Abstract
The incidence of head and neck cancer (HNC), constituting approximately one in ten cancer cases worldwide, affects approximately 644,000 individuals annually. Managing this complex disease involves various treatment modalities such as systemic therapy, radiation, and surgery, particularly for patients with locally advanced disease. HNC treatment necessitates a multidisciplinary approach due to alterations in patients’ genomes affecting their functionality. Predominantly, squamous cell carcinomas (SCCs), the majority of HNCs, arise from the upper aerodigestive tract epithelium. The epidemiology, staging, diagnosis, and management techniques of head and neck squamous cell carcinoma (HNSCC), encompassing clinical, image-based, histopathological and molecular profiling, have been extensively reviewed. Lymph node metastasis (LNM) is a well-known predictive factor for HNSCC that initiates metastasis and significantly impacts HNSCC prognosis. Distant metastasis (DM) in HNSCC has been correlated to aberrant expression of cancer cell-derived cytokines and growth factors triggering abnormal activation of several signaling pathways that boost cancer cell aggressiveness. Recent advances in genetic profiling, understanding tumor microenvironment, oligometastatic disease, and immunotherapy have revolutionized treatment strategies and disease control. Future research may leverage genomics and proteomics to identify biomarkers aiding individualized HNSCC treatment. Understanding the molecular basis, genetic landscape, atypical signaling pathways, and tumor microenvironment have enhanced the comprehension of HNSCC molecular etiology. This critical review sheds light on regional and distant metastases in HNSCC, presenting major clinical and laboratory features, predictive biomarkers, and available therapeutic approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The broad term head and neck cancer (HNC) describes cancers that manifest in the oral cavity, pharynx, larynx, thyroid, paranasal sinuses, nasal cavity and salivary glands. Two-thirds of the estimated 644,000 new cases of HNC each year are diagnosed in developing countries. About 350,000 estimated cancer deaths are HNC-related, while HNC is the sixth most prevalent type of cancer [1]. Head and neck squamous cell carcinoma (HNSCC), accounting for approximately 90% of all HNCs, mainly derived from the mucosal epithelium in the oral cavity, pharynx and larynx [2].
Approximately 10% of patients usually appear with a late-stage HNSCC that typically involves local and regional lymph nodes metastasis (LNM) which then could progress to distant metastasis (DM) [3]. The entire aerodigestive tract may be affected by secondary tumors, which can develop at 3–5% annual rates [4]. Patients with locally advanced HNSCC are at least 50% more likely to experience loco-regional relapses or DM, which are typically identified within the first two years of treatment [5]. Either another mucosal site or the location of a previously recognized dysplastic lesion, the reported risk of invasive cancer varies widely between 10 and 40% and is dependent on the histology and duration of follow-up [6]. Depending on the site of the primary tumor, there are different chances of developing a new, secondary tumor, however, the risk is higher for individuals who use tobacco and alcohol [7] (Fig. 1). One of the key elements determining HNSCC prognosis is the condition of the regional neck lymph nodes. Notably, even one positive metastatic lymph node can reduce the chances of survival by as much as 50% [8]. According to studies, 15% of patients with HNSCC who were N0 (negative for neck lymph nodes) during therapy but still were diagnosed HNSCC-positive have been found to have clinically evident DM [9]. Tumor diffusion occurs either by hematogenous spread to distant organs or by lymphatic spread to lymph nodes at local, regional or distant sites. In contrast to other histological types of HNC (e.g. adenoid cystic carcinoma), which can manifest late DM even more than 20 years after diagnosis, HNSCC presents DM shortly after treatment. In a study by Duprez et al. [10], 70% of the patients with DM were diagnosed within 1 year after treatment and 89% within 2 years, the lungs being the most predominant site. The risk of DM is intricately linked to various factors, including mainly the tumor site and size, the nodal status, and the histological grade. Moreover, lymph node extracapsular spread, locoregional residual disease and human papillomavirus (HPV) status, are all associated with an increased likelihood of DM in univariate and multivariate analysis [11]. These factors collectively underscore the complexity of metastatic progression in HNSCC and emphasize the importance of comprehensive risk assessment and management strategies.
Development of carcinogen-associated HNSCC. A list of etiological risk factors, such as exposure to carcinogens, genetic mutations, and epigenetic aberrations that may cause head and neck squamous cell carcinoma (HNSCC). Detoxification and/or accurate DNA repair sustain homeostasis. However, specific and critical aspects (shown in the right bottom panel) may contribute to genomic instability and development of HNSCC. Created with BioRender.com
LNM and DM of a primary tumor can be detected by several methods. Biomarker detection in liquid biopsy is the most promising non-invasive technique for monitoring metastatic spread during therapeutic response in HNSCC [12, 13]. Moreover, tumor biomarkers can be used in research to evaluate the cellular lineage and histogenic origin of various and distinct neoplasms and produce successful results [14]. However, to comprehend the metastatic process, a number of combined strategies have been used. Combining protein profiling and gene expression studies along with various systems biology approaches enabled the identification of pathways that play a role in the invasive mechanisms of HNSCC [15]. Histopathological image features and machine-learning algorithms can be used to predict somatic mutations, transcription and methylation subtypes, and prognosis of HNSCC [16]. Similarly, computed tomography and magnetic resonance imaging findings have demonstrated unique pathological and clinical characteristics according to HPV-status in HNSCC [17].
In this article we critically present and discuss on the current insights on clinical, imaging and pathological characteristics of HNSCC during LNM and DM. Moreover, we focus on the mechanistic insights on HNSCC progression and the fundamental role of molecular targeting in establishing effective therapeutic approaches.
Metastatic events and signaling pathways in HNSCC
There are numerous processes involved in metastasis. Major steps include tumor cell invasion into nearby tissue, endothelial transport of cancer cells into vessels, survival in the circulatory system, evasion of the immune system and establishment of a microenvironment conducive to colonization in distant organs [18]. The coordination of all these events is crucial to prevent the complete failure of this complex process. The preference of cancer cells for colonization in particular organs is a critical consideration [19]. In models of spontaneous metastasis, cancer cells proliferate in the circulatory system to maintain viability, are released, and form colonies near secondary sites. However, they often fail to replicate normal metastasis and instead develop niche pre-metastasis from specific growth of the primary tumor [20, 21]. Tumor budding is recognized as the initial histopathological event in metastasis and plays a pivotal role in its onset [22]. The significant correlation between high-grade budding and metastasis in various carcinomas, including different subsites of HNSCC, suggests the migratory ability of tumor buds [23, 24]. Aldehyde dehydrogenase 1 (ALDH1), a characteristic biomarker of cancer stem cells, is highly expressed in tumor budding cells in nasopharyngeal carcinoma. This observation raises the possibility that these budding cells possess the invasive and metastatic properties of cancer stem cells [25].
Several interlinked signaling cascades are often mediating cell behavior and prognosis in HNSCC [26]. These mainly involve cytokine signaling including the activation of TGF-βR (Fig. 2) and CXCR4 (Fig. 3), which mediate the functions of several extracellular matrix (ECM) regulators that enforce intracellular signaling enhancing cell migration and invasion leading to metastasis [27]. The TGF-βR pathway plays a vital role in the spread of HNSCC. In HNSCC, aberrant TGF-β signaling is common and fuels the tumor’s growth [28]. TGF-β can trigger a process called epithelial-mesenchymal transition (EMT), boosting the aggressive phenotype of cancer cells that move and invade more easily, thus facilitating the initiation of metastasis [29]. Although the concept of EMT is widely debated and its validity is not yet confirmed [30], it is still regarded as an important and advanced theory for the study of cancer metastases. Moreover, TGF-β signaling controls the activity of genes like E-cadherin and vimentin that are involved in cell adhesion, movement and invasion, and generates a group of cancer cells that are highly mobile and can spread rapidly to other parts of the body [31, 32].
Pathways in HNSCC cells involving growth factor receptors like TGFβ causing cell migration and invasion leading to metastasis. MKKs consist enzymes that phosphorylate and activate MAPKs, serving as intermediaries in cellular signalling pathways. MAPKs are protein kinases that regulate gene expression and cellular processes in response to extracellular stimuli through phosphorylation of target proteins. MAP3K7 is a protein kinase that activates downstream MKKs in the MAPK signalling pathway, involved in diverse cellular processes such as immune responses and inflammation. Abbreviations: TGFβ, transforming growth factor beta; TGFBR, transforming growth factor beta receptor; RAS, rat sarcoma virus; RAF, rapidly accelerated fibrosarcoma; MEK, mitogen-activated protein kinase kinase; MKK, MAP kinase kinase; MAP, mitogen-activated protein kinase; MAP3K7, mitogen-activated protein kinase kinase kinase 7; NF-κΒ, nuclear factor kappa B; PI3K, phosphoinositide 3 kinase; AKT, protein kinase B; mTOR, mammalian target of rapamycin; EMT, epithelial-to-mesenchymal transition; TFs, transcription factors; MMP, matrix metalloproteinase; DNA, deoxyribonucleic acid. Created with BioRender.com.
