Abstract
Rutin (Ru) is a flavonol glycoside, has significant scavenging characteristics against various reactive oxygen species, which exploits for widespread pharmacological activities such as anti-inflammatory and anti-allergic effects. This study aims to improve the bioavailability of iron oxide nanoparticles (IONPs) by coating them with Ru (Ru-IONPs). Considering this, IONPs and Ru-IONPs were prepared and characterized via various physical techniques. In addition, atomic absorption spectroscopy (AAS) has been used to assess the bio-distribution of the prepared formulation in vivo. Results revealed that the prepared IONPs and Ru-IONPs have a spherical shape with an average diameter of about 8 nm and 10 nm, respectively. Their surface potentials were found to be −19 ± 3.9 and −29.5 ± 5.4 mV, respectively. In vivo results revealed that single dose of IV administration of IONPs (16 mg/kg) elevated oxidative stress, indicated by the reduction of GSH in both heart and liver tissues, and increased their MDA contents. Also, IONPs administration resulted in hepatotoxicity characterized by a significant increase in ALT and AST levels in addition to cardiotoxicity characterized by a significant increase in CK-MB and LDH, in addition to the downregulation of heat shock protein 70 (HSP70) expression, while upregulation of TNF-α expression in both heart and liver tissues. Conversely, nearly all of these alterations were significantly ameliorated for animal groups administrated Ru-IONPs and the morphological injury’s counteraction in both heart and liver tissues. Therefore, we suggest that Ru could be used to alleviate the harmful effects and damages associated with IONPs administration due to its antioxidant, anti-inflammatory, and free radical scavenging properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to their physical, and chemical properties and the acceptable level of biocompatibility, iron oxide nanoparticles (IONPs) have a pivotal role in various medical applications such as magnetic resonance imaging, drug and gene delivery, cancer therapy, and catalysis [1, 2]. Among the many types of magnetic nanoparticles, IONPs are considered the most promising nano-formulation mainly because they are approved by the US Food and Drug Administration (FDA), and are relatively easily prepared. IONPs are approved by the FDA for various purposes such as contrast agents for imaging of lymph node metastasis and liver lesions in addition to iron efficiency anemia treatment [3]. For the recent pandemic emergency, researchers recommended IONPs for clinical trials of COVID-19 treatment after their molecular docking [4]. Despite this wide range of uses, there is insufficient information on the impact of IONPs on human and animal health [5]. Therefore, the analysis of the bioavailability of various formulations for IONPs is a pivotal area of research and a need of the hour.
A former study elucidated that IONPs toxicity of the organs of the mononuclear phagocytic system as the liver, spleen, central nervous system, lungs, and thyroid gland in addition to the heart [1]. Accumulation of high dose of ultrafine IONPs may cause oxidative stress, inflammation, cell lysis, and consequently cell death [6, 7]. It was reported that the toxicity of NPs depends on their physicochemical parameters, such as particle size and shape and surface modification [8], whereas, IONPs’ surface modification affects their in vivo bio-distribution and clearance time by affecting their plasma proteins’ binding [9]. Nanoparticles with negative charges are less likely to absorb plasma proteins, so they are more stable and can circulate longer in the blood. Moreover, it was reported that the neutral surfaces are the most biocompatible, but it is more susceptible to aggregation, while cationic nanoparticles surfaces may exhibit some platelet accumulations by attracting the negatively charged components of the cellular membranes as proteins and phospholipid head groups [10]. Surface coating of nanoparticles can therefore be a major strategy for limitation in toxicity associated with nano-formulation. Utilization of natural coating agents over the NPs will maintain their physicochemical stability [11]. In addition, capping of IONPs with a natural stabilizing coat is preferred for improvement of their biocompatibility, more specific targeting, and longer circulation lifetime by decreasing their clearance rate by the reticuloendothelial system [12].
It is believed that reactive oxygen species (ROS) is one of the underlying mechanisms of IONP-induced toxicity. Consequently, antioxidants are one of the key components for the efficient treatment of IONP-induced toxicity. Rutin (Ru) is a natural citrus flavonoid with a polyphenolic structure that can be used as an organic capping agent to modify the IONPs surface. Ru is found in tea, apples, buckwheat, and passionflowers and used for different medical purposes due to possessing multiple activities. It is non-toxic and exerts several biological and pharmacological activities including: antioxidant, cardio-protective, neuro-protective, anti-carcinogenic, cytoprotective, and has anti-diabetic effect [13]. The potent anti-viral activity of Ru against different pathogens of viral origin makes it to be used as a phytotherapy for COVID-19. Among various flavonoids that have been evaluated to oppose COVID-19, Ru had the highest binding affinity to the protease of severe acute respiratory syndrome of SARS-CoV-2, proposing it as the most favorable drug target to treat COVID-19 [14].
The current study aims to assess the effects of Ru coat on the bioavailability of iron oxide nanoparticles in rats. In addition, it investigates the effect of Ru coatings on the bio-distribution of IONPs within the critical organs of the biological system. To the best of the authors’ knowledge, this article is the first research investigating the protective effects of the antioxidant Ru coating against a single dose of IONPs-induced toxicities.
Materials and methods
Chemicals
Iron (II) chloride tetrahydrate (FeCl2·4H2O), iron (III) chloride hexahydrate (FeCl3·6H2O), ammonium hydroxide (NH4OH), nitric acid (HNO3), curcumin powder, ketamine/xylazine (KX) and phosphate-buffered saline (PBS) were purchased from (Sigma-Aldrich, USA). Dimethyl sulfoxide (DMSO) was purchased from Gibco (USA). Biochemical analysis kits for alanine aminotransferase (ALT), and aspartate aminotransferase (AST), albumin were purchased from Biolabo, SpectRum, and Biomed Diagnostic Inc.
Methods
Preparation of iron oxide nano-formulations
An aqueous solution of Fe (III) and Fe (II) salts with a molar ratio of (2:1) was dissolved in 40 ml of water and stirred for 15 min at 40 °C till the appearance of a clear brown color. To prepare Ru-IONPs, 100 μl of Ru solution (30 mg Ru dissolved in 1 ml DMSO) was added drop-wise. The mixture was heated and 5 ml of 28% ammonium hydroxide was added, till the mixture’s color turned black, while to prepare IONPs, 4.4 g of sodium citrate was added instead of Ru solution. The mixture was left to cool till a black precipitate was seen topped by a clear transparent supernatant. The black precipitates were washed twice to remove the remaining chemicals and the ammonium hydroxide. Centrifugation was used to collecting the prepared IONPs formulations [15].
Physicochemical characterization
IONPs and Ru-IONPs’ size and morphology were visualized by TEM (HR-TEM, JEM 2100; JEOL, Japan,) at an electron acceleration voltage of 200 kV. The surface potential of prepared nano-formulations was determined using the Zeta Potential/Particle Seizer (Zeta Potential/Particle Sizer Malvern PANalytical, Zetasizer Nano, NanoZs, UK). Dynamic light scattering (DLS) technique was used to measure the hydrodynamic size distribution and Polydispersity index (PDI) of nano-colloids. The mean hydrodynamic size and PDI of the prepared formulations were measured using the Zeta Sizer nano series (NanoZs, Malvern; UK). The measurements were repeated three times and the standard deviation (SD) was calculated using Origin 6.0 software.
