Abstract
Nanoparticle (NP) technologies are becoming commonplace in the development of vaccine delivery systems to protect against various diseases. The current study determined the efficacy of intranasal delivery of a 234 ± 87.5 nm poly lactic-co-glycolic acid nanoparticle vaccine construct in establishing protection against experimental respiratory pneumococcal infection. Nanoparticles encapsulating heat-killed Streptococcus pneumoniae (NP-HKSP) were retained in the lungs 11 days following nasal administration compared to empty NP. Immunization with NP-HKSP produced significant resistance against S. pneumoniae infection compared to administration of HKSP alone. Increased protection correlated with a significant increase in antigen-specific Th1-associated IFN-γ cytokine response by pulmonary lymphocytes. This study establishes the efficacy of NP-based technology as a non-invasive and targeted approach for nasal-pulmonary immunization against pulmonary infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Community-acquired pneumonia (CAP) remains the leading cause of morbidity and mortality worldwide despite advances in antimicrobial therapy and advances in the management of severe infections. Streptococcus pneumoniae (S. pneumoniae) in particular is responsible for an estimated 2 million deaths annually, making it the most common etiological risk for CAP (Tan 2012). Although conjugate and polysaccharide vaccines have been central to the prevention of S. pneumonia-induced CAP, the impact of vaccination particularly among the elderly has been less than expected due to a status quo in mortality rates. This lack in vaccine efficacy is believed to be attributed to less than optimal immune responses generated against current conjugate and polysaccharide vaccine constructs (Stano et al. 2010). Thus, a reduction in CAP-related deaths will be difficult to realize without improved strategies to augment immunity.
Evidence suggests that induction of immune responses locally across the respiratory mucosa enhances protective immunity against pathogens of the respiratory tract. Previous studies have shown that nasal immunization is advantageous in inducing protective immunity against respiratory, viral and bacterial infectious disease through the induction of local and systemic immune responses (Gutierro et al. 2002; Camacho et al. 2011; Cohen et al. 2011; Lindell et al. 2011). On the contrary, consideration of the potential limitations associated with nasal immunization is also of significant importance. In general, the respiratory mucosa is a volatile environment not unlike other mucosal sites (e.g., gastrointestinal) that could compromise the induction of immune responses resulting from the enzymatic destruction in vaccine components (Derudas et al. 2010). Also of concern is the potential for immune tolerance as routinely demonstrated in models of oral vaccination (Fattal et al. 2002; Gupta et al. 2007; Adam and Wright 2009).
Nanotechnology is emerging as a feasible approach to target activation of immune responses and promises to be an effective strategy to overcome current limitations mentioned above (Marriott et al. 2006; Gupta et al. 2007). We are particularly interested in the use of PLGA NPs. The use of PLGA NPs for targeting immune therapies provides numerous advantages including: biocompatibility, biodegradability, size specificity, composition and ease of production (Handsand and Lowman 2002; Gelperina et al. 2005; Adam and Wright 2009). Recently it has been shown that NP therapy provides a vehicle to activate a robust and lasting immune response against various pathogens (Keijzer et al. 2011). In the current study, we determined the efficacy of NP-HKSP-based vaccine against S. pneumoniae infection by targeting the respiratory mucosa for the induction of protective immunity. Our results demonstrate that intranasal administration of NP-HKSP produces enhanced protection against pneumococcal disease that is supported by a robust antigen-specific cell-mediated immune response.
Materials and methods
Animals
Adult (6–8 weeks of age) female CD-1 mice (Harlan Sprague–Dawley, Indianapolis, Indiana) were used in all studies. Mice were maintained under specific pathogen-free conditions on a 12:12 light/dark cycle (7:00 p.m–7:00 a.m). Mice were kept under optimal temperature and humidity controlled conditions. All studies were approved by the University of North Texas Health Science Center’s Institutional Animal Care and Use Committee (IACUC).