CXCR4 plays an important role in the spread of HNSCC. CXCR4 is a receptor that cooperates with CXCL12 to boost cancer cell motility, invasion and metastasis. Recent studies shed light on how this pathway works in HNSCC spreading. There was a significant increase in CXCR4 mRNA levels in highly metastatic cells compared to cells with less aggressive characteristics. In HNSCC, CXCR4 was linked to EMT markers, indicating that CXCR4 levels correlate closely with aggressive tumors, poor prognoses and disease spread. Additionally, the communication between HNSCC cells and lymphatic endothelial cells (LECs) was seen to promote tumor spread through CXCL5-CXCR2 signaling [33,34,35].
Pathways in HNSCC cells involving growth factor receptors like CXCR4 causing cell migration and invasion leading to metastasis. Abbreviations: CXCR4, C-X-C chemokine receptor type 4; PI3K, phosphoinositide 3 kinase; AKT, protein kinase B; MEK, mitogen-activated protein kinase kinase; ERK, extracellular signal-regulated kinase; IKKα/β, IκB Kinase α/β; NF-κB, nuclear factor kappa B; MMP-9, matrix metalloproteinase 9. Created with BioRender.com.
In HNSCC, multiple pathways activate the epidermal growth factor receptor (EGFR) (Fig. 4). When EGFR interacts with epidermal growth factor (EGF), heparin-binding EGF (HB-EGF), amphiregulin, transforming growth factor alpha (TGFα), epiregulin, and betacellulin, which are ligands of the HER family, a signal transduction cascade is initiated, activating numerous pathways simultaneously [36]. EGFR’s significance in various human tumors, particularly HNSCC, is crucial [37]. In these tumors, EGFR often becomes hyperactive, leading to downstream chaos, particularly in the PI3K/Akt/mTOR pathway. This disruption fuels the progression of HNSCC, promoting angiogenesis, tumor growth, invasion and metastasis [38,39,40]. EGFR serves as the primary driver of invasion in HNSCC. Activation of EGFR by triggers like EGF initiates a cascade of events that drive further invasion. This activation triggers pathways such as MAPK and PI3K, essential for cell growth, survival and motility. In HNSCC, EGFR promotes invasion through various mechanisms: enhancing cellular mobility by altering cell morphology, increasing MMP-9 to break down barriers, inducing an invasion-ready state (EGFR-EMT), and cooperating with pathways like c-MET/HGF for cell growth, invasion, and angiogenesis [41,42,43].
EGFR-evoked signaling pathways related to HNSCC invasion to adjacent tissues. Abbreviations: EGFR, epidermal growth factor receptor; RAS, rat sarcoma virus; RAF, rapidly accelerated fibrosarcoma; MEK, mitogen-activated protein kinase kinase; ERK, extracellular signal-regulated kinase; PI3K, phosphoinositide 3 kinase; AKT, protein kinase B; mTOR, mammalian target of rapamycin. Created with BioRender.com.
Certain signaling pathways, such as PD-1/PD-L1 and STAT3, have an impact in HNSCC associated with immune evasion, which is a fundamental mechanism in cancer evolution. Programmed death receptor-1 (PD-1) and its ligand PD-L1, play a vital role in immune evasion by HNSCC. A PD-1 - PD-L1 interaction results in T cells exhaustion and inhibition of the anti-tumor immune response. This pathway is often upregulated in HNSCC, permitting tumor cells to evade immune surveillance [44]. Signal Transducer and Activator of Transcription 3 (STAT3) is a transcription factor that is commonly activated in HNSCC. By upregulating the expression of immunosuppressive molecules such as PD-L1, TGF-β1, VEGF, IL-6 and IL-10, STAT3 promotes tumor growth and immune evasion [45, 46]. Moreover, STAT3 activation in tumor-associated immune cells leads to anti-tumor immune suppression [47].
Finally, the PI3K/AKT/mTOR pathway is also significant for immune evasion in HNSCC by promoting tumor cell survival, inducing immunosuppressive factors, inhibiting antigen presentation and amplifying regulatory T cell function [48, 49].
Clinical factors associated with the metastatic potential of HNSCC and the role of imaging techniques
During diagnosis, 2/3 of HNSCC nurture micro-metastasis and present local invasion. Despite advancements in cancer detection and treatment, residual signs of disseminated disease may persist, leading to tumor invasion and loco-regional or distant metastases, even after effective treatment of the primary tumor. Micro-metastases, which are multicellular secondary cancer cell clusters, often evade detection in clinical diagnostic scans and can remain active, representing a potential manifestation of this residual disease component [50].
Lymph node metastasis (LNM) is a well-known and clinically recognized prognostic factor for HNSCC and other solid malignancies [51]. In HNSCC regional LNM indicates aggressive tumor biology and acts as a location of subsequent DM [8, 52]. The metastatic spread of HNSCC to neck lymph nodes has been mainly documented at levels III and IV, sometimes with no discernible engagement at levels I and II. In addition, 5% of patients demonstrated “peppering” at multiple lymph node levels without any obvious macroscopic involvement [53]. About 10% of individuals with HNSCC may develop DM with lungs, bones and mediastinal lymph nodes being the most frequent and typical sites [54,55,56]. DM in HNSCC represent a complex and critical aspect of disease progression, which significantly impact survival and treatment options.
SCC was the most frequent histological type discovered in metastatic neck lymph nodes, according to all research conducted on the prevalence of metastatic disease in HNC patients. From HNC primary sites, SCC quickly proliferate [57]. The normal anatomical lymphatic pathways either delay or completely ignore the order in which nodal metastasis should develop. Clinical observations revealed that the involvement of the metastasis of various regions typically advances from the higher to the lower region of the neck in HNSCC, and this pattern can also be recognised in normal lymphography. In patients enduring HNSCC and non-HNSCC, the hazy movement of tumour cells escaping from typical lymph nodes that drain to other lymph nodes has been recorded or well documented [58].
The tumor-node-metastasis (TNM) staging, which is currently the most accurate indication of a patient’s prognosis and the elements that define the stage of disease progression as well as the course of treatment, takes into account both the main tumour dimension and LNM status [59]. Due to the low prevalence of DM at presentation, it is crucial to establish criteria for choosing people whose DM status should be assessed [60]. Greater nodal stage, involvement of the lower neck lymph nodes, and frequency of lymph node metastases are all clearly associated with the development of DM [61,62,63,64]. People at risk for DM and those in whom it is important to rule out such metastases typically undergo laboratory tests, computed tomography (CT) of the lungs, bone scintigraphy, and ultrasound (US) or CT of the liver due to the fact that the lungs, bone, and liver are the most prevalent locations of DM [65].
Patients with HNSCC represent almost two thirds of those with advanced cancer, as opposed to only a third of those with early-stage disease [66]. The likelihood of neighboring lymph nodes being infected by locally invasive HNSCCs is higher than the likelihood of hematogenous dissemination [67]. Additionally, the microenvironment of the primary site may have a different tumour ecology and phenotype than the metastatic LNs [68, 69]. More significantly, it has been revealed that tumor cells respond to treatment differently in various microenvironments [70, 71]. Therefore, growing evidence suggests that in order to determine the best course of treatment and enhance prognosis, the evaluation of cancer patients should be enhanced based on the underlying tumour and metastatic microenvironment. Surface measures alone have historically been used to stage primary tumors of the oral cavity. Depth of invasion (DOI) is now included in the T staging of primary tumours because of its prognostic impact on the likelihood of concealed metastases and disease-specific survival [72, 73]. Each successive edition of the TNM system has evolved as non-anatomic prognostic features have been introduced, and there has also been a concurrent recording of more prognostic variables and new information that isn’t yet appropriate for the staging criterion. Table 1 shows the tumor classification (T) for oral cancers according to the extent and DOI of primary tumor [74].
Imaging techniques can provide accurate non-invasive soft tissue characterization for assessing superficial primary sites and nodal basins. In head and neck imaging, it is possible to detect neck tumours, lesions of the salivary glands, thyroid nodules, and variations in the morphology of adjacent lymph nodes [75]. The primary site of HNC, nodal disease, and staging using the well-established TNM staging approach are commonly assessed with CT. The infra-hyoid neck may be evaluated well with minimal artifact movement with CT because of its rapid acquisition time. It may simultaneously check the thorax for lung metastases, synchronous primary lung lesions, paratracheal and upper mediastinal lymph nodes and more.
Since there are many neck lymph node levels to analyze and a variety of methodologies and criteria are given for metastatic lymph nodes, the assessment of imaging of lymph node metastasis in HNSCC is a significant difficulty for a radiologist conducting research on this problem. After analyzing all the predictors possible for metastasis of the lymph nodes on CT images, it was seen that the diameter of the lymph node was categorized in 2 ways: axial and coronal diameters as the shortest and longest, respectively [76]. The additional potential factors were long to short axis ratio, necrosis presence, lymph node conglomeration, primary tumor T-stage, etc. The definition given for necrosis was described as low density at the central position with irregular or circular rim kind of lymphatic tissue that was left as a residue [77, 78]. Descriptions of neighboring soft tissue infiltration included a poorly defined nodal region or infiltration into the muscles or fat strands in the neck. The overall extent of necrosis was categorized into several types: absence, presence, and cystic presence. By doing a visual analysis of all 3 types of degree of necrosis, it could be seen that a rim-like structure emerged with > 90% low density [79,80,81].
