Abstract
It is a well-known fact that the extension of the surgical intervention influences both the success and time of the patient’s recovery, the degree of the blood loss, i.e., overall the patients’ surgical burden. Disease itself determines extent of surgical procedure (minor, intermediate or major surgery), which affects the risk and frequency of complications. Previous works have contributed to the validation of differential scanning calorimetry (DSC) as a potential non-invasive tool for diagnosing and monitoring several illnesses. Hence, the main goal of this study was to measure the effect of each surgical intervention on its own to blood plasma composition. Peripheral venous blood samples were collected from patients who underwent minor (n = 8), intermediate (n = 9) and major surgical interventions (n = 7). According our DSC data of blood plasma components, from the thermodynamic parameters, namely from the thermal transitions (Tm1–Tm8) to calorimetric enthalpy (ΔHcal) in proportion corresponded to the size of surgical interventions (duration of operation time, length of incision, surgical intraoperative stress, blood loss, etc.). This examination has shown that intraoperative stress during any surgical intervention affects the composition of plasma proteins, which should be always considered in the evaluation of DSC results in any surgical study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Risk of operation depends on the extent of the surgical intervention, the burden of anesthesia and the comorbidities. Definition of surgical stress, namely an operative intervention is major, or minor have been arisen for the first time in 1917 during a correspondence between Dr. Robert Earl and his patient, Mr. Lewis S. Pilcher, which is published in the American scientific literature [1]. The question was as follows: “Define what is meant by minor surgery and what is meant by major surgery?” The answer is still in place today, and it is invariably true: accordingly “I would say that major surgery includes all work requiring a general anesthetic; all operations which involve openings into the great cavities of the body; all operations in the course of which hazards of severe hemorrhage are possible; all conditions in which the life of the patient is at stake; all conditions which require for their relief manipulations, for the proper performance of which special anatomical knowledge and manipulative skill are essential.” If we are looking for it, surgical or anesthesiologic textbooks do not say more about this question today.
After the first definition, the greatest step was in this theme when the American Society of Anesthesiologists developed the ASA physical status classification system of the patients in 1940. Later, the score system was modified and broadened and before surgery patients’ fitness can be classified into six categories [2, 3]. But surgical risk and stress should not be mistaken with the ASA score. The latter is shown in Table 1.
Generally, in elective operation the risk rises parallel to the extent of surgical area, if the length of surgery is longer than 2 h, with the amount of intraoperative blood loss and with the decrease in body temperature that is measured during the operation. Moreover, surgical risk continues to increase much more if it is an acute intervention [4].
The development of a surgical system like to ASA began in Switzerland in 1992 [5]. In this paper, Clavien and co-workers proposed general principles to classify complications of surgery based on a therapy-oriented, four-level severity grading. Recently, this system contains three grades, where major and complex interventions mean same degree of severity [6, 7]. Today, preoperative planning includes determination of severity degree, predictable blood loss and operative time associated with surgery. Postoperative outcome of the patient can be predicted with the knowledge of these risks (Table 2).
The timeliness of the question indicates a paper published in 2019 in The Lancet Commission on Global Surgery which identified that 313 million surgical procedures are performed worldwide each year. Startling data that number of postoperative deaths accounts for 7.7% of all deaths globally, making it on the “Top 10 global causes of death” list to the third (!) greatest contributor to deaths, after ischemic heart disease and stroke [8]. Besides this huge number, there is no doubt that we still know little about the surgical risk and surgical stress also. The stress itself and the consequences of them are known as a qualitative complex system. Changes in surgical stress can be measured under different surgical intervention as quantitative values would be useful information for everyday clinical practice.
From the 1960s, differential scanning calorimetry (DSC) is originally a well-known thermo-analytical method in the physical sciences. From the end of the twentieth century, DSC examination is a validly efficient method not only for the demonstration of structural changes, but also in numerous in vitro and in vivo biological systems [9,10,11]. Many researchers’ works from the beginning of the twenty-first century revealed its potential for cancer disease diagnostics performed on human blood plasma [12,13,14,15].
