Abstract
Background
Mothers’ awareness of hearing loss, its risk factors, and available detection and intervention choices have been well known to play an essential role in the early detection and intervention of hearing loss.
Objective
To investigate the knowledge and attitude of Syrian mothers toward infant hearing loss, early identification, and intervention.
Methods
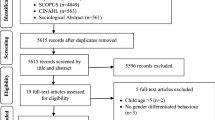
The “Maternal Views on Infant Hearing Loss” questionnaire was adapted and translated into Arabic and then administered to 100 Syrian mothers living in different neighborhoods in Ankara within the age range of 18–68 years old. The internal consistency for the main domains of the questionnaire was tested by Cronbach’s alpha coefficient. Descriptive statistics and Spearman’s rank correlation coefficient were used to evaluate the responses.
Results
The highest level of knowledge about the risk factors was about noise exposure (76%), while the lowest level of knowledge was about jaundice (25%). While 98% of the mothers had a positive attitude toward early detection, 97% of them did not mind the early intervention.
Conclusions
The present findings showed the need to improve mothers’ awareness about infant hearing loss risk factors, available detection, and intervention. Such results may help in performing programs that aim to increase awareness about hearing loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
Different studies have been performed to study the effect of maternal awareness on the application of newborn hearing screening or to study the factors affecting it. These studies were done in different geographies, but this is the first study to be done on Syrian refugees in the host country, Turkey. As previous studies showed that there is a need to increase mothers’ awareness of infant hearing loss, this study shows the need to increase refugees mothers’ awareness of infant hearing loss.
Introduction
Permanent hearing loss is a prevalent disorder in newborns as the rate of permanent unilateral and bilateral hearing loss worse than 40dB varies from 1 to 6 per 1000 (Bussé et al., 2020). According to World Health Organization, almost 80% of people with hearing loss live in low- and middle-income countries (WHO, 2021). Hearing loss is classified according to its time of onset into congenital and acquired hearing loss (Smith et al., 2005). Causes of congenital hearing loss are divided into genetic and nongenetic causes (Hosford-Dunn et al., 2007). Genetic causes can be syndromic, such as Alport syndrome and Usher syndrome, or nonsyndromic, such as mutations in the connexin 26 gene (Rehm, 2005). Nongenetic causes of congenital hearing loss include hypoxia, hyperbilirubinemia, ototoxic medications, very low birth weight, congenital infections such as cytomegalovirus, neonatal herpes simplex virus infection, rubella, syphilis, toxoplasmosis, and varicella syndrome (Roizen, 2003). Acquired hearing loss is a late-onset hearing loss that has different causes, such as head trauma, noise exposure, otitis media, meningitis, mumps, and measles viruses (Roizen, 2003; Smith et al., 2005). Regardless of the type of hearing loss, a significant language delay and poor academic achievements are the main effects of hearing loss on children (Yoshinaga-Itano et al., 1998). Although language deprivation is highly common among children with hearing difficulties, not all children with hearing difficulties are affected by it to the same degree. The exposure and the degree of access to a signed language, spoken language, or both are adequate to boost the mastery of the first language on a developmentally proper timetable (Hall et al., 2019).
Universal newborn hearing screening (UNHS) is a protocol being used in many countries globally. This protocol helps with the early identification of congenital hearing loss (Wroblewska-Seniuk et al., 2017). According to the Joint Committee on Infant Hearing, the identification of children with all types and degrees of hearing loss and lowering the age at the time of diagnosis are the main goals of UNHS. Indeed, early identification of hearing loss and early intervention ensure better language development (Yoshinaga-Itano et al., 1998).