A study by Morisala et al., aimed to identify CT imaging characteristics of sub-centimeter lymph nodes in oral SCC patients with clinically negative necks (cN0) to predict the likelihood of nodal metastases on histopathology. Retrospective review of patients undergoing elective neck dissection (END) demonstrated that round/oval shape, asymmetric number and disrupted fatty hilum of lymph nodes on pre-operative CT imaging were highly predictive of occult nodal disease. These findings provide valuable insights for guiding decision-making regarding END versus clinical surveillance in cN0 OCSCC patients [82]. In another study, Fujita et al. [17] aimed to explore imaging characteristics of nodal metastasis by HPV status in HNSCC and their influence on outcomes. CT and MRI data from 139 HNSCC patients were retrospectively reviewed. They found that in HPV-positive HNSCC, nodal metastases were notably more prevalent, whereas HPV-negative HNSCC exhibited a higher incidence of disease recurrence. Despite the majority of HPV-positive patients with nodal metastasis presenting extracapsular spread (ECS), their recurrence rates were comparatively lower than those of HPV-negative patients. These findings suggest a distinct pathological pattern and clinical behavior between HPV-positive and HPV-negative HNSCC.
Advanced functional MRI techniques, such as diffusion and perfusion imaging techniques, can also be used to detect metastatic LNs [83, 84]. Increased cell density during LNM may modify water diffusivity, which may be assessed by apparent diffusion coefficient (ADC) utilizing diffusion-weighted MRI (DWI-MRI) [83]. To evaluate tumor vascularity, dynamic contrast-enhanced (DCE)-MRI has been routinely employed. In contrast, positron emission tomography (PET) imaging with 18 F-fluorodeoxyglucose (18 F-FDG) shows inconsistent specificity (77–93%) but excellent sensitivity (92–100%) in identifying nodal metastases [85, 86]. Previous research looking at combining PET and MR imaging discovered that doing so might increase the sensitivity and specificity of finding LNM in HNSCC [87].
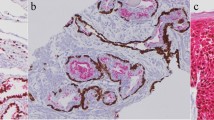
Histopathological features and metastatic behavior
Histopathological evaluation of HNSCC provides a microscopic glimpse into key tumor traits. These characteristics provide vital information about the tumor’s behavior, prognosis and potential treatment options. Among the notable histopathologic features is the tumor grade, which indicates how closely the cells resemble normal ones and plays a significant role in prognosis. According to tumor differentiation, patients with well-differentiated (WHO grade 1) and moderately-differentiated (WHO grade 2) tumors had better survival compared to poorly-differentiated (WHO grade 3) tumors [88]. The tumor’s size is another key determinant of cancer stage and propensity to spread. The invasive nature of HNSCC, infiltrating neighboring tissues like muscle, bone and blood vessels, critically influences prognostic outcomes. Furthermore, the infiltration of lymphatic and blood vessels increases the risk of metastasis to both nearby lymph nodes and distant locations. The invasion of nerves by HNSCC tumors not only causes pain, but also affects available treatment options. Surgical margins that reveal residual tumor cells after surgery indicate incomplete tumor removal, which increases the risk of recurrence. Moreover, the presence of immune cells within the tumor’s microenvironment may provide insight into the immune response against the tumor, potentially holding prognostic value [89,90,91].
The term “lymphatic invasion” refers to an invasion of a vessel’s tunica media together with intimal ulceration, while the existence of tumor cell aggregation inside endothelium-lined regions devoid of underlying muscle walls was referred to as vascular invasion [91]. A study by Adel M et al., was conducted in 571 patients (55 women and 516 men) with oral SCC (OSCC) aged at diagnosis from 21.9 to 86.8 years (median, 51.2 years). There was no evidence that lymphatic invasion was related to a specific sex or age group. Considering vascular invasion, a similar conclusion was reached for sex and age. Pathological differentiation, nodal metastases (p = 0.009), extracapsular dissemination, perineural invasion, and bone invasion all showed statistically significant relationship with lymphatic invasion, and tumor classification (T). Significant relationships between vascular invasion and T classification, extracapsular spread, nodal metastasis, perineural invasion, depth of invasion, and pathologic differentiation were also found. However, there was no significant relationship between vascular invasion and bone invasion. Overall, these correlations showed that the presence of neck metastasis, perineural invasion, extracapsular dissemination, poor differentiation, and deeper tumor depth was positively correlated with the histological findings of lymphatic and vascular invasion in the main OSCC tumors [92].
In order to properly detect and diagnose a tumour, one must have a comprehensive understanding of the tumour’s cellular, biochemical, molecular and pathophysiological aspects. Even though the undifferentiated tumour is still an issue, these patterns help the histopathologist make an accurate diagnosis. It is important to note that these histological patterns are not necessarily diagnostic, as variants and subpatterns can also be observed. Based on patterns found on hematoxylin and eosin-stained sections, the diagnosis may then be confirmed using certain stains, immunohistochemistry, and various molecular diagnostic methods [93]. It was also noted that the majority of OSCC patients with lymphatic or vascular invasion required postoperative adjuvant radiation or chemoradiotherapy since these illnesses were found to be closely related with a number of clinical variables [92].
Clinical and histological assessments remain the main prognostic methods in standard medical practice. Histological characteristics such as perineural invasion, vascular invasion, and the degree of differentiation are widely used as prognostic indicators when assessing patients with HNSCC [94,95,96]. The composition of tumour cells, the presence of stromal components, local immunological responses, and necrosis, are all factors that histological investigation can provide significantly more in-depth information about, all of which may be important prognostic indicators. Due to their predictive value in many types of cancer, these histological features are currently used in clinical practice [97,98,99]. When examining relationships with clinicopathological parameters in HNSCC, tumour necrosis and tumour budding were also found to be substantially correlated with tumour size and clinical stage [100]. In order to obtain additional histological information on the aggressiveness of HNSCC, assessment of tumour size to determine tumor/stroma ratio is a straightforward, reasonably priced procedure that may be utilised in any standard pathology clinic.
Molecular profile of the primary tumor and metastatic spread
HNSCC lesions which are a prevalent model for cancerization, allow for the development of numerous prognostic markers [101, 102]. Molecular pathologic features of HNSCC may differ greatly depending on the location and etiology of the disease [103]. The molecular and genetic characteristics of cancer cells may be the main predictors of metastasis in HNSCC, accompanied by indications of aggressive lymphatic and blood vessels spreading inside the primary tumor [104]. The links between genome alterations and patterns of dissemination in metastatic disease were found to be present in more than 50 types of tumors. This was done by analyzing genomic and clinical data from cohorts of more than 25,000 patients suffering from DM [105]. The most prevalent kind of genetic alteration in HNSCC is tumor-suppressor TP53 mutation which is present in almost 70% of cases [106]. TP53 mutations are often associated with immunotherapy and chemotherapy and could be used as a specific predictor of treatment response in HNSCC patients [107]. HNSCC has also been associated with mutations in other known oncogenes and tumor suppressors such as Cyclin D1, NOTCH1, PIK3CA, MYC, CDKN2A, PTEN and F-box/WD repeat-containing protein 7 [108, 109]. Moreover, various HNSCCs have been linked to a high prevalence of HRAS mutations, copy number changes, and abnormal expression levels of KRAS, NRAS, MYC and EGFR [108]. The genomic analysis of 110 Indian patients with HNSCC identified 5 additional commonly mutated (10–22% of patients) genes linked to OSCC-GB: USP9X (Ubiquitin-Specific Peptidase 9X), MLL4 (Mixed-lineage leukemia 4), ARID2 (AT- rich interactive domain-containing protein 2), UNC13C (UNC-13 homolog C), and TRPM3 (Transient receptor potential cation channel subfamily M member 3) [110]. Furthermore, three others genes WNT16, PARP1 (Poly (ADP-ribose) polymerases), and ATF4 (Activating Transcription factor 4) have a mutation frequency of about 50%. Since oral cancer is recognized for its high expression levels of PARP1, the mutation frequency exceeding 30% suggests that activating mutations are present in all tumor locations [111].
To understand molecular profiling techniques and approaches in HNSCC, we need to be aware of some approaches such as NGS (Next-Generation Sequencing) technology that includes targeted gene panels, whole genome sequencing and whole exome sequencing. NGS is limited to some specific genes, but it can also concentrate on regions that code for base pairs of the entire genome or it can also include the complete analysis of the tumor genome, which includes intronic regions [112]. Many studies have shown mutations that happen at the somatic hotspots get involved in tumorigenesis and are titled as drivers, which may be recurrent mutations occurring in areas of the genome. In some cases where the aberration in the target molecule occurs occasionally, it can be a challenging task taking patients suffering from rare mutations to clinical trials and can act as a barrier to the development of upcoming drugs on the market. A tumor labeled by intratumoral heterogeneity may have an impact on the efficiency of a therapy where a specific variation in the molecule can be called a true driver in a specific tumor [113, 114].
