Abstract
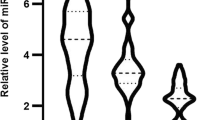
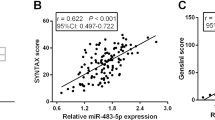
Acute coronary syndrome (ACS) is one of the leading causes of cardiovascular death. It seems that microRNA-21 and matrix metalloproteinase-9 implicated in the pathogenesis of cardiovascular diseases. The aim of this study was to investigate the role of circulating miR-21 and MMP-9 as biomarkers for ACS. Based on coronary angiography and electrocardiography results, 50 patients with ACS and 50 patients with stable coronary artery disease (stable CAD) were enrolled in this study. Samples were collected from patients and stored at −80 °C. Serum miR-21 gene expression was measured by quantitative real-time PCR method. Serum total MMP-9 was measured by enzyme-linked immunosorbent assay kit. Also, the activity of MMP-9 was measured by gelatin zymography. Patients with ACS had a significantly higher miR-21 level compared to the stable CAD (\(\log \, 2^{{ - \Delta C_{\text{t}} }}\) = 0.88 ± 0.06 and 0.31 ± 0.08 respectively, P < 0.001). At the same time, the serum levels and activity of MMP-9 were significantly higher in ACS patients compared to those with stable CAD (324.01 ± 17.57 and 204.6 ± 12.39 ng/mL, P < 0.001, and 2524.5 ± 131.3 and 1280.8 ± 19.6 units, P < 0.001, respectively). miR-21 expression levels were correlated positively with MMP-9, hs-CRP, and age and negatively with HDL-cholesterol (r = 0.33, P < 0.001, r = 0.22, P < 0.031, r = 0.26, P < 0.008, r = −0.32, P < 0.001, respectively). We concluded that increased serum expression of miR-21 and higher serum activity of MMP-9 may be useful indicators for ACS. However, we suggest further studies to be performed.





Similar content being viewed by others
References
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Greenlund K, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O’Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y, American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2009) Heart disease and stroke statistics—2009 update a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119:e21–e181
Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW (2000) Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med 343:915–922
Hackett D, Davies G, Chierchia S, Maseri A (1987) Intermittent coronary occlusion in acute myocardial infarction. N Engl J Med 317:1055–1059
Sarrafzadegan N, Gotay C (2015) CVD prevention in 2014: advances in the prevention of cardiovascular disease. Nat Rev Cardiol 12:71–73
Oerlemans MI, Mosterd A, Dekker MS, de Vrey EA, van Mil A, Pasterkamp G, Doevendans PA, Hoes AW, Sluijter JP (2012) Early assessment of acute coronary syndromes in the emergency department: the potential diagnostic value of circulating microRNAs. EMBO Mol Med 4:1176–1185
Hussain MU (2012) Micro-RNAs (miRNAs): genomic organisation, biogenesis and mode of action. Cell Tissue Res 349:405–413
Griffiths-Jones S, Grocock RJ, Van Dongen S, Bateman A, Enright AJ (2006) miRBase: microRNA sequences, targets and gene nomenclature. Nucleic Acids Res 34:D140–D144
Huntzinger E, Izaurralde E (2011) Gene silencing by microRNAs: contributions of translational repression and mRNA decay. Nat Rev Genet 12:99–110
Hwang H, Mendell J (2006) MicroRNAs in cell proliferation, cell death, and tumorigenesis. Br J Cancer 94:776–780
Chen KC, Wang YS, Hu CY, Chang WC, Liao YC, Dai CY, Juo SHH (2011) OxLDL up-regulates microRNA-29b, leading to epigenetic modifications of MMP-2/MMP-9 genes: a novel mechanism for cardiovascular diseases. FASEB J 25:1718–1728
Small EM, Frost RJ, Olson EN (2010) MicroRNAs add a new dimension to cardiovascular disease. Circulation 12:1022–1032
Small EM, Olson EN (2011) Pervasive roles of microRNAs in cardiovascular biology. Nature 469:336–342
Etheridge A, Lee I, Hood L, Galas D, Wang K (2011) Extracellular microRNA: a new source of biomarkers. Mutat Res Fund Mol Mech Mut 717:85–90