Nanoparticle construction
The PLGA NPs encapsulating HKSP were prepared by double emulsion method as previously described (Mukerjee and Vishwanatha 2009; Thamake et al. 2011). Briefly, 1 × 106 HKSP were lysed by sonication in 200 μl of phosphate-buffered saline (PBS), and 70 mg of PLGA (Lakeshore Biomaterials AL, USA) was dissolved in 1 ml of ethyl acetate. These two solutions were mixed and vortexed at maximum speed for 1 min to form primary water-in-oil emulsion. The primary emulsion was then mixed with 3 ml of 1 % polyvinyl alcohol (PVA) solution. This solution was sonicated using an ultrasonic processor UP200H system (Hielscher Ultrasonics GmbH, Germany) at 40 % amplitude for 2 min on continuous mode, in a clean glass vial immersed in ice, to prepare HKSP encapsulating PLGA NPs. The solution was further diluted to 20 ml with autoclaved water (0.22 μ filter sterilized) and stirred for 1 h at room temperature under mild vacuum to evaporate ethyl acetate. The solution was then centrifuged to collect NPs, and this process was repeated twice to remove excess PVA. The nanoparticle pellet was resuspended in 500 μl of autoclaved water and lyophilized using an ATR FD 3.0 system (ATR Inc. MO, USA). The final NPs were stored at −20 °C until further use.
To make fluorescently labeled HKSP NPs, nile red was premixed with PLGA solution in ethyl acetate (5 % v/v of 10 mg/ml nile red stock solution in ethyl acetate) and the remainder of the procedure was performed as explained above. Nile red is a lipophilic dye which partition into the organic phase and form complex with PLGA polymer. The excess of nile red is removed during the washes as the surfactant PVA helps in solubilization and removal of dye which is uncomplexed with PLGA (Ranjan et al. 2011). Nile red is a small molecule dye and does not affect the size of nanoparticles. Particle size of nanoparticles was determined by dynamic light scattering method (NanoTrac ULTRA) using aqueous suspension (1 mg/ml).
Intranasal immunization and infection
Mice were immunized on day 0 with either HKSP or NP-HKSP prepared from heat-killed S. pneumoniae by heating live bacteria in a water bath, set at 85° C, for 45–60 min (Hvalbye et al. 1999). Following dilution with PBS, immunization consisted of administrating a single dose of 4 × 105 colony forming unit (CFUs) equivalents of HKSP or NP-HKSP by intranasal route in two successive 40 μl volumes of 2 × 105 CFUs. This dose was determined by back-calculated based on the encapsulation efficiency.
S. pneumoniae strain #6301 (ATCC, Manassas, VA) was grown for 16 h to obtain mid-log phase cultures on blood agar plates. Mice were infected with 2 × 105 CFUs (LD80) of S. pneumoniae strain #6301 (ATCC, Manassas, VA) by intranasal route in a volume of 40 μl of Brain–Heart Infusion Broth (EMD, EMD Chemicals Inc. Gibbtown, NJ) or broth (e.g., sham infection) after anesthesia.
Determination of nanoparticle distribution in lungs
To visualize and confirm the distribution of NPs, we performed ex vivo imaging of mice lungs. Fluorescent NPs were prepared as explained in the nanoparticle construction section. Briefly, nile red stained NP-HKSP were suspended in autoclaved water at a concentration of 4 mg/ml and, 80 μl of NPs was administered via intranasal route as described above. Mice were killed on days 1 and 11 to visualize and confirm NP deposition the lungs based on preliminary evidence demonstrating NP retention (data not shown). Briefly, isolated lungs were perfused and washed with PBS before imaging. The isolated lungs were placed in a petri dish and imaged using Lumina XR imaging system (Caliper Life Sciences, CA). The background due to autofluorescence was collected and subtracted by the IVIS lumina XR imaging system software, which collects and subtracts autofluorescence while constructing the image, and the intensity was normalized to compare the fluorescence between days 1 and 11.
Lung leukocyte isolation
PBS-perfused lungs were harvested and finely minced after separation into single lobes and incubated in collagenase (Type II collagenase, Sigma-Aldrich, St. Louis, MO) digestion media containing 300 units/ml of DNase (Sigma-Aldrich) in RPMI 1640 culture media for 1 h and 30 min. After digestion, lungs were passed through a nylon mesh filter (LabPak, Depew, NY) into sterile 50-ml-conical tubes and washed twice in wash media (Hyclone, Logan, UT). Lung mononuclear cells were prepared by ficoll-hypaque (Lymphocyte M, Cedarlane, Laboratories, Ltd., Ontario, CA) centrifugation. Contaminating RBCs were removed using ACK lysis buffer as previously described (Kruisbeek 2001).
