki H et al (2021) A self assembled dextran-stearic acid-spermine nanocarrier for delivery of rapamycin as a hydrophobic drug. J Drug Deliv Sci Tech 66:102768
Tarvirdipour S et al (2016) Functionalized magnetic dextran-spermine nanocarriers for targeted delivery of doxorubicin to breast cancer cells. Int J Pharm 501(1–2):331–341
Ghadiri M et al (2017) Transferrin-conjugated magnetic dextran-spermine nanoparticles for targeted drug transport across blood-brain barrier. J Biomed Mater Res Part A 105(10):2851–2864
Du Y-Z et al (2010) Synthesis and antitumor activity of stearate-g-dextran micelles for intracellular doxorubicin delivery. ACS Nano 4(11):6894–6902
Mohammad-Taheri M, Vasheghani-Farahani E, Hosseinkhani H, Shojaosadati SA, Soleimani M (2012) Fabrication and characterization of a new MRI contrast agent based on a magnetic dextran–spermine nanoparticle system. Iranian Polym J 21(4):239–251
Ghadiri M et al (2017) Transferrin-conjugated magnetic dextran-spermine nanoparticles for targeted drug transport across blood-brain barrier. J Biomed Mater Res A 105(10):2851–2864
Jafarzadeh-Holagh S et al (2018) Self-assembled and pH-sensitive mixed micelles as an intracellular doxorubicin delivery system. J Colloid Interface Sci 523:179–190
Lê MQ et al (2019) Protein delivery by porous cationic maltodextrin-based nanoparticles into nasal mucosal cells: comparison with cationic or anionic nanoparticles. Int J Pharm: X 1:100001
Wu X et al (2018) Inhibition of intrinsic coagulation improves safety and tumor-targeted drug delivery of cationic solid lipid nanoparticles. Biomaterials 156:77–87
Ghadiri M et al (2017) In-vitro assessment of magnetic dextran-spermine nanoparticles for capecitabine delivery to cancerous cells. Iranian J Pharm Res: IJPR 16(4):1320
Azzam T et al (2002) Cationic polysaccharides for gene delivery. Macromolecules 35(27):9947–9953
Zhao T et al (2015) Self-assembly and cytotoxicity study of PEG-modified ursolic acid liposomes. Mater Sci Eng C Mater Biol Appl 53:196–203
Siepmann J, Peppas NA (2012) Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv drug Deliv Rev 64:163–174
Ramakrishna S et al (2012) Design and evaluation of drug release kinetics of meloxicam sustained release matrix tablets. Int J Curr Pharm Res 4(1):90–99
Mohammad-Taheri M et al (2012) Fabrication and characterization of a new MRI contrast agent based on a magnetic dextran–spermine nanoparticle system. Iranian Polym J 21(4):239–251
Kataoka K, Harada A, Nagasaki Y (2001) Block copolymer micelles for drug delivery: design, characterization and biological significance. Adv Drug Deliv Rev 47(1):113–131
Gothwal A, Khan I, Gupta U (2016) Polymeric micelles: recent advancements in the delivery of anticancer drugs. Pharm Res 33(1):18–39
Raveendran R, Bhuvaneshwar GS, Sharma CP (2016) Hemocompatible curcumin–dextran micelles as pH sensitive pro-drugs for enhanced therapeutic efficacy in cancer cells. Carbohyd Polym 137:497–507
Kazemi-Ashtiyani M, Hajipour-Verdom B, Satari M, Abdolmaleki P, Hosseinkhani S, Shaki H (2022) Estimating the two graph dextran–stearic acid–spermine polymers based on iron oxide nanoparticles as carrier for gene delivery. Biopolymers 113(7):23491
Danaei M et al (2018) Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics 10(2):57
Masarudin MJ et al (2015) Factors determining the stability, size distribution, and cellular accumulation of small, monodisperse chitosan nanoparticles as candidate vectors for anticancer drug delivery: application to the passive encapsulation of [(14)C]-doxorubicin. Nanotechnol Sci Appl 8:67–80
Ternullo S et al (2018) Deformable liposomes for skin therapy with human epidermal growth factor: The effect of liposomal surface charge. Eur J Pharm Sci 125:163–171
Liu X, Zhou H, Yu W (2013) Effect of surface charge of amphiphlic chitosan nanocarriers on drug release behavior. J Control Release 172(1):e78
Soheyla Honary FZ (2013) Effect of zeta potential on the properties of nano-drug delivery systems - a review (part 1). Tropical J Pharm Res 12(2):255–264
Pardeshi SR et al (2023) Novel crosslinked nanoparticles of chitosan oligosaccharide and dextran sulfate for ocular administration of dorzolamide against glaucoma. J Drug Deliv Sci Tech 86:104719
Haddad N et al (2022) The blood-brain barrier and pharmacokinetic/pharmacodynamic optimization of antibiotics for the treatment of central nervous system infections in adults. Antibiotics (Basel) 11(12):1843. https://doi.org/10.3390/antibiotics11121843