These facts encouraged us to use DSC method in field of surgery also. The goal of this pilot study was to measure thermal changes of human blood plasma by DSC method on patients who underwent elective small or intermediate, or major surgical interventions. Moreover, beyond measurements received curves were unsealed and were deconvoluted to main plasma protein components as well.
Materials and methods
Patient selection
To this study, three different patient groups were established. Those who had pigmented nevi excision have joined to the minor surgical group (n = 8). They had low surgical risk; the operation time was under half an hour, while the predicted blood loss was under 200 mL. Patients in intermediated operation group underwent lumpectomy due to benign breast lesions (n = 9). The pure surgical time in this medium risk patient group was under 1 h, while blood loss was less than 1000 mL. In contrast, major operative group (n = 7) contained that persons, who underwent pancreas surgical intervention after median laparotomy. Only that patients were selected to this group whose operative time (surgery without anesthesia) was longer than 2 h, and during this high-risk surgical intervention their blood loss was more than 1000 mL. In every group, the predicted and final blood loss was near the same, and under intervention patients did not receive any blood component transfusion. Each operation was performed in the Surgical Clinic of Pécs University, Hungary. The protocols were approved by regional ethical committee of the University (27.06.2008/3220; 360.316-12736/2009).
Blood sample collection and preparation
Peripheral blood samples were collected from patients (n = 24) after their surgical treatments, and from healthy controls ranging from 22 to 62 years old (n = 5). Blood samples were collected into the Vacutainer tubes containing EDTA (1.5 mg mL−1 of blood) centrifuged at 1.600 g for 15 min at 4 °C to separate plasma fraction from cell components. Native plasmas were stored at − 80 °C until DSC measurement.
Calorimetric measurement
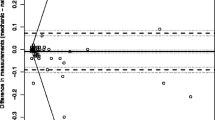
The thermal unfolding of the human plasma components was monitored by SETARAM Micro DSC-II calorimeter as previously described [16]. Briefly, all experiments were conducted between 0 and 100 °C. The heating rate was 0.3 K min−1 in all cases. Conventional Hastelloy batch vessels were used during the denaturation experiments with 850 µL sample volume in average. Reference sample was normal saline (0.9% NaCl). The sample and reference samples were equilibrated with a precision of ± 0.1 mg. The repeated scan of denatured sample was used as baseline reference, which was subtracted from the original DSC curve. We have plotted the CP heat flow (DSC-II is a heat flux instrument with hermetically closed vessels) in the function of temperature. Calorimetric enthalpy was calculated from the area under the heat flow curve by using two-point setting SETARAM peak integration.
Deconvolution of DSC thermal curve
Blood plasma is a complex protein mixture. Therefore, it contains from thermal point of view different “thermal domains” which can be assigned to the different compounds [17,18,19]. It means that a DSC scan can be decomposed into a sum of Gaussian curves such that their total area is the same as that of the experimental curve, within a reasonable error (< 1%). To have the best fitting, we applied more than five curves, but some contribution was less than the error of enthalpy determination, so they cannot influence our final interpretation of data.
Statistical analysis
All results are given in mean values ± standard error of the mean (SEM). Data were analyzed with one-way ANOVA. The level of significance was set at p < 0.05.