In vitro IFN-γ cytokine determination by total lung leukocytes
IFN-γ cytokine production was determined by sandwich ELISA method from lung supernatants cultured ex vivo for 4 days. All procedures were performed as described by the manufacturer. Briefly, flat-bottomed 96-well plates were coated with an optimal titration of capture antibody followed by overnight blocking using 10 % FBS in PBS to deter non-specific binding. After incubation of samples at 4 °C for 16 h, plates were incubated with biotin-conjugated detection antibody and streptavidin-HRP (horseradish peroxidase). Tetramethylbenzidine (TMB) peroxidase substrate solution (Rockland Immunochemicals, Inc. Gilbertsville, PA) was added to each well for colorimetric determination of concentration of each cytokine according to standard curve generated by reference concentration of cytokine at wavelength of 450 nm detected by colorimetric plate reader (Bioteck Instruments Inc. Winooski, VT). ELISA antibody set and recombinant cytokine for standard were purchased from R&D Systems (R&D Systems Inc. Minneapolis, MN) for recombinant IFN-γ.
Determination of bacterial colonization
To access bacterial growth, lung tissues were harvested and homogenized in sterile PBS. Tenfold dilutions of sample homogenates were plated in triplicate onto blood agar plates and incubated at 37 °C with 5 % CO2 overnight. CFUs were enumerated, and the results were expressed as log10 CFU as previously described (Kim et al. 2011).
Statistical analysis
Statistical analysis was performed using GraphPad Prism Version 5.0p (GraphPad Software, San Diego, USA). For multi-experimental group analysis, data were subjected to one-way ANOVA (analysis of variance). All data are expressed as mean ± standard error of mean (SEM). The two-tailed level of significance was set to p ≤ 0.05 for group differences.
Results
Particle size determination
The particle size is an important determinant of the fate of NPs in circulation. Smaller particles tend to mobilize in blood circulation due to rapid absorption from the site of deposition, whereas larger particles are retained at the site of administration and are cleared by reticuloendothelial system (RES). This property is particularly useful for our study due to the potential uptake of nanoparticles by antigen presenting cells (APCs), which are routinely found in the RES. The NP-HKSP prepared in this study was 234 ± 87.5 nm in size (Fig. 1).
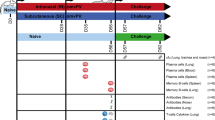
Deposition of NPs in lungs of mice following intranasal NP-HKSP administration
An initial study was performed to test the retention of NPs in lungs after intranasal administration. A comparison between the detection of empty NPs and NP-HKSP in the lungs of mice over the course of an 11-day incubation period demonstrated a significantly higher fluorescence intensity in the lungs of mice administered NP-HKSP by day 1. In contrast, minimal fluorescence was detected in the lungs of mice administered empty NPs. It has been previously suggested that 50:50 PLGA nanoparticles start degrading to lactic acid and glycolic acid after 10–14 days. As the nile red, used in this study to visualize nanoparticles, is complexed with PLGA, tracking these nanoparticles after that time will be redundant. After this time, the nanoparticle tracking may give false positive localization in other tissues based on distribution of free nile red dye. However, degradation of nanoparticles is dependent on several factors including type of drug, amount of drug and interaction of polymer-drug and nanoparticles with the host tissue. In our study, we found the antigen-encapsulated nanoparticles showed longer duration of retention, which could be due to the encapsulation of HKSP as well as interaction of nanoparticles with host tissues due to presence of immunogenic component, that is, HKSP. However, further studies need to be done to confirm this phenomenon. The fluorescence intensity was sustained in the lungs of mice administered NP-HKSP for at least 11 days compared to the lungs of mice administered empty NPs (Fig. 2).
