Abstract
Objective
For parents with opioid use disorder (OUD) and their children, group well child care (WCC) is an under-studied intervention that may reduce stigma, increase quality of care, and improve clinical outcomes. We explored barriers and facilitators to this intervention using an implementation science framework.
Methods
A qualitative study was conducted from October 2020–March 2021 as part of the planning phase of a cluster-randomized trial of group WCC. Parent participants were recruited from one urban, university-affiliated OUD treatment center to participate in semi-structured telephone interviews. Eligible parents had a child under two years old and were English speaking. Clinician participants were recruited from a nearby pediatric primary care practice. Inductive thematic analysis of interview responses was led by two investigators using open coding procedures.
Results
Thirty-one parents and thirteen pediatric clinicians participated in the interviews. Most parents (68%) reported that they would be likely or very likely to bring their child to the OUD treatment center for WCC. Six themes emerged describing perceived implementation barriers, including intervention difficulty, complexity, and potential negative outcomes such as loss of privacy. Six themes emerged as implementation facilitators: (1) focus on parental OUD and recovery, (2) peer support, (3) accessibility and coordination of care, (4) clinician skill and expertise in parental OUD, (5) increased time for patient care, and (6) continuity of care.
Conclusions for Practice
Parents and clinicians expressed multiple perceived benefits of this intervention. Identified barriers and facilitators will inform implementation and evaluation of group WCC within one OUD treatment program.
Significance
What is Already Known on the Subject? Birthing parents with opioid use disorder and their children often face social and economic hardships, including barriers to well child care engagement. Group well child care has improved family outcomes in other patient populations.
What this Study Adds? Birthing parents in treatment for opioid use disorder and pediatric clinicians identify potential facilitators of implementing group well child care within a parental treatment program; these facilitators include a focus on parental recovery and wellness, peer support, and accessibility and coordination of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Opioid use disorder (OUD) during pregnancy has emerged as a major United States (US) public health issue, with considerable focus on perinatal care of affected parents and newborns (Grossman et al., 2018; Kaplan et al., 2020; Patrick, 2017). Fewer studies have focused on pediatric primary care for these families, where risks for child health and development including poverty, stigma, and social isolation require ongoing attention (Gressler et al., 2019; Pryor et al., 2017; Sutter et al., 2017). Well child care (WCC) represents a critical opportunity for family support (American Academy of Pediatrics, 2023). Unfortunately, available studies suggest that despite multiple clinical concerns in infancy and early childhood among these families, attendance to recommended WCC visits is low (Beldick et al., 2023; Goyal et al., 2020; Jarlenski et al., 2020). Parents with OUD have reported their WCC experiences as lacking key aspects of family centeredness such as open communication and personalized care (Short et al., 2019, 2022). Simultaneously, pediatricians report a lack of time and resources to comprehensively address their questions and psychosocial needs (Rohde et al., 2023).
Group WCC, in which a group of families with similarly aged children receive WCC together during a longer visit, is one intervention which may engage, support, and empower parents with OUD. With group WCC, regularly scheduled WCC visits focus on child health and development, but also incorporate group discussion of topics such as family planning and stress reduction. Session planning guides are available through Centering Healthcare Institute that align with American Academy of Pediatrics recommendations (Centering Healthcare Institute [CHI], 2023). In addition to routine anticipatory guidance, these session planning guides include structured parental mindfulness exercises to reduce stress and promote emotional awareness for parents, as well as hands-on activities such as infant play. Thus, group WCC has unique potential to promote information sharing and peer support across multiple domains of parental and child wellness (Connor et al., 2018; DeLago et al., 2018; Platt et al., 2022). Prior studies suggest enhanced family resilience and interconnectedness, improved visit attendance, and increased satisfaction with care (Fenick et al., 2020; Irigoyen et al., 2021; Oldfield et al., 2020). Despite these benefits, group WCC remains underutilized, with numerous logistical challenges that include cost, space, and scheduling (Gaskin et al., 2021; Gresh et al., 2023).
