Abstract
The radiosynthesis of pharmaceutical grade [68Ga]Ga-NODAGA-Lys40-Exendin-4 was accomplished in a fixed tubing-based module, EZ Modular-Lab Standard. Purification of the product via hydrophilic-lipophilic balance cartridge, yielded satisfactory results with radiochemical purity > 98%. The decay-corrected radiochemical yield (RCY) with 50 µg of Exendin-4[Lys40(NODAGA)] was (78.7 ± 0.8)%, which, by far, to the best of our knowledge, is the highest RCY reported till date, using an automated synthesizer. The quality control parameters were in accordance with that of gallium (68Ga) Edotreotide® Injections, featuring in the European Pharmacopoeia. Pre-clinical dosimetry studies in animal models, with co-administration of kidney protectant, demonstrates promising potential of the product towards clinical translation to insulinoma patients.
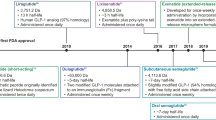
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peptide receptor radionuclide therapy (PRRT) using [177Lu]Lu-DOTATATE is not a viable option for treatment of pancreatic neuroendocrine tumors (PNET) or insulinomas. This is because of the insufficient concentration of two different somatostatin receptors (SSTR2 and SSTR5) on these types of cancer [1]. Typically in insulinomas, the density of overexpressed glucagon-like peptide-1 receptors (GLP1) is quite high. Hence targeting these overexpressed GLP1 with a suitable β or α emitting radionuclide tagged to a suitable GLP1 analogue ligand, was found to be a feasible treatment option for PNET [2,3,4,5]. Accurate planning for radionuclide therapy of insulinomas could be possible only after precise detection of these overexpressed GLP1 receptors. The precise detection of overexpressed GLP1 receptors was possible after tagging GLP1 analogues with suitable short-lived radioisotopes. For this purpose, GLP1 analogues after radiolabeling with gallium-68 or fluorine-18 were found to be an excellent tool for accurate and precise detection and also staging of insulinomas [6]. The commonly used analogues of GLP1 with ~ 50—55% similarity in amino acid sequence were found to be Exendin-4 and Exendin-3 [7]. Gallium-68 labeled Exendin-4 after coupling to various chelators namely NODAGA, DOTA, DO3A etc. was found to be an excellent diagnostic agent for detection of insulinomas [8,9,10].
Several studies have been reported for clinical dose preparation of [68Ga]Ga-Exendin-4 and [68Ga]Ga-Exendin-3 in recent times. The formulations were normally carried out (i) manually, under aseptic conditions [11, 12] (ii) semi-automated method [13] and (iii) fully-automated method [14,15,16]. Among these options, the fully automated radiochemical synthesis has always been a preferred choice for clinical dose preparation of [68Ga]Ga-Exendin-4, with respect to radiation protection, current good manufacturing practices (cGMP) and good laboratory practices (GLP), in a hospital radiopharmacy setting [14]. Till date, very few reports are available on the automated radiochemical synthesis of [68Ga]Ga-Exendin-4, due to the complexity in the solid phase extraction (SPE)-based purification of the final product. The SPE based purification is a process involving retention of both the radiolabeled product and the impurities in the SPE column. For effecting the separation of the radiolabeled impurities from the desired product, the SPE column needs to be eluted with suitable solvent having desirable polarity, prior to elution of the product. Also to increase the RCY of the final product, the retained [68Ga]Ga-Exendin-4 in the SPE column has to be eluted completely, which again can be facilitated by suitable solvent having appropriate polarity. This can be effected by the disruption of the weak Van der Waals forces existing between SPE sorbent and [68Ga]Ga-Exendin-4 [17, 18]. Moreover, none of the studies has reported the decay corrected (dc) or non- decay corrected (ndc) RCY more than 60% while using an automated synthesizer [9, 10].
The clinical dose preparation of [68Ga]Ga-Exendin-4, using cassette based automated synthesis modules namely Modular PharmLab, Modular-Lab PharmTracer and Scinotmics GRP® module has been reported [8,9,10, 13]. Basically the “fluid path” of these modules involved use of disposable cassette-based technique. Therefore, it has the advantages of (i) easy handling, (ii) no cleaning and sanitization process prior to radiolabeling (iii) better microbiological safety (iv) no cross-contamination and (iv) better cGMP and GLP compliance [15, 16]. Inspite of all these advantages of cassette based module (Modular Pharmlab, Modular-Lab PharmTracer and Scinotmics GRP®) used in clinical dose preparation of [68Ga]Ga-Exendin-4 over fixed tubing-based module (Modular-Lab Standard), the studies till date could achieve the dc or ndc RCY less than 60% [8,9,10].
