Abstract
The aim is to investigate the relationship between serum coagulation parameters (PT, APTT, D-D and FDP) before hospitalization and recurrence of chronic subdural hematoma (CSDH). 236 patients with CSDH who were diagnosed for the first time and had complete medical records were followed up for at least 90 days. Fifty patients (21.2%) had relapsed. Univariate analysis was conducted including general data, imaging data and test results. Serum coagulation parameters (PT, APTT, D–D and FDP) were detected for all CSDH patients. The study identified several factors that exhibited a significant correlation with chronic subdural hematoma (CSDH) recurrence. These factors included advanced age (p = 0.01), hypertension (p = 0.04), liver disease (p = 0.01), anticoagulant drug use (p = 0.01), antiplatelet drug use (p = 0.02), bilateral hematoma (p = 0.02), and single-layer hematoma (p = 0.01). In addition, the presence of fibrin/fibrinogen degradation products (FDP) exceeding 5 mg/L demonstrated a significant relationship with CSDH recurrence (P < 0.05). Notably, the combined assessment of D-dimer (D–D) and FDP exhibited a significant difference, particularly regarding recurrence within 30 days after surgery (P < 0.05). The simultaneous elevation of serum FDP and D–D levels upon admission represents a potentially novel predictor for CSDH recurrence. This finding is particularly relevant for patients who experience recurrence within 30 days following surgical intervention. Older individuals with CSDH who undergo trepanation and drainage should be closely monitored due to their relatively higher recurrence rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (CSDH) refers to the accumulation of fluid, blood, and degraded blood products between the dura and arachnoid membranes that envelop the brain’s surface. The global annual incidence of CSDH ranges from approximately 1.7 to 20.6 cases per 100,000 individuals, with a significant increase in incidence associated with advancing age (8 to 58 cases per 100,000 in individuals aged 65 years and older) [1, 2]. The mean age of onset is reported to be 76.8 years [3]. It is projected that by 2030, CSDH removal will become the most common neurosurgical procedure performed on adults in the United States.
The occurrence and progression of CSDH are linked to the increased permeability of abnormal blood vessels, the release of inflammatory mediators, and local coagulation mechanisms. Surgical evacuation of the subdural hematoma remains the primary treatment for symptomatic patients. The recurrence rate of CSDH ranges from 10.9 to 26.3% [3]. Recurrence poses a significant financial burden on individuals and society as a whole.
Although the precise mechanisms underlying the development of CSDH are not fully understood, several potential pathogenic processes have been investigated. Despite the availability of relatively systematic and standardized surgical methods and drug therapies for CSDH, the recurrence rate after treatment remains relatively high. Therefore, early identification of patients prone to CSDH recurrence holds great significance.
Several factors have been identified as being associated with CSDH recurrence, including male gender, advanced age, history of alcohol abuse, diabetes, renal failure, liver disease, use of anticoagulant or antiplatelet agents, and specific imaging findings of the hematoma.
In contrast, hematological parameters such as fibrinogen, neutrophils, eosinophils, and serum coagulation-related factors have been linked to infarct size, hemorrhage in cerebrovascular diseases (including cerebral hemorrhage or cerebral infarction), and the prognosis of affected patients. However, studies investigating hematological parameters and their relationship with CSDH are scarce [4]. Therefore, the present study aims to explore the association between serum coagulation parameters (prothrombin time, activated partial thromboplastin time, D-dimer, and fibrin/fibrinogen degradation products) measured before hospitalization and the recurrence of CSDH, to exploring the specific association between coagulation parameters and postoperative recurrence in CSDH, in order to provide a new direction for clinical research on the pathophysiology of chronic subdural hematoma in the future.
