Abstract
Background
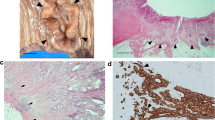
Oral Squamous Cell Carcinoma (OSCC) is a highly prevalent cancer in the Indian subcontinent. The major cause of mortality in OSCC patients is metastasis. Epithelial-to-mesenchymal transition (EMT) marks an important step in the metastatic process. Additionally, TP53, an important tumor suppressor gene, is also a significant determinant of the treatment outcome, and also plays a role in EMT. Therefore, understanding the interconnections between ultrastructural features, EMT status and TP53 mutational status is of vital importance.
Methods and results
The ultrastructure of five OSCC cell lines was visualized by transmission electron microscopy. Trans-well invasion and migration assays as well as scratch-wound assay, and the expression of various EMT-related genes were utilized to assess the EMT status of the cell lines. The TP53 exons were amplified for the ACOSC3, ACOSC4 and ACOSC16 cell lines and sequenced and the mutations in the gene were identified by sequence alignment. The TP53 mutation in the UPCI:SCC029B cell line has been previously reported, while UPCI:SCC040 has been reported to harbor a wild type TP53. The ACOSC4 cell line which showed the shortest intercellular gaps, also had the least invasive and migratory potential. Interestingly, ACOSC4 showed the highest expression of E-cadherin and the lowest expression of Vimentin, TWIST1, ZEB1, and MMPs. Additionally, TP53 gene of ACOSC4 was unmutated, whereas the ACOSC3 and ACOSC16 harbored TP53 mutations. The mutation in ACOSC3 (R196*) was also found in 7 TCGA samples. Similarly, the UPCI:SCC040 cell line that harbors a wild type TP53 showed shorter intracellular gaps.
Conclusions
Cellular migratory properties are associated with cellular ultrastructure, epithelial-to-mesenchymal transition status and the status of TP53 mutation in the genome.




Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Zini A, Czerninski R, Sgan-Cohen HD (2010) Oral cancer over four decades : epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. https://doi.org/10.1111/j.1600-0714.2009.00845.x
García-martín JM, Varela P, González M, Seoane JM (2019) Epidemiology of oral cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-61255-3
Zhang SZ, Xie L, Shang ZJ (2022) Burden of oral cancer on the 10 most populous countries from 1990 to 2019: estimates from the global burden of disease study 2019. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19020875
Chaffer CL, Weinberg RA (2011) A perspective on cancer cell metastasis. Science. https://doi.org/10.1126/science.1203543
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial-mesenchymal transition. Nature Publishing Group, New York, pp 178–196. https://doi.org/10.1038/nrm3758
Boyden S (1962) The chemotactic effect of mixtures of antibody and antigen on polymorphonuclear leucocytes. J Exp Med. https://doi.org/10.1084/jem.115.3.453
Corey G (2011) Scratch-wound assay. In: Wells CM, Parsons M, Wells C, Parsons M (eds) Cell migration. Springer, Berlin, pp 25–30
Bravo-cordero JJ, Hodgson L, Condeelis J (2012) Directed cell invasion and migration during metastasis. Curr Opin Cell Biol 24:277–283. https://doi.org/10.1016/j.ceb.2011.12.004
Yilmaz M, Christofori G (2009) EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastasis Rev. https://doi.org/10.1007/s10555-008-9169-0
Ivaska J, Pallari H, Nevo J, Eriksson JE (2007) Novel functions of vimentin in cell adhesion, migration, and signaling. Exp Cell Res. https://doi.org/10.1016/j.yexcr.2007.03.040
Vuoriluoto K, Haugen H, Kiviluoto S, Mpindi J, Nevo J, Gjerdrum C, Tiron C, Lorens JB, Ivaska J (2011) Vimentin regulates EMT induction by slug and oncogenic H-Ras and migration by governing Axl expression in breast cancer. Oncogene. https://doi.org/10.1038/onc.2010.509
Chang CJ, Chao CH, Xia W, Yang JY, Xiong Y, Li CW, Yu WH, Rehman SK, Hsu JL, Lee HH, Liu M, Chen C, Te, Yu D, Hung MC (2011) P53 regulates epithelial-mesenchymal transition and stem cell properties through modulating miRNAs. Nat Cell Biol. https://doi.org/10.1038/ncb2173
Dong P, Karaayvaz M, Jia N, Kaneuchi M, Hamada J, Watari H, Sudo S, Ju J, Sakuragi N (2013) Mutant p53 gain-of-function induces epithelial-mesenchymal transition through modulation of the miR-130b-ZEB1 axis. Oncogene 32:3286–3295. https://doi.org/10.1038/onc.2012.334
Whibley C, Pharoah PDP, Hollstein M (2009) p53 polymorphisms : cancer implications. Nat Rev Cancer. https://doi.org/10.1038/nrc2584
Vousden KH, Lane DP (2007) p53 in health and disease. Nat Rev Mol Cell Biol 8:275–283. https://doi.org/10.1038/nrm2147
Vogelstein B, Kinzler KW (2004) Cancer genes and the pathways they control. Nat Med. 10:789–799. https://doi.org/10.1038/nm1087
Gawas NP, Navarange SS, Chovatiya GL, Chaturvedi P, Waghmare SK (2019) Establishment and characterization of novel human oral squamous cell carcinoma cell lines from advancedstage tumors of buccal mucosa. Oncol Rep 41:2289–2298. https://doi.org/10.3892/or.2019.7003