The present attempt was focused on developing a fully automated radiolabeling of Exendin-4[Lys40(NODAGA)] with [68Ga]GaCl3 (sourced from a 68Ge/68Ga generator), using the existing fixed tubing-based or non-cassette based automated synthesizer (Modular-Lab Standard). The clinical dose formulation of [68Ga]Ga-Exendin-4 was carried out in Modular-Lab Standard after the radiosynthesis of [68Ga]Ga-DOTATATE and [68Ga]Ga-PSMA-11, using the same module on the same day. Modifications in the Modular-Lab Standard were carried out to facilitate the daily routine automated production of [68Ga]Ga-Exendin-4 with consistent ndc RCY and RCP of (60.9 ± 0.2)% and (98.5 ± 0.6)% respectively. Radiochemical reaction and purification conditions were modified to facilitate the automated production of [68Ga]Ga-Exendin-4, in the modified Modular-Lab Standard.
To the best of our knowledge, the automated radiosynthesis of [68Ga]Ga-Exendin-4 has not yet been reported, using any modular fixed tubing-based or non-cassette based commercial system after the necessary modification at the user end. Thus the present work reported herein, on the automated radiosynthesis of [68Ga]Ga-Exendin-4 in Modular-Lab Standard, which is routinely used for radiosynthesis of [68Ga]Ga-DOTATATE and [68Ga]Ga-PSMA-11 in our centre, with highest dc RCY of (78.7 ± 0.8)%, constitutes the first of its kind. The quality of the [68Ga]Ga-Exendin-4 thus synthesized was at par with of gallium (68Ga) Edotreotide® injection ([68Ga]Ga-DOTATOC), included in the European Pharmacopoeia. In-vitro and in-vivo pharmacokinetic studies were carried out in xenografted SCID mice for evaluating the diagnostic efficacy of the [68Ga]Ga-Exendin-4, and also providing preclinical evidence towards its clinical translation in human patients. Preclinical dosimetry was carried out to estimate dose to the patient, on administration of the product. The absorbed dose to organs and mean total body effective dose per unit activity administration (dose coefficient, mSv MBq−1) were estimated from biodistribution data of SCID mice without tumor xenografts. Dose extrapolation to humans was done by mass scaling of percentage injected activity in mice organs to reference adult male model (ICRP-89). The methodology adopted for dose estimations is MIRD (medical internal radiation dose) schema with OLINDA/EXM 2.0 software [19,20,21,22].
Materials and methods
Reagents and apparatus
Exendin-4[Lys40(NODAGA)] was purchased from Peptide Specialty Laboratories, Germany. Strata SCX (particle size: 54 µm, pore size: 73Ao) and plus HLB (sorbent weight: 225 mg, particle size: 60 µm, pore size: 80Ao) SPE cartridges for preconcentration and purification were purchased from Phenomenex, USA and Waters, USA, respectively. 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES, BioXtra® grade), L-Ascorbic acid (BioXtra® grade), Tween 80, sodium chloride (NaCl, BioXtra® grade) Hydrochloric acid (Suprapur grade, 30%) Ethanol (Emsure, Merck) and ethylenediaminetetraacetic acid (EDTA, 99.995% trace metal basis) were purchased from Merck, Germany. Hydrophilic PES membrane filters (0.20 μm) were purchased from Sartorius Stedim, Germany. The ultrapure water (UPW, Trace SELECT) was from Fluka, Switzerland was used for the preparation of various reagents required for radiochemical synthesis.