Materials and methods
Study population
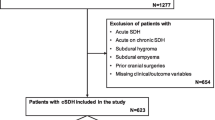
236 patients with CSDH who underwent trephination and subdural drainage for the first time in the Department of neurosurgery, Zhejiang provincial people’s hospital from September 2019 to February 2022 were retrospectively analyzed. In addition, their baseline profiles, imaging examination and blood tests were complete. All patients were confirmed by cranial CT or head magnetic resonance imaging (MRI) before surgery. Antiplatelet and/or anticoagulant agents were discontinued before surgery in all patients. For patients with elevated international standardized ratios at admission, we routinely administer intravenous fibrinogen K before surgery. Antiplatelet or anticoagulant agents are usually reapplied 1 month after surgery. The patients were informed that their clinical data should be used for medical research analysis. After obtaining the consent of the patients, CSDH patients with complete data before trepanation and drainage were accurately followed up for 90 days, the relevant clinical data of the patients were recorded, and the relevant data were retrospectively analyzed. The present study was approved by the ethnic aboard of Zhejiang provincial people’s hospital.
Inclusion and exclusion criteria
Inclusion criteria
To be eligible for the study, patients must meet the following criteria:
-
Age above 18 years.
-
Presence of chronic or subacute, uni- or bilateral subdural hematomas confirmed by cerebral computed tomography (CT) scan without contrast enhancement. Patients diagnosed with CSDH using a different imaging modality (e.g., magnetic resonance imaging) must undergo an additional CT scan.
-
Absence of clinical (Glasgow Coma Scale score ≤ 12, motor deficit < 4/5) and radiological signs of severity (midline shift > 5 mm, uncal transtentorial herniation) as assessed by the responsible neurosurgeon investigator.
-
Written informed consent obtained from the patients or their next of kin, taking into consideration the patients’ cognitive status.
Exclusion criteria
The following criteria will result in noninclusion of patients in the trial (any one criterion is sufficient for exclusion):
-
Clinical signs of severity (Glasgow Coma Scale score ≤ 12, motor deficit < 4/5).
-
Radiological signs of severity (midline shift > 5 mm, uncal transtentorial herniation).
-
Diabetes mellitus (the vascular endothelium is in an inflammatory response state when the body is in a chronic state of hyperglycemia, and coagulation failure is intimately linked to the rise in vascular active substances brought on by inflammatory reactions, vascular endothelial damage, etc.).
-
Contraindications for methylprednisolone, including uncontrolled infectious disease, evolutive viral disease (e.g., HIV, hepatitis, herpes, varicella, and herpes zoster), known psychiatric disorder, known hypersensitivity to methylprednisolone or lactose intolerance.
-
Previous surgery for CSDH within the past 6 months.
-
Pre-existing severe dementia, defined by a MMSE score < 16 unrelated to CSDH.
-
Neurological pathology associated with dementia.
-
Long-term corticosteroid treatment.
-
Patients under legal protection (conservatorship, trusteeship, and guardianship) or deprived of freedom.
-
Participation of the patient in other concurrent clinical research studies.
Sample collection and testing
Peripheral blood samples were collected from CSDH patients who met the inclusion and exclusion criteria following the standard clinical blood collection procedure. The blood samples were obtained 1 h prior to the surgical operation. The collection vessels used did not contain any anticoagulants, and the samples were kept at a temperature of 22–25 °C for 30 to 60 min. After this period, the serum, which appeared as a light-yellow supernatant precipitate surrounding the clot, was carefully aspirated. The serum was then transferred to 1.5 ml frozen storage tubes, and each sample was divided into three approximately equal parts of about 500 μl. The tubes were properly labeled with the sample number and type using a marker. Subsequently, the tubes were stored in a refrigerator at a temperature of − 80 °C. The samples designated for testing were placed in a dry ice transport box and sent to the laboratory for coagulation function tests. Throughout the study, all biological specimens were tested in duplicate whenever possible, and the average value of the test data was recorded as the experimental result.
Sample size
Since there were no previous studies addressing the specific question of this manuscript and no information about defining ideal sample size, we had no idea of the threshold of a sample pool. Hence, the present study included 236 patients. Initially, more than 240 patients were enrolled in the study. However, after applying the exclusion criteria, the final number of participants was 236.