The application of the UNHS is facing different challenges, such as lack of funds, shortages of staff, inadequate support services, and low public awareness (Olusanya et al., 2004). In fact, studies about the knowledge and attitude toward infant hearing loss have been performed in different geographical regions for different purposes. For example, studies have been conducted to support the success of UNHS programs by investigating maternal awareness and attitudes toward hearing loss in the populations of Nigeria and India (Olusanya et al., 2006; Ravi et al., 2016). Another study was performed in Northern India to gain insights into nurses’ knowledge and attitudes toward hearing loss in infants (Sanju et al., 2018). While a study in southwestern Uganda investigated factors associated with hearing aids refusal among mothers (Seguya et al., 2021). Another study from the Solomon Islands aimed to develop health promotion activities for reducing preventable causes of congenital hearing loss (Kaspar et al., 2017). Regarding the studies performed in Arab countries, two studies have been performed in Saudi Arabia and the United Arab Emirates to evaluate parental knowledge and attitudes toward childhood hearing loss (Alsudays et al., 2020; Ayas & Yaseen, 2021). These studies show the need to increase awareness and knowledge among parents about congenital hearing loss and UNHS, as poor knowledge about important risk factors such as jaundice and measles has been noticed, in addition to poor knowledge about early intervention and identification (Olusanya et al., 2006; Rajagopalan et al., 2014; Swanepoel & Almec, 2008).
Since 2011, the number of Syrians in Turkey has continued to increase due to the Syrian crisis. According to the Republic of Turkey Ministry of Interior Directorate General of Migration Management’s website, the number of Syrians under temporary protection status was 3.638.104 on 23/12/2020. Difficulties such as economic concerns, safety, food, and shelter problems that refugees face due to war and immigration cause malnutrition and stress for the pregnant woman, which causes impairment in fetal development (Cikrikci et al., 2020).
Since the rate of hearing loss and the UNHS test ‘Refer’ among Syrian newborns is higher than that among Turkish newborns, the rate of risk factors such as intensive care unit, consanguineous marriage, congenital infection, prematurity, low birth weight, and hyperbilirubinemia are also higher among Syrian newborns (Kaplama et al., 2020; Yücel et al., 2019). Thus, there is a need to increase awareness among Syrian mothers about infant hearing loss, its risk factors, and how the intervention and detection process would be.
To the best of our knowledge, there are no studies about maternal knowledge and attitudes toward hearing loss among Syrian refugees. This cross-sectional study aims to investigate the views of Syrian mothers in Ankara-Turkey on infant hearing loss and their attitudes toward early identification and intervention to help develop programs for increasing awareness of hearing loss.
Materials and Methods
Ethics approval was obtained on 30/03/2021 from Hacettepe University Non-Interventional Clinical Research Ethics Committee with the registration number of GO 21/70.
Subjects
This survey-based study was conducted among 100 Syrian mothers who lived in Ankara/Turkey. Participants were reached by visiting the neighborhoods in Ankara with a high Syrian population. To be included in the study, the mother had to be Syrian, older than 18 years, came to Turkey after 2011, resided in Ankara, and spoke Arabic as the native language. Participation in this study was voluntary. The mother was excluded from the study if she refused voluntary participation or did not meet any of the inclusion criteria. The participants’ demographic information is given in Table 1.
Questionnaire
The “Maternal views on infant hearing loss” questionnaire developed by Olusanya et al., (2006) was adapted and translated into Arabic after obtaining permission from Bolajoko O. Olusanya. At the beginning, the forward translation from English to Arabic was performed by an Arabic native translator, then the translation was reviewed by another native Arabic speaker. Following the backward translation from Arabic to English by another high proficient Arabic English translator, the translated questionnaire was compared with the original one, cognitive interviews were performed, and the translation was approved to be appropriate to use. The adapted questionnaire consisted of three parts and 25 questions. Ten questions aimed to collect demographic and socioeconomic information, and 12 questions in the knowledge part aimed to measure the knowledge about hearing loss risk factors and detection. Finally, the last part contained 3 questions about attitudes toward early detection and intervention.
Procedure
The interviews were conducted by two native Arabic speakers. Face-to-face interviews were conducted in the neighborhoods for 1 month, from June 2021 to July 2021. The study aims were explained to the participants, and they were given a phone number to contact if they had any questions about the study. The interviewers documented the participants’ consent and responses by using Google Forms.
Statistical Analysis
Each of the responses was evaluated with the following scores: no = 1; not sure = 2; yes = 3, for the purpose of analysis. Statistical Package for Social Sciences (SPSS version 23) for Mac was used for data analysis. The data distribution was statistically tested by the Shapiro-Wilk test which showed that data were abnormally distributed, wherefore, nonparametric statistical tests were used. Descriptive statistics were performed to incorporate frequency distributions, medians, and quartiles. Possible associations between mothers’ demographic profiles and their responses were explored by Spearman’s rank correlation coefficient. Only statistically significant correlations were reported in the results. For statistical significance, p < .05 was used as a cutoff. To test the internal consistency of the questionnaire, Cronbach’s analysis was applied.