Gallium-68 in the form of [68Ga]GaCl3 was sourced from the commercial 68Ge/68Ga generator (ITM AG, Germany) using 0.05N HCl generator eluent. All radiochemical syntheses were carried out using Eckert and Ziegler Modular-Lab Standard automated radiochemistry module (Germany). Analytical radio high performance liquid chromatography (radio-HPLC) was performed using HPLC system equipped with DAD UV and radioactive detectors [NaI(Tl)], connected in series, from Knauer, Germany and Elysia Raytest, Belgium. Radio thin layer chromatography (radio-TLC) was performed using NaI(Tl) radioactive detector from Bioscan, USA. Radionuclide purity (RNP) was determined by recording gamma ray usinghigh-purity germanium (HPGe) detector (Baltic Scientific Instruments, Russia), coupled to 64 k multi-channel analyzer (MCA) (ITECH instruments, France). Peptide {Exendin-4[Lys40(NODAGA)]} content as chemical impurities in the final product was quantified by Microvolume Spectrophotometer (Denovix Inc, USA). Gas chromatography was carried out in Chemito 7610 GC instrument from USA equipped with split/splitless injector inlet, flame ionization and thermal conductivity detector using helium as carrier gas. The HEPES content in the final product was estimated using TLC plate (silica gel 60Ao, F254, Merck, Germany) after incubating in Iodine vapor chamber. Apart from conventional estimation of HEPES, we have carried out the quantification of HEPES in the final product by Microvolume Spectrophotometer (Denovix Inc, USA). Endotoxin limit was quantified by gel-clot BET assay method using LAL reagent from Charles River Laboratories Inc, USA, while the sterility test was performed by direct inoculation method using soybean casein digest and fluid thioglycollate media from Himedia, India. Rat insulinoma cell line INS-1 (832/13) with overexpressed GLP1 receptor was used for the in-vitro cell binding studies and also used for developing tumor xenografts in female SCID mice for in-vivo distribution studies. PET/CT imaging of tumor xenografted SCID mice was carried out using Gemini Digital PET/CT scanner from Philips N.V, Netherlands.
Preparation of reagents for radiochemical synthesis
-
a)
0.05 M HCl was prepared by aseptically mixing 530 µL of 30% HCl (Suprapure® grade, purity: ≥ 99.99% trace metal basis) in 99.47 mL of ultrapure water and filtered through 0.22 µm sterile PES membrane syringe filter.
-
b)
Acidified NaCl (0.24 M HCl in 5 M NaCl, pH: ⁓ 2.0) was prepared by mixing 250 µL of 30% HCl (Suprapur® grade, purity: ≥ 99.99% trace metal basis) in 10 mL of 5 M NaCl (BioXtra grade, purity: ≥ 99.5%) and filtered through 0.22 µm sterile PES membrane syringe filter.
-
c)
Stock solution of Exendin-4[Lys40(NODAGA)] was prepared aseptically by dissolving 1 mg lyophilized powder in 1 mL of ultrapure water and aliquoted in volume of 75 µL and stored at − 20 °C.
Preconditioning of plus HLB Sep-Pak® cartridges
Plus HLB cartridge was conditioned with 1 mL of ultrapure ethanol followed by 1 mL of ultrapure water, and the cartridge was dried with 10 mL of air prior to pre-equilibration. Further, plus HLB cartridge was pre-equilibrated with 1 mL of acidified HEPES buffer (0.1 M HCl/2.5 M HEPES buffer in 8/1 v/v).
Automated radiochemical synthesis of [68Ga]Ga-Exendin-4: EZ Modular-Lab Standard
Eckert and Ziegler Modular-Lab Standard radiochemistry module with modification was used for radiochemical synthesis of [68Ga]Ga-Exendin-4 is as shown in Fig. 1a. Envisaging the present strategy, provision for an extra solvent container (6th) was made in the EZ Modular-Lab Standard, as a part of the modification carried out in the module. Also modification in the time list for radiolabeling sequence were programmed using graphical user interface (GUI) software to facilitate the sequential elution of various reagents from six different reservoirs for automated radiochemical synthesis and purification of [68Ga]Ga-Exendin-4 in EZ Modular-Lab Standard. The radiochemical synthesis protocol for radiolabeling Exendin-4[Lys40(NODAGA)] with [68Ga]GaCl3 was modified and depicted in Table 1. Step wise modification in the radiochemical synthesis process of [68Ga]Ga-Exendin-4 from that of [68Ga]Ga-DOTATATE using EZ Modular-Lab Standard has been described in Fig. 1b. The following workflow was applied in EZ Modular-Lab Standard for the production of [68Ga]Ga-Exendin-4.
Step 1 Elution and pre-concentration of [68Ga]GaCl3.
-
I.
[68Ga]Ga3+ (~ 1.11 GBq) in the form of [68Ga]GaCl3 was eluted from the 68Ge/68Ga generator with 4–5 mL of 0.05N HCl (Suprapur grade) and passed through Strata SCX (strong cation exchanger) column.
-
II.
In Strata SCX column, [68Ga]Ga3+ was trapped, while [68Ge]Ge3+ (if any) and other non radioactive metallic impurities were washed from the column and collected in the waste vial.
-
III.