Fourier transform infrared (FTIR) technique was used to investigate the nature of the interaction between RU and IONPs surfaces and to confirm the attachment of Ru to IONPs surfaces. The synthesized nano-formulations were ground with pure potassium bromide (KBr) and the mixtures of each sample were triturated into fine powders. The prepared samples were pressed using a mechanical press to produce translucent pellets and then analyzed using an FTIR spectrometer (Hitachi, Mod 4100, Japan). The recorded FTIR spectra were from 400 to 4000 cm−1 with a resolution of 4 cm−1.
Experimental design
Forty-two healthy adult female Sprague-Dawley albino rats weighing 200 ± 10 g were provided by National Organization for Drug Control and Research (NODCAR) breeding unit, in Giza, Egypt. Under controlled conditions (21 ± 1°C constant temperature, humidity 55%, 12 h light-dark cycle), rats were housed and administered a standard diet and water ad libitum. Water, food, and weight (gain or loss) were recorded weekly until the experiment ended.
Rats were divided into seven equal groups randomly (6 animals each) as follows:
Group | Treatment duration |
|---|---|
IONp, 1 h | Received a single IV injection dose of IONPs and sacrificed after 1 h. |
Ru-IONp, 1 h | Received a single IV injection dose of Ru-IONPs and sacrificed after 1 h. |
IONp, 1 day | Received a single IV injection dose of IONPs and sacrificed after 1 day. |
Ru-IONp, 1 day | Received a single IV injection dose of Ru-IONPs and sacrificed after 1 day. |
IONp, 1 week | Received a single IV injection dose of IONPs and sacrificed after 1 week. |
Ru-IONp, 1 week | Received a single IV injection dose of Ru-IONPs and sacrificed after 1 week. |
Blood was withdrawn then animals were sacrificed after different time intervals. Liver, heart, and kidney tissues were collected and kept at −20 °C for further analysis. Samples of the liver, and heart tissues were kept in formalin for histopathological examinations.
Atomic absorption spectroscopy (AAS)
Atomic absorption spectroscopy (AAS) was confirmed as a suitable method to assess the iron content at the biological tissues with a high level of precision [8, 16]. AAS was used to quantify the iron concentration throughout the liver, kidney, and heart tissues of the rats after receiving a single IV injection dose of 100 μl (16 mg/kg) of either Ru-IONPs or IONPs via the tail vein. At certain time intervals (1 h, 1 day, and 1 week) after injection, the animals were sacrificed and the mentioned organs (liver, kidney, and heart) were collected. These organs were dried, weighed and digested overnight with 2 ml of 70% nitric acid and 36% hydrochloric acid (with volume ratio 1:1 v/v) at 70 °C. After that, these solutions were diluted with deionized water to a final volume of 10 ml and filtered through a 0.2 μm polyethersulfone (PES) filter. The samples were then investigated via an atomic absorption spectrometer (Zeenit 700, Analytik Jena, Germany). The hollow-cathode lamp of the iron was adjusted depending on the equipment instructions. The flame background was adjusted via deuterium lamp [8].
Hepatic and cardiac parameters
Aspartate transaminase (AST) and alanine transaminase (ALT) were measured to evaluate liver function. The levels of lactate dehydrogenase (LDH) and creatine kinase-myocardial B fraction (CK-MB) were measured to assess heart function. The total iron content in the serum was measured to investigate the effect of the administrated magnetic nanoparticles on blood constituents. Additionally, the glucose level was measured. All measurements were performed according to the procedures of the biochemical kit assay.
Oxidative stress and antioxidant activity
Liver and heart tissues were homogenized in chilled 10 mM PBS with optimal pH 7.4 and homogenate (1 g/10 ml 75% aqueous methanol) was centrifuged and filtered. Malondialdehyde (MDA) and glutathione (GSH) contents were recorded using the high-performance liquid chromatography HPLC method [17, 18].
Histopathological examination
Specimens (heart and liver) were fixed in 10% formalin solution for 48 h and serial dilutions of alcohol were used for dehydration. Specimens were cleared in xylene and embedded in paraffin at 56 °C in a hot air oven for 24 h. Sections were sliced into 4 μm thick sections by a sledge microtome. The tissue sections were collected on glass slides, deparaffinized, stained with hematoxylin & eosin stain (H&E) then examined by light microscope [19].
Quantitative immunohistochemical analysis of TNF-α and HSP70
Immunohistochemical analysis was performed according to the manufacturer’s protocol. Deparaffinized retrieved tissue sections were treated with 0.3% H2O2 for 20 min. After that, heart and liver samples (1 week groups only were chosen due to observed significant difference) were incubated at 4°C overnight with anti-TNF-α (Abcam, Massachusetts, USA) (rabbit polyclonal antibody, code no. ab6671, the reaction is cytoplasmic and membranous and the +ve control was dendritic cells). It was used for the detection of tissue inflammation. While the reaction of anti-heat shock protein 70 (HSP70) (LabVision, USA) (Ab-2 mouse monoclonal antibody code no., NA.41, is nuclear and cytoplasmic and the +ve control was breast cancer). It was used for the detection of tissue improvement. An additional slide of heart and liver specimens was treated with a buffer solution at instead of primary antibodies in every run as the negative control. Tissue sections were washed out with PBS followed by incubation with a secondary antibody HRP Envision kit (DAKO) for 20 min. Then washed out again and incubated with diaminobenzidine as chromogen for 15 min. Tissue sections were washed with PBS then counterstained with hematoxylin, dehydrated, cleared in xylene then coverslipped for microscopic examination.
The morphometric study
The data were collected using the image analyzer computer system (Leica Qwin 500, England). The area % of TNF-α and HSP70 immune expressions were measured in 10 high power non- overlapping fields in each specimen using binary mode.
Statistical analysis
Data are expressed as mean ± SE. Comparisons between different groups were made using one-way analysis (ANOVA) and Tukey’s multiple comparisons test using the software GraphPad InStat and Statistical for the Social Sciences program (SPSS version 20.0, Chicago, USA). A probability level of less than 0.05 was accepted as statistically significant [20].
Results
Physicochemical characterization
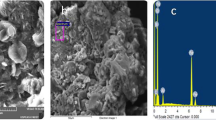
The TEM micrographs of the IONPs and Ru-IONPs have approximately convergent sizes, with spherical shapes and mean diameters of about 8 and 10 nm, respectively (Fig. 1a and b). The mean zeta potentials for the prepared IONPs and Ru-IONPs are represented in Table 1. The results demonstrated that the measured zeta potential value of the Ru-IONPs (−29.5 ± 5.4 mV) was highly negative as compared with that of the IONPs (−19 ± 3.9 mV). The hydrodynamic size of IONPs and Ru-IONPs was assessed in an aqueous solution (pH 7) represented at Fig. 2a and Table 1. The IONPs and Ru-IONPs have an average hydrodynamic size of 32.7 ± 8.7 and 43.8 ± 10.7 nm with a PDI of 0.291 and 0.234, respectively. The FTIR spectra of Ru, IONs, and Ru-IONs were recorded as shown in Fig. 2b. The absorption bands for the pure Ru are well resolved, but those of the Ru-IONs are rather broad. FTIR spectrum of Ru-IONPs shows a band at 1620 cm−1 which is attributed to the Ru COOH group. In addition, the represented band at 580 cm−1 indicates the stretching vibration mode of iron for the Fe-O group. The transmissions at 3613 cm−1 correspond to O–H stretching vibrations. For pure Ru, the transmission bands observed at 1600–850 cm−1 were attributed to the C–O stretching vibration of phenols, aryl ketones C=O stretching vibration, and the bending vibration of C–H aromatic hydrocarbon. For Ru-IONPs, the transmission peaks at 1050 cm−1 and 1470 cm−1 indicate the presence of the aforementioned RU functional groups at the nanoparticle surfaces.
