Abstract
In recent years, considerable attention focuses on making sustained release dosage forms also containing solid dispersions. The objective of this study is evaluation of imatinib base (IMA) solid dispersion physicochemical properties which can be useful to controlled release solid dosage formation. The solid dispersions were obtained by kneading method, containing of 10–90% w/w Pluronic F127 (PLU). Drug dissolution test was determined by rotating-disc system method in 0.1 M hydrochloric acid (pH 1.2) and phosphate buffer (pH 6.8). XRD, DSC, FTIR, and SEM observations were performed to evaluate the physical characteristics of solid dispersions. These studies showed that there was no chemical interaction of the IMA with PLU in the solid state and revealed that IMA and PLU form a simple eutectic phase diagram. Our research has shown that the dynamics of the release of imatinib base from solid dispersions with Pluronic F127 depends on the pH of dissolution medium. At pH 1.2, the presence of polymer in solid dispersion causes delaying of drug release due to formation a viscous gel layer, whereas at pH 6.8 significant enhancement of the drug dissolution rate from solid dispersions has been observed compared to pure IMA. The highest improvement was observed in solid dispersions containing 20 and 30% w/w polymer. The present investigation confirmed that the hydrophilic polymer Pluronic F127 could be applied as a suitable matrix to design modified release formulations of imatinib base.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
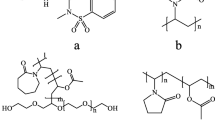
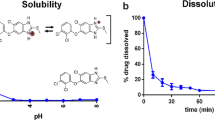
The rate or extent of dissolution of drug from any solid dosage form is a rate-limiting step in the poor process of water-soluble drug absorption. Imatinib N-(4-methyl-3-((4-(pyridin-3-yl)pyrimidin-2-yl)amino)phenyl)-4-((4methylpiperazin-1-yl)methyl)benzamide (see Fig. 1) is a first-generation antitumor protein tyrosine kinase inhibitor and antileucemia cytostatic agent, which shows low, pH-dependent solubility. In aqueous media, imatinib base is characterized by poor solubility (0.01 mg mL−1) [1]. However, the mesylate salt of imatinib, which exists as a polymorph with two principal forms, [2, 3] is very soluble in media at pH values ≤5.5, but in neutral and alkaline aqueous buffers is poorly soluble or insoluble [4]. Therefore, imatinib mesylate belongs to Class 2 of Biopharmaceutical Classification System (BCS) with a solubility of 1 mg mL−1 determined at pH 7.4 [4]. After oral administration, especially of the conventional dosage forms, imatinib mesylate is not absorbed to the same extent, when it passes the upper small intestine, where its absorption is the maximum. Recommended dosage form for this substance should be form, which continuously releases the drug in the stomach before reached its the absorption window, thus ensuring optimal bioavailability of substance [5]. Hence there is a great interest in the development of new imatinib formulations, which could maintain optimum therapeutic plasma drug concentrations to avoid inter-patient variability and side effects. The usual oral recommended dose of imatinib for humans is between 50 and about 1600 mg day−1, in two or four doses. The formulations provide rapid dissolution of the active ingredient that in turn results in its rapid increase in blood plasma levels above the therapeutic steady state levels, immediately after administration followed by approaching a decrease in blood plasma levels up to subtherapeutic plasma levels after about 12 h following oral administration, thus requiring additional dosing [5]. Vinod et al. [5] obtained gastroretentive floating tablets, which showed good floatation during the period of imatinib mesylate release. Ravindran et al. have developed single-unit-controlled release imatinib mesylate oral dosage form which can retain the drug in the stomach for prolonged duration by mucoadhesive nature of the dosage form and to achieve therapeutic levels over an extended period of 12 h for the treatment of chronic myelogenous leucemia and gastrointestinal stromal tumour [6].
Solid dispersions (SDs) are generally used in order to improve the dissolution rate and the bioavailability of poorly soluble active pharmaceutical ingredients (APIs). In the literature can be found also report on the application of solid dispersions for the controlled release of drugs [7]. Patil et al. [8] have used the SDs containing a polymer blend, such as hydroxypropylcellulose and ethylcellulose that allowed possible to precisely control the rate of release of water-soluble drug. The improvement of drug dissolution profile from solid dispersions is observed, when the ratio of carriers in solid dispersions increased, and the drug was dispersed better and the drug crystallinity decreased. In these solid dispersions, the main release mechanism is drug-controlled release. Other researchers observed the decrease in drug dissolution rate when the ratio of carrier in solid dispersions was increased. This can be explained by the carrier-controlled mechanism in which the gel or concentrated carrier layer is formed and acts as a diffusion barrier to delay drug release. Therefore, it is important identify of drug release mechanism from solid dispersions. In carrier-controlled release solid dispersions (CRSD), the carrier properties such as solubility, viscosity, gel-forming ability and the ratio of drug to carrier are the key factors affecting the drug dissolution profile. In CRSD, depending on the characteristic of polymers and the miscibility of the drug and carrier there are two main mechanisms by which the drug can be released from the system: diffusion and erosion. If the drugs and polymers are well dispersed in internal structure of solid dispersions, the diffusion of drugs through the matrix will be the main mechanism. If the drugs and carriers exist in separated particles, the solid dispersion erosion may become the main mechanism for drug release. In some solid dispersions, both of these mechanisms can control the drug release at the same time [9].