To date, research on group WCC for parents in treatment for OUD is limited. For this population, prior studies suggest an increased risk of maladaptive parenting, including heightened tendency towards harsh punishment, low responsiveness to child cues, and knowledge gaps regarding child development (Maguire et al., 2016; Rizzo et al., 2014; Sutter et al., 2017). Addressing these risks during WCC visits is a considerable challenge for pediatricians (Abatemarco et al., 2008, 2018). For these families, group WCC may improve child outcomes through multiple mechanisms, including healthcare engagement, parenting knowledge, and parent–child attachment. For parents with OUD, who often have significant trauma burden, parenting stress, and depressive symptoms, mindfulness may be a particularly useful tool within group WCC to strengthen their capacity to respond, interact, and attune to their child (Gannon et al., 2017).
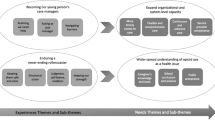
For the current study, we utilized an implementation science framework to explore factors that may impact the adaptation and delivery of group WCC for parents with OUD. Implementation science is increasingly recognized as the exploration of factors that may impede or support the real-world success of a given intervention, ultimately affecting efficacy, sustainability, and scalability (Damschroder et al., 2009). Given the complexity of group WCC as an intervention, and the clinical and psychosocial challenges of caring for parents with OUD and their children, we sought to understand barriers and facilitators to implementation.
Methods
This qualitative study was conducted in the planning phase of a cluster-randomized trial of group WCC co-located within an urban, university-affiliated OUD treatment program in Pennsylvania that provides medications for OUD (MOUD), therapy, case management and supportive services for pregnant and parenting women with OUD. Women eligible for this study were (1) receiving OUD services in the treatment program, (2) parent to a child under two years old, and (3) English-speaking. Participants also included clinicians (attendings, resident physicians, and nurses) from an urban, university-affiliated pediatric primary care practice predominately serving Medicaid-insured patients.
Procedures and Data Sources
Study procedures were conducted by our research team comprised of a public health researchers, epidemiologists, and psychologists. All procedures were conducted in accord with prevailing ethical principles and were reviewed and approved by relevant Institutional Review Boards. A waiver of written informed consent was granted, however all study participants provided verbal informed consent. Parental recruitment was conducted using convenience sampling to identify potential participants. Parents were telephoned to determine eligibility and ascertain interest in participation. A target sample size of 30 parents was planned to achieve thematic saturation (Demianczyk et al., 2022; Hennink & Kaiser, 2022). Enrolled parents were scheduled for a one-time, 30 min, semi-structured telephone interview. All interviews were conducted between October 2020 and January 2021 by one of two study team members. Each interview began with a brief survey asking participants to report demographics and information about their child’s healthcare experience. Parents were compensated for their time with $50.
All clinicians at the pediatric practice were recruited with an email containing a brief study description and contact information, and a reminder email one month later. We set an initial target sample size of approximately 15 clinicians, with plans to collect additional data if thematic saturation was not achieved (Hennink & Kaiser, 2022). Clinicians were interviewed by telephone between January and March 2021 by one study team member. Interviews were 30 min and semi-structured, and began with a brief survey asking about demographics and OUD training or education. No monetary compensation was provided.
Interview guides were developed using the Consolidated Framework for Implementation Research (CFIR) Guidelines (Damschroder et al., 2009). This framework contains multiple domains that can guide the assessment of potential barriers and facilitators to effective implementation (see Online Resource 1). As our study focused on pregnant and parenting women in treatment for OUD and their relationship as a mother to their child, the terms ‘mother’ and ‘maternal’ were used during the interviews, and for consistency will be used for the remainder of this report (National Institutes of Health, 2023). Because all interviews were conducted prior to group WCC implementation, the interview included the following brief description of group WCC to orient study participants: “With group pediatric care, a group of five to six moms and their infants see a pediatrician together for regular checkups. Each visit would last about an hour and a half, where everyone had some one-on-one time with the doctor, followed by time for group discussion about different topics, as well as some time to focus on mom’s health and wellness too. Each child would receive regular vaccines and screenings as part of the visit.” The interview continued with discussion prompts to explore barriers and facilitators to group WCC. Participants were specifically prompted to provide their perspective on mindfulness, which is a unique aspect of group WCC compared with routine WCC (CHI, 2023). For example, clinicians were asked, “Would you feel comfortable leading short breathing exercises or talking generally about mindfulness?” All interviews were audio recorded and transcribed with removal of identifiers. Interview transcripts were uploaded into Dedoose V 8.0.35 for qualitative coding and analysis.