All patients had their blood coagulation indicators examined, and samples of patients with various clinical outcomes were gathered in accordance with the requirements of the experimental design. To guarantee the precision and dependability of the experimental data, this study developed a robust and repeatable experimental procedure. To prevent the introduction of subjective bias, the data statistics procedure uses a double-blind experimental design in which the sample processing group is unknown to both the data analysts and the experimental operators. Strict experimental procedures and standardized operating protocols are implemented to ensure consistency and reproducibility of each experimental step. Detailed records of the experimental process, including data collection, are maintained for subsequent analysis and validation.
Statistical analysis
Statistical differences between the two groups were examined using Chi-square tests and Fisher exact tests. Further subgroup analyses were performed using the Chi-square tests and Fisher exact tests; statistical significance was defined as P < 0.05. All analyses were performed using the statistical software SPSS 20.0 version.
Results
Univariate analysis of baseline characteristics of patients with CSDH
236 patients with CSDH who were diagnosed for the first time and had complete medical records were followed up for at least 90 days. 50 patients (21.2%) had relapsed. Univariate analysis of the general data, imaging data and test results of 180 patients with CSDH who were included for the first time, as shown in Table 1. There was no difference in gender, smoking history, alcoholism history, and diabetes history. However, they included advanced age (≥ 80 years old) (p = 0.01), hypertension (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg) (p = 0.041), liver disease [Alanine Aminotransferase (ALT) > 40 U/L, Aspartate Aminotransferase (AST) > 34 U/L, Bilirubin > 1.2 mg/dL] (p = 0.01), anticoagulant drug use [Warfarin, heparin, low molecular weight heparin (LMWH), direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, apixaban, and edoxaban] (p = 0.01), antiplatelet drug use (Aspirin, clopidogrel, prasugrel, ticagrelor) (p = 0.02), bilateral hematoma (p = 0.02), and single-layer hematoma (p = 0.01); there was a statistically significant difference, as shown in Tables 1 and 2.
Serum FDP and DD increased simultaneously with CSDH recurrence
We conducted a comparison of the recurrence rates of CSDH patients based on serum coagulation parameters, including prothrombin time (PT), activated partial thromboplastin time (APTT), D-dimer (D–D), and fibrin/fibrinogen degradation products (FDP). Our analysis revealed no significant differences in recurrence rates based on PT, APTT, or D–D levels (P > 0.05). However, there was a significant difference observed in recurrence rates based on FDP levels (P < 0.05), as presented in Table 3.
To further investigate the relationship between D–D and FDP, we examined the recurrence rates of CSDH patients based on the combination of these two parameters. The combination demonstrated a significant difference (P < 0.05). Moreover, the combination showed a significant difference specifically in cases of recurrence within 30 days (P < 0.05), as presented in Tables 3 and 4.
Discussion
The pathophysiological mechanisms underlying the formation of chronic subdural hematoma (CSDH) have been the subject of study for over a century. Through extensive research, our understanding of the pathophysiological processes involved in CSDH formation has gradually improved [5,6,7]. In the seventeenth century, CSDH was initially recognized as a stroke, while in the nineteenth century, it was regarded as an inflammatory disease. It was not until the twentieth century that CSDH began to be recognized as a consequence of traumatic head injury. The first documented case of CSDH was reported in 1657 by Johan J. Wepfer [8] that described the presence of a large bloody cyst in the subdural space of a patient who had died from a stroke. Similar findings were reported by Morgagni 90 years later, further supporting the notion that CSDH was associated with strokes. In 1857, Virchow published a paper on the histological structure of the outer membrane of the hematoma, describing CSDH as a dural hemorrhage. He proposed a widely accepted hypothesis at the time, suggesting that the disease was caused by an inflammatory response of the dura. However, Virchow’s hypothesis focused on chronic inflammatory responses triggered by bacterial infections. It is important to note that not only infections, but also inflammatory responses can occur as a result of injury from any etiology. In the late 19th and early twentieth centuries, Trotter proposed trauma as a possible cause of CSDH, which garnered academic attention [9]. This viewpoint has been partially supported by studies, as it has been reported that over 80% of CSDH patients have a history of head trauma prior to the onset of symptoms [9]. CSDH can also result from vascular injury, inflammatory response, protein and cytokine-mediated cellular damage.