Trapped [68Ga]Ga3+ in strata SCX column was pre-concentrated with 515 µL freshly prepared acidified NaCl (0.2N HCl in 5 M NaCl) and eluted in to reaction vessel.
Step 2 Radio complexation of Exendin-4[Lys40(NODAGA)] with pre-concentrated [68Ga]GaCl3.
-
a.
Pre-concentrated [68Ga]GaCl3 (515 µL, ~ 1.11 GBq) was mixed with 600 µL of 2.5 M HEPES buffer containing 50 µL of Exendin-4[Lys40(NODAGA)] (50 µg, 10.70 nmoles) and 116 µL of L-ascorbic acid (100 mg/mL or 0.57 M), in the reaction vessel. The concentration of radio-protectant (L-ascorbic acid) in the reaction mixture during radiolabeling was maintained at ~ 51 mM.
-
b.
The reaction mixture was incubated at 95 °C for 15 min at pH ~ 5.0 and thereafter cooled to room temperature (25 °C) by adding 1.0 mL UPW containing 0.4 mL of 20 mM ultrapure EDTA and 30 µL of 10% Tween 80. While the final concentration of EDTA in reaction mixture is ~ 3.0 mM, the concentration of Tween 80 in the reaction mixture was ~ 0.11%, thereby preventing the sticking of the radiolabeled Exendin-4[Lys40(NODAGA)] on the wall of the reaction vessel.
Step 3 Purification through Plus HLB Sep-Pak® Cartridge.
-
a.
The reaction mixture was loaded on to pre-equilibrated plus HLB cartridge. The eluate was sent to waste vial.
-
b.
The plus HLB cartridge was washed with 3 mL of acidified HEPES buffer (0.1 M HCl/2.5 M HEPES buffer, 8/1 v/v) to remove [68Ga]Ga-EDTA and then with 1.5 mL of UPW to remove tracers of residual acidified HEPES buffer.
-
c.
The purified [68Ga]Ga-Exendin-4 (~ 0.85 GBq) was eluted from HLB cartridge using 0.8 mL of Emsure grade 100% absolute ethanol through 0.20 μm PES membrane syringe filter into the final product vial. Post elution of product with 100% absolute ethanol, 5 mL of sterile pyrogen free UPW was passed through the HLB cartridge and 0.20 μm PES membrane filter into the final product vial containing sterile pyrogen free ultrapure water (6 mL), 10% NaCl (1.0 mL) and 0.57 M L-ascorbic acid (0.45 mL). The final concentration of L-ascorbic acid (radio-protectant) in the product vial was 20 mM.
Quality control of [68Ga]Ga-Exendin-4
The pH of the product was measured by observing the color change of narrow range pH strips after spotting 1–2 µL of the final product. The RCP were assessed by radio-TLC {silica gel, 60Ao, using two different solvent system namely (i) 0.1 M sodium citrate buffer, pH: 5.0, (ii) 0.1 M EDTA in 0.25 M CH3COONH4, pH: ~ 5.5and (iii) 1MCH3COONH4 (pH:3.5) /CH3OH: 1/1 (v/v)}. RCP was also ascertained by radio-HPLC using gradient mode (Solvent: 0.1% TFA in H2O and CH3CN, gradient method: 0–20 min 90% to 30% water, 20–21 min 30% to 0% water, 21—30 min 0% water and 30–35 min 0% to 90% water using Eurosphere C-18 Reversed phase column {Dimension: 300 mm (Length) × 4 mm (Diameter), Particle size: 5 µm} coupled with NaI(Tl) and UV detector (wavelength set at 280 nm) maintaining a flow rate of 1.0 mL/min. The ethanol levels in the final product were detected by gas chromatography using a standardized procedure, with helium as carrier gas and polyethylene glycol capillary column {Dimension: 25 m (L) × 0.32 mm (ID), Thickness: 0.5 µm}. The column was maintained at a temperature of 70 °C during the operation. The Tween 80 in the final product was estimated by developing TLC-SG F254 with a solution of water/acetonitrile (25/75 v/v) as mobile phase, the developed TLC plate was dried with hot air and exposed to iodine vapor for 4 min. The developed intensity of color was compared to that of TLC-SG F254 chromatogram with known concentration of tween 80 (1, 0.5, 0.25, 0.1 and 0.05%) [9, 23]. The EL was quantified by gel-clot BET assay method using lysate with sensitivity 0.125 EU/mL at 200 maximum valid dilution (MVD). Sterility test was carried out by direct inoculation method.
