Abstract
Background
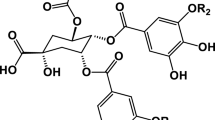
Nuclear factor-κB (NF-κB) has been identified as the major link between inflammation and cancer. Natural agents that inhibit this pathway are essential in attenuating inflammation induced by cancer or chemotherapeutic drugs. High intake of Brassicaceae vegetables has been determined to modulate essential pathways related to chronic diseases. In this study, we investigated the anti-proliferative and anti-inflammatory effects of the indole glucosinolates; indole-3-carbinol (I3C) and its metabolite 3,3-diindolylmethane (DIM) on the inflammatory biomarkers and miRNAs controlling the NF-κB pathway.
Methods and results
In our study, we inoculated Ehrlich ascites carcinoma (EAC) cells in female albino mice, which increased their packed cell volume and induced a significant increase in the levels of several cytokines and inflammatory biomarkers (NF-κB IL-6, IL-1b, TNF-α, and NO). A significant elevation in inflammatory-medicated miRNAs (miR-31 and miR-21) was also noted. Treatment with 5-fluorouracil (5-FU) significantly reduced packed cell volume and viable cell count. However, it was accompanied by a significant increase in the levels of inflammatory markers and expression of miR-31 and miR-21. Nevertheless, although treatment with indoles (I3C and DIM) significantly reduced the packed cell volume and viable cell count, their prominent effect was the marked reduction of all inflammatory biomarkers compared to both the EAC untreated group and the EAC group treated with 5-FU. Moreover, the anti-inflammatory effect of I3C or DIM was accompanied by a significant decrease in the expression of miR-31 and miR-21.
Conclusion
Our findings have; therefore, revealed that I3C and DIM have strong anti-inflammatory effects, implying that their use as a co-treatment with chemotherapeutic drugs can effectively improve the anti-tumor effect of chemotherapeutic drugs.



Similar content being viewed by others
Consent to publish
All authors mutually agree to forward this manuscript for submission. All authors discussed the results and contributed to the final form of the manuscript. We affirm that the submitted manuscript has not been previously published in any language anywhere and is not submitted for publication elsewhere.
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. https://doi.org/10.3322/caac.21492
Abo-Zeid MAM, Liehr T, El-Daly SM et al (2013) Molecular cytogenetic evaluation of the efficacy of photodynamic therapy by indocyanine green in breast adenocarcinoma MCF-7 cells. Photodiagn Photodyn Ther. https://doi.org/10.1016/j.pdpdt.2012.11.006
Didonato JA, Mercurio F, Karin M (2012) NF-κB and the link between inflammation and cancer. Immunol Rev. https://doi.org/10.1111/j.1600-065X.2012.01099.x
Wu J, Ding J, Yang J et al (2018) MicroRNA roles in the nuclear factor kappa B signaling pathway in cancer. Front Immunol 9:546
Maione F, Russo R, Khan H, Mascolo N (2016) Medicinal plants with anti-inflammatory activities. Nat Prod Res 30(12):1343–1352
Rayan A, Raiyn J, Falah M (2017) Nature is the best source of anticancer drugs: indexing natural products for their anticancer bioactivity. PLoS ONE. https://doi.org/10.1371/journal.pone.0187925
Agerbirk N, De Vos M, Kim JH, Jander G (2009) Indole glucosinolate breakdown and its biological effects. Phytochem Rev 8:101
Fuentes F, Paredes-Gonzalez X, Kong ANT (2015) Dietary glucosinolates sulforaphane, phenethyl isothiocyanate, indole-3-carbinol/3,3′-diindolylmethane: antioxidative stress/inflammation, Nrf2, epigenetics/epigenomics and in vivo cancer chemopreventive efficacy. Curr Pharmacol Rep 1(3):179–196
El-Daly SM, Gamal-Eldeen AM, Gouhar SA et al (2020) Modulatory effect of indoles on the expression of miRNAs regulating G1/S cell cycle phase in breast cancer cells. Appl Biochem Biotechnol 192:1208–1223. https://doi.org/10.1007/s12010-020-03378-8
Montgomery M, Srinivasan A (2019) Epigenetic gene regulation by dietary compounds in cancer prevention. Adv Nutr 10(6):1012–1028
Ozaslan M, Karagoz I, Kilic I, Guldur M (2013) Ehrlich ascites carcinoma. Afr J Biotechnol. https://doi.org/10.5897/AJBx10.017
Chen L, Watkins JF (1970) Evidence against the presence of H2 histocompatibility antigens in Ehrlich ascites tumour cells. Nature. https://doi.org/10.1038/225734a0