Results
The present outcomes showed that 70% of the mothers were aware that hearing loss could be congenital. Concerning the knowledge of risk factors, the highest scores were for prolonged noise exposure (76%), high fever (67%), and ear discharge (66%). On the other hand, the lowest knowledge scores were for jaundice (25%), convulsion (32%), native medicine (34%), and measles (36%).
Regarding knowledge about identification and intervention, while 74% of the mothers believed that hearing loss identification was possible soon after birth, 14% of them did not. However, only 54% of them were aware that early intervention was possible.
With regard to attitude, almost all mothers had a positive attitude toward detection and intervention, as 98% of mothers wanted their child to be tested right after birth, and 97% of them did not mind using the hearing aids if necessary. However, providing hearing aids at no cost did not change this percentage. Table 2 summarizes the survey results and percentiles, while Fig. 1 shows the participants’ knowledge regarding the risk factors.
The education level of the mothers showed that 9% (n = 9) of the mothers were not educated at all, 60% (n = 60) of them were educated to elementary school, 19% (n = 19) of them were educated to middle school, 8% (n = 8) of them were educated to high school, and 4% (n = 4) were educated to university. Moderate positive correlations were found between the education level and each of the statements “Babies can be born with hearing loss” (r = .242, p = .015), “Prolonged noise exposure can cause hearing loss” (r = .260, p = .009), and “Detection is possible soon after birth” (r = .303, p = .002). Additionally, a correlation was found between the “Do you have children born in Turkey” demographic question and the “Detection is possible soon after birth” statement (r = .381, p = .001). Regarding the question of hearing loss cases in the family, one of the mothers reported having a hearing loss, 2 mothers reported having children with hearing loss, and 5 mothers reported having family members with hearing loss. The Cronbach’s alpha coefficient was 0.733 for knowledge and 0.741 for attitude, meaning that the internal consistency of the questionnaire was acceptable.
Discussion
This study investigated the knowledge and attitude of Syrian mothers in Ankara toward infant hearing loss. The present results showed that there was a good level of knowledge about hearing loss and its risk factors among Syrian mothers in Ankara.
Of the participants, 70% were aware that hearing loss could be congenital, which was explained by the answer “Yes” to the “Babies can be born with hearing loss” statement. Such results were consistent with studies by Wang et al., (2017), Alsudays et al., (2020), and Olusanya et al., (2006), as the knowledge about the congenital hearing loss was high in their studies but was contradictory to the results of Ayas & Yaseen (2021), Kaspar et al., (2017) and Ravi et al., (2016), as the awareness about congenital hearing loss was low. Such inconsistencies might be due to educational levels, as a statistically significant correlation was found between the educational level and this statement in the present study (r = .242, p = .015). Additionally, differences in study regions, populations, and cultural beliefs might have affected the results.
The highest positive response toward the risk factors in our study was for prolonged noise exposure, as 76% of participants answered with “yes” to the “Prolonged noise exposure can cause hearing loss” statement. Such findings might be related to the education level, as a significant correlation was found between this statement and the education level (r = .260, p = .009). Furthermore, mothers’ experience with noise exposure during the war might have had its effect too, as some mothers reported that they had relatives who lost their hearing due to explosions. This result was consistent with the study by Wang et al., (2017) conducted in China, showing that the highest awareness among participants was for prolonged noise exposure. The authors explained their results by the effort that the government and media carried out, such as the promulgation of the Law of the People’s Republic of China on the Prevention and Control of Environmental Noise Pollution in 1996. In contrast, the lowest awareness among participants in the present study was toward jaundice, as only 25% of the mothers answered with “yes” to the “Jaundice can cause hearing loss” statement. Wang et al., (2017) and Alsudays et al., (2020) reported a similar result, as the participants had the lowest awareness toward jaundice, and this was a surprising finding since jaundice is well known to be very frequent in infants. However, this might be due to the misconception that jaundice would be normal in infancy regardless of its severity (Seguya et al., 2021).