The application of NGS techniques and its related methodologies is useful for understanding the integration of clinical, histopathological and molecular data for assessing metastatic risk in HNSCC. The results of an NGS study can also provide a physician with a list of drugs that can be adapted for patients suffering from cancer [115]. In large-scale tumor profiling studies using NGS methods, significant genomic similarities were found between different types of tumors, which actively shared alterations in driver genes. A BRAF mutation, which has been found in many types of tumors, is an example of this scenario [116]. The alterations in the genome don’t always show the way to the activation or addiction of the oncogenic pathway. There are also some cells that become dependent on one cell for activating a specific oncogenic pathway. In spite of high success rates for analyzing molecular structures to detect HNSCC in patients, NGS technology has shown to be more accurate and faster than other approaches. Utilizing artificial intelligence (AI), particularly in the realm of automated image analysis, has emerged as a valuable tool in the diagnostic assessment of HNC, including HNSCC. The application of AI extends to the classification of lymph nodes in locally-advanced HNSCC, presenting promising diagnostic support. A growing body of research explores the potential of AI and machine learning (ML) in enhancing HNC detection across various imaging modalities. These approaches demonstrate the capacity to achieve levels of accuracy surpassing human judgement in data predictions. However, for widespread clinical integration, the necessity for large-scale, multi-centric prospective studies becomes apparent, facilitating the seamless transition of AI technologies into routine clinical practice [117].
A significant prognostic and predictive marker for HNSCC is the presence of HPV. HPV-positive HNSCC constitutes a significant subset, comprising up to a quarter of all HNSCC cases, with primary tumors predominantly originating from the oropharynx, notably the tonsil and base of tongue [118]. Metastasis to cervical lymph nodes often marks the initial presentation of HPV- positive HNSCC and can be detected via fine-needle aspiration, frequently exhibiting cystic characteristics with a non-keratinizing, basaloid morphology. The determination of HPV status in metastatic HNSCC holds substantial therapeutic and prognostic implications, given the more favorable prognosis associated with HPV-positive tumors compared to conventional HNSCC. Therefore, HPV testing is recommended for any SCC of unknown primary identified in neck lymph nodes. Numerous techniques have been used in supplementary research to distinguish between HPV-positive and -negative HNSCC. These techniques include immunohistochemistry (IHC) staining for p16 as a surrogate marker, HPV polymerase chain reaction (PCR) testing for viral DNA or RNA detection, HPV in situ hybridization (ISH) analysis and more recent methods that are actively being researched [119, 120]. As it identifies transcriptionally active HPV, RT-PCR amplification of viral E6/E7 mRNA is currently regarded as the “gold standard” for the diagnosis of clinically relevant HPV infection inside tumour tissues. The technique is trustworthy when used with formalin-fixed paraffin-embedded (FFPE) samples as well as fresh frozen specimens [120]. Besides, for cancers that are HPV-positive, inactivating the p16 gene is a very important target. Examining and learning more about DNA damage repair genes and how destructive they may be is becoming a certain and promising strategy to combat HPV-negative cancers as well. Exploring and understanding etiological features is also another approach to defining the characteristics of the tumor and metastasis [121].
Emerging therapeutic approaches for HNSCC
Patients with recurrent HNSCC may be candidates for salvage surgery, further radiation, or chemotherapy, however this is not always applicable to patients with DM. Nowadays, various metastatic cancers, including HNSCC, are presently addressed using immunotherapy as a frontline approach, often combined with conventional chemotherapy, targeted therapy or other modalities. Cetuximab, was the first a monoclonal antibody that emerged as a promising immunotherapy option in the management of locally advanced HNSCC. Cetuximab acts by targeting the extracellular domain of EGFR, which along with EGF are upregulated in 90% of HNSCC patients and linked with poor outcomes [122]. Clinical trials have demonstrated its efficacy when combined with standard treatments such radiotherapy or platinum-based chemotherapy. In a study by Bonner et al., the combination of cetuximab and radiation resulted in a 45.6% 5-year overall survival rate compared to a radiation-only (36.4%) approach [123]. Similarly Vermoken et al. reported a prolonged median overall survival from 7.4 months in the chemotherapy-alone group to 10.1 months when cetixumab added to the regimen [124].
In 2016, the anti-PD-1 immune checkpoint inhibitors (ICIs) nivolumab and pembrolizumab were both approved for HNSCC patients with recurrent or metastatic HNSCC. In 2019, pembrolizumab was approved for first-line treatment either as monotherapy in PD-L1 expressing tumors or combined with chemotherapy [125]. ICIs function by prompting the host’s immune system to identify abnormal cells, employing immune cells’ cytotoxic capabilities to target cancerous cells, particularly those specific to tumors and responsive to T cell cytotoxicity. T cells activate tumor cells via a two-way signaling pathway: the first signal involves T cell receptor recognition of tumor cells presenting major histocompatibility complex (MHC) antigens, while the second signal results from interaction with co-stimulatory factors and B7 molecules on antigen-presenting cells (APCs) [126]. Without both signals, T cell activation is hindered. Immune checkpoints regulate immune response initiation and cessation, as well as T cell activation and other host immune activities [127]. Immunotherapeutic approaches may necessitate a distinct evaluation compared to standard anti-tumor treatments. Patients receiving ICIs may experience hyper-progression characterized by rapid tumor growth or pseudo-progression, an initial tumor enlargement followed by regression [128]. Hyper-progression correlates with poor survival and may result from an excessive immune response, PD-1 mediated tumor promotion or familial cancer predisposition. Pseudo-progression may elucidate enhanced chemotherapy efficacy post anti-PD-1 therapy failure. Comparing nivolumab to a three-component cetuximab, docetaxel, and methotrexate regimen during disease progression, nivolumab exhibited a complete survival scale of 7.7 months [129]. Reduction relative to nivolumab could stem from crossover effects in the chemotherapy group, where patients often receive immunotherapy with secondary effects. Additionally, the less favorable outcomes with weekly nivolumab compared to three-weekly docetaxel, commonly used due to its efficacy, may contribute to the discrepancy [129]. Today, both nivolumab and pembrolizumab, were found to be effective in platinum sensitive patients with recurrent or metastatic HNSCC [130].
Although chemotherapy is considered the standard treatment for metastatic HNSCC, radiation techniques, such as stereotactic body radiotherapy, can also provide palliation. After careful patient selection, high-dose regimens could be used in metastatic patients with good performance status. In addition, oligometastatic disease can be treated more effectively in some clinical settings [131]. However, there are relatively few clinical and radiological indicators of radiation therapy toxicity and response to treatment, and they are not frequently employed in clinical practice for head and neck tumors. One of the most exciting areas of study is the “omics” method. It might generate a lot of data that could be used to forecast patient toxicity and the response to radiation treatment [132].
Clinical experiments conducted over the past ten years have demonstrated the prognostic role of numerous molecules involved in tumor metastasis and growth. None of them have received much attention in clinical practice up to this point, most likely because research on their expression, typically using quantitative or immunohistochemical methods, has shown that these molecules are involved in the development of tumors without being able to conclusively attribute to them a specific marker function for HNSCC metastases. Clinicians may have the chance to develop novel diagnostic strategies, therapeutic integration, and meticulous follow-up if a significant molecular marker that can predict cervical lymph node metastasis from a primary tumor biopsy is found. This is in addition to the conventional clinicopathological parameters. The follow up care and strategies for HNSCC can be classified into 2 types which are standardized and personalized, respectively. The predetermined therapy program for HNSCC patients over a period of approximately five years essentially constitutes the typical follow-up [133]. The Bowen’s key method is used to determine whether it is feasible to offer a standardized or personalized follow up to a HNSCC patient. It suggests that a specific framework of feasibility studies is present in the areas of focus to treat such a patient [134]. Data collection, management, and a certain sample size are additional requirements for validating the personalized treatment plans and follow-up strategies for HNSCC. One of the surveys showed that 25% of HNC patients chose personalized follow up after making a decision [135].
Conclusions and future perspectives
The ability to detect the presence of micro-metastases or the metastatic potential of a tumour at an early stage might influence the development of metastatic tumours and the treatment strategy. Numerous potential applications in HNSCC treatment have been revealed through invasion studies. The simplest strategy is to develop inhibitors directed at molecules crucial for invasion. Today, clinical and histological assessment of the tumor is still used to predict HNSCC metastatic risk. It has also been made possible by developments made in the past ten years in understanding the molecular pathways involved in neoplastic tumour formation to identify molecules that could be used as potential prognostic indicators for this malignancy. Sometimes the patterns of certain genomic alterations vary among patients. Clinical parameters must also be tested to ensure the quality of drug screening assays. Comprehending forthcoming advancements in HNSCC technology, along with enhancing capabilities to detect biomarkers and evaluate medications, could significantly enhance the management of this malignancy.
Data availability
No datasets were generated or analysed during the current study.
