Abstract
A 34-year-old female patient presented with hair loss due to black dot tinea capitis caused by Trichophyton tonsurans for 6 months. Hair loss progressed to painful swelling for 2 months due to kerion Celsi which may be associated with treatment like topical minoxidil, antibiotic and corticosteroid previously. The patient was treated with oral Itraconazole initially without success but cured by Terbinafine eventually. It’s very interesting that the patient caught kerion celsi secondary to a four-month history of hair loss due to black dot tinea capitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
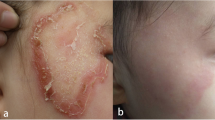
A 34-year-old female presented with a 6-month history of hair loss (Fig. 1a) and a 2-month history of painful swelling of the scalp. Her condition had been treated as androgenic alopecia, bacterial folliculitis and seborrheic dermatitis with topical minoxidil, antibiotic and corticosteroid previously for over 2 months, but without improvement. She reported a normal menstrual cycle and a recent haircut at a barbershop prior to hair loss. Additionally, she denied any direct contact with pets and history of tinea of herself and her family members. Physical examination revealed erythematous, boggy, and purulent plaques with abscess formation, greasy scabs and hair loss on her occiput (Fig. 1b). The lesion was tender and the hair pull test was positive. Under dermoscopy, broken hairs, black dots, pustules and scales were observed (Fig. 2a). Direct microscopy of broken hair revealed arthroconidia and hyphae within hair shafts (Fig. 3a). Skin biopsy of scalp lesion revealed arthroconidia within hair shafts (Fig. 3b). Flat, powdery, reddish-brown colonies were observed 2 weeks after incubation on Sabouraud dextrose agar medium (Fig. 4a). Microscopic examination of the smear of colony revealed many inflated, pear-shaped microconidia, borne on matchstick-like stalks (Fig. 4b). This was identified by DNA sequencing of the D1/D2 region of the large subunit of the 28S ribosomal RNA gene as Trichophyton tonsurans (GenBank Accession No. ON614136).
The patient was treated with oral Itraconazole at 200 mg twice a day and prednisolone at 20 mg daily for 2 weeks. Subcutaneous abscesses subsided and the pain was relieved gradually, but her hair loss developed from occiput to vertex. On her vertex, broken hairs, black dots, comma hairs, corkscrew hairs and pustules were seen under dermoscopy at this time (Fig. 2b). Itraconazole was replaced by Terbinafine at 250 mg daily and the lesion resolved after 10 weeks. (Fig. 1c). Subsequent fungal direct microscopy and culturing results were both negative for three times.
Tinea capitis mainly affects preadolescent children. In China, only 7.7% of patients with tinea capitis are adults. Kerion celsi is a severe inflammatory condition of the tinea capitis and is usually caused by zoophilic or geophilic pathogens. Among these organisms, Microsporum canis is the most common cause in China. Adult kerion celsi caused by Trichophyton tonsurans is exceptionally rare. Trichophyton tonsurans is an anthropophilic dermatophyte which usually causes asymptomatic but indolent infections in adults. Our patient may be infected from other people during haircut at a barbershop. Interestingly, the patient was presented with kerion celsi secondary to a 4-month history of black dot tinea capitis. It is possible that her treatment with topical minoxidil, antibiotic and corticosteroid promoted the development from a black dot capitis to kerion celsi. Tinea capitis should be considered in an adult with hair loss, comma hairs and corkscrew hairs under dermoscopy are helpful to differentiate it from androgenic alopecia and seborrheic dermatitis. Current evidence supports that terbinafine is an effective first-line choice for tinea capitis infected with Trichophyton species while itraconazole and fluconazole are alternative but not optimal choices.
Acknowledgements
Not applicable.
Funding
This work was supported by the Medical Science and Technology Project from Guangzhou Institute of Dermatology (No. 202102).
Author information
Authors and Affiliations
Contributions
QY collected and verified patient information, participated in the treatment, and was a major contributor in writing the manuscript. QL and X-Z contributed to data collection of patients. YL and YL diagnosed and treated the patient and participated in revising the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing of interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ye, Qr., Luo, Yw., Zhou, X. et al. Adult Kerion Celsi Caused by Trichophyton tonsurans Secondary to Black Dot Tinea Capitis. Mycopathologia 188, 589–591 (2023). https://doi.org/10.1007/s11046-022-00701-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00701-1