Telmer CA, An J, Malehorn DE, Zeng X, Gollin SM, Ishwad CS, Jarvik JW (2003) Detection and assignment of TP53 mutations in tumor DNA using peptide mass signature genotyping. Hum Mutat 22:158–165. https://doi.org/10.1002/humu.10248
White JS, Weissfeld JL, Ragin CCR, Rossie KM, Martin CL, Shuster M, Ishwad CS, Law JC, Myers EN, Johnson JT, Gollin SM (2007) The influence of clinical and demographic risk factors on the establishment of head and neck squamous cell carcinoma cell lines. Oral Oncol 43:701–712. https://doi.org/10.1016/j.oraloncology.2006.09.001
Suarez-Arnedo A, Figueroa FT, Clavijo C, Arbeláez P, Cruz JC, Muñoz-Camargo C (2020) An image J plugin for the high throughput image analysis of in vitro scratch wound healing assays. PLoS ONE. https://doi.org/10.1371/journal.pone.0232565
Rivlin N, Brosh R, Oren M, Rotter V (2011) Mutations in the p53 tumor suppressor gene: important milestones at the various steps of tumorigenesis. Genes Cancer 2:466–474
Sánchez-Tilló E, Lázaro A, Torrent R, Cuatrecasas M, Vaquero EC, Castells A, Engel P, Postigo A (2010) ZEB1 represses E-cadherin and induces an EMT by recruiting the SWI/SNF chromatin-remodeling protein BRG1. Oncogene. https://doi.org/10.1038/onc.2010.102
Liu S, Liu L, Ye W, Ye D, Wang T, Guo W, Liao Y, Xu D, Song H, Zhang L, Zhu H, Deng J, Zhang Z (2016) High vimentin expression associated with lymph node metastasis and predicated a poor prognosis in oral squamous cell carcinoma. Sci Rep. https://doi.org/10.1038/srep38834
Duan Y, He Q, Yue K, Si H, Wang J, Zhou X, Wang X (2017) Hypoxia induced Bcl-2/Twist1 complex promotes tumor cell invasion in oral squamous cell carcinoma. Oncotarget. https://doi.org/10.18632/oncotarget.13890
Hashiguchi Y, Kawano S, Goto Y, Yasuda K, Kaneko N, Sakamoto T, Matsubara R, Jinno T, Maruse Y, Tanaka H, Morioka M, Hattori T, Tanaka S, Kiyoshima T, Nakamura S (2018) Tumor-suppressive roles of ∆Np63β-miR-205 axis in epithelial-mesenchymal transition of oral squamous cell carcinoma via targeting ZEB1 and ZEB2. J Cell Physiol 233:6565–6577. https://doi.org/10.1002/jcp.26267
Yu T, Wu Y, Helman JI, Wen Y, Wang C, Li L (2011) CXCR4 promotes oral squamous cell carcinoma migration and invasion through inducing expression of MMP-9 and MMP-13 via the ERK signaling pathway. Mol Cancer Res 9:161–172. https://doi.org/10.1158/1541-7786.MCR-10-0386
Takahara T, Kasamatsu A, Yamatoji M, Iyoda M, Kasama H, Saito T, Takeuchi S, Endo-Sakamoto Y, Shiiba M, Tanzawa H, Uzawa K (2017) SIPA1 promotes invasion and migration in human oral squamous cell carcinoma by ITGB1 and MMP7. Exp Cell Res 352:357–363. https://doi.org/10.1016/J.YEXCR.2017.02.026
Lu L, Xue X, Lan J, Gao Y, Xiong Z, Zhang H, Jiang W, Song W, Zhi Q (2014) MicroRNA-29a upregulates MMP2 in oral squamous cell carcinoma to promote cancer invasion and anti-apoptosis. Biomed Pharmacother 68:13–19. https://doi.org/10.1016/J.BIOPHA.2013.10.005
Ganly AI (2000) p53 alterations in recurrent squamous cell cancer of the head and neck refractory to radiotherapy. Br J Cancer. https://doi.org/10.1054/bjoc.1999.0932
Acknowledgements
We thank the ACTREC Digital Imaging, Electron Microscopy and Sequencing facilities. We thank Prof Susanne M Gollin, University of Pittsburg, USA for providing the UPCI:SCC029B and UPCI:SCC040 cell lines.
Funding
Sushant S Navarange is supported by Council of Scientific and Industrial Research (CSIR) fellowship. Darshan Mehta is supported by ACTREC fellowship. The present study was supported from the grant of ACTREC-TMC intramural fund (Grant No. 3542) and Department of Atomic Energy (DAE), Government of India (Grant No. 4598).
Author information
Authors and Affiliations
Contributions
SKW conceived and designed the study. Material preparation, data collection and analysis was performed by SSN, DM, SB, SGS, SKW and SG. SKW reviewed the data and the manuscript. The first draft of the manuscript was written by SSN and SKW. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All the three cell lines such as ACOSC3, ACOSC4 and ACOSC16, were established from the oral cancer patient samples from Tata Memorial Centre. This study was performed in line with the principles of Helsinki. Approval was granted by the Institutional Human Ethics Committee (Dated: December 14, 2015–IEC/188).
Consent to participant
Informed consent was obtained from all the individual participants included in the study. This study was approved by the Institutional Human Ethics Committee.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the images in this manuscript.
Additional information
Publisher’s Note
Springer nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Navarange, S.S., Bane, S.M., Mehta, D. et al. Epithelial-to-mesenchymal transition status correlated with ultrastructural features, and TP53 mutation in patient-derived oral cancer cell lines. Mol Biol Rep 50, 8469–8481 (2023). https://doi.org/10.1007/s11033-023-08720-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08720-x