References
Parkin DM, Bray F, Ferlay J, Pisani P (2002) Global Cancer Statistics, CA: A Cancer Journal for Clinicians, vol. 55, no. 2, pp. 74–108, Mar. 2005, https://doi.org/10.3322/canjclin.55.2.74
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR (2020) Head and neck squamous cell carcinoma. Nat Rev Dis Primers. 6(1):92. https://doi.org/10.1038/s41572-020-00224-3. Erratum in: Nat Rev Dis Primers. 2023;9(1):4. PMID: 33243986; PMCID: PMC7944998
Edwards BK et al (2005) Oct., Annual Report to the Nation on the Status of Cancer, 1975–2002, Featuring Population-Based Trends in Cancer Treatment, JNCI: Journal of the National Cancer Institute, vol. 97, no. 19, pp. 1407–1427, https://doi.org/10.1093/jnci/dji289
Khuri FR et al (2006) Apr., Randomized Phase III Trial of Low-dose Isotretinoin for Prevention of Second Primary Tumors in Stage I and II Head and Neck Cancer Patients, JNCI: Journal of the National Cancer Institute, vol. 98, no. 7, pp. 441–450, https://doi.org/10.1093/jnci/djj091
Weber RS et al (Jan. 2003) Outcome of Salvage Total Laryngectomy Following Organ Preservation Therapy. Archives Otolaryngology–Head Neck Surg 129(1):44. https://doi.org/10.1001/archotol.129.1.44
Lee JJ et al (2000) Predicting cancer development in oral leukoplakia: ten years of translational research. Clin Cancer Res 6(5):1702–1710
Goldenberg D et al (2004) Dec., Habitual Risk Factors for Head and Neck Cancer, Otolaryngology–Head and Neck Surgery, vol. 131, no. 6, pp. 986–993, https://doi.org/10.1016/j.otohns.2004.02.035
Audet N, Beasley NJ, MacMillan C, Jackson DG, Gullane PJ, Kamel-Reid S (Dec. 2005) Lymphatic vessel density, nodal metastases, and prognosis in patients with Head and Neck Cancer. Archives Otolaryngology–Head Neck Surg 131(12):1065. https://doi.org/10.1001/archotol.131.12.1065
Spector JG et al (2001) Jun., Delayed Regional Metastases, Distant Metastases, and Second Primary Malignancies in Squamous Cell Carcinomas of the Larynx and Hypopharynx, The Laryngoscope, vol. 111, no. 6, pp. 1079–1087, https://doi.org/10.1097/00005537-200106000-00028
Duprez F et al (Sep. 2017) Distant metastases in head and neck cancer. Head Neck 39(9):1733–1743. https://doi.org/10.1002/hed.24687
Hasegawa T et al (2015) Jun., Risk Factors Associated with Distant Metastasis in Patients with Oral Squamous Cell Carcinoma, Otolaryngology–Head and Neck Surgery, vol. 152, no. 6, pp. 1053–1060, https://doi.org/10.1177/0194599815580980
Nonaka T, Wong DTW (2018) Liquid Biopsy in Head and Neck Cancer: Promises and Challenges. J Dent Res. ;97(6):701–708. doi: 10.1177/0022034518762071. Epub 2018 Mar 7. PMID: 29513618; PMCID: PMC5960882
Kabzinski J, Kucharska-Lusina A, Majsterek I (2023) RNA-Based Liquid Biopsy in Head and Neck Cancer. Cells 12(14):1916. https://doi.org/10.3390/cells12141916PMID: 37508579; PMCID: PMC10377854
Basheeth N, Patil N (Oct. 2019) Biomarkers in Head and Neck Cancer an Update. Indian J Otolaryngol Head Neck Surg 71:1002–1011. https://doi.org/10.1007/s12070-019-01683-1
Goesswein D et al (May. 2018) Expressional analysis of disease-relevant signalling-pathways in primary tumours and metastasis of head and neck cancers. Sci Rep 8(1). https://doi.org/10.1038/s41598-018-25512-7
Chen L, Zeng H, Zhang M, Luo Y, Ma X (2021) Histopathological image and gene expression pattern analysis for predicting molecular features and prognosis of head and neck squamous cell carcinoma, Cancer Med, vol. 10, no. 13, pp. 4615–4628, Jul. https://doi.org/10.1002/cam4.3965
Fujita A et al (Oct. 2016) Imaging characteristics of metastatic nodes and outcomes by HPV status in head and neck cancers. Laryngoscope 126(2):392–398. https://doi.org/10.1002/lary.25587
Guan X (Sept. 2015) Cancer metastases: challenges and opportunities. Acta Pharm Sin B 5(5):402–418. https://doi.org/10.1016/j.apsb.2015.07.005
Chambers AF, Groom AC, MacDonald IC (2002) Dissemination and growth of cancer cells in metastatic sites, Nature Reviews Cancer, vol. 2, no. 8, pp. 563–572, Aug. https://doi.org/10.1038/nrc865
Gómez-Cuadrado L, Tracey N, Ma R, Qian B, Brunton VG (2017) Mouse models of metastasis: progress and prospects, Disease Models & Mechanisms, vol. 10, no. 9, pp. 1061–1074, Sep. https://doi.org/10.1242/dmm.030403
Francia G, Cruz-Munoz W, Man S, Xu P, Kerbel RS (2011) Mouse models of advanced spontaneous metastasis for experimental therapeutics, Nature Reviews Cancer, vol. 11, no. 2, pp. 135–141, Feb. https://doi.org/10.1038/nrc3001
Koike Y et al (2020) Sep., Machine learning-based histological classification that predicts recurrence of peripheral lung squamous cell carcinoma, Lung Cancer, vol. 147, pp. 252–258, https://doi.org/10.1016/j.lungcan.2020.07.011
Sarioglu S et al (2010) Feb., Tumor budding as a prognostic marker in laryngeal carcinoma, Pathology - Research and Practice, vol. 206, no. 2, pp. 88–92, https://doi.org/10.1016/j.prp.2009.09.006
Almangush A, Pirinen M, Heikkinen I, Mäkitie AA, Salo T, Leivo I (2018) Tumour budding in oral squamous cell carcinoma: a meta-analysis, British Journal of Cancer, vol. 118, no. 4, pp. 577–586, Feb. https://doi.org/10.1038/bjc.2017.425
Luo W, Li L, Li S, Jiang H, Chen X (2010) [Influence of celecoxib on invasiveness of human high-metastatic nasopharyngeal carcinoma cell line CNE-2Z]., Zhonghua er bi yan hou tou jing wai ke za zhi = Chinese journal of otorhinolaryngology head and neck surgery, vol. 45, no. 11, pp. 941–5, Nov. [Online]. Available: http://www.ncbi.nlm.nih.gov/pubmed/21215211
Mughees M, Sengupta A, Khowal S, Wajid S (Feb. 2021) Mechanism of tumour microenvironment in the progression and development of oral cancer. Mol Biol Rep 48(2):1773–1786. https://doi.org/10.1007/s11033-020-06054-6
Karamanos NK et al (2021) Dec., A guide to the composition and functions of the extracellular matrix, The FEBS Journal, vol. 288, no. 24, pp. 6850–6912, https://doi.org/10.1111/febs.15776
White RA, Malkoski SP, Wang X-J (2010) TGFβ signaling in head and neck squamous cell carcinoma, Oncogene, vol. 29, no. 40, pp. 5437–5446, Oct. https://doi.org/10.1038/onc.2010.306
Smith A, Teknos TN, Pan Q (Apr. 2013) Epithelial to mesenchymal transition in head and neck squamous cell carcinoma. Oral Oncol 49(4):287–292. https://doi.org/10.1016/j.oraloncology.2012.10.009
Jolly MK, Ware KE, Gilja S, Somarelli JA, Levine H (2017) EMT and MET: necessary or permissive for metastasis? Mol. Oncol 11:755–769. https://doi.org/10.1002/1878-0261.12083
Pang X, Tang Y, Liang X (2018) Transforming growth factor–β signaling in head and neck squamous cell carcinoma: Insights into cellular responses (Review), Oncology Letters, Aug. https://doi.org/10.3892/ol.2018.9319
Takahashi K et al (Sep. 2022) TGF-β generates a population of cancer cells residing in G1 phase with high motility and metastatic potential via KRTAP2-3. Cell Rep 40(13):111411. https://doi.org/10.1016/j.celrep.2022.111411
Yoon Y et al (2007) Aug., CXC Chemokine Receptor-4 Antagonist Blocks Both Growth of Primary Tumor and Metastasis of Head and Neck Cancer in Xenograft Mouse Models, Cancer Research, vol. 67, no. 15, pp. 7518–7524, https://doi.org/10.1158/0008-5472.CAN-06-2263
Albert S et al (2013) Dec., Focus on the role of the CXCL12/CXCR4 chemokine axis in head and neck squamous cell carcinoma, Head & Neck, vol. 35, no. 12, pp. 1819–1828, https://doi.org/10.1002/hed.23217
Lee B, Jang JY, Seo C, Kim C (Jan. 2021) Crosstalk between head and neck cancer cells and lymphatic endothelial cells promotes tumor metastasis via CXCL5-CXCR2 signaling. FASEB J 35(1). https://doi.org/10.1096/fj.202001455R
Johnson DE (Jul. 2012) Targeting proliferation and survival pathways in head and neck cancer for therapeutic benefit. Chin J Cancer 31(7):319–326. https://doi.org/10.5732/cjc.011.10404
Pomerantz RG, Grandis JR (Apr. 2003) The role of epidermal growth factor receptor in head and neck squamous cell carcinoma. Curr Oncol Rep 5(2):140–146. https://doi.org/10.1007/s11912-003-0101-z