Quantification of peptide content in [68Ga]Ga-Exendin-4
The concentration of peptide {Exendin-4[Lys40(NODAGA)]} content in the final product was quantified by Bradford Assay at 595 nm using Microvolume Spectrophotometer with inbuilt Absorbance Colorometrics App. Exendin-4[Lys40(NODAGA)] solutions of known concentrations (50, 35, 17, 8, 4, 2 and 1 µg/mL) were prepared in a volume of 1.0 mL. The standard Exendin-4[Lys40(NODAGA)] solutions were prepared in a matrix containing ethanol (100%), UPW, NaCl (10%) and L-ascorbic acid (0.57 M). Each of the standard Exendin-4[Lys40(NODAGA)] solutions (20 µL of each standard) were incubated with Bradford reagent (80 µL) at room temperature (25 °C) for 5 min. Absorbance was measured for each of the concentrations at 595 nm wavelength. The known concentrations were plotted against the corresponding absorbance (595 nm) resulting in a standard curve. The linearity of the data (r2: 0.995–0.996) for Exendin-4[Lys40(NODAGA)] against the standard curve demonstrates that Beer’s law is obeyed over the concentration ranging from 50 to 1.0 µg/mL. The concentration of peptide in the samples of [68Ga]Ga-Exendin-4 was estimated from the standard curve.
Quantification of HEPES content in [68Ga]Ga-Exendin-4
The HEPES content in the final product was estimated by developing TLC chromatogram with a solution of water/acetonitrile (25/75 v/v) as mobile phase and incubating in Iodine chamber for 15 min [23, 24]. The HEPES quantification method as described in Pharmeuropa, does not quantify the exact concentration, rather it gives a limit. In our study, we had standardized a protocol to quantify the concentration of HEPES in the final product using microvolume spectrophotometer, which has not been reported till date. HEPES solutions of known concentrations (50, 40, 30, 20, 10, 5 and 2.5 µg/mL) were prepared in a volume of 1 mL. The standard HEPES solutions were prepared in a matrix containing ethanol (100%), UPW, NaCl (10%) and L-ascorbic acid (0.57 M). Absorbance was measured at 260 nm wavelength using Microvolume Spectrophotometer with inbuilt absorbance UV–Vis App. The known concentrations were plotted against the corresponding absorbance resulting in a standard curve. The linearity of the data (r2: 0.994–0.995) for HEPES against the standard curve demonstrates that Beer’s law is obeyed over the concentration ranging from 50 to 2.5 µg/mL. The concentration of HEPES in samples of [68Ga]Ga-Exendin-4 was estimated from the standard curve.
In-vitro stability studies of [68Ga]Ga-Exendin-4
In-vitro stability of the [68Ga]Ga-Exendin-4 was analyzed in saline as well as in human serum. In-vitro saline stability of the final product was assessed by incubating 800 µL of [68Ga]Ga-Exendin-4 in 2 mL of saline at room temperature (25 °C) for 2 h post-radiolabeling, and its stability was determined by radio-HPLC.
For the analysis of [68Ga]Ga-Exendin-4 stability in human serum, the product (150 µL) was incubated in 250 µL human blood serum (obtained from healthy volunteers) at 37 °C for 1 h [25, 26]. Post incubation, serum proteins were precipitated using 200 µL acetonitrile by centrifugation at 4000 g for 10 min, and serum samples were stored at 25 °C upto 1 h. The serum stability of [68Ga]Ga-Exendin-4 (RAC: 56.4 MBq/mL) on storage, at 25 °C was evaluated by radio-TLC. To quantify the activity remaining in the precipitated protein, the protein pellet was washed thrice with phosphate buffered saline (PBS) and centrifuged, in order to separate the supernatant solution from the precipitate. The activity associated with protein pellet was estimated using well-type NaI(Tl) scintillation gamma counter.
In-vitro cell binding studies of [68Ga]Ga-Exendin-4
Affinity of [68Ga]Ga-Exendin-4 to GLP1 was analyzed using in-vitro cell binding studies with rat insulinoma cell line INS-1 832/13 having overexpressed GLP1. Cell lines were grown in a tissue culture dish using Iscove’s Modified Dulbecco’s Medium (IMDM) supplemented by 10% Fetal bovine serum (FBS) in 5% CO2, at 37 °C. A fixed number of cells (2.5 × 106) were harvested and incubated in cell internalization buffer with the 0.15 pmol of [68Ga]Ga-Exendin-4 (~ 1 ng peptide, 14.5 × 10–3 MBq in 0.5 mL), for different time intervals (15, 30, 45, 60 and 120 min) at 37 °C. The extent of non-specific binding was analyzed by incubating the same number of cells and radiotracers with an addition of 0.2 nmol of cold Exendin-4[Lys40(NODAGA)]. Binding studies with MCF7 (GLP1 negative) cells were also carried out in identical condition to ascertain the specificity of radiotracer. After incubation, the cells were washed twice with cold 0.05 M phosphate buffered saline (PBS), centrifuged and the cell pellets were counted in a well-type NaI(Tl) scintillation gamma counter.