In this study, imatinib base solid dispersions were formulated with Pluronic F127 by kneading method, and next XRD, DSC, FTIR, and SEM observations were performed. In vitro dissolution study was conducted in media at pH 1.2 and pH 6.8. Pluronic F127 has been recently widely used as wetting and solubilizing agents as well as surface adsorption excipients. They are employed to enhance the solubility, dissolution, and bioavailability of many hydrophobic drugs as hydrophilic carrier for its excellent surfactant properties and oral safety [10]. Based on the results dissolution studies of solid dispersions of atorvastatin calcium with poloxamer 407 conducted in phosphate buffer (pH 7.4) and water, Nasrin et al. [11] confirm that polymer might be efficient in formulating both immediate release and sustained release oral dosage form of drug with improved dissolution. The higher ratios of poloxamer 407 in solid dispersions allow to sustain the release rate of drug, caused tendency to gel of polymer in higher proportion at elevated temperature [11].
Experimental
Materials
Imatinib base (99% purity) synthesized by Silesian Catalysts (Poland), Pluronic F127 were supplied by Sigma-Aldrich (USA). Concentrated volumetric solution hydrochloric acid 0.1 mol L−1 was purchased from Avantor Performance Materials Poland SA (Poland). Ethanol HPLC grade were obtained from Avantor Performance Materials Poland SA (Poland), acetonitrile HPLC grade were obtained from JT Baker (USA), and potassium dihydrogen phosphate and 0.05% tetrabutylammonium hydrogen sulphate 98% from Acros Organics (USA).
Preparation of solid dispersion
Suitable amounts of IMA and PLU were weighed and mixed in agate mortar with addition of sufficient volume of ethanol to get the consistency like a slurry. The solvent was then completely evaporated at 40–45 °C with continuous stirring to obtain dry mass. Afterwards dry mass was triturated in an agate mortar and sieved through a sieve with a mesh size of 315 μm. The pulverized solid dispersions were stored in a desiccator at room temperature until use. The mass ratios of the IMA/PLU mixtures were: 90/10, 80/20, 70/30, 60/30, 50/50, 40/60, 30/70, 20/80, and 10/90%, respectively.
Drug content
Equivalent weight of solid dispersions containing 10 mg of imatinib were weighed accurately and dissolved in 50 mL of acetonitrile. The solution was filtered and IMA content was analysed.
Differential scanning calorimetry (DSC)
The heat flux type calorimeter DSC 214 Polyma (Netzsch, Germany) was used to obtain DSC curves of pure components and solid dispersions. The measurements and data analysis were carried out using Proteus software (Netzsch, Germany). Calibration of DSC instrument was performed using the solid–solid transition temperature of adamantane (-64.5 °C), and melting points of indium (156.6 °C), tin (231.9 °C), bismuth (271.4 °C), and zinc (419.5 °C) as a standards [12, 13]. About 4–5 mg of each sample was placed and sealed in 40-µL standard aluminium crucible with a pierced lid. The same type of empty crucible was used as a reference.
The DSC scans of all prepared samples were run in triplicate using dry nitrogen (99.999% purity) as a purge gas at a flow rate of 50 cm3 min−1. The samples were heated in the temperature range of 25–250 °C at a heating rate of 10 °C min−1.
Powder X-ray diffraction analysis (XRPD)
Powder X-ray diffraction patterns were recorded on a D2 Phaser powder diffractometer (Bruker, Germany) with CuKα radiation with LynxEye detector. The degree of diffractions was measured at 15° min−1 between 5° and 60° (2θ) with an accuracy of 0.02° throughout the measurement range, at 0.5 s step−1.
Fourier transform infrared (FTIR) spectroscopy
FTIR spectra were registered by using Nicolet 380 spectrometer (Thermo Scientific). Samples were mixed with potassium bromide (KBr) and compressed into a disc using the Specac hydraulic press (Mettler Toledo, Switzerland) before scanning from 4000 to 450 cm−1.