Janecka-Widła A, Majchrzyk K, Mucha-Małecka A, Biesaga B (2021) EGFR/PI3K/Akt/mTOR pathway in head and neck squamous cell carcinoma patients with different HPV status. Pol J Pathol 72(4):296–314. https://doi.org/10.5114/pjp.2021.113073
Swick AD et al (Jul. 2017) Cotargeting mTORC and EGFR Signaling as a therapeutic strategy in HNSCC. Mol Cancer Ther 16(7):1257–1268. https://doi.org/10.1158/1535-7163.MCT-17-0115
Fernández-Mateos J et al (Dec. 2016) Epidermal growth factor receptor (EGFR) pathway polymorphisms as predictive markers of cetuximab toxicity in locally advanced head and neck squamous cell carcinoma (HNSCC) in a Spanish population. Oral Oncol 63:38–43. https://doi.org/10.1016/j.oraloncology.2016.10.006
Zuo J et al (2011) Sep., Activation of EGFR promotes squamous carcinoma SCC10A cell migration and invasion via inducing EMT-like phenotype change and MMP‐9‐mediated degradation of E‐cadherin, Journal of Cellular Biochemistry, vol. 112, no. 9, pp. 2508–2517, https://doi.org/10.1002/jcb.23175
Shi E et al (Aug. 2023) 5ʹ-Ectonucleotidase CD73/NT5E supports EGFR-mediated invasion of HPV-negative head and neck carcinoma cells. J Biomed Sci 30(1):72. https://doi.org/10.1186/s12929-023-00968-6
Raj S et al (Dec. 2022) Molecular mechanism(s) of regulation(s) of c-MET/HGF signaling in head and neck cancer. Mol Cancer 21(1):31. https://doi.org/10.1186/s12943-022-01503-1
Ferris RL (2015) Immunology and Immunotherapy of Head and Neck Cancer. J Clin Oncol 33(29):3293–3304. https://doi.org/10.1200/JCO.2015.61.1509Epub 2015 Sep 8. PMID: 26351330; PMCID: PMC4586169
Bu LL, Yu GT, Wu L, Mao L, Deng WW, Liu JF, Kulkarni AB, Zhang WF, Zhang L, Sun ZJ (2017) STAT3 induces immunosuppression by upregulating PD-1/PD-L1 in HNSCC. J Dent Res 96(9):1027–1034 Epub 2017 Jun 12. PMID: 28605599; PMCID: PMC6728673
Geiger JL, Grandis JR, Bauman JE (2016) The STAT3 pathway as a therapeutic target in head and neck cancer: barriers and innovations. Oral Oncol 56:84–92. https://doi.org/10.1016/j.oraloncology.2015.11.022Epub 2015 Dec 28. PMID: 26733183; PMCID: PMC5590227
Kortylewski M, Kujawski M, Wang T, Wei S, Zhang S, Pilon-Thomas S, Niu G, Kay H, Mulé J, Kerr WG, Jove R, Pardoll D, Yu H (2005) Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat Med
Vander Broek R, Mohan S, Eytan DF, Chen Z, Van Waes C (2015) The PI3K/Akt/mTOR axis in head and neck cancer: functions, aberrations, cross-talk, and therapies. Oral Dis 21(7):815–825. https://doi.org/10.1111/odi.12206Epub 2013 Dec 23. PMID: 24219320
Sun P, Meng LH (2020) Emerging roles of class I PI3K inhibitors in modulating tumor microenvironment and immunity. Acta Pharmacol Sin 41(11):1395–1402. https://doi.org/10.1038/s41401-020-00500-8Epub 2020 Sep 16. PMID: 32939035; PMCID: PMC7656798
Pantel K, Alix-Panabières C (Jul. 2019) Liquid biopsy and minimal residual disease — latest advances and implications for cure. Nat Reviews Clin Oncol 16(7):409–424. https://doi.org/10.1038/s41571-019-0187-3
Kawada K, Taketo MM (2011) Significance and Mechanism of Lymph Node Metastasis in Cancer Progression, Cancer Research, vol. 71, no. 4, pp. 1214–1218, Feb. https://doi.org/10.1158/0008-5472.CAN-10-3277
Shah JP, Gil Z (2009) Current concepts in management of oral cancer – Surgery, Oral Oncology, vol. 45, no. 4–5, pp. 394–401, Apr. https://doi.org/10.1016/j.oraloncology.2008.05.017
Ferlito A et al (2002) Dec., Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes, Oral Oncology, vol. 38, no. 8, pp. 747–751, https://doi.org/10.1016/S1368-8375(02)00052-0
Takes RP et al (Sep. 2012) Distant metastases from head and neck squamous cell carcinoma. Part I. Basic aspects. Oral Oncol 48(9):775–779. https://doi.org/10.1016/j.oraloncology.2012.03.013
Liu JC, Bhayani M, Kuchta K, Galloway T, Fundakowski C (Jan. 2019) Patterns of distant metastasis in head and neck cancer at presentation: implications for initial evaluation. Oral Oncol 88:131–136. https://doi.org/10.1016/j.oraloncology.2018.11.023
Lu H-J et al (Jan. 2022) Prediction model of distant metastasis in oral cavity squamous cell Carcinoma with or without Regional Lymphatic Metastasis. Front Oncol 11. https://doi.org/10.3389/fonc.2021.713815
de Bree R, Deurloo EE, Snow GB, Leemans CR (2000) Screening for Distant Metastases in Patients With Head and Neck Cancer, The Laryngoscope, vol. 110, no. 3, pp. 397–401, Mar. https://doi.org/10.1097/00005537-200003000-00012
Xie Q, Ding J, Chen Y (Jun. 2021) Role of CD8 + T lymphocyte cells: interplay with stromal cells in tumor microenvironment. Acta Pharm Sin B 11:1365–1378. https://doi.org/10.1016/j.apsb.2021.03.027
Chung MK, Lee GJ, Choi N, Cho J-K, Jeong H-S, Baek C-H (2015) Comparative study of sentinel lymph node biopsy in clinically N0 oral tongue squamous cell carcinoma: Long-term oncologic outcomes between validation and application phases, Oral Oncology, vol. 51, no. 10, pp. 914–920, Oct. https://doi.org/10.1016/j.oraloncology.2015.07.007
Dennington ML, Carter DR, Meyers AD (1980) Distant metastases in head and neck epidermoid carcinoma, The Laryngoscope, vol. 90, no. 2, pp. 196–201, Feb. https://doi.org/10.1288/00005537-198002000-00002
Vikram B, Strong EW, Shah JP, Spiro R (1984) Failure at the primary site following multimodality treatment in advanced head and neck cancer, Head & Neck Surgery, vol. 6, no. 3, pp. 720–723, Jan. https://doi.org/10.1002/hed.2890060303
Zbaren P, Lehmann W (1987) Frequency and Sites of Distant Metastases in Head and Neck Squamous Cell Carcinoma: An Analysis of 101 Cases at Autopsy, Archives of Otolaryngology - Head and Neck Surgery, vol. 113, no. 7, pp. 762–764, Jul. https://doi.org/10.1001/archotol.1987.01860070076020
Leemans CR, Tiwari R, Nauta JPJ, Van der Waal I, Snow GB (1993) Regional lymph node involvement and its significance in the development of distant metastases in head and neck carcinoma, Cancer, vol. 71, no. 2, pp. 452–456, Jan. https://doi.org/10.1002/1097-0142(19930115)71:2<452::AID-CNCR2820710228>3.0.CO;2-B
Alvi A, Johnson JT (Sep. 1997) Development of distant metastasis after treatment of advanced-stage head and neck cancer. Head Neck 19(6):500–505. https://doi.org/10.1002/(SICI)1097-0347(199709)19:6<500::AID-HED7>3.0.CO;2-2
de Bree R et al (2015) Dec., Advances in diagnostic modalities to detect occult lymph node metastases in head and neck squamous cell carcinoma, Head & Neck, vol. 37, no. 12, pp. 1829–1839, https://doi.org/10.1002/hed.23814
Probert JC, Thompson RW, Bagshaw MA (Jan. 1974) Patterns of spread of distant metastases in head and neck cancer. Cancer 33(1):127–133. https://doi.org/10.1002/1097-0142(197401)33:1<127::AID-CNCR2820330119>3.0.CO;2-L
Bhatia R, Bahadur S (1987) Distant metastasis in malignancies of the head and neck, The Journal of Laryngology & Otology, vol. 101, no. 9, pp. 925–928, Sep. https://doi.org/10.1017/S0022215100102993
Akita H et al (Jun. 2009) Effects of neoadjuvant chemotherapy on primary tumor and lymph node metastasis in esophageal squamous cell carcinoma: additive association with prognosis. Dis Esophagus 22(4):291–297. https://doi.org/10.1111/j.1442-2050.2008.00879.x
Falck A-K, Fernö M, Bendahl P-O, Rydén L (Dec. 2013) St Gallen molecular subtypes in primary breast cancer and matched lymph node metastases - aspects on distribution and prognosis for patients with luminal A tumours: results from a prospective randomised trial. BMC Cancer 13(1):558. https://doi.org/10.1186/1471-2407-13-558
Fruhwirth GO, Diocou S, Blower PJ, Ng T, Mullen GED (2014) A Whole-Body Dual-Modality Radionuclide Optical Strategy for Preclinical Imaging of Metastasis and Heterogeneous Treatment Response in Different Microenvironments, Journal of Nuclear Medicine, vol. 55, no. 4, pp. 686–694, Apr. https://doi.org/10.2967/jnumed.113.127480