Effect on in vivo iron distribution
The distributions of iron in the liver, kidneys, and heart tissues at 1 h, 1 day, and 1 week after administrated of IONPs and Ru-IONPs are illustrated in Fig. 3. After 1 h, iron accumulates more efficiently in the liver > kidney > heart in both IONPs and Ru-IONPs groups when compared to the control group. After 1 day, iron accumulates more efficiently in the kidney > liver > heart in the IONPs group while more efficiently in the liver > kidney > heart in the Ru-IONPs group when compared to the control group. After 1 week, iron accumulates more efficiently in the liver > kidney > heart in the IONPs group while more efficiently in the kidney > liver > heart in the Ru-IONPs group when compared to the control group. There are significant differences between IONPs and Ru-IONPs in kidney iron deposition at every time interval and in the heart at 1 day only.
Effect on hepatic parameters
Compared with the control group, the activity of AST significantly increased for the IONPs group by 19 %, 1 day post-injection while increased for both IONPs and Ru-IONPs groups by 42 % and 18 %, respectively, 1 week post-injection. However, AST activity in IONPs revealed non-significant changes, 1 h post-injection, and in Ru-IONPs, 1 h, and 1 day post-injection if compared to the control group. On the other hand, ALT activity increased in the IONPs group by 17%, 1 day post-injection but increased in both IONPs and Ru-IONPs group by 46 % and 22 %, respectively, 1 week post-injection in comparison with the control group. Accordingly, AST and ALT activities significantly decreased in the Ru-IONPs group (−17%) compared to IONPs, 1 week post-injection. Though, there was a no-significant change in the AST and ALT activities in the Ru-IONPs group compared to the IONPs group, 1 h, and 1 day post-injection (Fig. 4).
Effect on cardiac parameters
Figure 5 showed a significant increase in CK-MB level for the IONPs group by 24 %, 1 day post-injection while increased for both IONPs and Ru-IONPs groups by 3 folds and 1.3 folds, respectively, 1 week post-injection compared to the control group. On the contrary, LDH activity significantly increased only in the IONPs group by 24 % and 42 %, 1 day, and 1 week post-injection, respectively versus the control group. In contrast, both CK-MB and LDH significantly decreased in the Ru-IONPs group, 1 week post-injection by 2.4 folds and 1.3 folds, respectively concerning that of IONPs, 1 week.
Effect on oxidative stress and antioxidant activity
Regarding GSH content of the heart, there was a significant decrease in both IONPs and Ru-IONPs groups by −14 % and −11 %, respectively 1 day post-injection while decreased for the IONPs groups by −17 %, 1 week post-injection compared to the control group. Though hepatic content of GSH recorded a significant decrease in both IONPs and Ru-IONPs groups by −22 % and −7 %, respectively 1 day post-injection while decreased for the IONPs groups by −15 %, 1 week post-injection compared to the control group. Meanwhile, these cardiac and hepatic GSH contents displayed a significant increase the in Ru-IONPs group, 1 week post-injection by 17 % and 13 %, respectively if compared with IONPs, 1 week. Concerning the MDA level in the heart, there was a significant increase in the IONPs group by 11 %, 1 h post-injection as compared to the control group. But it significantly increased in both IONPs and Ru-IONPs groups by 26 % and 18 %, respectively 1 day post-injection, and by 43 and 14 %, respectively 1 week post-injection compared to the control group. At the same time, MDA level in the liver exhibited a significant increase in both IONPs and Ru-IONPs groups by 28 % and 15 %, respectively 1 day post-injection and by 42 and 14 %, respectively 1 week post-injection compared to the control group. Conversely, these cardiac and hepatic MDA levels displayed a significant decrease in the Ru-IONPs group, 1 week post-injection by −20 % and −25 %, respectively if compared with IONPs, 1 week (Fig. 6).
Cardiac and hepatic (A and B) GSH (μmol/g tissue) and (C and D) MDA (nmol/g tissue) contents in control and treated animals, sacrificed after 1 h, 1 day, and 1 week. Data are mean ± SE (n = 6). aSignificantly different from control. bSignificantly different from uncoated IONP, sacrificed after same duration
Effects on histopathological and immunohistochemical examination
Hematoxylin and Eosin stain of the heart
The control group showed normal architecture of myocardium; branching and anastomosing cardiac muscle fibers running in different directions with central oval vesicular nuclei, acidophilic sarcoplasm, and blood vessels in the connective tissue in-between muscle fibers (Fig. 7a). IONp, 1 week group showed pale cardiac muscle cells with nuclear ghosts and vacuolation in sarcoplasm, eosinophilic cardiac muscle cells with small pyknotic nuclei, waviness of muscle fibers, extravasated blood, and wide interstitial space between fibers (Fig. 7b). Ru-IONP, 1 week group showed a normal arrangement of cardiac muscle fibers with central nuclei and acidophilic sarcoplasm separated with little interstitial spaces containing blood vessels. Some fibers are dark acidophilic and widely separated (Fig. 7c and d).
A photomicrograph of a rat myocardium in different experimental groups (a) control group (H&EX400): showing the normal architecture of myocardium; branching and anastomosing cardiac muscle fibers (thin arrows) running in different directions with central oval vesicular nuclei, acidophilic sarcoplasm and blood vessels (bv) in the connective tissue in-between muscle fibers. (b) IONP, 1 week group (H&EX400): showing pale cardiac muscle cells with nuclear ghosts (thick arrow) and vacuolation (V) in sarcoplasm, eosinophilic cardiac muscle cells with small pyknotic nuclei (thin arrow), waviness of muscle fibers (arrowhead), extravasated blood (E) and wide interstitial space between fibers (W). (c and d): Ru-IONp, 1 week group (c: H&EX200 ) (d: H&EX400 ): showing the normal arrangement of cardiac muscle fibers (thick arrows) with central nuclei and acidophilic sarcoplasm separated with little interstitial spaces containing blood vessels (bv). Some fibers are dark acidophilic and widely separated (thin arrow)
Hematoxylin and Eosin stain of the liver
The control group showed normal polygonal pale acidophilic hepatocytes with central vesicular nuclei arranged in rows around the central vein and separated by narrow blood sinusoids lined by endothelium and Kupffer cells (Fig. 8a). Normal portal tracts containing bile ducts lined by simple cuboidal epithelium and portal vein branches were also observed in the control group (Fig. 8b). IONP, 1 week group (Fig. 8c and d) showed dilated and congested central vein, sinusoids with hypertrophied Kupffer cells, apoptosis with pyknotic nuclei of hepatocytes (Fig. 8c), hyperplasia and pleomorphism of cells lining bile ducts in the portal tract in addition to the dilated and congested vein (Fig. 8d). Ru-IONP, 1 week group (Fig. 8e and f) showed a normal arrangement of hepatocytes around the normal central vein, apparently normal bile ducts in the portal tract. Blood sinusoids (S) appear congested (Fig. 8e), decreased cellular infiltration, and improved cellular lining of bile ducts in the portal tract. Many hepatocytes appear normal with vesicular nuclei (Fig. 8f).