Data Analyses
Survey data were analyzed using descriptive statistics. Interview data were analyzed using an inductive thematic approach. Thematic analysis focuses on the subjective human experience and emphasizes participants’ experiences, feelings and perceptions (Braun & Clarke, 2006). Coding was led by two researchers with support from three medical students. Coders first independently reviewed seven transcripts with preliminary thematic categories in mind to develop maternal and clinician codebooks. Discrepancies between coders were examined and discussed, and the codebooks were refined. Another nine transcripts were then coded by the two primary coders to establish inter-coder reliability (pooled Cohen’s Kappa coefficient; maternal K = 0.87 and clinician K = 0.85), after which the remaining transcripts were divided among the two primary coders.
Transcript excerpts were organized into emergent themes. Because our interviews included specific questions about mindfulness in group WCC as a potential benefit, participant responses regarding barriers and facilitators to mindfulness activities were analyzed separately to avoid biasing results. Thematic saturation was reached when no new themes were identified, separately for maternal and clinician data (Starks & Trinidad, 2007). Findings were shared with two maternal and two clinician participants to confirm or challenge findings. Debrief sessions were also held with other research team members to further validate or challenge interpretations of the data. Results are reported in accordance with Consolidated Criteria for Reporting Qualitative Research Guidelines (Tong et al., 2007).
Results
Participant Characteristics
Of 76 mothers contacted for recruitment, 31 enrolled and completed telephone interviews. The majority (84%) endorsed having received some type of therapy or service in a group format, and of those participants, 73% rated their overall experience with receiving care in a group format as either excellent or very good. Most (68%) reported that they would be likely or very likely to bring their child to the OUD treatment center for WCC. Of 53 clinicians invited to participate, 13 enrolled and completed telephone interviews. All clinician participants reported experience working with mothers receiving MOUD, and most (92%) had received some form of training about substance use disorders during their careers (see Table 1).
Six themes emerged corresponding with potential barriers to implementing group WCC (Table 2), and six themes emerged as potential facilitators (Table 3). Thematic saturation was achieved by the seventeenth interview for mothers and the fourth interview for clinicians.
Barriers
Intervention Complexity: Resource Intensiveness
Clinicians noted the need for equipment, supplies, and staff for routine WCC screenings and procedures during group WCC. They also noted the need for a large enough space with an adjacent private area for individual care. Some clinicians questioned whether it was possible to fit group content and individual time for each family into a 90 min session. Clinical documentation and limited reimbursement within a fee-for-service model were also raised as potential barriers.
Loss of Privacy as a Potential Negative Outcome
While some mothers noted that they would feel comfortable discussing most topics in a group, others stated discomfort discussing topics they perceived to be private or sensitive, such as their substance use history, their relationship with their partner/child’s father, or their child’s special healthcare needs. In some cases, mothers reported concern that other mothers in the group may judge their child or their ability as a parent. Several clinicians similarly expressed concern that mothers may be hesitant to speak about personal issues within the group setting and stated that one-to-one time with each mother to address these issues may be necessary.
Intervention Difficulty: Addressing Comprehensive Medical and Psychosocial Care Needs
Some clinicians questioned the appropriateness of addressing specific medical and developmental concerns within the group setting and how this attention towards an individual family could be balanced with attention towards the whole group. They also raised concerns about obtaining child/family history, assessing development, providing tailored education and recommendations, and answering specific questions that may relate to only one child in the group. When mothers expressed perceived challenges regarding attention to individual healthcare needs during group sessions, their concerns related primarily to their own privacy and comfort.
Intervention Complexity: Intricacy of Scheduling
Participants described scheduling challenges and competing demands as potential barriers to group WCC. Mothers identified job responsibilities and OUD treatment schedules as potentially conflicting across group participants. Clinicians noted the potential difficulty of fitting group sessions into their clinic schedule, emphasizing the need for dedicated time for group WCC rather than adding it to an already fully scheduled clinic day. Participants identified inclement weather and other unforeseen circumstances as additional challenges.