Padera TP et al (2008) Aug., Differential response of primary tumor versus lymphatic metastasis to VEGFR-2 and VEGFR-3 kinase inhibitors cediranib and vandetanib, Molecular Cancer Therapeutics, vol. 7, no. 8, pp. 2272–2279, https://doi.org/10.1158/1535-7163.MCT-08-0182
Spiro RH, Huvos AG, Wong GY, Spiro JD, Gnecco CA, Strong EW (1986) Predictive value of tumor thickness in squamous carcinoma confined to the tongue and floor of the mouth, The American Journal of Surgery, vol. 152, no. 4, pp. 345–350, Oct. https://doi.org/10.1016/0002-9610(86)90302-8
Ebrahimi A et al (2014) Sep., Minimum Nodal Yield in Oral Squamous Cell Carcinoma: Defining the Standard of Care in a Multicenter International Pooled Validation Study, Annals of Surgical Oncology, vol. 21, no. 9, pp. 3049–3055, https://doi.org/10.1245/s10434-014-3702-x
Huang SH, O’Sullivan B (Jul. 2017) Overview of the 8th Edition TNM classification for Head and Neck Cancer. Curr Treat Options Oncol 18:40. https://doi.org/10.1007/s11864-017-0484-y
Oren N, Vaysberg A, Ginat DT (Dec. 2019) Updated WHO nomenclature of head and neck lesions and associated imaging findings. Insights into Imaging 10(1):72. https://doi.org/10.1186/s13244-019-0760-4
Castelijns JA, van den Brekel MW (2002) Imaging of lymphadenopathy in the neck, European Radiology, vol. 12, no. 4, pp. 727–738, Apr. https://doi.org/10.1007/s003300101102
Steinkamp HJ, Cornehl M, Hosten N, Pegios W, Vogl T, Felix R (1995) Cervical lymphadenopathy: ratio of long- to short-axis diameter as a predictor of malignancy, The British Journal of Radiology, vol. 68, no. 807, pp. 266–270, Mar. https://doi.org/10.1259/0007-1285-68-807-266
Som PM (May 1992) Detection of metastasis in cervical lymph nodes: CT and MR criteria and differential diagnosis. Am J Roentgenol 158(5):961–969. https://doi.org/10.2214/ajr.158.5.1566697
Hoang JK, Vanka J, Ludwig BJ, Glastonbury CM (Jan. 2013) Evaluation of cervical lymph nodes in Head and Neck Cancer with CT and MRI: Tips, traps, and a systematic Approach. Am J Roentgenol 200(1):W17–W25. https://doi.org/10.2214/AJR.12.8960
van den Brekel MW et al (Nov. 1990) Cervical lymph node metastasis: assessment of radiologic criteria. Radiology 177(2):379–384. https://doi.org/10.1148/radiology.177.2.2217772
Gor DM, Langer JE, Loevner LA (2006) Imaging of Cervical Lymph Nodes in Head and Neck Cancer: The Basics, Radiologic Clinics of North America, vol. 44, no. 1, pp. 101–110, Jan. https://doi.org/10.1016/j.rcl.2005.08.006
Morisada MV, Bewley AF, Broadhead K, Assadsangabi R, Paydar A, Birkeland AC, Abouyared M, Qi L, Ivanovic V CT predictors of sub-centimeter occult lymph node metastases in oral cavity squamous cell carcinoma: A case-control study. Neuroradiol J. 2023 Dec 26:19714009231224447. doi: 10.1177/19714009231224447. Epub ahead of print. PMID: 38148295
Sumi M et al (2003) Discrimination of metastatic cervical lymph nodes with diffusion-weighted MR imaging in patients with head and neck cancer. Am J Neuroradiol 24(8):1627–1634
Klerkx WM et al (2010) Feb., Detection of Lymph Node Metastases by Gadolinium-Enhanced Magnetic Resonance Imaging: Systematic Review and Meta-analysis, JNCI: Journal of the National Cancer Institute, vol. 102, no. 4, pp. 244–253, https://doi.org/10.1093/jnci/djp514
Monteil J et al (2011) Lymph node assessment with 18F-FDG-PET and MRI in uterine cervical cancer. Anticancer Res 31(11):3865–3871
Song B-I et al (2012) Sep., 18 F-FDG Uptake by Metastatic Axillary Lymph Nodes on Pretreatment PET/CT as a Prognostic Factor for Recurrence in Patients with Invasive Ductal Breast Cancer, Journal of Nuclear Medicine, vol. 53, no. 9, pp. 1337–1344, https://doi.org/10.2967/jnumed.111.098640
Yoon DY et al (2009) Mar., CT, MR, US, 18F-FDG PET/CT, and their combined use for the assessment of cervical lymph node metastases in squamous cell carcinoma of the head and neck, European Radiology, vol. 19, no. 3, pp. 634–642, https://doi.org/10.1007/s00330-008-1192-6
Amit Badola P, Mehta S, Mehra S, Sood (2023) Epidemiology and survival analysis of head and neck cancer: results from comprehensive care center in North India. Oral Oncol Rep 6:100022. https://doi.org/10.1016/j.oor.2023.100022
Naz S, Salah K, Khurshid A, Hashmi AA, Faridi N (May 2015) Head and Neck Squamous Cell Carcinoma - comparative evaluation of pathological parameters in Young and Old patients. Asian Pac J Cancer Prev 16(9):4061–4063. https://doi.org/10.7314/APJCP.2015.16.9.4061
Xu B et al (2021) Sep., The prognostic role of histologic grade, worst pattern of invasion, and tumor budding in early oral tongue squamous cell carcinoma: a comparative study, Virchows Archiv, vol. 479, no. 3, pp. 597–606, https://doi.org/10.1007/s00428-021-03063-z
Jimenez L, Jayakar SK, Ow TJ, Segall JE (2015) Mechanisms of Invasion in Head and Neck Cancer, Archives of Pathology & Laboratory Medicine, vol. 139, no. 11, pp. 1334–1348, Nov. https://doi.org/10.5858/arpa.2014-0498-RA
Adel M et al (2015) Oct., Evaluation of Lymphatic and Vascular Invasion in Relation to Clinicopathological Factors and Treatment Outcome in Oral Cavity Squamous Cell Carcinoma, Medicine, vol. 94, no. 43, p. e1510, https://doi.org/10.1097/MD.0000000000001510
Dive A, Bodhade A, Mishra M, Upadhyaya N (2014) Histological patterns of head and neck tumors: an insight to tumor histology. J Oral Maxillofacial Pathol 18(1):58. https://doi.org/10.4103/0973-029X.131912
Alkhadar H, Macluskey M, White S, Ellis I (2020) Perineural invasion in oral squamous cell carcinoma: Incidence, prognostic impact and molecular insight, Journal of Oral Pathology & Medicine, vol. 49, no. 10, pp. 994–1003, Nov. https://doi.org/10.1111/jop.13069
Colonia-García A, Salazar-Peláez LM, Serna-Ortiz CA, Álvarez-Sánchez LG, de Andrade CR (2022) Prognostic value of lymphovascular and perineural invasion in squamous cell carcinoma of the tongue, Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, vol. 133, no. 2, pp. 207–215, Feb. https://doi.org/10.1016/j.oooo.2021.08.021
Huang Q et al (Mar. 2023) Prognostic impact of lymphovascular and perineural invasion in squamous cell carcinoma of the tongue. Sci Rep 13(1):3828. https://doi.org/10.1038/s41598-023-30939-8
Kemi N et al (Aug. 2018) Tumour-stroma ratio and prognosis in gastric adenocarcinoma. Br J Cancer 119(4):435–439. https://doi.org/10.1038/s41416-018-0202-y
Sullivan L, Pacheco RR, Kmeid M, Chen A, Lee H (2022) Tumor stroma ratio and its significance in locally Advanced Colorectal Cancer. Curr Oncol 29(5):3232–3241. https://doi.org/10.3390/curroncol29050263PMID: 35621653; PMCID: PMC9139914
Maibach F, Sadozai H, Seyed Jafari SM, Hunger RE, Schenk M (2020) Tumor-infiltrating lymphocytes and their prognostic value in cutaneous melanoma. Front Immunol 11:2105. https://doi.org/10.3389/fimmu.2020.02105PMID: 33013886; PMCID: PMC7511547
Caruntu A, Moraru L, Lupu M, Ciubotaru DA, Dumitrescu M, Eftimie L, Hertzog R, Zurac S, Caruntu C, Voinea OC (2021) Assessment of histological features in squamous cell Carcinoma Involving Head and Neck skin and Mucosa. J Clin Med 10(11):2343. https://doi.org/10.3390/jcm10112343PMID: 34071843; PMCID: PMC8199467
Braakhuis BJM, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH (2003) A genetic explanation of Slaughter’s concept of field cancerization: evidence and clinical implications. Cancer Res 63(8):1727–1730
Choi S, Myers JN (2008) Molecular Pathogenesis of Oral Squamous Cell Carcinoma: Implications for Therapy, Journal of Dental Research, vol. 87, no. 1, pp. 14–32, Jan. https://doi.org/10.1177/154405910808700104
Leemans CR, Snijders PJF, Brakenhoff RH (2018) The molecular landscape of head and neck cancer. Nat Rev Cancer 18(5):269–282. https://doi.org/10.1038/nrc.2018.11Epub 2018 Mar 2
Allen CT, Law JH, Dunn GP, Uppaluri R (2013) Emerging insights into head and neck cancer metastasis, Head & Neck, vol. 35, no. 11, pp. 1669–1678, Nov. https://doi.org/10.1002/hed.23202
