Abstract
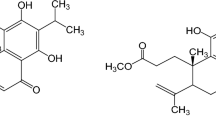
Curcumin (CUR) is an extract of Curcuma longa Linn., which has various pharmacological activities. The instability, low water solubility and bioavailability of CUR greatly limit its clinical application. This work prepared Pluronic F127-liposome-encapsulated curcumin (CUR-LIP-F127) and explored its functional role in wound healing. Liposome-encapsulated curcumin (CUR-LIP) and CUR-LIP-F127 were prepared. Human keratinocyte cell line (HaCaT) was treated with CUR, Pluronic F127-liposome (LIP-F127) and CUR-LIP-F127, or combined with ML385 (Nrf2 inhibitor). The expression of mRNAs and proteins was detected by quantitative real-time PCR and western blotting. MTT and wound healing assays were performed to detect cell viability and migration. CUR, LIP-F127 and CUR-LIP-F127 all had no influence on cell viability of HaCaT cells. CUR-LIP-F127 treatment significantly accelerated cell migration and enhanced the expression of nuclear factor erythroid-related factor 2 (Nrf2) and kelch-like erythroid cell-derived protein 1 (Keap1) in HaCaT cells with respect to CUR or LIP-F127 treatment. ML385 treatment impaired CUR-LIP-F127-mediated promotion of migration and up-regulation of Nrf2 and Keap1 in HaCaT cells. This work demonstrated that CUR-LIP-F127 activated Nrf2/Keap1 signaling pathway to promote migration of HaCaT cells, suggesting that CUR-LIP-F127 may contribute to wound healing.




Similar content being viewed by others
Data availability
Not applicable.
References
Zomer H, Trentin A (2018) Skin wound healing in humans and mice: challenges in translational research. J Dermatol Sci 90:3–12. https://doi.org/10.1016/j.jdermsci.2017.12.009
Monavarian M, Kader S, Moeinzadeh S, Jabbari E (2019) Regenerative scar-free skin wound healing. Tissue engineering. Part B, Rev 25:294–311. https://doi.org/10.1089/ten.TEB.2018.0350
Martin R (2020) Wound healing. Surgical Clin North America 100:ix–xi. https://doi.org/10.1016/j.suc.2020.05.012
Sorg H, Tilkorn D, Hager S, Hauser J, Mirastschijski U (2017) Skin wound healing: an update on the current knowledge and concepts. European surgical research. Europaische chirurgische Forschung Recherches chirurgicales europeennes 58:81–94. https://doi.org/10.1159/000454919
Grabowski G, Pacana M, Chen E (2020) Keloid and hypertrophic scar formation, prevention, and management: standard review of abnormal scarring in orthopaedic surgery. J Am Acad Orthop Surg 28:e408–e414. https://doi.org/10.5435/jaaos-d-19-00690
Rodrigues M, Kosaric N, Bonham C, Gurtner G (2019) Wound healing: a cellular perspective. Physiol Rev 99:665–706. https://doi.org/10.1152/physrev.00067.2017
Everts P, Onishi K, Jayaram P, Lana J, Mautner K (2020) Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. https://doi.org/10.3390/ijms21207794
Gauglitz G, Zedler S, von Spiegel F, Fuhr J, von Donnersmarck G, Faist E (2012) Functional characterization of cultured keratinocytes after acute cutaneous burn injury. PLoS ONE 7:e29942. https://doi.org/10.1371/journal.pone.0029942
Jiang Z, Wei J, Yang W, Li W, Liu F, Yan X, Yan X, Hu N, Li J (2020) MicroRNA-26a inhibits wound healing through decreased keratinocytes migration by regulating ITGA5 through PI3K/AKT signaling pathway. Biosci Rep. https://doi.org/10.1042/bsr20201361
Koike Y, Yozaki M, Utani A, Murota H (2020) Fibroblast growth factor 2 accelerates the epithelial-mesenchymal transition in keratinocytes during wound healing process. Sci Rep 10:18545. https://doi.org/10.1038/s41598-020-75584-7
Kotha R, Luthria D (2019) Curcumin: biological, pharmaceutical, nutraceutical, and analytical aspects. Molecules (Basel, Switzerland). https://doi.org/10.3390/molecules24162930
Kim Y, Clifton P (2018) Curcumin, cardiometabolic health and dementia. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15102093
Burge K, Gunasekaran A, Eckert J, Chaaban H (2019) Curcumin and intestinal inflammatory diseases: molecular mechanisms of protection. Int J Mol Sci. https://doi.org/10.3390/ijms20081912
Dei Cas M, Ghidoni R (2019) Dietary curcumin: correlation between bioavailability and health potential. Nutrients. https://doi.org/10.3390/nu11092147
Ipar V, Dsouza A, Devarajan P (2019) Enhancing curcumin oral bioavailability through nanoformulations. Eur J Drug Metab Pharmacokinet 44:459–480. https://doi.org/10.1007/s13318-019-00545-z
Feng T, Wei Y, Lee R, Zhao L (2017) Liposomal curcumin and its application in cancer. Int J Nanomed 12:6027–6044. https://doi.org/10.2147/ijn.s132434
