Abstract
Background
Candida auris is an emerging pathogen associated with outbreaks in clinical settings. Isolates of the pathogen have been geographically clustered into four clades with high intra-clade clonality. Pathogenicity varies among the clades, highlighting the importance of understanding these differences.
Objectives
To examine the physiological and biochemical properties of each clade of C. auris to improve our understanding of the fungus.
Methods
Optimal growth temperatures of four strains from three clades, East Asia, South Asia and South Africa, were explored. Moreover, assimilation and antifungal susceptibility properties of 22 C. auris strains from the three clades were studied.
Results
The optimal growth temperatures of all strains were 35–37 °C. Assimilation testing demonstrated that the commercial API ID 32 C system can be used to reliably identify C. auris based on the biochemical properties of the yeast. Notably, C. auris can be uniquely differentiated from commonly clinical fungi by its ability to assimilate raffinose and inability to utilize D-xylose, suggesting a useful simple screening tool. The antifungal susceptibility results revealed that all strains are resistant against fluconazole (minimal inhibitory concentration (MIC) 4 to > 64 µg/mL) and miconazole (MIC 8 to > 16 µg/mL), with strains from the Japanese lineage showing relatively lower MIC values (1–4 µg/mL). Conversely, itraconazole, voriconazole, amphotericin B, micafungin and caspofungin were active against most of the tested strains. On the clade level, East Asian strains generally showed lower MICs against azoles comparing to the other clades, while they displayed MICs against flucytosine higher than those of strains from South Africa and South Asia clades.
Conclusion
Our data suggest a simple identification approach of C. auris based on its physiological and biochemical properties and highlight aspects of C. auris population from various clades.

Similar content being viewed by others
References
Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53:41–44.
Chowdhary A, Sharma C, Duggal S, Agarwal K, Prakash A, Kumar Singh PK, Jain S, Kathuria S, Randhawa HS, Hagen F, Meis JF. New clonal strain of Candida auris, Delhi, India. Emerg Infect Dis. 2013;19:1670–3.
Sarma S, Kumar N, Sharma S, Govil D, Ali T, Mehta Y, Rattan A. Candidemia caused by amphotericin B and fluconazole resistant Candida auris. Indian J Med Microbiol. 2013;31:90–1.
Chowdhary A, Anil Kumar V, Sharma C, Prakash A, Agarwal K, Babu R, Dinesh KR, Karim S, Singh SK, Hagen F, Meis JF. Multidrug-resistant endemic clonal strain of Candida auris in India. Eur J Clin Microbiol Infect Dis. 2014;33:919–26.
Magobo RE, Corcoran C, Seetharam S, Govender NP. Candida auris-associated candidemia. South Africa Emerg Infect Dis. 2014;20:1250–1.
Calvo B, Melo AS, Perozo-Mena A, Hernandez M, Francisco EC, Hagen F, Meis JF, Colombo AL. First report of Candida auris in America: clinical and microbiological aspects of 18 episodes of candidemia. J Infect. 2016;73:369–74.
Borman AM, Szekely A, Johnson EM. Comparative pathogenicity of United Kingdom isolates of the emerging pathogen Candida auris and other key pathogenic Candida species. mSphere. 2016;1:e00189–16.
Borman AM, Szekely A, Johnson EM. Isolates of the emerging pathogen Candida auris present in the UK have several geographic origins. Med Mycol. 2017;55:563–7.
Schelenz S, Hagen F, Rhodes JL, Abdolrasouli A, Chowdhary A, Hall A, Ryan L, Shackleton J, Trimlett R, Meis JF, Armstrong-James D, Fisher MC. First hospital outbreak of the globally emerging Candida auris in a European hospital. Antimicrob Resist Infect Control. 2016;5:35.
Govender NP, Magobo RE, Mpembe R, Mhlanga M, Matlapeng P, Corcoran C, Govind C, Lowman W, Senekal M, Thomas J. Candida auris in South Africa, 2012–2016. Emerg Infect Dis. 2018;24:2036–40.
Tsay S, Kallen A, Jackson BR, Chiller TM, Vallabhaneni S. Approach to the investigation and management of patients with Candida auris, an emerging multidrug-resistant yeast. Clin Infect Dis. 2018;66:306–11.
Welsh RM, Bentz ML, Shams A, Houston H, Lyons A, Rose LJ, Litvintseva AP. Survival, persistence, and isolation of the emerging multidrug-resistant pathogenic yeast Candida auris on a plastic health care surface. J Clin Microbiol. 2017;55:2996–3005.
Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, Colombo AL, Calvo B, Cuomo CA, Desjardins CA, Berkow EL, Castanheira M, Magobo RE, Jabeen K, Asghar RJ, Meis JF, Jackson B, Chiller T, Litvintseva AP. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017;64:134–40.
Chow NA, de Groot T, Badali H, Abastabar M, Chiller TM, Meis JF. Potential fifth clade of Candida auris, Iran, 2018. Emerg Infect Dis. 2019;25:1780–1.
Kwon YJ, Shin JH, Byun SA, Choi MJ, Won EJ, Lee D, Lee SY, Chun S, Lee JH, Choi HJ, Kee SJ, Kim SH, Shin MG. Candida auris clinical isolates from South Korea: identification, antifungal susceptibility, and genotyping. J Clin Microbiol. 2019;57:e01624-e1718.
Lee WG, Shin JH, Uh Y, Kang MG, Kim SH, Park KH, Jang HC. First three reported cases of nosocomial fungemia caused by Candida auris. J Clin Microbiol. 2011;49:3139–42.
Mizusawa M, Miller H, Green R, Lee R, Durante M, Perkins R, Hewitt C, Simner PJ, Carroll KC, Hayden RT, Zhang SX. Can multidrug-resistant Candida auris be reliably identified in clinical microbiology laboratories? J Clin Microbiol. 2017;55:638–40.
Kathuria S, Singh PK, Sharma C, Prakash A, Masih A, Kumar A, Meis JF, Chowdhary A. Multidrug-resistant Candida auris misidentified as Candida haemulonii: characterization by matrix-assisted laser desorption ionization–time of flight mass spectrometry and DNA sequencing and its antifungal susceptibility profile variability by Vitek 2, CLSI broth microdilution, and Etest method. J Clin Microbiol. 2015;53:1823–30.
Kordalewska M, Zhao Y, Lockhart SR, Chowdhary A, Berrio I, Perlin DS. Rapid and accurate molecular identification of the emerging multidrug-resistant pathogen Candida auris. J Clin Microbiol. 2017;55:2445–52.
Leach L, Zhu Y, Chaturvedi S. Development and validation of a real-time PCR assay for rapid detection of Candida auris from surveillance samples. J Clin Microbiol. 2018;56:e01223-e1317.
Yamamoto M, Alshahni MM, Tamura T, Satoh K, Iguchi S, Kikuchi K, Mimaki M, Makimura K. Rapid detection of Candida auris based on loop-mediated isothermal amplification (LAMP). J Clin Microbiol. 2018;56:e00591-e618.
Vatanshenassan M, Boekhout T, Mauder N, Robert V, Maier T, Meis JF, Berman J, Then E, Kostrzewa M, Hagen F. Evaluation of microsatellite typing, ITS sequencing, AFLP fingerprinting, MALDI-TOF MS, and Fourier-transform infrared spectroscopy analysis of Candida auris. J Fungi (Basel). 2020;6:146.
Forgács L, Borman AM, Prépost E, Tóth Z, Kardos G, Kovács R, Szekely A, Nagy F, Kovacs I, Majoros L. Comparison of in vivo pathogenicity of four Candida auris clades in a neutropenic bloodstream infection murine model. Emerg Microbes Infect. 2020;9:1160–9.
APIWEBTM. https://apiweb.biomerieux.com/login. Accessed 1 June 2020.
Lapage SP, Bascomb S, Willcox WR, Curtis MA. Identification of bacteria by computer: general aspects and perspectives. J Gen Microbiol. 1973;77:273–90.
Centers for Disease Control and Prevention. Identification of Candida auris. https://www.cdc.gov/fungal/candida-auris/identification.html. Accessed 24 June 2020.
Cendejas-Bueno E, Kolecka A, Alastruey-Izquierdo A, Theelen B, Groenewald M, Kostrzewa M, Cuenca-Estrella M, Gómez-López A, Boekhout T. Reclassification of the Candida haemulonii complex as Candida haemulonii (C. haemulonii group I), C. duobushaemulonii sp. nov. (C. haemulonii group II), and C. haemulonii var. vulnera var. nov.: three multiresistant human pathogenic yeasts. J Clin Microbiol. 2012;50:3641–51.
Rhodes J, Abdolrasouli A, Farrer RA, Cuomo CA, Aanensen DM, Armstrong-James D, Fisher MC, Schelenz S. Genomic epidemiology of the UK outbreak of the emerging human fungal pathogen Candida auris. Emerg Microbes Infect. 2018;7:1–12.
