Abstract
Background
On the background of the epidemiological link between diabetes and oral cancer, the present study aimed to analyze the potential involvement of selected glucose transporters (GLUT1/GLUT3/GLUT4), if any, in such putative association.
Methods and results
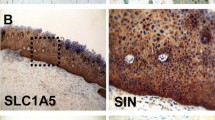
Oral carcinogenesis was induced by 4-nitroquinoline N-oxide in 10 non-diabetic and 10 diabetic rats; 8 non-diabetic and 7 diabetic rats served as controls. Expressions of selected GLUTs at mRNA and protein levels were analyzed in oral tissue (normal/lesion) by quantitative real-time PCR and immunohistochemistry respectively. Premalignant lesions (hyperplasia/dysplasia/carcinoma-in-situ) appeared on tongues of carcinogen-treated animals. Significant increase of GLUT1mRNA level was seen from normal to lesion tongues, along increasing lesion grades (from hyperplasia/mild dysplasia to moderate/severe dysplasia) and in lesions induced under hyperglycemic condition than that induced under normoglycemic one; a similar trend was found in transcript variant-1 of GLUT1, but not in variant-2. GLUT3 and GLUT4 mRNA levels were comparable among lesions irrespective of grades and glycemic status. Concordant to mRNA level, overall expression of GLUT1 protein was higher in tongue lesions in presence of hyperglycemia than in absence of such condition; non-lesion portions of tongues exposed to carcinogen showed a similar trend. Moreover in carcinogen-treated groups, non-lesion and lesion portions of tongues under hyperglycemic condition showed predominantly membranous expression for GLUT1 which was again significantly higher than equivalent portions of tongue under normoglycemic condition.
Conclusion
Hyperglycemia seemed to favor GLUT1 over-expression and membrane localization of the protein during oral carcinogenesis. GLUT1 transcript variant-1 appeared to be more important than variant-2 in disease pathogenesis.





Similar content being viewed by others
References
Mauri-Obradors E, Estrugo-Devesa A, Jané-Salas E, Viñas M, López-López J (2017) Oral manifestations of diabetes mellitus. A systematic review. Med Oral Patol Oral Cir Bucal 22(5):e586–e594
Cervino G, Fiorillo L, Laino L, Herford AS, Lauritano F, Giudice GL, Famà F, Santoro R, Troiano G, Iannello G, Cicciù M (2018) Oral health impact profile in celiac patients: analysis of recent findings in a literature review. Gastroenterol Res Pract 2018:7848735
Cohn A, Sofia AM, Kupfer SS (2014) Type 1 diabetes and celiac disease: clinical overlap and new insights into disease pathogenesis. Curr Diab Rep 14(8):517
Seethalakshmi C, Reddy RC, Asifa N, Prabhu S (2016) Correlation of salivary pH, incidence of dental caries and periodontal status in diabetes mellitus patients: a cross-sectional study. J Clin Diagn Res 10(3):ZC12–ZC14
Gandara BK, Morton TH (2011) Non-periodontal oral manifestations of diabetes: a framework for medical care providers. Diabetes Spectr 24(4):199–205
Cervino G, Terranova A, Briguglio F, De Stefano R, Famà F, D’Amico C, Amoroso G, Marino S, Gorassini F, Mastroieni R, Scoglio C, Catalano F, Lauritano F, Matarese M, Lo Giudice R, Nastro Siniscalchi E, Fiorillo L (2019) Diabetes: oral health related quality of life and oral alterations. Biomed Res Int 2019:5907195
Al-Maskari AY, Al-Maskari MY, Al-Sudairy S (2011) Oral manifestations and complications of diabetes mellitus: a review. Sultan Qaboos Univ Med J 11(2):179–186
Dikshit RP, Ramadas K, Hashibe M, Thomas G, Somanathan T, Sankaranarayanan R (2006) Association between diabetes mellitus and pre-malignant oral diseases: a cross sectional study in Kerala, India. Int J Cancer 118(2):453–457