In the course of an intracranial trauma, the effect of external head forces can lead to rupture of intracranial blood vessels, resulting in hemorrhage and haematoma. In addition, due to the anatomical characteristics of intracranial blood vessels and the particular location of brain tissue, some intracranial blood vessels are susceptible to tensile or shear forces, which also increase the risk of vessel rupture. Following haematoma formation, blood components and breakdown products enter the brain tissue and cause an inflammatory response [10, 11]. This inflammatory response causes edema and infiltration of inflammatory cells into the brain tissue, which further aggravates the damage to the brain tissue and also promotes re-rupture of the blood vessel and hemorrhage, creating a vicious cycle. The blood components and decomposition products in the haematoma contain a number of proteins, cytokines, etc., which can directly or indirectly cause cell damage and apoptosis in the brain tissue, accelerating the formation and expansion of the haematoma [8].
CSDH is a relatively rare but serious intracranial disorder that can occur as a result of bleeding disorders (e.g., anticoagulant use and platelet dysfunction). These patients may have coagulation abnormalities such as platelet dysfunction, coagulation factor deficiencies or abnormalities which may increase the risk of bleeding and lead to the formation and development of hematomas. In addition, some patients may be on long-term anticoagulant medication (e.g., warfarin), which can also increase the incidence of chronic subdural hematomas [6, 8]. The present study aimed to investigate the relationship between serum coagulation parameters (PT, APTT, D–D, and FDP) and the recurrence of CSDH. The results revealed several important findings that shed light on the factors contributing to CSDH recurrence and have implications for clinical practice.
First, advanced age was found to be significantly correlated with CSDH recurrence. This finding is consistent with previous studies that have demonstrated age as a risk factor for CSDH recurrence. It is well known that aging is associated with changes in the brain vasculature, such as increased vessel fragility and decreased vascular elasticity, which may predispose older individuals to CSDH recurrence [5]. Furthermore, age-related comorbidities, including hypertension and liver disease, were also identified as significant factors associated with CSDH recurrence. These findings highlight the importance of considering age and associated comorbidities when assessing the risk of CSDH recurrence in clinical practice [6].
Second, the use of anticoagulant and antiplatelet drugs was found to be significantly associated with CSDH recurrence. Anticoagulant and antiplatelet medications are commonly prescribed for various medical conditions, such as atrial fibrillation and cardiovascular diseases, to prevent thromboembolic events. However, these medications can disrupt the balance of the coagulation system, leading to increased bleeding tendencies and potentially contributing to CSDH recurrence [7]. This finding underscores the need for careful management and monitoring of patients on anticoagulant and antiplatelet therapy who undergo surgical treatment for CSDH.
Importantly, the study identified elevated levels of fibrin degradation products (FDP) as a significant predictor of CSDH recurrence. FDP is a marker of fibrinolysis, reflecting the breakdown of fibrin clots. The presence of elevated FDP levels suggests increased fibrinolytic activity and impaired hemostasis, which may contribute to the recurrence of CSDH [8, 9]. This finding highlights the potential role of the coagulation–fibrinolysis system in the pathogenesis of CSDH and suggests that monitoring FDP levels could aid in identifying patients at higher risk of recurrence.
Furthermore, the combination of D–D and FDP levels showed a significant difference, particularly in cases of recurrence within 30 days. D–Dimer is a specific marker of fibrin degradation and reflects the formation and breakdown of blood clots [10, 11]. The significant association between D–Dimer and CSDH recurrence, especially in the early postoperative period, suggests that ongoing fibrinolysis and clot formation may contribute to early recurrence. This finding emphasizes the importance of closely monitoring patients during the initial postoperative period to detect early signs of recurrence. However, most of the previous studies were from the clinical perspective, and the pathophysiological mechanism involved in postoperative hematoma recurrence is still in its infancy [12,13,14,15,16,17].