Results
Previous recorded DSC plasma profile from healthy individuals contained 5 well-resolved transitions at about 56 °C, 62 °C, 65 °C, 74 °C and 82 °C (17–19). Tm1 transition can be attributed mainly to fibrinogen, Tm2 to albumin, Tm3 to immunoglobulins and albumin minor tail, Tm4 to complement protein C3, IgA, IgG, and finally Tm5 to one part of IgG and transferrin. Although the DSC data from our study reveal heterogeneity in the curves, some common characteristics for the majority after surgery plasma profiles were observable. Generally, after any surgical intervention patients’ blood plasma curves were shifted more or less toward lower denaturation temperatures compared to healthy controls. Figure 1a–c shows measured calorimetric changes of blood plasma proteins as a cumulated curves (black lines, experimental). Thereafter measured main thermal curve (black line) deconvoluted usually was unfolded to 5–8 melting components (colored lines). The order of appearance of each component in case of five transition temperatures was green, blue, pink, dark yellow, and purple. The order in case of eight Tms was the follows: green, blue, pink, dark yellow, navy, purple, brown, and dark cyan.
Following minor surgery, the first transition temperature (fibrinogen) from deconvoluted patients curves remained on the healthy controls’ temperature (56 °C) value. While the second transition giving albumin’s melting point showed mild decrease, the third immunoglobulins melting temperature decreased from 65.3 to 64.1 °C. The decrease was more significant for Tm4, but Tm5 slightly increased (Fig. 1a; Table 3). After intermediate surgical intervention, blood plasma melting temperatures showed a downward trend compared to both samples from healthy volunteers, and from patients after minor surgery. There was only one exception, Tm3, where transition temperature showed mild increase. The most dominant changes occurred in plasma after major surgery. Surprisingly, during deconvolution of blood plasma cumulative DSC curve was separable to eight well-separated melting components. Accordingly, Tm1 was lower than ever before; this decrease was more than 10 °C (45 °C vs. 56 °C). The Tm7 was near to the healthy Tm4, while Tm8 was near to control Tm5 values. According to temperature range, the given melting temperatures between Tm2 and Tm6 were near similar which are in healthy Tm2 and Tm3.
The calorimetric enthalpy, as an indicator of overall thermal stability of the whole system, showed a mild decrease after minor surgery compared to control (1.29 J g−1 vs. 0.94 J g−1). According to our measurements, the enthalpy changed parallel and in proportional manner to the size of surgical intervention (1.11 J g−1; 1.45 J g−1).
Discussion
These results can be considered as novel because no other results describing blood plasma such changes with thermo-analytical method on patients who underwent different sizes of surgery. Several research groups have investigated blood plasma changes in patients who treated for cancer, inflammatory disease or other causes. But this is the first research that shows the extent of surgical invasiveness alone influences the change in plasma composition. Having regard to the lack of comparable articles, we assume that there are three reasons for the explanation of change. First, with an increase in surgical time patient gets more intravenous infusions, which means extra fluid administration will dilute blood plasma protein components. There may be visible a “purifier” picture of diluted plasma proteins, including any small proteins or peptides also. According to our hypothesis transition temperatures change not only numerically. There is no doubt that qualitative changes may also be responsible for the dramatic changes in melting temperatures after 2 h surgery. Other researchers explained these results with conformational changes or protein modifications during their calorimetric denaturation [20]. Third possible explanation is that specific interactions should be between small and most abundant proteins or other circulating molecules which are present in different diseases [21]. The obtained results suggest that mapping of human plasma proteins by DSC method and they introduce should be a possible novel and non-invasive diagnostic tool. Nevertheless, further studies are needed to prove our assumptions and for a reassuring interpretation of given results.
Despite the fact that the development of surgery has been going on for thousands of years, and modern surgery is more than 170 years old, it is still a question of what size of stress a patient has on surgery. In many cases, university textbooks or conventional blood tests do not give an exact answer. This article highlighted the significant difference in categorization of surgical procedures. The results obtained are extremely different, but this paper focused on the problem and on the changes causing surgical intervention which should be taken into account when evaluating the thermoanalytical changes measured during each surgical procedure.
References
Earl R. Definition of major and minor surgery: a question and an answer. Ann Surg. 1917;65:799.
Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–4.
Fitz-Henry J. The ASA classification and peri-operative risk. Ann R Coll Surg Engl. 2011;93:185–7.