Wang G-K, Zhu J-Q, Zhang J-T, Li Q, Li Y, He J, Qin Y-W, Jing Q (2010) Circulating microRNA: a novel potential biomarker for early diagnosis of acute myocardial infarction in humans. Eur Heart J 31:659–666
Cheng Y, Liu X, Yang J, Lin Y, Da-Zhong X, Qi L, Deitch EA, Huo Y, Delphin ES, Zhang C (2009) MicroRNA-145, a novel smooth muscle cell phenotypic marker and modulator, controls vascular neointimal lesion formation. Circ Res 105:158–166
Liu X, Cheng Y, Zhang S, Lin Y, Yang J, Zhang C (2009) A necessary role of miR-221 and miR-222 in vascular smooth muscle cell proliferation and neointimal hyperplasia. Circ Res 104:476–487
Sen CK, Roy S (2012) microRNA 21 in tissue injury and inflammation. Cardiovasc Res 96:230–233
Jazbutyte V, Thum T (2010) microRNA-21: from cancer to cardiovascular disease. Curr Drug Targets 11:926–935
Cheng Y, Zhang C (2010) microRNA-21 in cardiovascular disease. J Cardiovasc Transl Res 3:251–255
Raitoharju E, Lyytikäinen LP, Levula M, Oksala N, Mennander A, Tarkka M, Klopp N, Illig T, Kähönen M, Karhunen PJ, Laaksonen R (2011) miR-21, miR-210, miR-34a, and miR-146a/b are up-regulated in human atherosclerotic plaques in the Tampere Vascular Study. Atherosclerosis 219:211–217
Finn AV, Nakano M, Narula J, Kolodgie FD, Virmani R (2010) Concept of vulnerable/unstable plaque. Arterioscler Thromb Vasc Biol 30:1282–1292
Jabłońska-Trypuć A, Matejczyk M, Rosochacki S (2016) Matrix metalloproteinases (MMPs), the main extracellular matrix (ECM) enzymes in collagen degradation, as a target for anticancer drugs. J Enzyme Inhib Med Chem 23:1–7
Page-McCaw A, Ewald AJ, Werb Z (2007) Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol 8:221–233
Nagase H, Visse R, Murphy G (2006) Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res 69:562–573
Galis ZS, Sukhova GK, Lark MW, Libby P (1994) Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest. 94:2493–2498
Visse R, Nagase H (2003) Matrix metalloproteinases and tissue inhibitors of metalloproteinases structure, function, and biochemistry. Circ Res 92:827–839
Fan X, Wang E, Wang X, Cong X, Chen X (2014) microRNA-21 is a unique signature associated with coronary plaque instability in humans by regulating matrix metalloproteinase-9 via reversion-inducing cysteine-rich protein with Kazal motifs. Exp Mol Pathol 96:242–249
Han L, Yue X, Zhou X, Lan FM, You G, Zhang W, Zhang KL, Zhang CZ, Cheng JQ, Yu SZ, Pu PY (2012) microRNA-21 expression is regulated by β-catenin/STAT3 pathway and promotes glioma cell invasion by direct targeting RECK. CNS Neurosci Ther 18:573–583
Weaver WD, Simes RJ, Betriu A, Grines CL, Zijlstra F, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, DeWood MA, Ribichini F (1997) Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA 278:2093–2098
Wintersperger BJ, Nikolaou K (2005) Basics of cardiac MDCT: techniques and contrast application. Eur Radiol 15:B2–B9
Ro S, Park C, Jin J, Sanders KM, Yan W (2006) A PCR-based method for detection and quantification of small RNAs. Biochem Biophys Res Commun 351:756–763
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, Mueller R, Nolan T, Pfaffl MW, Shipley GL, Vandesompele J (2009) The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55:611–622
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative CT method. Nat Protoc 3:1101–1108
Kroh EM, Parkin RK, Mitchell PS, Tewari M (2010) Analysis of circulating microRNA biomarkers in plasma and serum using quantitative reverse transcription-PCR (qRT-PCR). Methods 50:298–301
Frankowski H, Gu Y-H, Heo JH, Milner R, del Zoppo GJ (2012) Use of gel zymography to examine matrix metalloproteinase (gelatinase) expression in brain tissue or in primary glial cultures. Astrocytes 814:221–233