Intervention Difficulty: Managing Group Dynamics
Both mothers and clinicians discussed the potential challenge of including mothers in treatment for OUD at different stages of recovery and with different levels of knowledge regarding child development and parenting. Several mothers expressed concern for group disruptions from participants arriving late, not taking the group seriously, or consistently deviating from the discussion topic. Several clinicians expressed concern that mothers may bring outside interpersonal conflict into the group setting, that a small number of participants could dominate the discussion, or that comparisons between mothers or children could disrupt the group dynamic. The importance of ground rules developed in collaboration with group participants was emphasized by some clinicians. A few clinicians also noted concern that mothers may have difficulty focusing on the content in a noisy group setting or that clinicians may be pulled in different directions when trying to address maternal information needs.
COVID-19 Exposure as a Potential Negative Outcome
Participants noted that the COVID-19 pandemic could impede implementation, and that precautions such as masking and social distancing would mitigate risk. Several clinicians noted that mandatory vaccination would help but may not be feasible. Some mothers stated that a virtual format would be preferable for group WCC during the pandemic and that they would not likely participate if this option was unavailable. Several mothers emphasized the need to protect children and mothers with chronic health conditions that may place them at higher risk for COVID-19 complications.
Facilitators
Focus on Maternal OUD and Recovery as an Intervention Benefit
Mothers described how content related to intergenerational substance use, effects of maternal substance use on child development, and maternal health/stress would be highly beneficial to include in group WCC. Both clinicians and mothers shared perspectives on potential for group WCC to facilitate health literacy through discussion and education around tailored health topics specific to children affected by maternal OUD.
Peer Support as an Intervention Benefit
Mothers and clinicians both spoke about how group WCC would normalize parenting challenges and reassure mothers. Mothers noted how group WCC would offer them an opportunity to build relationships with other mothers and allow their children to socialize with other children of their same age. They were supportive of the inclusion of other support persons in the group visit (i.e., partners, spouses, parents). Clinicians felt that community sharing would enrich the content they typically offer and provide more insight for them into this population, thereby enhancing the therapeutic relationship.
Accessibility and Coordination of Care as an Intervention Benefit
Overall, the co-location of pediatric care with maternal OUD treatment was viewed by participants as helpful to implementation. Most mothers remarked how co-location would make them feel more comfortable and would reduce barriers to access. Mothers were also interested in whether attendance to group WCC sessions could count towards their OUD treatment participation. Most clinicians remarked how they perceived it would create an enjoyable environment, both for patients and themselves.
Clinician Skills and Experience in Caring for Mothers with OUD
Participants spoke about how clinician training in substance use and experience working with families affected by maternal substance use would facilitate implementation, fostering a trusting and comfortable environment for pediatric care, and reducing stigma (Table 3). Additionally, clinicians noted training in group WCC facilitation would be imperative.
More Time for Patient Care as an Intervention Benefit
Clinicians and mothers perceived the longer visit duration in group WCC to support more time for discussion. Clinicians appreciated the opportunity to provide anticipatory guidance to multiple families in one session. They also described the longer visit as an opportunity to learn more about their patients, through more meaningful interactions and shared learning through discussion.
Clinician Continuity as an Intervention Benefit
Mothers discussed the value of continuity of care to facilitate trust and ease with the clinician. Clinicians discussed how group WCC would better facilitate the development of the therapeutic relationship through longer regular visits. They noted how this consistent interaction would nurture understanding and familiarity, leading to identification of care gaps or emergent health issues more readily.
Incorporating Mindfulness
Emergent themes corresponding with potential barriers and facilitators to incorporating mindfulness into group WCC are reported in Table 4. Mothers and clinicians expressed interest and support for mindfulness activities as part of the intervention.
Discussion
In this qualitative study, attitudes towards group WCC among mothers with OUD and clinicians seem to support our hypotheses that this intervention will improve engagement in care, parenting knowledge, and maternal-child attachment. However, several challenges may impede successful implementation if not appropriately addressed.