A photomicrograph of sections of rat liver in different experimental groups. (a) Control group (H&EX400): showing normal polygonal pale acidophilic hepatocytes with central vesicular nuclei (thick arrows) arranged in rows around the central vein (CV) and separated by narrow blood sinusoids lined by endothelium and Kupffer cells (thin arrow). (b: H&EX400): showing normal portal tract containing bile ducts lined by simple cuboidal epithelium (thick arrow) and branch of the portal vein (thin arrow). (c) IONp, 1 week group (H&EX400): showing dilated and congested central vein (CV), sinusoids (S) with hypertrophied Kupffer cells (thin arrows), apoptosis with pyknotic nuclei of hepatocytes (thick arrows). (d): IONp, 1 week group (H&EX400): showing hyperplasia and pleomorphism of cells lining bile ducts in the portal tract (thin arrows) in addition to dilated and congested veins (V). (e) Ru-IONp, 1 week group (H&EX200) showing a normal arrangement of hepatocytes around normal central vein (CV), apparently normal bile ducts in portal tract (thin arrow). Blood sinusoids (S) appear congested. (f) Ru-IONp, 1 week group (H&EX400) showing decreased cellular infiltration and improved cellular lining of bile ducts in the portal tract (thin arrows). Many hepatocytes appear normal with vesicular nuclei (thick arrows)
TNF-α immunostaining of the heart
The control group showed a negative immunoexpression of TNF-α in the cytoplasm and nuclei of cardiac muscle fibers (Fig. 9a). IONp, 1 week group showed positive immunoexpression of TNF-α in the cytoplasm of muscle fibers (Fig. 9b). Ru-IONp 1 week group showed decreased positive immunoexpression of TNF-α in the cytoplasm of muscle fibers (Fig. 9c) (Table 2).
A photomicrograph of sections of rat myocardium in different experimental groups (TNF-α X400). (a) Control group showing negative immune expression of TNF-α in cytoplasm and nuclei of muscle fibers (arrows). (b) IONp, 1 week group showing positive immune expression of TNF-α in the cytoplasm of muscle fibers (arrows). (c) Ru-IONp, 1 week group showing decreased positive immune expression of TNF-α in the cytoplasm of muscle fibers (arrows). (d) Mean values of TNF-α in heart tissues of different experimental groups. aSignificantly different from control. bSignificantly different from uncoated IONP, sacrificed after 1 week. IONPs, iron oxide nanoparticles; Ru-IONPs, rutin-coated IONPs; TNF-α, Tumor necrosis factor-α
TNF-α immunostaining of the liver
The control group showed positive immunoexpression of TNF-α in the cytoplasm of a few hepatocytes and negative immunoexpression of TNF-α in the cytoplasm of most hepatocytes (Fig. 10a). IONp, 1 week group showed increased positive immunoexpression of TNF-α in the cytoplasm of hepatocytes (Fig. 10b). Ru-IONp, 1 week group showed decreased positive immunoexpression of TNF-α in the cytoplasm of hepatocytes (Fig. 10c, and d) ( Table 2).
A photomicrograph of sections of rat liver in different experimental groups (TNF-α ×400). (a) Control group showing positive immune expression of TNF-α in the cytoplasm of few hepatocytes (thin arrows) and negative immune expression of TNF-α in the cytoplasm of most hepatocytes (thick arrows). (b) IONp, 1 week group showing increased positive immune expression of TNF-α in the cytoplasm of hepatocytes (arrows). (c and d) Ru-IONp, 1 week group showing decreased positive immune expression of TNF in the cytoplasm of hepatocytes (arrows). (e) Mean values of TNF-α in liver tissues of different experimental groups. aSignificantly different from control. bSignificantly different from uncoated IONP, sacrificed after 1 week. IONPs, iron oxide nanoparticles; Ru-IONPs, rutin-coated IONPs; TNF-α, Tumor necrosis factor-α
HSP70 immunostaining of the heart
The control group showed some positive immunoexpression of HSP70 in nuclei and the cytoplasm of cardiac muscle fibers (Fig. 11a). IONp, 1 week group showed minimal positive immunoexpression of HSP70 in the cytoplasm of muscle fibers (Fig. 11b). Ru-IONp 1 week group showed increased positive immunoexpression of HSP70 in nuclei and the cytoplasm of muscle fibers (Fig. 11c and Table 2).
A photomicrograph of sections of rat myocardium in different experimental groups (HSP70 ×400). (a) Control group showing some positive immune expression of HSP70 in nuclei and cytoplasm of muscle fibers (arrows). (b) IONp, 1 week group showing minimal positive immune expression of HSP70 in the cytoplasm of muscle fibers (arrows). (c) Ru-IONp, 1 week group showing increased positive immune expression of HSP70 in nuclei and cytoplasm of muscle fibers (arrows). (d) Mean values of HSP70 in heart tissues of different experimental groups. aSignificantly different from control. bSignificantly different from uncoated IONP, sacrificed after 1 week. IONPs, iron oxide nanoparticles; Ru-IONPs, rutin-coated IONPs; Hsp70, Heat shock protein 70
In the liver
The control group showed some positive immunoexpression of HSP70 in the nuclei and cytoplasm of hepatocytes (Fig. 12a). IONp 1 week group showed positive immunoexpression of HSP70 in the cytoplasm of some hepatocytes and negative immunoexpression in the nuclei (Fig. 12b). Ru-IONp, 1 week group showed increased positive immunoexpression of HSP70 in nuclei and the cytoplasm of hepatocytes (Fig. 12c and d) (Table 2).
A photomicrograph of sections of rat liver in different experimental groups (HSP70 ×400). (a) Control group showing some positive immune expression of HSP70 in nuclei and cytoplasm of hepatocytes (arrows). IONp, 1 week group (b) showing positive immune expression of HSP70 in cytoplasm of some hepatocytes (thin arrows) and negative immune expression in the nuclei (thick arrows). (c and d) Ru-IONp, 1 week group showing increased positive immune expression of HSP70 in nuclei and cytoplasm of hepatocytes (arrows). (e) Mean values of HSP70 in liver tissues of different experimental groups. aSignificantly different from control. bSignificantly different from uncoated IONP, sacrificed after 1 week. IONPs, iron oxide nanoparticles; Ru-IONPs, rutin-coated IONPs; Hsp70, Heat shock protein 70
Discussion
IONPs have great potential medical applications including, tissue healing, anemia treatments, and magnetic hyperthermia in cancer treatment. However, possible associated liver and heart toxicities are reported and these toxicities may be varied depending on nanoparticles characteristics (size, shape, and surface modification) [21]. Despite the wide application of IONPs, little is known about the detailed mechanism of their cardiac and hepatic toxic effects. The effects of a single IV dose of iron oxide nano-formulations are not well mentioned at previous studies and there is no study on the role of Ru coating on the nanoparticles acute toxicities. We aimed to evaluate the cardiotoxic and hepatotoxic effects of IONPs in vivo and assessing the protective effect of Ru against these toxic effects.