In light of these findings, the management of CSDH patients should involve a comprehensive assessment of risk factors, including age, comorbidities, and medication use. Close monitoring of coagulation parameters, particularly FDP and D-Dimer levels, may provide valuable insights into the risk of CSDH recurrence. Identifying patients at higher risk of recurrence can guide decisions regarding postoperative management, such as the duration of anticoagulant or antiplatelet therapy and the need for closer surveillance.
Limitations
It is important to acknowledge some limitations of this study. First, one limitation of this study is the relatively small sample size, with only 236 patients included. A larger sample size would provide greater statistical power and enhance the generalizability of the findings. The small sample size may limit the ability to draw robust conclusions and extrapolate the results to larger populations. This study relied on clinical records and data collected during routine clinical practices, which have inherent limitations, including potential biases, missing data, and the inability to establish causal relationships. Employing a prospective study design with standardized data collection methods could yield more reliable and comprehensive results. Second, some confounding factors may bring some bias to the final results. Third, hemoglobin, platelet, and serum creatinine measurements are lacking, and these parameters could provide valuable information regarding the patients’ overall health status and potential underlying conditions that may influence the recurrence of CSDH. The absence of these measurements limits a comprehensive analysis of their potential association with CSDH recurrence. Fourth, the absence of exploration regarding the indications for anticoagulant use, such as atrial fibrillation (AFib), pulmonary embolism (PE), and deep vein thrombosis (DVT), should be considered. Anticoagulant therapy is commonly indicated in patients with AFib to prevent stroke and systemic embolism, as well as in patients with PE or DVT to prevent clot propagation and recurrence. However, this study does not provide information on whether the patients included had these indications for anticoagulant therapy. The absence of this data limits the understanding of the potential impact of anticoagulant use on the recurrence of CSDH and may affect the generalizability of the findings to populations with different indications for anticoagulation.
Conclusion
This study provides valuable insights into the relationship between serum coagulation parameters and the recurrence of CSDH. The simultaneous elevation of serum FDP and D-D levels upon admission represents a potentially novel predictor for CSDH recurrence. This finding is particularly relevant for patients who experience recurrence within 30 days following surgical intervention. Older individuals with CSDH who undergo trepanation and drainage should be closely monitored due to their relatively higher recurrence rate.
Advanced age, comorbidities, and medication use were identified as significant risk factors for CSDH recurrence. These findings have important implications for risk stratification and the development of tailored management strategies for CSDH patients. Further research is warranted to validate these findings and elucidate the underlying mechanisms contributing to CSDH recurrence.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Kan P, Maragkos GA, Srivatsan A et al (2021) Middle meningeal artery embolization for chronic subdural hematoma: a multi-center experience of 154 consecutive embolizations. Neurosurgery 88(2):268–277. https://doi.org/10.1093/neuros/nyaa379
Takei J, Inomata T, Aoki T et al (2023) Development and validation of a recurrent prediction model for patients with unilateral chronic subdural hematoma without hematoma volumetric analysis. Clin Neurol Neurosurg. https://doi.org/10.1016/j.clineuro.2023.107678
Havryliv T, Devinyak O, Yartym O, Smolanka A, Volodymyr S, Okoro EU (2023) Single-center comparison of chronic subdural hematoma evacuation outcomes under local versus general anesthesia. World Neurosurg. https://doi.org/10.1016/j.wneu.2023.12.116