HKSP encapsulation sustains NP retention in lungs of antigen. Naïve mice were administered preparations of fluorescently labeled empty NP or NP encapsulated with HKSP. Deposition of NP formulations was determined on day 1 and day 11 using Lumina XR imaging system. Images are representative of five animals per group
NP-HKSP immunization promotes potent antigen-specific IFN-γ cytokine recall response
Local cell-mediated immune responses are essential for optimal protective adaptive immunity against S. pneumoniae and other pulmonary infectious diseases (Lexau 2005). The current study determined how administration of NP-HKSP by intranasal route would induce an antigen-specific IFN-γ cytokine recall response by pulmonary lymphocytes. The results demonstrated a significant generation in antigen-induced IFN-γ cytokine production by lung lymphocytes isolated from mice immunized with NP-HKSP compared to the lungs of mice immunized with HKSP alone and compared to mice immunized with empty NPs. NPs encapsulated with antigen produced >150 pg of IFN-γ compared to less than 90 pg produced by antigen alone (Fig. 3).
HKSP-encapsulated NP immunization enhances antigen-specific IFN-γ cytokine production by pulmonary leukocytes. Lung leukocytes isolated from mice previously immunized with NP-Ag or NP-HKSP were stimulated in vitro to determine their ability to secrete IFN-γ in response to HKSP stimulation. Bars represent mean (n = 5) ± std. error. Asterisk * indicates significant differences (p ≤ 0.05) between experimental groups
NP-HKSP immunization improves protection against pulmonary S. pneumoniae infection
To test the efficacy of intranasal NP-based formulations as a potential strategy for vaccination against S. pneumonia infection, mice previously administered either NP-HKSP, HKSP alone or empty NPs were subsequently challenged with high doses of S. pneumoniae infection (LD80). As shown in Fig. 4, bacterial load in the lungs of mice previously administered NP-HKSP was 1,000-fold lower than compared to HKSP alone.
HKSP-encapsulated NP immunization enhances resistance against subsequent S. pneumoniae infection. Mice previously receiving intranasal administration of HKSP or NP-HKSP were challenged with S. pneumoniae. Bacterial colonization in the lungs was determined 1 day later. Bar graph represents mean (n = 5) ± std. error. Asterisk * indicates significant difference (p ≤ 0.05) between experimental groups
Discussion
Acquired resistance of pneumococcal bacterial strains/serotypes to available antibiotics and the ineffectiveness of current conjugate and polysaccharide vaccines warrant development of new modalities to boost self-immune defenses. Adjunctive therapies such as the use of nanoparticle delivery systems are being considered for their ability to manipulate immune responses against infectious disease (Gupta et al. 2007). The capability of these particles to slowly release its encapsulated proteins/peptides allows for more protection, making NPs a focus for vaccine development. NP technologies are emerging for their use in enhancing immunity, particularly against respiratory pathogens (Lexau 2005). In our current studies, we were able to establish that NP-HKSP immunization generates greater bacterial resistance compared to HKSP immunization. This is one of the first studies to identify NP technology as a promising advanced approach in prevention of S. pneumoniae infection, the major etiological pathogen of CAP.
Previous studies highlight the significance of nasal–pulmonary immunization in increasing the efficacy of vaccination against respiratory pathogens compared to the standard intramuscular route of immunization (Lexau 2005). However, controversy still remains regarding the robustness of immunization and the potential adverse inflammatory reactions that are commonly observed in response to antigen exposures across respiratory tissues (Arredouani et al. 2006; Kim et al. 2011). In the present study, we demonstrated that NPs as a potential vehicle for vaccines antigens could produce resistance against the targeted pathogen. The PLGA-based nanoparticles are biodegradable and non-immunogenic. In fact, it is one of the few US FDA approved biodegradable polymers used in nanomedicine field. Using an experimental model of S. pneumoniae infection, we demonstrated an increased protection in terms of reducing bacterial colonization along the respiratory tissues compared to immunization using heat-killed cell lysate antigenic preparations alone. Also worth noting was our inability to detect bacterial numbers in the systemic compartments of the spleen and blood of mice immunized with the NP-HKSP construct compared to immunization of HKSP alone (data not shown). This suggests that nasal delivery of antigen encapsulated in NPs not only enhances resistance across the local site of immunization, but also prevents the potential for bacterial dissemination. Thereby, potentially reducing the incidence of mortality risk associated commonly with S. pneumoniae infection observed in immune compromised individuals (Tan, 2012).