WHO Guidelines for Safe Surgery. Section II. In: Ten essential objectives for safe surgery: review of the evidence and recommendations. 2009. p. 9–96.
Clavien P, Sanabria J, Strasberg S. Proposed classification of complication of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–12.
Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32:533–6.
Nepogodiev D, Martin J, Biccard B, Makupe A, Bhangu A, National Institute for Health Research Global Health Research Unit on Global Surgery. Global burden of postoperative death. Lancet. 2019;393:401.
Lőrinczy D, Könczöl F, Gaszner B, Belágyi J. Structural stability of actin filaments as studied by DSC and EPR. Thermochim Acta. 1998;322:95–100.
Schäffer B, Lőrinczy D, Szakály S. DSC and EPR investigation of the effect of fat crystallization on the consistency of butter. J Therm Anal. 1996;47:515–24.
Ferencz A, Nedvig K, Lőrinczy D. DSC examination of the intestinal tissue following ischemic injuries. In: Lőrinczy D, editor. Thermal analysis in medical application. Budapest: Akadémiai Kiadó; 2011. p. 255–69.
Garbett NC, Mekmaysy CS, DeLeeuw L, Chaires JB. Clinical application of plasma thermograms. Utility, practical approaches and considerations. Methods. 2015;76:41–50.
Ferencz A, Fekecs T, Lőrinczy D. Differential scanning calorimetry as a new method to monitor human plasma in melanoma patients with regional limph node or distal metastases. In: Yaguang X, editor. Skin cancer book. Rijeka: InTech; 2011. p. 141–53.
Medhi M, Zapf I, Fekecs T, Nedvig K, Lőrinczy D, Ferencz A. Influence of oxidative injury and monitoring of blood plasma by DSC on patients with psoriasis. J Therm Anal Calorim. 2016;123:2037–43.
Bűcs G, Nőt LG, Dandé Á, Wiegand N, Lőrinczy D. Detection of joint capsule changes by differential scanning calorimetry (DSC) in different types of hip disorders to evaluate surgical techniques (a preliminary report). J Therm Anal Calorim. 2017;130:1293–6.
Ferencz A, Lőrinczy D. DSC measurements of blood plasma on patients with chronic pancreatitis and operable and inoperable pancreatic adenocarcinoma. J Therm Anal Calorim. 2017;127:1187–92.
Garbett NC, Mekmaysy C, Helm CV, Jenson AB, Chaires JB. Differential scanning calorimetry of blood plasma for clinical diagnosis and monitoring. Exp Mol Pathol. 2009;86:186–91.
Todinova S, Krumova S, Kurtev P, Dimitrov V, Djongov L, Dudunkov Z, Taneva SG. Calorimetry-based profiling of blood plasma from colorectal cancer patients. Biochim Biophys Acta. 2012;1820:1879–85.
Michnik A, Drzazga Z. Thermal denaturation of mixtures of human serum proteins: DSC study. J Therm Anal Calorim. 2010;101:513–8.
Garbett NC, Miller JJ, Jenson AB, Miller DM, Chaires JB. Interrogation of the plasma proteome with differential scanning calorimetry. Clin Chem. 2007;53:2012–4.
Zhou M, Lucas DA, Chan KC, Issaq HJ, Petricoin EF, Liotta LA, Veenstra TD, Conrads TP. An investigation into the human serum “interactome”. Electrophoresis. 2004;25:1289–98.
Acknowledgements
Open access funding provided by Semmelweis University (SE). This research was funded by Grant OTKA (C272 for D.L. and PD77474 for A.F.), and PTE ÁOK Research Grant (114-603/2009 for A.F.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferencz, A., Lőrinczy, D. Surgical stress detection in human blood plasma by DSC. J Therm Anal Calorim 142, 783–788 (2020). https://doi.org/10.1007/s10973-020-09518-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-020-09518-w