Regarding ear discharge, our findings were consistent with Kaspar et al., (2017), Ayas & Yaseen (2021), Wang et al., (2017), Swanepoel & Almec (2008), Olusanya et al., (2006), and Alsudays et al., (2020), as a high percentage of mothers answered “yes” to the statement “Ear discharge can cause hearing loss”. These results were probably due to the high prevalence of otitis media with effusion in the developing countries, which lends ear discharge as a known cause of hearing loss (Olusanya et al., 2006). Similar to ear discharge, high fever was also highly recognized as a risk factor among mothers in the present study, which agreed with Wang et al., (2017) and Olusanya et al., (2006), but it was less frequently identified by mothers in other countries, such as the United Arab Emirates and Solomon Islands (Ayas & Yaseen, 2021; Swanepoel & Almec, 2008). Similar to the study by Wang et al., (2017), the reason for this high knowledge in the present study might be because of social knowledge. In Syrian society, “high fever can cause brain damage” has been a popular saying, as in the Chinese population.
Indeed, for other risk factors (drugs, convulsions, asphyxia, native medicine, and measles), the knowledge was poor to some extent, as the percentage of knowledge for these risk factors was 46%, 32%, 44%, 34%, and 36%, respectively. The maternal knowledge about the ototoxicity effect of drugs in previous studies Olusanya et al., (2006), Seguya et al., (2021), and Ravi et al., (2016), was comparable with the present results but surprisingly was different from Kaspar et al., (2017), while the percentage of positive answers was 43.3%. The author considered it to be good knowledge and attributed it to the quinine-based malaria treatment, which caused ototoxicity. With respect to measles, contradictory results were reported in previous studies; for example, in the study by Olusanya et al., (2006), where the study was performed in Nigeria, a high level of knowledge was reported by mothers about measles as a risk factor for hearing loss. Additionally, in Seguya et al., (2021) where the study was performed in Uganda, a high level of knowledge was detected for measles. In contrast, in Wang et al., (2017) and Swanepoel & Almec (2008), where these studies were performed in China and South Africa, respectively, the knowledge of measles was poor, similar to the present results. The reason for this difference was attributed to the well-established immunization program in Nigeria, which aided parental knowledge of various diseases, and to the high prevalence of measles in many communities that made them aware of it (Olusanya et al., 2006). The poor knowledge about the other risk factors might be a result of the shortage of education given to mothers during antenatal care (Swanepoel & Almec, 2008).
Regarding mothers’ knowledge of early detection and intervention, the present findings revealed a good level, as 74% answered with “yes” to the “Detection is possible soon after birth” statement, while only 54% answered with “yes” to the “Hearing impaired children can still hear & speak” statement, however, many mothers assured that only when the intervention been done in appropriate time, hearing and speaking might be developed. Indeed, not all deaf and hard of hearing children may have the access to the spoken language, in this condition the sign language is a choice. Furthermore, children who are exposed to sign language during infancy can develop age-expected vocabulary skills, also, early visual language experience affected children’s letter-writing skills and supported literacy development (Caselli et al., 2021; Wilbur, 2000). These results were in line with Wang et al., (2017) and Swanepoel & Almec (2008), but the percentages were higher than those in Alsudays et al., (2020) and Ayas & Yaseen (2021). Such differences might be caused by the lack of programs that might increase community awareness among mothers, as Ayas & Yaseen (2021) explained. Additionally, education level might have affected this, as a statistically significant correlation was found between the responses to the “detection is possible soon after birth” statement and the education level (r = .303, p = .002). Furthermore, another correlation was found between the same statement and the demographic question “Do you have children born in Turkey?” (r = .381, p = .001), which might have explained that the mothers’ knowledge of this statement improved by their experience as newborn hearing screening has been applied in Turkey.
Almost all mothers in this study had an overwhelmingly positive attitude toward early detection and intervention, as 98% of them positively answered the “would like baby tested after birth” question, and 97% of them reported that their child would use hearing aids if needed. Furthermore, providing hearing aids at no cost did not change this percentage. Similar results were reported in other studies despite the difference in region and culture (Alsudays et al., 2020; Olusanya et al., 2006; Swanepoel & Almec, 2008; Wang et al., 2017). In contrast, a study from India reported that the percentage of positive attitudes toward hearing aid usage was only 54.3%, which might be a result of the social stigma correlated with hearing aid use (Ravi et al., 2016).