McCann CJ, Glover BM, Menown IBA, Moore MJ, McEneny J, Owens CG, Smith B, Sharpe PC, Young IS, Adgey JA (2008) Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponin T. Eur Heart J 29:2843–2850
Libby P, Ridker PM, Maseri A (2002) Inflammation and atherosclerosis. Circulation 105:1135–1143
Urbich C, Kuehbacher A, Dimmeler S (2008) Role of microRNAs in vascular diseases, inflammation and angiogenesis. Cardiovasc Res 79:581–588
Galt SW, Lindemann S, Allen L, Medd DJ, Falk JM, McIntyre TM, Prescott SM, Kraiss LW, Zimmerman GA, Weyrich AS (2002) Outside-in signals delivered by matrix metalloproteinase-1 regulate platelet function. Circ Res 90:1093–1099
Cardellini M, Menghini R, Martelli E, Casagrande V, Marino A, Rizza S, Porzio O, Mauriello A, Solini A, Ippoliti A, Lauro R (2009) TIMP3 is reduced in atherosclerotic plaques from subjects with type 2 diabetes and increased by SirT1. Diabetes 58:2396–2401
Tsai P-C, Liao Y-C, Wang Y-S, Lin H-F, Lin R-T, Juo S-H (2013) Serum microRNA-21 and microRNA-221 as potential biomarkers for cerebrovascular disease. J Vasc Res 50:346–354
Hansson GK, Hermansson A (2011) The immune system in atherosclerosis. Nat Immunol 12:204–212
Zucker S, Hymowitz M, Conner C, Zarrabi HM, Hurewitz AN, Matrisian L, Boyd D, Nicolson G, Montana S (1999) Measurement of matrix metalloproteinases and tissue inhibitors of metalloproteinases in blood and tissues: clinical and experimental applications. Ann N Y Acad Sci 878:212–227
Ardi VC, Kupriyanova TA, Deryugina EI, Quigley JP (2007) Human neutrophils uniquely release TIMP-free MMP-9 to provide a potent catalytic stimulator of angiogenesis. Proc Natl Acad Sci 104:20262–20267
Morrison CJ, Butler GS, Rodríguez D, Overall CM (2009) Matrix metalloproteinase proteomics: substrates, targets, and therapy. Curr Opin Cell Biol 21:645–653
Kai H, Ikeda H, Yasukawa H, Kai M, Seki Y, Kuwahara F, Ueno T, Sugi K, Imaizumi T (1998) Peripheral blood levels of matrix metalloproteases-2 and-9 are elevated in patients with acute coronary syndromes. J Am Coll Cardiol 32:368–372
Blankenberg S, Rupprecht HJ, Poirier O, Bickel C, Smieja M, Hafner G, Meyer J, Cambien F, Tiret L, AtheroGene Investigators (2003) Plasma concentrations and genetic variation of matrix metalloproteinase 9 and prognosis of patients with cardiovascular disease. Circulation 107:1579–1585
Packard RR, Libby P (2008) Inflammation in atherosclerosis: from vascular biology to biomarker discovery and risk prediction. Clin Chem 54:24–38
Hoekstra Menno, van der Lans Christian AC, Halvorsen Bente, Gullestad Lars, Kuiper Johan, Aukrust Pål, van Berkel Theo JC, Biessen Erik AL (2010) The peripheral blood mononuclear cell microRNA signature of coronary artery disease. Biochem Biophys Res Commun 394:792–797
Santos-Martínez MJ, Medina C, Jurasz P, Radomski MW (2008) Role of metalloproteinases in platelet function. Thromb Res 121:535–5342
Kotani T, Takeuchi T, Takai S, Yoshida S, Hata K, Nagai K, Wakura D, Isoda K, Makino S, Hanafusa T (2012) Serum levels of matrix metalloproteinase (MMP) 9, a risk factor for acute coronary syndrome, are reduced independently of serum MMP-3 by anti-TNF-α antibody (infliximab) therapy in patients with rheumatoid arthritis. J Pharmacol Sci 120:50–53
Acknowledgments
The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences and Chamran Hospital, Isfahan, Iran, according to the Helsinki Declaration. All study participants were informed about the study, and their written consent forms were obtained. This project was supported by grant number 394289 from the Isfahan University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Darabi, F., Aghaei, M., Movahedian, A. et al. The role of serum levels of microRNA-21 and matrix metalloproteinase-9 in patients with acute coronary syndrome. Mol Cell Biochem 422, 51–60 (2016). https://doi.org/10.1007/s11010-016-2805-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-016-2805-z