Rabbani P, Soares M, Hameedi S, Kadle R, Mubasher A, Kowzun M, Ceradini D (2019) Dysregulation of Nrf2/Keap1 redox pathway in diabetes affects multipotency of stromal cells. Diabetes 68:141–155. https://doi.org/10.2337/db18-0232
Rabbani P, Abdou S, Sultan D, Kwong J, Duckworth A, Ceradini D (2018) In Vivo imaging of reactive oxygen species in a murine wound model. JoVE. https://doi.org/10.3791/58450
Lin L, Li C, Zhang D, Yuan M, Chen C, Li M (2020) Synergic effects of berberine and curcumin on improving cognitive function in an Alzheimer’s disease mouse model. Neurochem Res 45:1130–1141. https://doi.org/10.1007/s11064-020-02992-6
El Nebrisi E, Javed H, Ojha S, Oz M, Shehab S (2020) Neuroprotective effect of curcumin on the nigrostriatal pathway in a 6-hydroxydopmine-induced rat model of Parkinson’s disease is mediated by α7-nicotinic receptors. Int J Mol Sci. https://doi.org/10.3390/ijms21197329
Zheng Y, Yang X, Tan J, Tian R, Shen P, Cai W, Liao H (2021) Curcumin suppresses the stemness of non-small cell lung cancer cells via promoting the nuclear-cytoplasm translocation of TAZ. Environ Toxicol 36:1135–1142. https://doi.org/10.1002/tox.23112
Shabeeb D, Musa A, Abd Ali H, Najafi M (2020) Curcumin protects against radiotherapy-induced oxidative injury to the skin. Drug Des Dev Ther 14:3159–3163. https://doi.org/10.2147/dddt.s265228
Kim D, Choi C, Park J, Lee S (2020) Nanospheres loaded with curcumin improve the bioactivity of umbilical cord blood-mesenchymal stem cells via C-SRC activation during the skin wound healing process. Cells. https://doi.org/10.3390/cells9061467
Kamar S, Abdel-Kader D, Rashed L (2019) Beneficial effect of Curcumin Nanoparticles-Hydrogel on excisional skin wound healing in type-I diabetic rat: histological and immunohistochemical studies. Ann Anatomy 222:94–102. https://doi.org/10.1016/j.aanat.2018.11.005
Orsu P, Haider H, Koyyada A (2021) Bioengineering for curcumin loaded carboxymethyl guargum/reduced graphene oxide nanocomposites for chronic wound healing applications. Int J Pharm 606:120928. https://doi.org/10.1016/j.ijpharm.2021.120928
Abbas M, Hussain T, Arshad M, Ansari A, Irshad A, Nisar J, Hussain F, Masood N, Nazir A, Iqbal M (2019) Wound healing potential of curcumin cross-linked chitosan/polyvinyl alcohol. Int J Biol Macromol 140:871–876. https://doi.org/10.1016/j.ijbiomac.2019.08.153
Sajadimajd S, Khazaei M (2018) Oxidative stress and cancer: the role of Nrf2. Curr Cancer Drug Targets 18:538–557. https://doi.org/10.2174/1568009617666171002144228
Liu H, Xu X, Wu R, Bi L, Zhang C, Chen H, Yang Y (2021) Antioral squamous cell carcinoma effects of carvacrol via inhibiting inflammation, proliferation, and migration related to Nrf2/Keap1 pathway. Biomed Res Int 2021:6616547. https://doi.org/10.1155/2021/6616547
Li P, Liu X, Xing W, Qiu H, Li R, Liu S, Sun H (2022) Exosome-derived miR-200a promotes esophageal cancer cell proliferation and migration via the mediating Keap1 expression. Mol Cell Biochem 477:1295–1308. https://doi.org/10.1007/s11010-022-04353-z
Valcarcel-Ares M, Gautam T, Warrington J, Bailey-Downs L, Sosnowska D, de Cabo R, Losonczy G, Sonntag W, Ungvari Z, Csiszar A (2012) Disruption of Nrf2 signaling impairs angiogenic capacity of endothelial cells: implications for microvascular aging. J Gerontol Series A, Biol Sci Med Sci 67:821–829. https://doi.org/10.1093/gerona/glr229
Hayashi R, Himori N, Taguchi K, Ishikawa Y, Uesugi K, Ito M, Duncan T, Tsujikawa M, Nakazawa T, Yamamoto M, Nishida K (2013) The role of the Nrf2-mediated defense system in corneal epithelial wound healing. Free Radical Biol Med 61:333–342. https://doi.org/10.1016/j.freeradbiomed.2013.04.008
Acknowledgements
We would like to give our sincere gratitude to the reviewers for their constructive comments.
Funding
This work was supported by Hunan Provincial Health Commission (202104101005) and Hunan Administration of traditional Chinese Medicine (2021227).
Author information
Authors and Affiliations
Contributions
QZ: Conceptualization, Methodology, Supervision, Writing- Original draft preparation, Investigation, Writing- Reviewing and Editing. XC: Data curation, Software. YH: Visualization, Validation. YZ: Conceptualization, Supervision, Writing- Original draft preparation, Writing- Reviewing and Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Q., Cai, X., Huang, Y. et al. Pluronic F127-liposome-encapsulated curcumin activates Nrf2/Keap1 signaling pathway to promote cell migration of HaCaT cells. Mol Cell Biochem 478, 241–247 (2023). https://doi.org/10.1007/s11010-022-04481-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-022-04481-6