Despite the presence of some statistically significant correlations between responses and demographic information, we assumed that having a larger sample might have improved these correlations. More specifically, the effects of education level on the awareness could be clearer if there was a larger number of educated mothers, but in this study, most of the mothers had low education level.
While conducting this study, several limitations were faced due to the COVID-19 pandemic. The interview should have been done in the open air and kept short. Otherwise, more detailed information or data could have been collected. Another limitation was the fear of some refugees talking with the researchers, which made the number of the present sample smaller than targeted. Furthermore, most of the participants were from the same city in Syria, so further studies with a more diverse sample in a larger population are believed to be needed. It would also be good to examine the relationship between the level of mothers’ knowledge and the development of children in future studies. Evaluating knowledge with a single short questionnaire is the primary limitation. Despite this limitation, valuable data were presented in this population. Moreover, having no information about mothers’ or family members’ hearing loss type, degree and causes is thought to be an important limitations of the present study. However, the present study in Syrian mothers is a first attempt towards understanding their awareness of infant hearing loss, its symptoms, and risk factors. Syrian refugees may still be in a period of integration to a country other than their motherland and they may still have difficulties to have access to social rights such as newborn hearing screening programs. Research for their awareness may strongly support their access to early detection of hearing loss as well as to efficient intervention methods such as hearing aids or cochlear implants.
Despite the good knowledge level of some risk factors, the present results ensured that there was a need to increase refugees’ awareness about hearing loss, its risk factors, available early intervention and detection procedures through well-planned programs, or by providing brochures in the most visited healthcare centers.
Conclusions
Mothers’ responses to the Arabic version of “The Maternal Views on Infant Hearing Loss” questionnaire in this study reveal good knowledge about hearing loss and its risk factors in infants, with an excellent attitude toward early detection and intervention. However, there is still a need to increase the knowledge about other widespread risk factors. Increasing awareness could be done through organizing programs in partnership with governmental and non-governmental organizations that care about refugees or by supplying maternal care centers with appropriate brochures about hearing loss.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Alsudays, A. M., Alharbi, A. A., Althunayyan, F. S., Alsudays, A. A., Alanazy, S. M., Al-Wutay, O., & Alenezi, M. M. (2020). Parental knowledge and attitudes to childhood hearing loss and hearing services in Qassim, Saudi Arabia. BMC pediatrics, 20(1), 1–6
Ayas, M., & Yaseen, H. (2021). Knowledge and Attitudes of Parents towards Childhood Hearing Loss and Pediatric Hearing Services in Sharjah, United Arab Emirates. International Journal of Environmental Research and Public Health, 18(12), 6188
Bussé, A. M., Hoeve, H. L., Nasserinejad, K., Mackey, A. R., Simonsz, H. J., & Goedegebure, A. (2020). Prevalence of permanent neonatal hearing impairment: systematic review and Bayesian meta-analysis. International journal of audiology, 59(6), 475–485
Caselli, N., Pyers, J., & Lieberman, A. M. (2021). Deaf children of hearing parents have age-level vocabulary growth when exposed to American Sign Language by 6 months of age. The Journal of Pediatrics, 232, 229–236
Cikrikci, S., Deni̇z, H., & Gulsen, S. (2020). Comparison of Hearing Screening Results of Syrian Refugees and Turkish Newborns.International journal of pediatric otorhinolaryngology,110095
Hall, M. L., Hall, W. C., & Caselli, N. K. (2019). Deaf children need language, not (just) speech. First Language, 39(4), 367–395
Hosford-Dunn, H., Roeser, R. J., & Valente, M. (2007). Audiology: diagnosis. Thieme
Kaplama, M. E., Yukkaldiran, A., & Ak, S. (2020). Newborn hearing screening results: Comparison of Syrian and Turkish newborns; factors influencing the difference. International journal of pediatric otorhinolaryngology, 138, 110390