The necessity for improved vaccine strategies is in part associated with a lack in long-lasting antigen-specific acquired immune responses. As shown in Fig. 2, NP-encapsulated antigen were retained in lungs to a greater extent than empty NPs. While the precise mechanism to explain this finding is unknown, it does raise interest in defining antigen-particle interactions. One explanation could be that antigen encapsulation promotes the uptake by resident and circulating pulmonary macrophages, allowing for a prolonged local immune response. Future studies which address such intrapulmonary cellular interactions would provide important insight into future NP-based vaccine construction as immunomodulators. Recently, studies have documented inefficient generation of cell-mediated T cell responses associated with several conjugate and polysaccharide pneumococcal vaccines (Ballester et al. 2011). A hallmark of protective immunity is routinely associated with induction of IFN-γ cytokine responses as they promote the activation of macrophage responses, enabling intracellular bacterial killing (Bogart et al. 2004). In our current study, we examined the difference in antigen-mediated IFN-γ cytokine recall responses given NP-HKSP delivery system. As shown in Fig. 3, re-exposure of lung lymphocytes isolated from mice immunized with NP-HKSP construct produced a significantly stronger production of IFN-γ. On the basis of this finding, one might predict that encapsulation of target pneumococcal conjugate peptide and/or polysaccharide would be advantageous in compensating for the previously reported deficiency in adaptive/memory cell-mediated immunity (Haddadi et al. 2007; Ballester et al. 2011; Heuking and Borchard 2012; Tan 2012).
In summary, this study extends the potential advantages for the use of NPs in vaccine development against infectious disease including S. pneumonia infection, which is a major cause of mortality rates. The results provide evidence that nasal delivery of NP-HKSP produces effective immunity. Although our current findings demonstrate protective efficacy, consideration of potential adverse effects associated with this approach will increase its promise clinically. Moreover, because PLGA-based NPs and other formulations afford the capacity to coat and/or link substrates to its surface, it is expected that future studies whereby targeting of specific immune cells will be developed thereby advancing vaccine technologies. Such cells include macrophages and dendritic cells, which are important against pneumococcal and other infectious diseases.
References
Adam A, Wright A (2009) Mucosal perspectives in pneumococcal vaccine development: a meeting summary. Vaccine 28:2–6
Arredouani M, Yang Z, Ning Y et al. (2006) The scavenger receptor MARCO is required for lung defense against pneumococcal pneumonia and inhaled particles. J Exp Med 177
Ballester M, Nembrini C, Dhar N et al (2011) Nanoparticle conjugation and pulmonary delivery enhance the protective efficacy of Ag85B and CpG against tuberculosis. Vaccine 29(40):6959–6966
Bogart D, De Groot R, Hermans P (2004) Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4:144–154
Camacho AI, de Souza J, Sanchez-Gomez S et al (2011) Mucosal immunization with shigella flexneri outer membrane vesicles induced protection in mice. Vaccine 29(46):8222–8229
Cohen JM, Khandavilli S, Camberlein E et al (2011) Protective contributions against invasive Streptococcus pneumoniae pneumonia of antibody and Th17-cell responses to nasopharyngeal colonisation. Plos One. doi:10.1371/journal.pone.0025558
Derudas M, Brancale A, Naesens L et al (2010) Application of the phosphoramidate ProTide approach to the antiviral drug ribavirin. Bioorg Med Chem 18(7):2748–2755. doi:10.1016/j.bmc.2010.02.015
Fattal E, Pecquet S, Couvreur P, Andremont A (2002) Biodegradable microparticles for the mucosal delivery of antibacterial and dietary antigens. Int J Pharm 242(1–2):15–24