The potential barriers raised by our participants align with previously reported financial, structural, and procedural factors that have been shown to be important for group WCC implementation (Gresh et al., 2023). As participants have noted, staffing, training, space, and equipment are required for group WCC, underscoring the importance of a supportive policy environment and commensurate funding streams (Gresh et al., 2023; Connor et al., 2018). Examples of potential financial support include the federally-funded Healthy Start initiative, state-level funds, and in-kind service grants from Centering Healthcare Institute (National Healthy Start Association, 2023; CHI, 2023). For our project, upfront costs for staffing and equipment are supported through a federal research grant as a randomized clinical trial (Short et al., 2023). Long term, the cost effectiveness of group WCC relates to several factors including patient volume and clinician productivity (Yoshida et al., 2014). Although group WCC is typically reimbursed under traditional fee-for-service payment models, there are promising examples across the U.S. of enhanced reimbursement for group visits under a value-based payment model (Prenatal-to-3 Policy Impact Center, 2023; CHI, 2019). To maintain a sufficient volume of mothers with OUD, we anticipate needing flexible enrollment procedures, and frequent communication with high-risk obstetrical providers, birth hospitals, and OUD treatment staff. Scheduling for group WCC will require coordination between OUD treatment staff and pediatric clinical staff in the form of regular, multidisciplinary meetings.
Although most mothers in our sample reported positive experiences with group formatted care, concerns about privacy and group dynamics were raised by study participants. As recommended for all group WCC programs, we plan to use a large room with enough physical space to accommodate group activities as well as semi-private discussions (Gresh et al., 2023). Interdisciplinary co-facilitation is also generally recommended to assist the primary clinician in navigating group dynamics (Griswold & Walker, 2021; Marchel et al., 2015). Given that our group WCC sessions may include mothers in different stages of OUD recovery, we plan to incorporate a nurse practitioner from the OUD treatment staff as a co-facilitator with content expertise in OUD and familiarity with the treatment circumstances for each mother.
In order to ensure that group WCC meets the comprehensive care needs of each family, we will develop a health assessment questionnaire for group visits to facilitate history taking and identify specific concerns, as is common in other group WCC programs (Gresh et al., 2023). We will also tailor the content of group discussions to reflect parental priorities for anticipatory guidance (Goyal et al., 2023). Furthermore, we will develop printed informational handouts about these topics that are visually pleasing and easy to read. We will conduct semi-structured, individual interviews with mothers receiving group WCC during implementation to obtain feedback on group visit content, formatting, and written materials (Short et al., 2023).
COVID-19 emerged as a potential barrier, although this topic was specifically prompted. Of note, we conducted this study in late 2020, before COVID-19 vaccination became widely available. Given the continually evolving public health response to COVID-19, we anticipate that clinician and maternal attitudes will also change. Currently, our findings support the use of available federal guidance towards risk reduction, i.e. masking and encouraging vaccination (Centers for Disease Control and Prevention, 2023).
Finally, participants were overall supportive of mindfulness activities but identified potential barriers to this aspect of group WCC. Multiple clinician resources for integrating mindfulness into group WCC sessions in the form of brief breathing or movement exercises are available through Centering Healthcare Institute. We anticipate that this particular aspect of group WCC will align well with the trauma-informed, mindfulness-based practices already being implemented at this OUD treatment center (Gannon et al., 2017).
Limitations
Because participants reported their projected and not actual experiences with group WCC, these data should be interpreted with caution. Furthermore, social desirability and selection bias may have impacted responses, particularly given the response rate < 50% for both maternal and clinician participants. Clinicians who participated were mostly non-Hispanic White and female, and purposive recruitment was not used to increase sample diversity. The maternal participant sample was also disproportionately non-Hispanic White compared with our local maternal OUD treatment population, which is estimated to be approximately two-thirds non-Hispanic White and at least 20% non-Hispanic Black. Given known racial-ethnic disparities in access to MOUD, future research should focus on the perspectives of minoritized parents with OUD and interventions to improve health equity (Gao et al., 2022; Tucker, 2022).
Conclusions
Group WCC is perceived to confer multiple advantages over traditional WCC for mothers with OUD, but with multiple implementation challenges. Findings are being used to adapt group WCC for mothers with OUD and their children, and to integrate this intervention within one maternal OUD treatment program. Future research will study implementation outcomes such as attendance and fidelity to the intervention, as well as family outcomes (WCC engagement and experience, parenting knowledge, and maternal-child attachment).
Data Availability
Data is available from the authors upon request.
Code Availability
Not applicable.