Mishra S, Tamta AK, Sarikhani M et al (2018) Subcutaneous Ehrlich Ascites Carcinoma mice model for studying cancer-induced cardiomyopathy. Sci Rep. https://doi.org/10.1038/s41598-018-23669-9
Medhat D, Hussein J, El-Naggar ME et al (2017) Effect of Au-dextran NPs as anti-tumor agent against EAC and solid tumor in mice by biochemical evaluations and histopathological investigations. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2017.05.043
Vincent PC, Nicholls A (1967) Comparison of the growth of the Ehrlich ascites tumor in male and female mice. Cancer Res 27(6):1058–1065
Yasuda M, Kato S, Yamanaka N et al (2013) 5-HT3 receptor antagonists ameliorate 5-fluorouracil-induced intestinal mucositis by suppression of apoptosis in murine intestinal crypt cells. Br J Pharmacol 168:1388–1400. https://doi.org/10.1111/bph.12019
Grubbs CJ, Steele VE, Casebolt T et al (1995) Chemoprevention of chemically-induced mammary carcinogenesis by indole-3-carbinol. Anticancer Res 15(3):709–716
Gao N, Cheng S, Budhraja A et al (2012) 3, 3′-Diindolylmethane exhibits antileukemic activity in vitro and in vivo through a Akt-dependent process. PLoS ONE. https://doi.org/10.1371/journal.pone.0031783
Reed GA, Sunega JM, Sullivan DK et al (2008) Single-dose pharmacokinetics and tolerability of absorption-enhanced 3,3′-diindolylmethane in healthy subjects. Cancer Epidemiol Biomark Prev. https://doi.org/10.1158/1055-9965.EPI-08-0520
Howells LM, Moiseeva EP, Neal CP et al (2007) Predicting the physiological relevance of in vitro cancer preventive activities of phytochemicals. Acta Pharmacol Sin 28(9):1274–1304
Moshage H, Kok B, Huizenga JR, Jansen PLM (1995) Nitrite and nitrate determinations in plasma: a critical evaluation. Clin Chem 41:892–896. https://doi.org/10.1093/clinchem/41.6.892
Passing H, Bablok W (2009) A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in Clinical Chemistry, Part I. Clin Chem Lab Med 21:709–720. https://doi.org/10.1515/cclm.1983.21.11.709
El-Daly SM, Hussein J (2019) Genetically engineered CAR T-immune cells for cancer therapy: recent clinical developments, challenges, and future directions. J Appl Biomed. https://doi.org/10.32725/jab.2019.005
Greten FR, Grivennikov SI (2019) Inflammation and cancer: triggers, mechanisms, and consequences. Immunity 51(1):27–41
Ben-Neriah Y, Karin M (2011) Inflammation meets cancer, with NF-κB as the matchmaker. Nat Immunol 12(8):715–723
El-Daly SM, Medhat D, El-Bana M et al (2021) Stimulatory effect of docosahexaenoic acid alone or loaded in zinc oxide or silver nanoparticles on the expression of glucose transport pathway. Prostaglandins Other Lipid Mediat. https://doi.org/10.1016/j.prostaglandins.2021.106566
Esteve M (2020) Mechanisms underlying biological effects of cruciferous glucosinolate-derived isothiocyanates/indoles: a focus on metabolic syndrome. Front Nutr 7:111
Biersack B (2020) 3,3’-Diindolylmethane and its derivatives: nature-inspired strategies tackling drug resistant tumors by regulation of signal transduction, transcription factors and microRNAs. Cancer Drug Resist. https://doi.org/10.20517/cdr.2020.53
An Q, Robins P, Lindahl T, Barnes DE (2007) 5-Fluorouracil incorporated into DNA is excised by the Smug1 DNA glycosylase to reduce drug cytotoxicity. Cancer Res. https://doi.org/10.1158/0008-5472.CAN-06-2960
Zhang N, Yin Y, Xu SJ, Chen WS (2008) 5-Fluorouracil: mechanisms of resistance and reversal strategies. Molecules 13(8):1551–1569
Groves TR, Farris R, Anderson JE et al (2017) 5-Fluorouracil chemotherapy upregulates cytokines and alters hippocampal dendritic complexity in aged mice. Behav Brain Res. https://doi.org/10.1016/j.bbr.2016.08.039
Chang CT, Ho TY, Lin H et al (2012) 5-Fluorouracil induced intestinal mucositis via nuclear factor-κB activation by transcriptomic analysis and in vivo bioluminescence imaging. PLoS ONE 7:1–8. https://doi.org/10.1371/journal.pone.0031808
De Sousa FL, De Miranda JAL, Da Silva MC et al (2020) Role of rutin in 5-fluorouracil-induced intestinal mucositis: prevention of histological damage and reduction of inflammation and oxidative stress. Molecules. https://doi.org/10.3390/molecules25122786
Reed GA, Arneson DW, Putnam WC et al (2006) Single-dose and multiple-dose administration of indole-3-carbinol to women: pharmacokinetics based on 3,3′-diindolylmethane. Cancer Epidemiol Biomark Prev 15:2477–2481. https://doi.org/10.1158/1055-9965.EPI-06-0396
Bradlow HL, Zeligs MA (2010) Diindolylmethane (DIM) spontaneously forms from indole-3-carbinol (I3C) during cell culture experiments. In Vivo (Brooklyn) 24(4):387–391