Ujpál M, Matos O, Bíbok G, Somogyi A, Szabó G, Suba Z (2004) Diabetes and oral tumors in Hungary: epidemiological correlations. Diabetes Care 27(3):770–774
Basu R, Mandal S, Ghosh A, Poddar TK (2008) Role of tobacco in the development of head and neck squamous cell carcinoma in an eastern Indian population. Asian Pac J Cancer Prev 9(3):381–386
Jiang X, Wu J, Wang J, Huang R (2019) Tobacco and oral squamous cell carcinoma: a review of carcinogenic pathways. Tob Induc Dis 12:29
Vairaktaris E, Kalokerinos G, Goutzanis L, Spyridonidou S, Vassiliou S, Derka S, Nkenke E, Yapijakis C, Vylliotis A, Lazaris A, Patsouris E (2007) Diabetes alters expression of p53 and c-myc in different stages of oral oncogenesis. Anticancer Res 27(3B):1465–1473
Goutzanis L, Vairaktaris E, Yapijakis C, Kavantzas N, Nkenke E, Derka S, Vassiliou S, Acil Y, Kessler P, Stavrianeas N, Perrea D, Donta I, Skandalakis P, Patsouris E (2007) Diabetes may increase risk for oral cancer through the insulin receptor substrate-1 and focal adhesion kinase pathway. Oral Oncol 43(2):165–173
Fantin VR, St-Pierre J, Leder P (2006) Attenuation of LDH-A expression uncovers a link between glycolysis, mitochondrial physiology, and tumor maintenance. Cancer Cell 9(6):425–434
García-Jiménez C, García-Martínez JM, Chocarro-Calvo A, De la Vieja A (2013) A new link between diabetes and cancer: enhanced WNT/β-catenin signaling by high glucose. J Mol Endocrinol 52(1):R51-66
Wood IS, Trayhurn P (2003) Glucose transporters (GLUT and SGLT): expanded families of sugar transport proteins. Br J Nutr 89:3–9
Macheda ML, Rogers S, Best JD (2005) Molecular and cellular regulation of glucose transporter (GLUT) proteins in cancer. J Cell Physiol 202(3):654–662
Angadi VC, Angadi PV (2015) GLUT-1 immunoexpression in oral epithelial dysplasia, oral squamous cell carcinoma, and verrucous carcinoma. J Oral Sci 57(2):115–122
Ohba S, Fujii H, Ito S, Fujimaki M, Matsumoto F, Furukawa M, Yokoyama J, Kusunoki T, Ikeda K, Hino O (2010) Overexpression of GLUT-1 in the invasion front is associated with depth of oral squamous cell carcinoma and prognosis. J Oral Pathol Med 39(1):74–78
Fukuzumi M, Hamakawa H, Onishi A, Sumida T, Tanioka H (2000) Gene expression of GLUT isoforms and VHL in oral squamous cell carcinoma. Cancer Lett 161(2):133–140
Demeda CF, Carvalho CH, Aquino AR, Nonaka CF, Souza LB, Pinto LP (2014) Expression of glucose transporters 1 and 3 in metastatic and non-metastatic lower lip squamous cell carcinoma. Braz Dent J 25(5):372–378
Starska K, Forma E, Jóźwiak P, Bryś M, Lewy-Trenda I, Brzezińska-Błaszczyk E, Krześlak A (2015) Gene and protein expression of glucose transporter 1 and glucose transporter 3 in human laryngeal cancer-the relationship with regulatory hypoxia-inducible factor-1α expression, tumor invasiveness, and patient prognosis. Tumour Biol 36(4):2309–2321
Feitosa SG, Viana KF, Luna ECM, Costa FWG, Cavalcante RB, Chaves FN, Chaves HV, Pereira KMA (2018) Immunohistochemical evaluation of GLUT-3 and GLUT-4 in oral epithelial dysplasia and oral squamous cell carcinoma. Asian Pac J Cancer Prev 19(7):1779–1783
Kanojia D, Vaidya MM (2006) 4-Nitroquinoline-1-oxide induced experimental oral carcinogenesis. Oral Oncol 42(7):655–667
Amawi KF, Alkhatib AJ (2020) Urtica pilulifera in treating pre-diabetic rat model to control the blood glucose, lipids and oxidative stress. Med Arch 74(3):168–171
Tamura I, Sakaki T, Chaqour B, Howard PS, Ikeo T, Macarak EJ (2003) Correlation of P-cadherin and beta-catenin expression and phosphorylation with carcinogenesis in rat tongue cancer induced with 4-nitroquinoline 1-oxide. Oral Oncol 39(5):506–514
Ranganathan K, Kavitha L (2019) Oral epithelial dysplasia: classifications and clinical relevance in risk assessment of oral potentially malignant disorders. J Oral Maxillofac Pathol 23(1):19–27