Nguyen B et al (Feb. 2022) Genomic characterization of metastatic patterns from prospective clinical sequencing of 25,000 patients. Cell 185(3):563–575e. https://doi.org/10.1016/j.cell.2022.01.003
Mulder FJ, Pierssens DDCG, Baijens LWJ et al (2021) Evidence for different molecular parameters in head and neck squamous cell carcinoma of nonsmokers and nondrinkers: systematic review and meta-analysis on HPV, p16, and TP53. Head Neck 43:303–322. https://doi.org/10.1002/hed.26513
Wei M, Zhi J, Li L, Wang W (2023) Predicting therapeutic responses in head and neck squamous cell carcinoma from TP53 mutation detected by cell-free DNA. Transl Cancer Res 12(12):3604–3617. https://doi.org/10.21037/tcr-23-878Epub 2023 Dec 11. PMID: 38197078; PMCID: PMC10774070
Mountzios G, Rampias T, Psyrri A (Oct. 2014) The mutational spectrum of squamous-cell carcinoma of the head and neck: targetable genetic events and clinical impact. Ann Oncol 25(10):1889–1900. https://doi.org/10.1093/annonc/mdu143
Fernández-Mateos J et al (Oct. 2020) Oncogenic driver mutations predict outcome in a cohort of head and neck squamous cell carcinoma (HNSCC) patients within a clinical trial. Sci Rep 10(1):16634. https://doi.org/10.1038/s41598-020-72927-2
Maitra A et al (2013) Dec., Mutational landscape of gingivo-buccal oral squamous cell carcinoma reveals new recurrently-mutated genes and molecular subgroups, Nature Communications, vol. 4, no. 1, p. 2873, https://doi.org/10.1038/ncomms3873
Kossatz S et al (Feb. 2016) Detection and delineation of oral cancer with a PARP1 targeted optical imaging agent. Sci Rep 6(1):21371. https://doi.org/10.1038/srep21371
Vlachogiannis G et al (Feb. 2018) Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science 359(6378):920–926. https://doi.org/10.1126/science.aao2774
Le Tourneau C et al (Oct. 2015) Molecularly targeted therapy based on tumour molecular profiling versus conventional therapy for advanced cancer (SHIVA): a multicentre, open-label, proof-of-concept, randomised, controlled phase 2 trial. Lancet Oncol 16(13):1324–1334. https://doi.org/10.1016/S1470-2045(15)00188-6
Bailey MH et al (Apr. 2018) Comprehensive Characterization of Cancer Driver Genes and Mutations. Cell 173(2):371–385. https://doi.org/10.1016/j.cell.2018.02.060. .e18
Agarwal R et al (2014) Targeted therapy for hereditary cancer syndromes: hereditary breast and ovarian cancer syndrome, Lynch syndrome, familial adenomatous polyposis, and Li-Fraumeni syndrome. Discov Med 18(101):331–339
Le DT et al (Jul. 2017) Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 357(6349):409–413. https://doi.org/10.1126/science.aan6733
Mahmood H, Shaban M, Rajpoot N, Khurram SA (Jun. 2021) Artificial Intelligence-based methods in head and neck cancer diagnosis: an overview. Br J Cancer 124(12):1934–1940. https://doi.org/10.1038/s41416-021-01386-xEpub 2021 Apr 19
Chaturvedi AK et al (Nov. 2011) Human papillomavirus and rising Oropharyngeal Cancer incidence in the United States. J Clin Oncol 29:4294–4301. https://doi.org/10.1200/JCO.2011.36.4596
Krane JF (2013) Role of cytology in the diagnosis and management of HPV-associated head and neck carcinoma, Acta Cytol, vol. 57, no. 2, pp. 117–126, doi: 10.1159/000346715. Epub 2013 Feb 28
Venuti A, Paolini F (2012) HPV Detection Methods in Head and Neck Cancer, Head and Neck Pathology, vol. 6, no. S1, pp. 63–74, Jul. https://doi.org/10.1007/s12105-012-0372-5
Kordbacheh F, Farah CS (Jul. 2021) Molecular pathways and druggable targets in Head and Neck squamous cell carcinoma. Cancers 13:3453. https://doi.org/10.3390/cancers13143453
Ang KK, Andratschke NH, Milas L (2004) Epidermal growth factor receptor and response of head-and-neck carcinoma to therapy. Int J Radiat Oncol Biol Phys. ;58(3):959 – 65. https://doi.org/10.1016/j.ijrobp.2003.07.010. PMID: 14967456
Bonner JA et al (2006) Feb., Radiotherapy plus Cetuximab for Squamous-Cell Carcinoma of the Head and Neck, New England Journal of Medicine, vol. 354, no. 6, pp. 567–578, https://doi.org/10.1056/NEJMoa053422
Vermorken JB, Mesia R, Rivera F et al (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 359(11):1116–1127. https://doi.org/10.1056/NEJMoa0802656
Bhatia A, Burtness B (2023) Treating Head and Neck Cancer in the age of Immunotherapy: a 2023 Update. Drugs 83(3):217–248. https://doi.org/10.1007/s40265-023-01835-2Epub 2023 Jan 16. PMID: 36645621
Mei Z, Huang J, Qiao B, Lam AK (Dec. 2020) Immune checkpoint pathways in immunotherapy for head and neck squamous cell carcinoma. Int J Oral Sci 12(1):16. https://doi.org/10.1038/s41368-020-0084-8
Kalbasi A, Ribas A (Jan. 2020) Tumour-intrinsic resistance to immune checkpoint blockade. Nat Rev Immunol 20(1):25–39. https://doi.org/10.1038/s41577-019-0218-4
Saâda-Bouzid E et al (2017) Jul., Hyperprogression during anti-PD-1/PD-L1 therapy in patients with recurrent and/or metastatic head and neck squamous cell carcinoma, Annals of Oncology, vol. 28, no. 7, pp. 1605–1611, https://doi.org/10.1093/annonc/mdx178
Cohen EEW et al (Dec. 2019) The Society for Immunotherapy of Cancer consensus statement on immunotherapy for the treatment of squamous cell carcinoma of the head and neck (HNSCC). J Immunother Cancer 7(1):184. https://doi.org/10.1186/s40425-019-0662-5
Yamashita G, Okamoto I, Ito T, Tokashiki K, Okada T, Tsukahara K (2023) Efficacy of Nivolumab and Pembrolizumab in Platinum-sensitive Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma. Anticancer Res. ;43(8):3679–3683. https://doi.org/10.21873/anticanres.16550. PMID: 37500154
Ordoñez R, Otero A, Jerez I, Medina JA, Lupiañez-Pérez Y, Gomez-Millan J (2019) Role of radiotherapy in the treatment of metastatic head and neck cancer, OncoTargets and Therapy, vol. Volume 12, pp. 677–683, Jan. https://doi.org/10.2147/OTT.S181697
Vishwanath V, Jafarieh S, Rembielak A (2020) The role of imaging in head and neck cancer: an overview of different imaging modalities in primary diagnosis and staging of the disease. J Contemp Brachytherapy 12(5):512–518. https://doi.org/10.5114/jcb.2020.100386
van de Weerd C et al (2023) Jul., Evaluation of a remote monitoring app in head and neck cancer follow-up care, Cancer Medicine, vol. 12, no. 14, pp. 15552–15566, https://doi.org/10.1002/cam4.6202
Bowen DJ et al (2020) Mar., Patient-reported outcomes in the Translational Breast Cancer Research Consortium, Cancer, vol. 126, no. 5, pp. 922–930, https://doi.org/10.1002/cncr.32615
Fleuren MAH, Paulussen TGWM, Van Dommelen P, Van Buuren S (2014) Towards a measurement instrument for determinants of innovations, International Journal for Quality in Health Care, vol. 26, no. 5, pp. 501–510, Oct. https://doi.org/10.1093/intqhc/mzu060
Acknowledgements
ZP acknowledges the funding programme “MEDICUS”, of the University of Patras, Greece.
Funding
This study received no external funding.
Open access funding provided by HEAL-Link Greece.
Author information
Authors and Affiliations
Contributions
N.S.M.: conceptualization, writing the manuscript, literature review, editing; D.S., E.K.: writing contribution, literature review; E.G., E.T. and A.D.: literature review, editing; Z.P.: writing contribution, literature review, editing; N.K.K.: conceptualization, editing, supervision.
Corresponding author
Ethics declarations
Ethical statement
It is not applicable.
Competing interests
No conflicts of interest, financial or otherwise, are declared by the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mastronikolis, N.S., Delides, A., Kyrodimos, E. et al. Insights into metastatic roadmap of head and neck cancer squamous cell carcinoma based on clinical, histopathological and molecular profiles. Mol Biol Rep 51, 597 (2024). https://doi.org/10.1007/s11033-024-09476-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09476-8