Kim HW, Kim J, Kim J et al (2014) 3,3’-Diindolylmethane inhibits lipopolysaccharide-induced microglial hyperactivation and attenuates brain inflammation. Toxicol Sci. https://doi.org/10.1093/toxsci/kft240
Xiao C, Ghosh S (2005) NF-κB, an evolutionarily conserved mediator of immune and inflammatory responses. Adv Exp Med Biol 560:41–45
Yamamoto Y, Gaynor RB (2004) IκB kinases: key regulators of the NF-κB pathway. Trends Biochem Sci 29(2):72–79
Natarajan K, Abraham P, Kota R, Isaac B (2018) NF-κB-iNOS-COX2-TNF α inflammatory signaling pathway plays an important role in methotrexate induced small intestinal injury in rats. Food Chem Toxicol. https://doi.org/10.1016/j.fct.2018.06.040
El-Daly SM, Abba ML, Patil N, Allgayer H (2016) miRs-134 and-370 function as tumor suppressors in colorectal cancer by independently suppressing EGFR and PI3K signalling. Sci Rep. https://doi.org/10.1038/srep24720
El-Daly SM, Bayraktar R, Anfossi S, Calin GA (2020) The interplay between microRNAs and the components of the tumor microenvironment in B-cell malignancies. Int J Mol Sci 21(9):3387
El-Daly SM, Abba ML, Gamal-Eldeen AM (2017) The role of microRNAs in photodynamic therapy of cancer. Eur J Med Chem. https://doi.org/10.1016/j.ejmech.2017.10.011
El-Daly SM, Omara EA, Hussein J et al (2019) Differential expression of miRNAs regulating NF-κB and STAT3 crosstalk during colitis-associated tumorigenesis. Mol Cell Probes. https://doi.org/10.1016/j.mcp.2019.101442
El-Daly SM, Morsy SM, Medhat D et al (2019) The diagnostic efficacy of circulating miRNAs in monitoring the early development of colitis-induced colorectal cancer. J Cell Biochem 120:16668–16680. https://doi.org/10.1002/jcb.28925
Winkle M, El-Daly SM, Fabbri M, Calin GA (2021) Noncoding RNA therapeutics—challenges and potential solutions. Nat Rev Drug Discov. https://doi.org/10.1038/s41573-021-00219-z
Wang H, Tan Z, Hu H et al (2019) MicroRNA-21 promotes breast cancer proliferation and metastasis by targeting LZTFL1. BMC Cancer. https://doi.org/10.1186/s12885-019-5951-3
El-Daly SM, Gouhar SA, Gamal-Eldeen AM et al (2019) Synergistic effect of α-solanine and cisplatin induces apoptosis and enhances cell cycle arrest in human hepatocellular carcinoma cells. Anticancer Agents Med Chem. https://doi.org/10.2174/1871520619666190930123520
Yang Z, Fang S, Di Y et al (2015) Modulation of NF-κB/miR-21/PTEN pathway sensitizes non-small cell lung cancer to cisplatin. PLoS ONE. https://doi.org/10.1371/journal.pone.0121547
Shi J, Ma X, Su Y et al (2018) miR-31 mediates inflammatory signaling to promote re-epithelialization during skin wound healing. J Investig Dermatol. https://doi.org/10.1016/j.jid.2018.03.1521
Yan S, Xu Z, Lou F et al (2015) NF-κB-induced microRNA-31 promotes epidermal hyperplasia by repressing protein phosphatase 6 in psoriasis. Nat Commun. https://doi.org/10.1038/ncomms8652
Yu T, Ma P, Wu D et al (2018) Functions and mechanisms of microRNA-31 in human cancers. Biomed Pharmacother 108:1162–1169. https://doi.org/10.1016/j.biopha.2018.09.132
Funding
This research was partially supported by the National Research Centre, Cairo, Egypt (Grant No. 11010332, PI; Sherien M. El-Daly).
Author information
Authors and Affiliations
Contributions
El-Daly S.M., Fathy S.A., Mohamed R.M., and El-Khayat Z. developed the idea and planned the work. Salem A.Z., Medhat D., and El-Daly S.M., performed the required experiments. Medhat D., El-Daly S.M., and Salem A.Z. wrote the manuscript in consultation with El-Khayat Z., Fathy S.A., Mohamed R.M. participated in drafting the article and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All animal procedures of the current protocol were approved by the Animal Ethics Committee of the National Research Centre, Cairo, Egypt.
Informed consent
We verify a significant contribution from all the authors listed on the title page, and that they are fully aware of the manuscript's content, verify that the data and its interpretation are valid and legitimate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salem, A.Z., Medhat, D., Fathy, S.A. et al. Indole glucosinolates exhibit anti-inflammatory effects on Ehrlich ascites carcinoma cells through modulation of inflammatory markers and miRNAs. Mol Biol Rep 48, 6845–6855 (2021). https://doi.org/10.1007/s11033-021-06683-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06683-5