Scanning electron microscopy (SEM)
The samples were covered with gold and palladium (60:40; sputter current 40 mA; sputter time 50 s) using a Quorum machine (Quorum International, USA) and examined under a Zeiss EVO MA25 scanning electron microscope.
Intrinsic dissolution rate (IDR) studies
Dissolution tests were carried out under sink conditions in the two different media: 1000 mL of 0.1 M HCL and 1000 mL of phosphate buffer pH 6.8 at 37 ± 0.5 °C and rotational speeds of 50 rpm. The dissolution system was fitted with SR8-PLUS (Hanson) and 7-channel peristaltic pump. IMA (100.0 mg) or an equivalent amount of solid dispersion discs were prepared compressing powder in hydraulic press (Specac, Mettler Toledo) for 1 min under 2 t compression force, using a 13-mm punch. Samples were withdrawn at appropriate time intervals. Quantitative determination for IMA was performed with HPLC system (System GOLD 126, Beckman Coulter) with a UV–VIS detector. The analysis was conducted using Zorbax SB-C8 column (250 × 4.6 mm, 5 μm, Agilent). Analysis was performed by gradient elution with mixture of acetonitrile and 0,02 M potassium dihydrogen phosphate (KH2PO4) with 0.05% tetrabutylammonium hydrogen sulphate solution with a steady flow rate of 1 mL min−1. Substances eluted from the column were identified by UV–visible detector at 236 nm. External standards of IMA were used to obtain calibration curves. Linear calibration curves for IMA in 0.1 M HCl solution and in phosphate buffer pH 6.8 were obtained in the range of 2.5–120 µg mL−1 (linearity r 2 = 0.999) and 0.4–60 µg mL−1 (linearity r 2 = 0.999), respectively.
Results and discussion
Drug content
The imatinib base content of the formulations was found to be in the range of 98.22–103.28% of the declared amount. Table 1 lists results from studies of drug content in solid dispersions.
Differential scanning calorimetry study
Figure 2 presents heating curves for all the samples performed at a rate of 10 °C min−1.
Melting points of the pure IMA and pure PLU were found to be 209.7 and 55.8 °C, respectively. All of the DSC curves recorded for solid dispersions show two endothermal effects, first with the onset at the invariant temperature (onset at 52.5 °C) and second corresponding to the completely melting of appropriate sample. It indicates the formation of eutectic mixture between IMA and PLU. Figure 3 shows the phase diagram of IMA/PLU constructed on the basis of the DSC results. The eutectic point composition was determined by Tamman’s triangle construction [14]. Figure 4 presents the values of the eutectic melting enthalpy ΔH (J g−1) for a given dispersions versus mass ratio of IMA. The values of the eutectic melting enthalpy ΔH (Fig. 4, filled circles) go to zero for a composition corresponding to pure IMA, indicating no formation of a terminal solid solution. The characteristic overlapping of eutectic and liquidus events into a single peak can be observed on the DSC curves near the eutectic point. For this reason, the eutectic composition was determined by plotting the non-eutectic melting enthalpy of IMA (Fig. 4, open circles) as a function of the mass ratio of IMA and extrapolating the fitted line to value of zero. The parameters of the eutectic point have been established as follows:
-
Eutectic composition: mass fraction of IMA 2.3%, mass fraction of PLU 97.7%;
-
Eutectic temperature: 52.5 °C.
X-ray diffraction
The X-ray diffraction patterns of IMA, PLU, and solid dispersions are presented in Fig. 5. This crystalline imatinib base were characterized pattern with peaks at about 5.88, 9.34, 11.85, 12.65, 13.89, 14.96, 15.71, 17.75, 18.48, 19.59, 20.75, 23.98, 24.95, and 28.11 (2θ). The X-ray diffractograms of pure PLU showed the distinct peaks at 18.89° band 23.09°. These data reveal that the typical drug crystalline peaks were still detectable (with reduced intensity and less number) in the solid dispersion, suggesting a simple mixing of drugs and carriers.
Fourier transform infrared spectroscopy
Figure 6 presents FTIR spectra of Pluronic F127, imatinib and its solid dispersions. The spectra of pure drug shows characteristic peak at 3279 cm−1, at 2795 cm−1, at 1646 cm−1, at 1575 cm−1, at 1531 cm−1, at 1453 cm−1, at 1291 cm−1, at 1165 cm−1, at 1110 cm−1, at 926 cm−1, at 858 cm−1, at 796 cm−1, at 703 cm−1, at 647 cm−1 [15]. FTIR spectrum of poloxamer 407 is characterized by principal absorption peaks at 2882 cm−1 (C–H stretch aliphatic), 1343 cm−1 (in-plane O–H bend) and 1100 cm−1 (C–O stretch), which were consistent in all binary systems with the drug. This indicates the absence of drug–excipient interactions, as all the specific peaks of drug were present in the solid dispersion.