Moon SM, Ahn MY, Kwon SM, Kim SA, Ahn SG, Yoon JH (2012) Homeobox C5 expression is associated with the progression of 4-nitroquinoline 1-oxide-induced rat tongue carcinogenesis. J Oral Pathol Med 41(6):470–476
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25(4):402–408
Perrone F, Suardi S, Pastore E, Casieri P, Orsenigo M, Caramuta S, Dagrada G, Losa M, Licitra L, Bossi P, Staurengo S, Oggionni M, Locati L, Cantu G, Squadrelli M, Carbone A, Pierotti MA, Pilotti S (2006) Molecular and cytogenetic subgroups of oropharyngeal squamous cell carcinoma. Clin Cancer Res 12(22):6643–6651
Ribeiro DA, Fracalossi ACC, Gomes TS, Oshima CTF (2009) COX-2 expression during 4-nitroquinoline 1-oxide induced rat tongue carcinogenesis. Basic Appl Pathol 2:9–14
Schwartzenberg-Bar-Yoseph F, Armoni M, Karnieli E (2004) The tumor suppressor p53 down-regulates glucose transporters GLUT1 and GLUT4 gene expression. Cancer Res 64:2627–2633
Shahnavaz SA, Regezi JA, Bradley G, Dubé ID, Jordan RC (2000) p53 gene mutations in sequential oral epithelial dysplasias and squamous cell carcinomas. J Athol 190(4):417–422
Wang G, Guo X, Floros J (2003) Human SP-A 3′-UTR variants mediate differential gene expression in basal levels and in response to dexamethasone. Am J Physiol Lung Cell Mol Physiol 284(5):L738-748
Maiti GP, Ghosh A, Mondal P, Baral A, Datta S, Samadder S, Nayak SP, Chakrabarti J, Biswas J, Sikdar N, Chowdhury S, Roy B, Roychowdhury S, Panda CK (2015) SNP rs1049430 in the 3′-UTR of SH3GL2 regulates its expression: clinical and prognostic implications in head and neck squamous cell carcinoma. Biochim Biophys Acta 1852(5):1059–1067
Mamun AA, Hayashi H, Yamamura A, Nayeem MJ, Sato M (2020) Hypoxia induces the translocation of glucose transporter 1 to the plasma membrane in vascular endothelial cells. J Physiol Sci 22(1):44
Kujan O, Shearston K, Farah CS (2017) The role of hypoxia in oral cancer and potentially malignant disorders: a review. J Oral Pathol Med 46(4):246–252
Jóźwiak P, Krześlak A, Bryś M, Lipińska A (2015) Glucose-dependent glucose transporter 1 expression and its impact on viability of thyroid cancer cells. Oncol Rep 33(2):913–920
Acknowledgements
We are thankful to the Hon’ble Vice Chancellor, Presidency University Kolkata, India. Financial support for this work was provided by Department of Higher Education Science & Technology and Biotechnology [793(Sanc.)/ST/P/S&T/1G-2/2016, Dt. 06/12/2016] to Dr. Amlan Ghosh.
Author information
Authors and Affiliations
Contributions
SD and JA did RTPCR, immunohistochemistry and analyzed the data. SD wrote the first draft of the manuscript. JA did statistical analyses and wrote the manuscript. AR did histological analyses and associated diagnostic evaluation of tongue lesions. Animal experimentation and associated data analysis was done under supervision of SSB and PM. SA did statistical analysis and critically reviewed the manuscript. AG conceived the study design, interpreted overall data and prepared the final version of the manuscript. All authors approved the final draft of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declared any conflict of interest relevant to the content of this article.
Ethical approval
The study was approved by the Institutional Animal Ethical Committee of Presidency University registered under Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), India.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dalal, S., Adhikary, J., Roy, A. et al. Impact of hyperglycemia on the expression of GLUT1 during oral carcinogenesis in rats. Mol Biol Rep 49, 8369–8380 (2022). https://doi.org/10.1007/s11033-022-07653-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07653-1