Gelperina S, Kisich K, Iseman M, Heifets L (2005) The potential advantages of nanoparticle drug delivery systems in chemotherapy of tuberculosis. Am J Respir Crit Care Med 172(12):1487–1490
Gupta P, Khatri K, Goyal A, Mishra K, Vyas SP (2007) M-cell targeted biodegradable PLGA nanoparticles for oral immunization against hepatitis B. J Drug Target 15:701–713
Gutierro I, Hernandez R, Igartua M, Gascon A, Pedraz J (2002) Size dependent immune response after subcutaneous, oral and intranasal administration of BSA loaded nanoparticles. Vaccine 21(1–2):67–77
Haddadi A, Elamanchili P, Lavasanifar A, Das S. (2007). Delivery of rapamycin by PLGA nanoparticles enhances its suppressive activity on dendritic cells. Wiley Periodicals
Handsand M, Lowman A (2002) Biodegradable nanoparticles for drug delivery and targeting. Curr Opin Solid State Mater Sci 6:319–327
Heuking S, Borchard G (2012) Toll-like receptor-7 agonist decoration enhances the adjuvanticity of chitosan-DNA nanoparticles. J Pharm Sci 101(3):1166–1177
Hvalbye BK, Aaberge IS, Lovik M et al (1999) Intranasal immunization with heat-inactivated streptococcus pneumoniae protects mice against systemic pneumococcal infection. Infect Immun 67(9):4320–4325
Keijzer C, Slutter B, van der Zee R et al (2011) PLGA, PLGA-TMC and TMC-TPP nanoparticles differentially modulate the outcome of nasal vaccination by inducing tolerance or enhancing humoral immunity. Plos One. doi:10.1371/journal.pone.0026684
Kim BJ, Kayembe K, Simecka JW et al (2011) Corticotropin-releasing hormone receptor-1 and 2 activity produces divergent resistance against stress-induced pulmonary streptococcus pneumoniae infection. J Neuroimmunol 237(1–2):57–65. doi:10.1016/j.jneuroim.2011.06.016
Kruisbeek AM (2001) Isolation of mouse mononuclear cells. In: Coligan JE et al (eds) Current protocols in immunology chapter 3, unit 3.1. doi:10.1002/0471142735.im0301s39
Lexau C (2005) Changing epidemiology of invasive pneumococcal disease among older adults in the era of pediatric pneumococcal conjugate vaccine. JAMA 294:2043–2051
Lindell DM, Morris SB, White MP et al (2011) A novel inactivated intranasal respiratory syncytial virus vaccine promotes viral clearance without Th2 associated vaccine-enhanced disease. Plos One. doi:10.1371/journal.pone.0021823
Marriott H, Hellewell P, Cross S et al (2006) Decreased alveolar macrophage apoptosis is associated with increased pulmonary inflammation in a murine model of pneumococcal pneumonia. J Immunol 177(9):6480–6488
Mukerjee A, Vishwanatha JK (2009) Formulation, characterization and evaluation of curcumin-loaded PLGA nanospheres for cancer therapy. Anticancer Res 29(10):3867–3875
Ranjan AP, Zeglam K, Mukerjee A, Thamake S, Vishwanatha JK (2011) A sustained release formulation of chitosan modified PLCL: poloxamer blend nanoparticles loaded with optical agent for animal imaging. Nanotechnology. doi:10.1088/0957-4484/22/29/295104
Stano A, van der Vlies AJ, Martino MM et al (2010) PPS nanoparticles as versatile delivery system to induce systemic and broad mucosal immunity after intranasal administration. Vaccine 29(4):804–812
Tan S (2012) Phenotype and function of conventional dendritic cells are not compromised in aged mice. Immunol Cell Biol. doi:10.1038/icb.2011.104
Thamake SI, Raut SL, Ranjan AP, Gryczynski Z, Vishwanatha JK (2011) Surface functionalization of PLGA nanoparticles by non-covalent insertion of a homo-bifunctional spacer for active targeting in cancer therapy. Nanotechnology. doi:10.1088/0957-4484/22/3/035101
Acknowledgments
We would like to acknowledge Lindsey Kuehm, MS, Rutika Kokate, M.S, C.R.M and Xiangle Sun, Ph.D., for assistance in the execution of experimental techniques associated with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mott, B., Thamake, S., Vishwanatha, J. et al. Intranasal delivery of nanoparticle-based vaccine increases protection against S. pneumoniae . J Nanopart Res 15, 1646 (2013). https://doi.org/10.1007/s11051-013-1646-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-013-1646-x