Wang C, Liu C (2023) Surgical treatment of chronic subdural hematoma by twist drill craniotomy: a 9-year, single-center experience of 219 cases. Clin Neurol Neurosurg. https://doi.org/10.1016/j.clineuro.2023.107891
Kweon SB, Kim S, Kwon MY et al (2023) Natural course of chronic subdural hematoma following surgical clipping of unruptured intracranial aneurysm by pterional approach. J Cerebrovasc Endovasc Neurosurg 25(4):390–402. https://doi.org/10.7461/jcen.2023.E2023.04.017
Goto D, Amano Y, Asayama B, Kamiyama K, Osato T, Nakamura H (2023) Significant correlation between structural changes in the net-like appearance on postoperative cranial magnetic resonance images and hematoma recurrence in cases of chronic subdural hematoma. Neurol Med Chir 63(4):152–157. https://doi.org/10.2176/jns-nmc.2022-0196
Kim KH, Lee Y (2023) Medical management of chronic subdural hematoma. Korean J Neurotrauma 19(3):288–297. https://doi.org/10.13004/kjnt.2023.19.e47
Sadeghian H, Chida K, Motiei-Langroudi R (2023) Editorial: chronic subdural hematoma: overview of recent therapeutic advancements. Front Neurol. https://doi.org/10.3389/fneur.2023.1155680
Rodriguez B, Morgan I, Young T et al (2023) Surgical techniques for evacuation of chronic subdural hematoma: a mini-review. Front Neurol. https://doi.org/10.3389/fneur.2023.1086645
Msheik A, Gerges T, Al Mokdad Z, Abbass D, Mohanna A, Aoude A (2023) Revolutionizing treatment for chronic subdural hematoma: promising outcomes with middle meningeal artery embolization. Cureus. https://doi.org/10.7759/cureus.39733
Jiang R, Zhao S, Wang R et al (2018) Safety and efficacy of atorvastatin for chronic subdural hematoma in chinese patients: a randomized clinicaltrial. JAMA Neurol 75(11):1338–1346. https://doi.org/10.1001/jamaneurol.2018.2030
Crider K, Williams J, Qi YP et al (2022) Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD014217
Jensen TSR, Andersen-Ranberg N, Poulsen FR, Bergholt B, Hundsholt T, Fugleholm K (2020) The danish chronic subdural hematoma study-comparison of hematoma age to the radiological appearance at time of diagnosis. Acta Neurochir 162(9):2007–2013. https://doi.org/10.1007/s00701-020-04472-w
Sale D (2021) Single versus double burr hole for drainage of chronic subdural hematoma: randomized controlled study. World Neurosurg 146:e565–e567. https://doi.org/10.1016/j.wneu.2020.10.140
Bartley A, Jakola AS, Tisell M (2020) The influence of irrigation fluid temperature on recurrence in the evacuation of chronic subdural hematoma. Acta Neurochir 162(3):485–488. https://doi.org/10.1007/s00701-019-04150-6
Lutz K, Kamenova M, Schaedelin S et al (2019) Time to and possible risk factors for recurrence after burr-hole drainage of chronic subdural hematoma: a subanalysis of the cSDH-drain randomized controlled trial. World Neurosurg 132:e283–e289. https://doi.org/10.1016/j.wneu.2019.08.175
Wang D, Tian Y, Wei H et al (2022) Risk factor analysis of the conservative treatment in chronic subdural hematomas: a substudy of the ATOCH trial. Adv Ther 39(4):1630–1641. https://doi.org/10.1007/s12325-022-02057-w
Acknowledgements
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was supported by the Zhejiang Medical and Health Technology Project (2021KY1131).
Author information
Authors and Affiliations
Contributions
Tian-Yu Liang conceived study design and content concept; Zhen Bao, Gang Cui, and Jian-Min Qu performed the data collection, extraction and analyzed the data; Zhen Bao was responsible for literature search; Sen Xu made major revisions to the manuscript; Tian-Yu Liang interpreted and reviewed the data and drafts.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by Ethics Committee of the Zhejiang provincial people’s hospital. Written informed consent was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bao, Z., Xu, S., Cui, G. et al. The relationship between serum coagulation parameters and the recurrence of chronic subdural hematoma. Mol Cell Biochem (2024). https://doi.org/10.1007/s11010-024-05019-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11010-024-05019-8