Ghadiri M et al (2017) In-vitro assessment of magnetic dextran-spermine nanoparticles for capecitabine delivery to cancerous cells. Iran J Pharm Res 16(4):1320–1334
Rani NNIM et al (2022) Surface-engineered liposomes for dual-drug delivery targeting strategy against methicillin-resistant Staphylococcus aureus (MRSA). Asian J Pharm Sci 17(1):102–119
Avazzadeh R et al (2017) Synthesis and application of magnetite dextran-spermine nanoparticles in breast cancer hyperthermia. Prog Biomater 6:75–84
Xu J et al (2015) Preparation and evaluation of vancomycin-loaded N-trimethyl chitosan nanoparticles. Polymers 7(9):1850–1870
Mok H, Zhang M (2013) Superparamagnetic iron oxide nanoparticle-based delivery systems for biotherapeutics. Expert Opin Drug Deliv 10(1):73–87
Eliyahu H et al (2006) Relationships between chemical composition, physical properties and transfection efficiency of polysaccharide-spermine conjugates. Biomaterials 27(8):1646–1655
Siepmann J, Peppas NA (2001) Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv Drug Deliv Rev 48(2):139–157
Tavakol M, Vasheghani-Farahani E, Hashemi-Najafabadi S (2013) The effect of polymer and CaCl 2 concentrations on the sulfasalazine release from alginate-N O-carboxymethyl chitosan beads. Prog in Biomater 2:1–8
Vollmerhaus PJ, Breukink E, Heck AJ (2003) Getting closer to the real bacterial cell wall target: biomolecular interactions of water-soluble lipid II with glycopeptide antibiotics. Chemistry 9(7):1556–1565
Zazo H, Colino CI, Lanao JM (2016) Current applications of nanoparticles in infectious diseases. J Control Release 224:86–102
Baran A et al (2022) Investigation of antimicrobial and cytotoxic properties and specification of silver nanoparticles (AgNPs) derived from Cicer arietinum L. green leaf extract. Front Bioeng Biotech 10:1–11. https://doi.org/10.3389/fbioe.2022.855136
Baran A et al (2021) Ecofriendly synthesis of silver nanoparticles using ananas comosus fruit peels: anticancer and antimicrobial activities. Bioinorganic Chem App 2021:2058149
Kiem S, Schentag JJ (2006) Relationship of minimal inhibitory concentration and bactericidal activity to efficacy of antibiotics for treatment of ventilator-associated pneumonia. Semin Respir Crit Care Med 27(1):51–67
Mouton JW, Vinks AA (2005) Relationship Between minimum inhibitory concentration and stationary concentration revisited. Clin Pharmacokinetics 44(7):767–768
Kalhapure RS et al (2015) Nanoengineered drug delivery systems for enhancing antibiotic therapy. J Pharm Sci 104(3):872–905
Stebbins ND, Ouimet MA, Uhrich KE (2014) Antibiotic-containing polymers for localized, sustained drug delivery. Adv Drug Deliv Rev 78:77–87
Ferraro MJ (2001) Should we reevaluate antibiotic breakpoints? Clin Infect Dis 33(Suppl 3):S227–S229
Jorgensen JH (2004) Who defines resistance? The clinical and economic impact of antimicrobial susceptibility testing breakpoints. Semin Pediatr Infect Dis 15(2):105–108
Kumar, Vrinda S, Vinayan KP (2024) Comparative in vivo biodistribution and pharmacokinetic evaluation of phenytoin sodium loaded polymeric nanomicelles and marketed phenytoin sodium iv. J Nanoparticle Res 26(2):24
Shariare MH et al (2024) Phospholipid-based nano drug delivery system of curcumin using MSP1D1 protein and poloxamer 407: a comparative study for targeted drug delivery to the brain. J Nanoparticle Res 26(1):12
Author information
Authors and Affiliations
Contributions
N.A. conceived the study design, carried out the experiments, prepared, analyzed, and manipulated data, and prepared the manuscript draft. H.S. contributed to analyzing and manipulating data, editing figures, and preparation of the manuscript draft. S.J.H. contributed to the sample preparation and editing of images. F.G. contributed to the interpretation of drug release results and commented on the manuscript. E.V.F. supervised the research activity planning and execution, including mentorship external to the core team and the final editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abri, N., Vasheghani-Farahani, E., Shaki, H. et al. Magnetic dextran-spermine nanoparticles as pH-sensitive carriers for antibiotic delivery. J Nanopart Res 26, 73 (2024). https://doi.org/10.1007/s11051-024-05979-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-024-05979-4