Commonly, the size of NPs is the predominant factor in controlling their clearance and distribution. For medical applications the size of nanoparticles should be in the range of 5–100 nm in which the blood circulation time are enhanced [22]. Too small nanoparticles will be rapidly removed via kidneys, but if they too large, it is efficiently trapped by cells in the reticuloendothelial system (RES) organs [23]. This indicates that the prepared nano-formulations within the suitable size range of medical application. Additionally, it was found that spherical-shaped nanoparticles are much less toxic compared to rod-shaped nanoparticles [11].
The higher negative surface potential of Ru-IONPs gives an advantage in reducing the tendency of nanoparticles to adsorb the plasma proteins and elevate nanoparticles’ stability at the physiological condition and thus prolonging their circulation time [24, 25]. It was reported that negatively charged nanoformulations characterized with lower albumin adsorption which in turn can explain their better blood circulation [26]. The PDI value of prepared non-formulations indicates their higher monodisperse distribution. Changes in both of size and surface charge of Ru-IONPs can be used as proof for successful coating of IONPs. FTIR spectra of IONPs, Ru, and Ru-IONPs were performed to assess the interaction of Ru coating of IONPs surfaces. In the Ru spectrum, the 1620 cm−1 peak is assignable to the asymmetric stretching vibration of the C=O group from the COOH group of Ru. This peak shifts to an intense band in the Ru-IONPs spectrum, revealing the binding of Ru to the surface of IONPs and the formation of complexes between Ru and IONPs. The results of the present study are consistent with a previous study in which citrate and IONPs complexes rendered partial single bond character to the C=O bond resulting in its weakening and shifting of its stretching frequency to a lower value [27]. Moreover, the transmission bands observed at 1600–850 cm−1 of the C–O stretching vibration of phenols, and aryl ketones C=O, in addition to the bending vibration of C–H aromatic hydrocarbon present in the polyphenolic compound Ru bioflavonoid (C27H30O16). The presence of these functional groups in the RU may help in the reduction, capping, and stabilization of prepared nanoparticles. On the contrary, the reduction in OH frequency in the Ru-IONPs spectrum verified the bonding between Ru and IONPs [28]. In another study, it was found that short peaks observed from 500 to 800 cm−1 were assigned to the presence of metal-oxygen (Fe-O) in the chitosan-IONPs spectrum [29]. These findings are in line with the study which reported that the represented band at 580 cm−1 indicates the stretching vibration mode of iron for the Fe-O group in the Ru-IONPs spectrum. The presence of the aforementioned Ru functional groups in the Ru-IONPs spectrum supports the coating of Ru on synthesized IONPs. In addition, O–H stretching vibrations peak showed a significant broadening and shifting in the Ru-IONPs spectrum, suggesting more formation of hydroxyl bonds between Ru and IONPs surfaces.
Small IONPs, however, may pose a serious health risk due to their tendency to be accumulated in cells and tissues at high concentrations and be more difficult to be eliminated. IONPs are metabolized in vivo to ions by the Kupffer cells in the liver and macrophages in the spleen, thus IONPs remain in these organs for a long time, causing toxicity risk. This can explain the level of accumulation of IONPs at organs in the descending order; liver>kidney>heart, after 1 week from the introduction of a single IV dose of uncoated IONPs formulation. Notably, the accumulation of iron in the liver, kidney, and heart tissues is significantly changed at all time intervals after administration of IONPs and Ru-coated IONPs formulations if compared to controls. After treatment with Ru-coated IONPs formulation, the accumulation of iron is significantly changed in the kidney tissue at all-time intervals and changed in the heart tissue only after 1-h exposure as compared to uncoated IONPs. We found also that the increased size of Ru-IONPs than IONPs make their accumulation in kidney tissue in higher concentration 1wk after exposure. The same result was recorded by a previous study that showed that for IONPs with a size of 30–35 nm the level of accumulation of iron in organs in the descending order; spleen>blood>liver>kidney>lung> heart>testicle>brain [30]. Our findings also agree with those of a previous study that showed that after 10 consecutive days of administration of IONPs formulations with several capping agents, (citrate [Cit-IONPs], curcumin [Cur-IONPs], and chitosan [CS-IONPs]) varied among various tissues. The authors demonstrated that the highest iron accumulation after the administration of Cit-IONPs was observed in the liver. In contrast, the highest iron accumulation after the administration of CS-IONPs was observed in the spleen, indicating that their clearance was mainly done via the spleen. Unsurprisingly, the uncoated IONPs group showed a higher accumulation of iron in the kidney for filtering them out from the body [8].
As expected, the liver is the major distribution site due to the Kupffer cell’s phagocytosis of NPs and increased blood supply in the liver [31]. Moreover, the liver plays a major role in the metabolic transformation of drugs; therefore, it is exposed to damage caused by drugs. Plasma levels of liver enzyme activity (ALT and AST) are proper markers for liver toxicity and hepatocellular integrity and their increase indicates their leakage from hepatic cells. A significant increase in AST and ALT is observed in the IONPs group, reaching its maximum at week 1, suggesting nanoparticles accumulation of IONPs in hepatocytes. These results are in harmony with a previous study that showed a transient increase in ALT and AST activities after single-dose administration of IONPs in mice reaching its maximum at week 1, then it began gradually decreasing until week 3 [24]. However, the AST and ALT activities were only slightly increased after 1 week of Ru-IONPs administration, indicating minimal hepatotoxicity of the promising Ru-IONP. This may be attributed to role of Ru in the maintenance of the plasma membrane integrity of hepatic cells and preventing enzymes leakage into the blood, in harmony with a recent study [32]. They proved the hepatoprotective effect of Ru on butachlor-induced hepatotoxicity and they suggested that the effect was due to the antioxidant effect of Ru.
CK-MB and LDH are enzymes classified as cardiotoxicity markers and their activities increase after IONPs administration reaching its maximum at week 1 indicates the induction of myocardial injury in the present study. These results are in line with a former study that reported that the elevated activities of CK-MB and LDH in rats administered hydroxyapatite nanoparticles have resulted from their leakage within the circulation from cardiomyocytes due to cardiac muscular tissue damage [33]. Conversely, the Ru-IONPs, 1 week group showed a significant decrease in CK-MB and LDH activities, compared to uncoated IONPs with restoration of CK-MB normal values. These results demonstrated that Ru could attenuate the myocardial injury that may be caused by IONPs. In agreement with our results, Ru reduced the elevated activities of serum enzymes related to heart function including CK-MB and LDH induced by doxorubicin in a previous work [34].