Change history
28 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10995-023-03774-6
Abbreviations
- AAP:
-
American academy of pediatrics
- CHI:
-
Centering healthcare institute
- MOUD:
-
Medications for opioid use disorder
- OUD:
-
Opioid use disorder
- WCC:
-
Well child care
References
Abatemarco, D. J., Gubernick, R. S., LaNoue, M. D., Pohlig, R. T., Slovin, S. R., Healy, J. A., & Kairys, S. (2018). Practicing safety: A quality improvement intervention to test tools to enhance pediatric psychosocial care for children 0–3 years. Primary Health Care Research & Development, 19(4), 365–377. https://doi.org/10.1017/S1463423617000810
Abatemarco, D. J., Kairys, S. W., Gubernick, R. S., & Kairys, J. A. (2008). Expanding the pediatrician’s black bag: A psychosocial care improvement model to address the “new morbidities.” Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources, 34(2), 106–115.
American Academy of Pediatrics. (2023). Maternal-infant health and opioid use program: recovery-friendly family-centered pediatrics. https://www.aap.org/en/patient-care/opioids/maternal-infant-health-and-opioid-use-program/recovery-friendlypediatric- care/
Beldick, S. R., Rohde, J. F., Short, V. L., Abatemarco, D. J., & Goyal, N. K. (2023). Pediatric primary care diagnoses among children with intrauterine opioid exposure. Journal of Health Care for the Poor and Underserved, 34(1), 161–179. https://doi.org/10.1353/hpu.2023.0011
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Centering Healthcare Institute. (2019). Aligning value-based payment with centeringpregnancy. Retrieved April 9, 2019, from https://www.centeringhealthcare.org/uploads/files/Aligning-Value-Based-Payment-with-CenteringPregnancy.pdf
Centering Healthcare Institute. (2023). http://www.centeringhealthcare.org
Centers for Disease Control and Prevention. (2023). Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
Connor, K. A., Duran, G., Faiz-Nassar, M., Mmari, K., & Minkovitz, C. S. (2018). Feasibility of implementing group well baby/well woman dyad care at federally qualified health centers. Academic Pediatrics, 18(5), 510–515. https://doi.org/10.1016/j.acap.2017.09.011
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50. https://doi.org/10.1186/1748-5908-4-50
DeLago, C., Dickens, B., Phipps, E., Paoletti, A., Kazmierczak, M., & Irigoyen, M. (2018). Qualitative evaluation of individual and group well-child care. Academic Pediatrics, 18(5), 516–524. https://doi.org/10.1016/j.acap.2018.01.005
Demianczyk, A. C., Bechtel Driscoll, C. F., Karpyn, A., Shillingford, A., Kazak, A. E., & Sood, E. (2022). Coping strategies used by mothers and fathers following diagnosis of congenital heart disease. Child: Care, Health and Development, 48(1), 129–138. https://doi.org/10.1111/cch.12913
Fenick, A. M., Leventhal, J. M., Gilliam, W., & Rosenthal, M. S. (2020). A randomized controlled trial of group well-child care: Improved attendance and vaccination timeliness. Clinical Pediatrics, 59(7), 686–691. https://doi.org/10.1177/0009922820908582
Gannon, M., Mackenzie, M., Kaltenbach, K., & Abatemarco, D. (2017). Impact of mindfulness-based parenting on women in treatment for opioid use disorder. Journal of Addiction Medicine, 11(5), 368–376. https://doi.org/10.1097/ADM.0000000000000336
Gao, Y. A., Drake, C., Krans, E. E., Chen, Q., & Jarlenski, M. P. (2022). Explaining racial-ethnic disparities in the receipt of medication for opioid use disorder during pregnancy. Journal of Addiction Medicine, 16(6), e356–e365. https://doi.org/10.1097/ADM.0000000000000979
Gaskin, E., Yorga, K. W., Berman, R., Allison, M., & Sheeder, J. (2021). Pediatric group care: A systematic review. Maternal and Child Health Journal, 25(10), 1526–1553. https://doi.org/10.1007/s10995-021-03170-y
Goyal, N. K., Rohde, J. F., Short, V., Patrick, S. W., Abatemarco, D., & Chung, E. K. (2020). Well-child care adherence after intrauterine opioid exposure. Pediatrics. https://doi.org/10.1542/peds.2019-1275
Goyal, N.,K., Sood, E., Gannon, M., Harris, G., Hand, D.J., Abatemarco, D.J., Short, V. L. (2023). Priorities for well child care of families affected by parental opioid use disorder (in press). Journal of Addiction Medicine.