Kaspar, A., Newton, O., Kei, J., Driscoll, C., Swanepoel, D. W., & Goulios, H. (2017). Parental knowledge and attitudes to childhood hearing loss and hearing services in the Solomon Islands. International journal of pediatric otorhinolaryngology, 103, 87–92
Olusanya, B., Luxon, L., & Wirz, S. (2004). Benefits and challenges of newborn hearing screening for developing countries. International journal of pediatric otorhinolaryngology, 68(3), 287–305
Olusanya, B., Luxon, L., & Wirz, S. (2006). Maternal views on infant hearing loss in a developing country. International journal of pediatric otorhinolaryngology, 70(4), 619–623
Rajagopalan, R., Selvarajan, H. G., Rajendran, A., & Ninan, B. (2014). Grandmothers’ perspective on hearing loss in children and newborn hearing screening. Indian Journal of Otology, 20(1), 20
Ravi, R., Yerraguntla, K., Gunjawate, D. R., Rajashekhar, B., Lewis, L. E., & Guddattu, V. (2016). Knowledge and attitude (KA) survey regarding infant hearing loss in Karnataka, India. International journal of pediatric otorhinolaryngology, 85, 1–4
Rehm, H. L. (2005). A genetic approach to the child with sensorineural hearing loss. Paper presented at the Seminars in perinatology
Roizen, N. J. (2003). Nongenetic causes of hearing loss. Mental retardation and developmental disabilities research reviews, 9(2), 120–127
Sanju, H. K., Aggarwal, K., Choudhary, M., & Yadav, A. K. (2018). Knowledge and attitude of nurses towards infant hearing impairment in North India. Ind J Anat Sur Head Neck Brain, 4(1), 9–13
Seguya, A., Bajunirwe, F., Kakande, E., & Nakku, D. (2021). Maternal knowledge on infant hearing loss and acceptability of hearing aids as an intervention at a Referral Hospital in southwestern Uganda. International journal of pediatric otorhinolaryngology, 145, 110722
Smith, R. J., Bale Jr, J. F., & White, K. R. (2005). Sensorineural hearing loss in children. The Lancet, 365(9462), 879–890
Swanepoel, D., & Almec, N. (2008). Maternal views on infant hearing loss and early intervention in a South African community. International journal of audiology, 47(sup1), S44–S48
Wang, X., Wu, D., Zhao, Y., Li, D., & He, D. (2017). Knowledge and attitude of mothers regarding infant hearing loss in Changsha, Hunan province, China. International journal of audiology, 56(12), 997–1002
Wilbur, R. B. (2000). The Use of ASL to Support the Development of English and Literacy. The Journal of Deaf Studies and Deaf Education, 5(1), 81–104. doi:https://doi.org/10.1093/deafed/5.1.81
World Health Organization (2021). Deafness and hearing loss. Fact sheets. Retrieved from https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
Wroblewska-Seniuk, K. E., Dabrowski, P., Szyfter, W., & Mazela, J. (2017). Universal newborn hearing screening: methods and results, obstacles, and benefits. Pediatric research, 81(3), 415–422
Yoshinaga-Itano, C., Sedey, A. L., Coulter, D. K., & Mehl, A. L. (1998). Language of early-and later-identified children with hearing loss. Pediatrics, 102(5), 1161–1171
Yücel, A., Alataş, N., Yücel, H., Güllüev, M., Özsöz, E., & Uğur, C. (2019). Newborn hearing screening results of refugees living in our city and the factors affecting the results. International journal of pediatric otorhinolaryngology, 123, 187–190
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Diala Hussein, as the primary author contributed to study conception/design, data collection/analysis and writing of the paper, Hilal Dinçer D’Alessandro contributed to study design, data analysis and scientific review, Merve Özbal Batuk contributed to study design and scientific review, Amar Ekhwan contributed to study design and data collection, and Gonca Sennaroğlu contributed to study design and scientific review.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Ethic approval was obtained on 30/03/2021 from Hacettepe University Non-Interventional Clinical Research Ethics Committee with the registration number of GO 21/70.
Consent to Participate
Appropriate consents were taken from the participants.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hussein, D., D’Alessandro, H.D., Batuk, M.Ö. et al. Views of Syrian Mothers in Ankara on Infant Hearing Loss: Cross-sectional Survey. Matern Child Health J 26, 2247–2253 (2022). https://doi.org/10.1007/s10995-022-03488-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-022-03488-1