Interestingly, the production of ROS, which could cause oxidative stress, and inflammation, and consequently damage to proteins, cell membranes, and DNA, is a predominant mechanism of IONPs toxicity [35]. In accordance, the present study showed that IONPs induce oxidative stress, especially after 1hr and 1wk, either through the production of ROS or the depletion of endogenous antioxidants. Overproduction of ROS in IONP-treated rats induced lipid peroxidation in liver and heart tissues by a significant increase in hepatic and cardiac MDA content, consuming their antioxidant GSH contents, compared to the control group. This indicates that IONPs may induce hepatic and cardiac toxic effects through oxidative stress. The current results were consistent with previous studies that stated that IONP injection could induce oxidative stress and considerably hinder the main processes of antioxidants in particular the antioxidant GSH system [36]. On the contrary, rats treated with Ru-IONP efficiently reduced MDA while increasing GSH cardiac and hepatic contents in the current study when compared to either the IONP group. In line with our results, previous study established that RU is effective at preventing liver toxicity by reducing MDA levels while increasing glutathione-S-transferase, glutathione peroxidase, and superoxide dismutase activity as well as GSH concentrations [37]. The antioxidant properties of RU have been described in various previous studies due to its role as a ROS scavenger by donating hydrogen atoms to superoxide anions and hydroxyl and peroxy radicals [13, 38]. Moreover, RU is oxidized to a quinone, which helps to reduce the risk of cardiovascular disease by upregulating the nuclear factor erythroid 2-related factor-mediated endogenous antioxidant response, a transcriptional factor that regulates cellular responses to oxidative stress [38]. The second main underlying mechanism of the cytotoxic effects of IONPs on a cellular level is iron release. When taken up by cells through endocytosis, IONPs decompose into ions directly or through a lysosome way hence, not only the coating of the nanoparticle is of great importance, but also the method of its preparation [1]. Ru has metal-chelating capabilities, thereby preventing metal ion-induced peroxidation [39].
Histopathological and immunohistochemical results confirmed all previously discussed findings, supporting the decreased hepatic and cardiac injuries in histopathological biopsies after the treatment Ru-IONPs groups, compared to uncoated IONPs. In the current study, cardiac and hepatic toxicities were confirmed by histopathological changes including pale cardiac muscle cells with nuclear ghosts and vacuolation in sarcoplasm, eosinophilic cardiac muscle cells with small pyknotic nuclei, waviness of muscle fibers, extravasated blood and wide interstitial space between fibers in heart tissues of IONPs 1 week group. Such findings matched with a recent study that revealed cellular degeneration and necrosis in the heart after IONPs exposure [40]. However, Ru-coated IONPs administration ameliorated the structural damages induced by uncoated IONPs in the different organs due to its antioxidant properties through scavenging free radicals. In line with our findings, a previous study stated that suppression of autophagy and apoptosis by administration of Ru could attenuate doxorubicin-induced cardiotoxicity [34]. The liver is the principal organ of detoxification, and as a result of the damage induced, there were degenerative changes in the liver tissues of the IONPs 1 week group. We observed apoptotic hepatocytes with pyknotic nuclei, hypertrophied Kupffer cells, dilated and congested veins, sinusoids in addition to hyperplasia, and pleomorphism of cells lining the bile ducts in portal tracts. Our findings agree with a previous study revealed the presence of signs of toxicity being predominant for groups treated with uncoated IONPs [8]. However, Cur-IONPs and CS-IONPs showed mild toxicity when administered at the same doses, in harmony with our results that exhibited that Ru-IONPs were capable of maintaining hepatocytes and cardiomyocytes’ normal structure and increasing their vitality. Moreover, Ru alleviated the pathological damage of these tissues even in the presence of their high iron contents, indicating that Ru did not reduce tissue damage by inhibiting iron content but it might enhance the body’s resistance to IONPs. In agreement with our results, a previous work proved that Ru provided potential chemopreventive effects against doxorubicin-induced hepatotoxicity by suppressing oxidative stress, inflammation, and apoptosis [37]. Regarding the effect of IONPs on heart tissue, the microscopic examination revealed a severe toxic effect on myocardial fibers in our study where most fibers were fragmented with pale acidophilic sarcoplasm and pyknotic nuclei. In addition, focal areas of hyalinization and hemorrhage in between myocardial fibers were noted, and such findings matched the findings of IONPs effects in a recent study [40]. Besides direct cardiac exposure to them, the cardiovascular system is also affected by NPs’ secondary effects on other organs, leading to systemic cardiovascular toxicity. However, Ru-coated IONPs administration ameliorated the structural damages induced by uncoated IONPs in the cardiac tissue which might be also due to its antioxidant properties through scavenging free radicals.
Another mechanism of the cytotoxic effects of IONPs is accountable for inducing inflammation and consequently, activation of NF-κB signaling. As supported with the present immunohistochemical findings, the precipitation of IONPs in liver and cardiac tissues causes the recruitment of inflammatory cells, which in return induces ROS and cytokines generation. TNF-α is not expressed in normal cardiomyocytes, but after cardiotoxicity activation of mononuclear macrophages in cardiomyocytes, generating TNF-α in large amounts in the myocardium for nourishing and enhancing neutrophils recruitment in inflammation sites [33]. A similar pattern of immunohistochemical results was observed in the examined liver. The immune expression of TNF-α, a proinflammatory cytokine, was increased significantly in both the liver and cardiac tissues of rats treated with IONPs in the current study. When rats were treated with Ru-IONPs, the immune expression of TNF-α in both cardiac and liver tissues decreased significantly. These findings are consistent with previous studies that proved that TNF-α suppression contributes at least in part to the anti-inflammatory, anti-necrotic, and antiapoptotic effects of Ru in both liver and cardiac tissues, respectively [37, 38]. They found that acute myocardial infarction, unstable angina pectoris, and heart failure all appear to be linked to NF-κB activation, which controls the production of cytokines including TNF-α. Moreover, Ru has shown therapeutic and preventive impacts in various cardiovascular disease forms [38, 39].
Heat shock proteins (HSPs) are an important protective mechanism of hepatocytes in liver injury conditions and plays crucial roles in liver regeneration. Their depletion causes hepatocyte injury and death while their overexpression alleviates multiple stress-induced liver injuries [41]. Furthermore, the primary HSP70 protein maintains the structural and functional integrity of different organs against stress-induced tissue damage cells [42]. In this study, rats treated with IONPs showed a down regulation in HSP70 immune expression whereas its immune expression was markedly upregulated in rats treated with Ru-IONPs. We suggested that the reduction of HSP70 induced by IONPs is related to oxidative stress, apoptosis, cardiovascular abnormality, and heart tissue damage. In line with our results, a previous study recommended that the expression profiling of small heat shock proteins be included in the nanotoxicity of IONPs [43]. While Ru-IONPs caused overexpression of HSP70, leading to an increase in liver and heart resistance to stressors. These results are in agreement with the previous findings that concluded that resveratrol, another polyphenolic compound, activates the endogenous antioxidant defense system and subsequently enhances the antioxidative status, leading to an increase in the expression of HSP and protecting against heat stress-mediated liver injury [42].