Gresh, A., Wilson, D., Fenick, A., Patil, C. L., Coker, T., Rising, S. S., Glass, N., & Platt, R. (2023). A conceptual framework for group well-child care: A tool to guide implementation, evaluation, and research. Maternal and Child Health Journal, 27, 991–1008. https://doi.org/10.1007/s10995-023-03641-4
Gressler, L. E., Shah, S., & Shaya, F. T. (2019). Association of criminal statutes for opioid use disorder with prevalence and treatment among pregnant women with commercial insurance in the united states. JAMA Network Open, 2(3), e190338. https://doi.org/10.1001/jamanetworkopen.2019.0338
Griswold S. A., & Walker H. The Joys & Challenges of Inclusive Co-Facilitation. Centering Healthcare Institute Webinar. Retrieved December 1, 2021, from https://centeringhealthcare.org/store/webinars/the-joys-challenges-of-inclusive-co-facilitation-12-01-21
Grossman, M. R., Lipshaw, M. J., Osborn, R. R., & Berkwitt, A. K. (2018). A novel approach to assessing infants with neonatal abstinence syndrome. Hospital Pediatrics, 8(1), 1–6. https://doi.org/10.1542/hpeds.2017-0128
Hennink, M., & Kaiser, B. N. (2022). Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Social Science & Medicine, 292, 114523. https://doi.org/10.1016/j.socscimed.2021.114523
Irigoyen, M. M., Leib, S. M., Paoletti, A. M., & DeLago, C. W. (2021). Timeliness of immunizations in centeringparenting. Academic Pediatrics, 21(6), 948–954. https://doi.org/10.1016/j.acap.2020.11.022
Jarlenski, M. P., Krans, E. E., Kim, J. Y., Donohue, J. M., James, A. E., Kelley, D., Stein, B. D., & Bogen, D. L. (2020). Five-year outcomes among medicaid-enrolled children with in utero opioid exposure. Health Affairs (project Hope), 39(2), 247–255. https://doi.org/10.1377/hlthaff.2019.00740
Kaplan, H. C., Kuhnell, P., Walsh, M. C., Crowley, M., McClead, R., Wexelblatt, S., Ford, S., Provost, L. P., Lannon, C., Macaluso, M., Ohio Perinatal Quality Collaborative. (2020). Orchestrated testing of formula type to reduce length of stay in neonatal abstinence syndrome. Pediatrics. https://doi.org/10.1542/peds.2019-0914
Maguire, D. J., Taylor, S., Armstrong, K., Shaffer-Hudkins, E., Germain, A. M., Brooks, S. S., Cline, G. J., & Clark, L. (2016). Long-term outcomes of infants with neonatal abstinence syndrome. Neonatal Network: NN, 35(5), 277–286. https://doi.org/10.1891/0730-0832.35.5.277
Marchel, M. A., Winesett, H., Hall, K., Luke, S., Duluth, P., & Ladd, M. C. (2015). Holding the holders: An interdisciplinary group well-child model. Zero to Three Journal, 2015, 15–20.
National Healthy Start Association. (2023). Healthy Start Initiative. https://www.nationalhealthystart.org/healthy-start-initiative/
National Institutes of Health. (2023). Inclusive and gender-neutral language. https://www.nih.gov/nih-style-guide/inclusive-gender-neutral-language#pregnant-people
Oldfield, B. J., Rosenthal, M. S., & Coker, T. R. (2020). Update on the feasibility, acceptability, and impact of group well-child care. Academic Pediatrics, 20(6), 731–732. https://doi.org/10.1016/j.acap.2020.02.029
Patrick, S. W. (2017). A comprehensive approach to the opioid epidemic. Obstetrics and Gynecology, 130(1), 7–9. https://doi.org/10.1097/AOG.0000000000002118
Platt, R. E., Acosta, J., Stellmann, J., Sloand, E., Caballero, T. M., Polk, S., Wissow, L. S., Mendelson, T., & Kennedy, C. E. (2022). Addressing psychosocial topics in group well-child care: A multi-method study with immigrant Latino families. Academic Pediatrics, 22(1), 80–89. https://doi.org/10.1016/j.acap.2021.05.001
Prenatal-to-3 Policy Impact Center. (2023). Group prenatal care. https://pn3policy.org/pn-3-state-policy-roadmap-2022/us/group-prenatal-care/
Pryor, J. R., Maalouf, F. I., Krans, E. E., Schumacher, R. E., Cooper, W. O., & Patrick, S. W. (2017). The opioid epidemic and neonatal abstinence syndrome in the USA: A review of the continuum of care. Archives of Disease in Childhood. Fetal and Neonatal Edition, 102(2), F183–F187. https://doi.org/10.1136/archdischild-2015-310045