Eyre DW, Sheppard AE, Madder H, Moir I, Moroney R, Quan TP, Griffiths D, George S, Butcher L, Morgan M, Newnham R, Sunderland M, Clarke T, Foster D, Hoffman P, Borman AM, Johnson EM, Moore G, Brown CS, Walker AS, Peto TEA, Crook DW, Jeffery KJM. A Candida auris outbreak and its control in an intensive care setting. N Engl J Med. 2018;379:1322–31.
Szekely A, Borman AM, Johnson EM. Candida auris isolates of the Southern Asian and South African lineages exhibit different phenotypic and antifungal susceptibility profiles In Vitro. J Clin Microbiol. 2019;57:e02055-e2118.
Köhler JR, Hube B, Puccia R, Casadevall A, Perfect JR. Fungi that infect humans. Microbiol Spectr. 2017;5(3).
Ghosh AK, Paul S, Sood P, Rudramurthy SM, Rajbanshi A, Jillwin TJ, Chakrabarti A. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry for the rapid identification of yeasts causing bloodstream infections. Clin Microbiol Infect. 2015;21:372–8.
Girard V, Mailler S, Chetry M, Vidal C, Durand G, van Belkum A, Colombo AL, Hagen F, Meis JF, Chowdhary A. Identification and typing of the emerging pathogen Candida auris by matrix-assisted laser desorption ionisation time of flight mass spectrometry. Mycoses. 2016;59:535–8.
Wickerhan LJ, Burton KA. Carbon assimilation tests for the classification of yeasts. J Bacteriol. 1948;56:363–71.
Bowman PI, Ahearn DG. Evaluation of commercial systems for the identification of clinical yeast isolates. J Clin Microbiol. 1976;4:49–53.
Bergan T, Hollum AB, Vangdal M. Evaluation of four commercial biochemical test systems for identification of yeasts. Eur J Clin Microbiol. 1982;1:217–22.
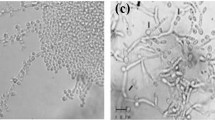
Larkin E, Hager C, Chandra J, Mukherjee PK, Retuerto M, Salem I, Long L, Isham N, Kovanda L, Borroto-Esoda K, Wring S, Angulo D, Ghannoum M. The emerging pathogen Candida auris: growth phenotype, virulence factors, activity of antifungals, and effect of SCY-078, a novel glucan synthesis inhibitor, on growth morphology and biofilm formation. Antimicrob Agents Chemother. 2017;61:e02396-e2416.
Wanger A, Mills K, Nelson PW, Rex JH. Comparison of Etest and National Committee for Clinical Laboratory Standards broth macrodilution method for antifungal susceptibility testing: enhanced ability to detect amphotericin B-resistant Candida isolates. Antimicrob Agents Chemother. 1995;39:2520–2.
Flowers SA, Colon B, Whaley SG, Schuler MA, Rogers PD. Contribution of clinically derived mutations in ERG11 to azole resistance in Candida albicans. Antimicrob Agents Chemother. 2015;59:450–60.
Yurkov AM, Kachalkin AV, Daniel HM, Groenewald M, Libkind D, de Garcia V, Zalar P, Gouliamova DE, Boekhout T, Begerow D. Two yeast species Cystobasidium psychroaquaticum f.a. sp. nov. and Cystobasidium rietchieii f.a. sp. nov. isolated from natural environments, and the transfer of Rhodotorula minuta clade members to the genus Cystobasidium. Antonie Van Leeuwenhoek. 2015;107:173–85.
Acknowledgments
The authors express their sincere appreciation for those who have provided some of the fungal strains.
Funding
This work was supported in part by the Emerging/Re-emerging Infectious Disease Project of the Japan Agency for Medical Research and Development, AMED (JP20fk108094).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AMR Mycosis Control Research in the Environment of Treatment and Education for Physically and Mentally Handicapped Persons is an endowed department supported with an unrestricted grant from the Social Welfare Corporation Hirakata Ryoikuen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Hamid Badali.
Supplementary Information
Below is the link to the electronic supplementary material.
11046_2020_526_MOESM1_ESM.tiff
Growth curves of four strains. The strains were inoculated into PDB at a concentration of 104 CFU/mL and cultured at different temperatures. The absorbance was measured at 660 nm once every 1–3 h up to 17 h after culturing. The results were generated from three independent experiments and represent the average growth rate of the four strains
Supplementary file1 (TIFF 5.77 MB)
Rights and permissions
About this article
Cite this article
Du, M., Hu, W., Tamura, T. et al. Investigation of the Physiological, Biochemical and Antifungal Susceptibility Properties of Candida auris. Mycopathologia 186, 189–198 (2021). https://doi.org/10.1007/s11046-020-00526-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-020-00526-w