Conclusion
Consistent with all these previous findings, the main toxic mechanisms of IONPs were possibly cumulative cellular oxidative stress, inflammation of cells, and induce indirect damage to the DNA of the living systems. Ru can be used to alleviate these harmful effects through its antioxidative, anti-inflammatory, and antiapoptotic properties. Ru has a hepatoprotective and cardioprotective effect by maintaining functional integrity and improving cellular antioxidant status. Our results revealed the safety of Ru-IONPs when being used as an image contrast agent and drug nanocarrier.
Data availability
All data generated or analysed during this study are included in this published article.
References
Chrishtop VV, Mironov VA, Prilepskii AY, Nikonorova VG, Vinogradov VV (2021) Organ-specific toxicity of magnetic iron oxide-based nanoparticles. Nanotoxicology 15:167–204. https://doi.org/10.1080/17435390.2020.1842934
Fahmy HM, Saad OA, Fathy MM (2023) Insight into the photothermal therapeutic impacts of silica-coated iron oxide nanocomposites. J Drug Deliv Sci Technol 84:104540. https://doi.org/10.1016/j.jddst.2023.104540
Ventola CL (2017) Progress in nanomedicine : approved and investigational nanodrugs progress in nanomedicine. Pharm Ther 42:742–755
Abo-zeid Y, Ismail NSM, McLean GR, Hamdy NM (2020) A molecular docking study repurposes FDA approved iron oxide nanoparticles to treat and control COVID-19 infection. Eur J Pharm Sci 153:1–7. https://doi.org/10.1016/j.ejps.2020.105465
Mihailovic V, Katanic Stankovic JS, Selakovic D, Rosic G (2021) An overview of the beneficial role of antioxidants in the treatment of nanoparticle-induced toxicities. Oxid Med Cell Longev 2021:1–21. https://doi.org/10.1155/2021/7244677
Yarjanli Z, Ghaedi K, Esmaeili A, Rahgozar S, Zarrabi A (2017) Iron oxide nanoparticles may damage to the neural tissue through iron accumulation, oxidative stress, and protein aggregation. BMC Neurosci 18:1–12. https://doi.org/10.1186/s12868-017-0369-9
Gaharwar US, Kumar S, Rajamani P (2020) Iron oxide nanoparticle-induced hematopoietic and immunological response in rats. RSC Adv 10:35753–35764. https://doi.org/10.1039/d0ra05901c
Fahmy HM, Abd El-Daim TM, Ali OA, Hassan AA, Mohammed FF, Fathy MM (2021) Surface modifications affect iron oxide nanoparticles’ biodistribution after multiple-dose administration in rats. J Biochem Mol Toxicol 35:1–10. https://doi.org/10.1002/jbt.22671
Arami H, Khandhar A, Liggitt D, Krishnan KM (2015) In vivo delivery, pharmacokinetics, biodistribution and toxicity of iron oxide nanoparticles. Chem Soc Rev 44:8576–8607. https://doi.org/10.1039/c5cs00541h
Fröhlich E (2016) Action of nanoparticles on platelet activation and plasmatic coagulation. Curr Med Chem 23:408–430
Jiang Z, Shan K, Song J, Liu J, Rajendran S, Pugazhendhi A, Jacob JA, Chen B (2019) Toxic effects of magnetic nanoparticles on normal cells and organs. Life Sci 220:156–161. https://doi.org/10.1016/j.lfs.2019.01.056
Pucci C, Degl'Innocenti A, Gümüş MB, Ciofani G (2022) Superparamagnetic iron oxide nanoparticles for magnetic hyperthermia: recent advancements, molecular effects, and future directions in the omics era. Biomater Sci 10:2103–2121. https://doi.org/10.1039/D1BM01963E
Hussein MMA, Gad E, Ahmed MM, Arisha AH, Mahdy HF, Swelum AAA, Tukur HA, Saadeldin IM (2019) Amelioration of titanium dioxide nanoparticle reprotoxicity by the antioxidants morin and rutin. Environ Sci Pollut Res 26:29074–29084. https://doi.org/10.1007/s11356-019-06091-0
Zothantluanga JH (2021) Molecular docking simulation studies, toxicity study, bioactivity prediction, and structure-activity relationship reveals Rutin as a potential inhibitor of SARS-CoV-2 3CL pro. J Sci Res 65:96–104. https://doi.org/10.37398/JSR.2021.650511
Fathy MM, Nasser L, El-Sokkary G, Rasheedy MS (2021) Combined chemo-photothermal therapy of metastatic mammary adenocarcinoma using curcumin-coated iron oxide nanoparticles. Bionanoscience 11:447–453. https://doi.org/10.1007/s12668-021-00841-6
Wortmann AC, Froehlich PE, Pinto RB, Magalhães RB, Álvares-Da-Silva MR, Ferreira JJ, Silveira TR (2007) Hepatic iron quantification by atomic absorption spectrophotometry: full validation of an analytical method using a fast sample preparation. Spectroscopy 21:161–167 https://content.iospress.com/articles/spectroscopy/spe310 (accessed December 17, 2023)
Augustin A, Böker T, Blumenröder S, Lutz J, Spitznas M (1994) Free radical scavenging and antioxidant activity of allopurinol and oxypurinol in experimental lens-induced uveitis. Invest Ophthalmol Vis Sci 35:3879–3904 https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1056.5483&rep=rep1&type=pdf (accessed May 26, 2022)
Begic A, Djuric A, Gobeljic B, Stevanovic I, Lukic V, Stanojevic I, Ninkovic M, Saso L, Vojvodic D, Djukic M (2017) The simple isocratic HPLC—UV method for the simultaneous determination of reduced and oxidized glutathione in animal tissue. Akjournals Com 29:67–84. https://doi.org/10.1556/1326.2017.29.1.5
Swisher B, Bancroft JD, Gamble M (2002) Microorganisms. In: Bancroft JD, Gamble M (eds) Theory and Practice of Histological Techniques, 5th edn. Churchill Livingstone, London, p 337
R. Levesque, SPSS programming and data management: a guide for SPSS and SAS users, 3 rd. edit, United States of America, 2007.