Rizzo, R. A., Neumann, A. M., King, S. O. C., Hoey, R. F., Finnell, D. S., & Blondell, R. D. (2014). Parenting and concerns of pregnant women in buprenorphine treatment. MCN. The American Journal of Maternal Child Nursing, 39(5), 319–324. https://doi.org/10.1097/NMC.0000000000000066
Rohde, J. K., Goyal, N. K., Canter, K., Houff, M., Bodt, B., Pachter, L., & Di Guglielmo, M. D. (2023). Pediatric primary care clinicians’ views on needs and challenges in caring for infants with intrauterine opioid exposure and their families. Journal of Child Health Care. https://doi.org/10.1177/1367493523116867
Short, V. L., Abatemarco, D. J., Sood, E., Hand, D. J., Gannon, M., Hossain, M. J., & Goyal, N. K. (2023). The Child Healthcare at MATER Pediatric Study (CHAMPS): A 2-arm cluster randomized control trial of group well child care for mothers in treatment for opioid use disorder and their children. Trials, 24, 333. https://doi.org/10.1186/s13063-023-07357-2
Short, V. L., Gannon, M., Sood, E., Harris, G., Kale, A., Abatemarco, D. J., Hand, D. J., & Goyal, N. (2022). Opportunities to increase well-child care engagement for families affected by maternal opioid use disorder: Perceptions of mothers and clinicians. Academic Pediatrics. https://doi.org/10.1016/j.acap.2022.07.013
Short, V. L., Goyal, N. K., Chung, E. K., Hand, D. J., & Abatemarco, D. J. (2019). Perceptions of pediatric primary care among mothers in treatment for opioid use disorder. Journal of Community Health, 44(6), 1127–1134. https://doi.org/10.1007/s10900-019-00701-1
Starks, H., & Trinidad, S. B. (2007). Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research, 17(10), 1372–1380. https://doi.org/10.1177/1049732307307031
Sutter, M. B., Gopman, S., & Leeman, L. (2017). Patient-centered care to address barriers for pregnant women with opioid dependence. Obstetrics and Gynecology Clinics of North America, 44(1), 95–107. https://doi.org/10.1016/j.ogc.2016.11.004
Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
Tucker, E. B. (2022). Mandated reporting of perinatal substance use: The root of inequity. JAMA Pediatrics, 176(11), 1073–1075. https://doi.org/10.1001/jamapediatrics.2022.3404
Yoshida, H., Fenick, A. M., & Rosenthal, M. S. (2014). Group well-child care: An analysis of cost. Clinical Pediatrics, 53(4), 387–394. https://doi.org/10.1177/0009922813512418
Funding
This study was supported by the Agency for Healthcare Research and Quality (AHRQ), 1R18HS027399-01. The funding agency was not involved in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
NKG conceptualized the study, created the survey and interview guides, and drafted and revised the manuscript. MG helped to plan the study, analyzed the data, and drafted and revised the manuscript. ES helped to plan the study, analyzed the data, and drafted and revised the manuscript. GH collected and analyzed the data, and drafted and revised the manuscript. EF collected and analyzed the data, and drafted and revised the manuscript. DA helped to plan the study, interpreted the data, and drafted and revised the manuscript. DH helped to plan the study, interpreted the data, and drafted and revised the manuscript. SL helped to plan the study, interpreted the data, and drafted and revised the manuscript. VS conceptualized the study, created the survey and interview guides, recruited and enrolled study participants, collected the data, and contributed to manuscript writing and revision. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Ethical Approval
This study was reviewed and approved by our Institutional Review Board.
Consent to Participate
All study participants provided informed consent.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goyal, N., Gannon, M., Sood, E. et al. Group Well Child Care for Mothers with Opioid Use Disorder: Framework for Implementation. Matern Child Health J 27 (Suppl 1), 75–86 (2023). https://doi.org/10.1007/s10995-023-03762-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03762-w