Scanning electron microscopy (SEM)
SEM photomicrographs (in 300× magnifications) of pure IMA, PLU, and obtained solid dispersions are shown in Fig. 7. From the photomicrograph of pure drug IMA, it is clear that the drug was present as irregular shaped crystals, whereas poloxamer 407 was characterized by spherical particles with very smooth surface. The SEM photomicrographs of obtained solid dispersions showed crystalline homogeneous mixture of drug particles dispersed in the polymer carrier. Microcrystalline character of drug particles has demonstrated also by method of XRPD.
Intrinsic dissolution rate (IDR) studies
IDR determination is used inter alia to investigation of mass transfer phenomena during the dissolution process, determination of pH–dissolution rate profiles, effect of pH on the solubilization of poorly soluble drugs, and understanding of the relationship between the dissolution rate and crystalline form [16]. Intrinsic dissolution rate is defined as the dissolution rate of a pure compound under the condition of constant surface area. IDR was determined according to the equation:
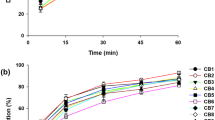
where \(\frac{{d_{\text{m}} }}{{d_{\text{t}} }}\) is the maximum slope in the dissolution curve evaluated at the start of the dissolution process, A is the area of the drug disc (cm2), m is the mass (mg), t is the time (min). The determination of the dissolution rate in comparison with solubility studies does not depend on saturation concentration of API in the medium; it is less sensitive to the errors related to possible phase changes within the formulation. IDR at pH 1.2 of pure IMA, its solid dispersions with PLU, and the linear relationship between the amount of the dissolved drug and time are given in Table 2. Results suggest that the dissolution rate of IMA from solid dispersions containing PLU is lower than that of the pure substance. After 45 min of testing, depending on the formulation composition, the IDR decreased by half for the 90/10 IMA/PLU composition and by more than 20-fold for the 10/90 IMA/PLU % w/w formulations. These results correspond to a dissolved amount of 47.25 and 3.43% of the total active pharmaceutical ingredient (API) for the 90/10 and 10/90 IMA/PLU % w/w formulations, respectively. In this time, 86.27% of the pure IMA was dissolved. As the polymer concentration increases, the dissolution decreases due to water penetration, the polymer relaxation, and the forming a viscous gel layer. This layer controls and retards the release of drug, and the effect depends on the polymer content in solid dispersion. Figure 8 shows the dissolution profiles of IMA from solid dispersions within 120 min. A dissolution profile plateau at pH 1.2 was observed after 55 min of dissolution tests for pure drug. This plateau corresponds to 100% of dissolved IMA.
Dissolution profiles of pure IMA, and its solid dispersions with PLU over a period of 120 min at phosphate buffer pH 6.8 are shown in Fig. 9. At this time, the pure IMA was not dissolved in buffer at pH 6.8, and means the amount of drug in the collected samples, was below detectable concentration by HPLC method. Solid dispersions of IMA with PLU significantly enhanced the dissolution rate of IMA within 120 min as compared to pure IMA. The highest improvement was observed in solid dispersions containing 20 and 30% w/w polymer.
Conclusions
In the literature, many studies reported for the preparation of controlled release system using solid dispersion technique, with application polymers: ethylcellulose and hydroxypropylmethylcellulose, poly(ethylene oxide)-carboxyvinyl polymer, Eudragit or Kollidon [17]. There are no data regarding the use of Pluronic F127 to create carrier-controlled release solid dispersions. Determination of physicochemical properties and behaviour of drug–polymer solid dispersion in different pH media allow an assessment of the possibility of their use in oral modified release dosage forms. Our research has shown that the dynamics of the release of imatinib base from solid dispersions with Pluronic F127 depends on the pH of dissolution medium. At pH 1.2, the presence of polymer in solid dispersion causes delaying of drug release due to formation a viscous gel layer, whereas at pH 6.8 significant enhancement of the drug dissolution rate from solid dispersions has been observed compared to pure IMA. The highest improvement was observed in solid dispersions containing 20 and 30% w/w polymer. Based on DSC results, it has been found that IMA and PLU form a simple eutectic system containing 2.3% w/w of IMA at the eutectic point. Establishing previously unknown IMA/PLU phase diagram can prove relevant for the formulation of oral modified release dosage forms. The present investigation confirmed that the hydrophilic polymer Pluronic F127 could be applied as a suitable matrix to design controlled release formulations of imatinib base. The carrier-controlled release solid dispersions can deliver an adequate amount of drug for an extended period of time and thus offer many advantages such as improved patient compliance due to reduced dosing frequency, decreased side effects, more constant or prolonged therapeutic effect for poorly water-soluble drugs.