Fu H, Miao C, Rui Y, Hu F, Shen M, Xu H, Zhang C, Dong Y, Wang W, Gu H, Duan Y (2019) Strategy to prevent cardiac toxicity induced by polyacrylic acid decorated iron MRI contrast agent and investigation of its mechanism. Biomaterials 222:119442. https://doi.org/10.1016/j.biomaterials.2019.119442
Feng Q, Liu Y, Huang J, Chen K, Huang J, Xiao K (2018) Uptake, distribution, clearance, and toxicity of iron oxide nanoparticles with different sizes and coatings. Sci Rep 8:1–13. https://doi.org/10.1038/s41598-018-19628-z
McNeil SE (2005) Nanotechnology for the biologist. J Leukoc Biol 78:585–594. https://doi.org/10.1189/jlb.0205074
Elbialy NS, Aboushoushah SF, Alshammari WW (2019) Long-term biodistribution and toxicity of curcumin capped iron oxide nanoparticles after single-dose administration in mice. Life Sci 230:76–83. https://doi.org/10.1016/j.lfs.2019.05.048
Ghorbani M, Bigdeli B, Jalili-baleh L, Baharifar H, Akrami M, Dehghani S, Goliaei B, Amani A, Lotfabadi A, Rashedi H, Haririan I, Alam NR, Hamedani MP, Khoobi M (2018) Curcumin-lipoic acid conjugate as a promising anticancer agent on the surface of gold-iron oxide nanocomposites: a pH-sensitive targeted drug delivery system for brain cancer theranostics. Eur J Pharm Sci 114:175–188. https://doi.org/10.1016/j.ejps.2017.12.008
Patil S, Sandberg A, Heckert E, Self W, Biomaterials SS, U. (2007) Protein adsorption and cellular uptake of cerium oxide nanoparticles as a function of zeta potential. Biomaterials 28(2007):4600–4607 https://www.sciencedirect.com/science/article/pii/S0142961207005546 (accessed December 17, 2023)
Nigam S, Barick K, Bahadur D (2011) Development of citrate-stabilized Fe3O4 nanoparticles: conjugation and release of doxorubicin for therapeutic applications. J Magn Magn Mater 323:237–243. https://doi.org/10.1016/j.jmmm.2010.09.009
Saleemi MA, Alallam B, Yong YK, Lim V (2022) Synthesis of zinc oxide nanoparticles with bioflavonoid Rutin: characterisation, antioxidant and antimicrobial activities and in vivo cytotoxic effects on Artemia Nauplii. Antioxidants 11:1853. https://doi.org/10.3390/antiox11101853
Bharathi D, Bhuvaneshwari V (2019) Synthesis of zinc oxide nanoparticles (ZnO NPs) using pure bioflavonoid rutin and their biomedical applications: antibacterial, antioxidant and cytotoxic activities. Res Chem Intermed 45:2065–2078. https://doi.org/10.1007/s11164-018-03717-9
Gaharwar US, Meena R, Rajamani P (2019) Biodistribution, clearance and morphological alterations of intravenously administered iron oxide nanoparticles in male wistar rats. Int J Nanomedicine 14:9677–9692. https://doi.org/10.2147/IJN.S223142
Valentini X, Rugira P, Frau A, Tagliatti V, Conotte R, Laurent S, Colet JM, Nonclercq D (2019) Hepatic and renal toxicity induced by TiO2 nanoparticles in rats: a morphological and metabonomic study. J Toxicol 2019. https://doi.org/10.1155/2019/5767012
Olayinka ET, Kehinde SA, Olajide AT (2023) Attenuation of Rutin on Butachlor-induced hepatotoxicity in rats, Ajayi Crowther J. Pure. Appl Sci 2:1–8. https://doi.org/10.56534/acjpas.2023.02.01.01
Mosa IF, Abd HH, Abuzreda A, Yousif AB, Assaf N (2021) Chitosan and curcumin nanoformulations against potential cardiac risks associated with hydroxyapatite nanoparticles in wistar male rats. Int J Biomater 2021. https://doi.org/10.1155/2021/3394348
Mahmoud HUR, Ahmed OM, Fahim HI, Ahmed NA, Ashour MB (2020) Effects of rutin and quercetin on doxorubicin-induced renocardiotoxicity in male wistar rats. Adv Anim Vet Sci 8:370–384. https://doi.org/10.17582/JOURNAL.AAVS/2020/8.4.370.384
Mishra M, Panda M (2021) Reactive oxygen species: the root cause of nanoparticle-induced toxicity in Drosophila melanogaster. Free Radic Res 55:919–935. https://doi.org/10.1080/10715762.2021.1914335
Mohammed ET, Hashem KS, Abdelazem AZ, Foda FAMA (2020) Prospective protective effect of ellagic acid as a SIRT1 activator in iron oxide nanoparticle-induced renal damage in rats. Biol Trace Elem Res 198:177–188. https://doi.org/10.1007/s12011-020-02034-w
Ahmed OM, Elkomy MH, Fahim HI, Ashour MB, Naguib IA, Alghamdi BS, Mahmoud HUR, Ahmed NA (2022) Rutin and quercetin counter doxorubicin-induced liver toxicity in wistar rats via their modulatory effects on inflammation, oxidative stress, apoptosis, and Nrf2. Oxid Med Cell Longev 2022. https://doi.org/10.1155/2022/2710607
Oluranti OI, Alabi BA, Michael OS, Ojo AO, Fatokun BP (2021) Rutin prevents cardiac oxidative stress and inflammation induced by bisphenol A and dibutyl phthalate exposure via NRF-2/NF-κB pathway. Life Sci 284:119878. https://doi.org/10.1016/j.lfs.2021.119878
Rahmani S, Naraki K, Roohbakhsh A, Hayes AW, Karimi G (2023) The protective effects of rutin on the liver, kidneys, and heart by counteracting organ toxicity caused by synthetic and natural compounds. Food Sci Nutr 11:39–56. https://doi.org/10.1002/fsn3.3041
Amin R, Abd Elaliem N, Abdeen A, Ibrahim S, Elsafty M, Beder E (2023) Prospective ameliorative activity of neem (Azadirachta Indica) on iron oxide nanoparticle-induced multiple organ injury via attenuating TNF-α pathway. Benha Vet Med J 44:55–60. https://doi.org/10.21608/bvmj.2023.189946.1636
Bi J, Zhang J, Ke M, Wang T, Wang M, Liu W, Du Z, Ren Y, Zhang S, Wu Z, Lv Y, Wu R (2022) HSF2BP protects against acute liver injury by regulating HSF2/HSP70/MAPK signaling in mice. Cell Death Dis 13:1–9. https://doi.org/10.1038/s41419-022-05282-x
Khafaga AF, Noreldin AE, Taha AE (2019) The adaptogenic anti-ageing potential of resveratrol against heat stress-mediated liver injury in aged rats: role of HSP70 and NF-kB signalling. J Therm Biol 83:8–21. https://doi.org/10.1016/j.jtherbio.2019.04.012
Basaki M, Keykavusi K, Sahraiy N, Akbari G, Hejazi M (2022) Small heat shock protein’s gene expression response to iron oxide nanoparticles in the brain. Biol Trace Elem Res 200:1791–1798. https://doi.org/10.1007/s12011-021-02761-8
Acknowledgements
This work was carried out at NODCAR. All are acknowledged for creating conducive environment to perform experimental aspects.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research received no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Dr. Ehsan Khedre] and [Dr. Mohamed Fathy]. [Dr. Doaa Ebrahim] and [Nehad Ahmed Sadek] did the histopathological work. The first draft of the manuscript was written by [Dr. Ehsan Khedre] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for the experimental protocols was granted by the Scientific Research Ethics Committee in the Faculty of Medicine, Fayoum University (R 312). The study complied also with the Guide for Care and Use of Laboratory Animals issued by the US National Institutes of Health (NIH Publication No. 8023, revised 1978).
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamed, E.K., Fathy, M.M., Sadek, N.A. et al. The effects of rutin coat on the biodistribution and toxicities of iron oxide nanoparticles in rats. J Nanopart Res 26, 49 (2024). https://doi.org/10.1007/s11051-024-05949-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-024-05949-w