References
Sweetman SC, editor. Martindale: the complete drug reference. 36th ed. London: The Pharmaceutical Press; 2009.
Bellur Atici E, Karlığa B. Quantitative determination of two polymorphic forms of imatinib mesylate in a drug substance and tablet formulation by X-ray powder diffraction, differential scanning calorimetry and attenuated total reflectance Fourier transform infrared spectroscopy. J Pharm Biomed Anal. 2015;114:330–40.
Mucha I, Baranowski P, Owczarek A, Gajda M, Pluta J, Górniak A, Niklewicz P, Karolewicz B. Thermal stability and decompositions kinetics under non-isothermal conditions of imatinib mesylate α form. J Pharm Biomed Anal. 2016;129:9–14.
Benet LZ, Broccatelli F, Oprea TI. BDDCS applied to over 900 drugs. AAPS J. 2011;13:519–47.
Vinod KR, Santosh V, Sandhya S, Otilia BJ, David B, Padmasri A. A comparative in vitro drug release prospective with two different polymers for the development of floating single unit dosage form of imatinib mesylate for chronic myelogenous leukemia. Ars Pharm. 2012;53:1–7.
Ravindran VK, Vasa S, Subadhra S, Banji D, Banji O, Rao YM. Comparative study of mucoadhesive polymers carbopol 974P and sodium carboxymethyl cellulose for single unit dosage of imatinib mesylate. Malays J Pharm Sci. 2012;1:61–77.
Giri TK, Kumar K, Alexander A, Ajazuddin Badwaik H, Tripathi DK. A novel and alternative approach to controlled release drug delivery system based on solid dispersion technique. Bull Fac Pharm (Cairo Univ). 2012;50:147–59.
Patil SA, Kuchekar BS, Chabukswar AR, Jagdale SC. Formulation and evaluation of extended-release solid dispersion of metformin hydrochloride. J Young Pharm. 2010;2:121–9.
Vo CL, Park C, Lee B. Current trends and future perspectives of solid dispersions containing poorly water-soluble drugs. Eur J Pharm Biopharm. 2013;85:799–813.
Wagh VT, Jagtap VA, Shaikh TJ, Nandedkar SY. Formulation and evaluation of glimepiride solid dispersion tablets for their solubility enhancement. J Adv Sci Res. 2012;3:36–41.
Nasrin F. Development and in vitro characterization of atorvastatin calcium Poloxamer 407 solid dispersions systems. IJPT. 2014;5:6151–64.
van Ekeren PJ, van Genderen ACG, van den Berg GJK. Redetermination of the thermodynamic properties of the solid–solid transition of adamantane by adiabatic calorimetry to investigate the suitability as a reference material for low-temperature DSC-calibration. Thermochim Acta. 2006;446:33–5.
Della Gatta G, Richardson MJ, Sarge SM, Stolen S. Standards, calibration and guidelines in microcalorimetry. Part 2. Calibration standards for differential scanning calorimetry (IUPAC technical report). Pure Appl Chem. 2006;78:1455–76.
Rycerz L. Practical remarks concerning phase diagrams determination on the basis of differential scanning calorimetry measurements. J Therm Anal Calorim. 2013;113:231–8.
Kompella A, Adibhatala KSBR, Rachakonda S, Nannapeneni VCh. Process for the preparation of highly pure crystalline imatinib base. U.S. Patent US 13/634,725.
Yu LX, Carlin AS, Amidon GL, Hussain AS. Feasibility studies of utilizing disk intrinsic dissolution rate to classify drugs. Int J Pharm. 2004;270:221–7.
Kim HJ, Lee SH, Lim EA, Kim JS. Formulation optimization of solid dispersion of mosapride hydrochloride. Arch Pharm Sci Res. 2011;34:1467–75.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Karolewicz, B., Gajda, M., Górniak, A. et al. Pluronic F127 as a suitable carrier for preparing the imatinib base solid dispersions and its potential in development of a modified release dosage forms. J Therm Anal Calorim 130, 383–390 (2017). https://doi.org/10.1007/s10973-017-6139-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-017-6139-1