In-vivo biodistribution studies of [68Ga]Ga-Exendin-4
In-vivo biodistribution studies were conducted in SCID mouse with tumor xenografts, induced with rat insulinoma cells (INS-1 832/13). Xenograft was allowed to grow for about 2 months until the tumor developed to about ~ 1 cm3 volume. Whole body distribution kinetics of intravenously administered radiotracer with and without kidney protection agent (Gelofusine) was evaluated in SCID mice and Wistar rat models [27]. Since Exendin-4 follows a fast renal excretory and renal uptake, gelofusine was administered to the mice to protect the kidney 30 min prior to intravenous administration of [68Ga]Ga-Exendin-4 (3.7–5.5 MBq in 50–70 µL] through the tail vein. Mice were sacrificed at definite time intervals post-administration of radiotracer for biodistribution studies. In rats, uptake of radiotracer in organs 1 h post-administration was analysed using PET/CT imaging, following an identical procedure.
Preclinical dosimetry
Estimation of the organ-absorbed doses and total effective whole-body dose were carried out based on MIRD methodology [20, 21]. Towards this, [68Ga]Ga-Exendin-4 (7.4–11.1 MBq) was injected intravenously into non-tumour bearing SCID mice, through the tail vein after pre-administration of kidney protectant gelofusine (~ 8 mg in 200 µL per mice). Biodistribution data at 1 h, 2 h and 3 h post-administration time points were plotted in OLINDA/EXM 2.0 software to obtain time-activity curves. The organ uptake values (non-corrected for physical decay of radionuclide) were integrated from time zero to infinity to estimate cumulated activity (MBq-h) and effective half-life (h) of radiotracer in the organs. For the radioactivity distributed uniformly in the region of source tissue (rS), the mean absorbed dose D (rT, TD) to the target tissue (rT), over a time-integration period (TD) can be written as per the current MIRD notation, D (rT, TD) = ∑rs à (rS, TD)S(rT ← rS), where “à (rS, TD)” is the time-integrated activity (total number of nuclear transformations) in rS over TD, while “S(rT ← rS)” is absorbed dose in rT per nuclear transformation in rS [28].
The organ distribution data in mouse was extrapolated to estimate dose to human using S-values (mGy MBq−1 h−1) for adult reference male model (ICRP-89) and relative mass scaling method, applying correction factor for mass differences between mice and human species. The percentage of injected activity (%IA) in the mouse organ contents were extrapolated to human organ contents using organ weight and total body weight of human and mice by the equation, %IAanimal x [weightbody/weightorgan]animal × [weightorgan/weightbody]human = %IAhuman. These values (non-decay corrected for physical half-life) were plotted for each time point post injection for obtaining time-activity curves (TAC) by a mono-exponential fitting, through three data points, to determine cumulated activity in each source organ [29]. The kinetic value (cumulated activity per unit administered activity, MBq-h/MBq) for each source organ were determined by dividing the cumulated activity in the source organ by the total injected activity.
Results
Automated radiochemical synthesis of [68Ga]Ga-Exendin-4
In EZ Modular-Lab Standard, a fully automated radiochemical synthesis of pharmaceutical grade [68Ga]Ga-Exendin-4 was carried out successfully, with suitable modification in the radiochemical synthesis process. The radiochemical synthesis was carried out in 25 ± 2 min. The ndc RCY of all the batches of [68Ga]Ga-Exendin-4 (n = 8) thus prepared were (60.9 ± 0.2)%. The dc RCY of [68Ga]Ga-Exendin-4 was (78.7 ± 0.8)% considering 25 min from end of elution (EOE) of [68Ga]GaCl3 from 68Ge/68Ga generator to the end of synthesis (EOS).
Quality control of [68Ga]Ga-Exendin-4
The pharmaceutical grade [68Ga]Ga-Exendin-4 product was found to be clear and colorless, while pH was in the range of 4.5–5.0. The activity concentration (AC) was between 55 and 60 MBq/mL. The RCP of [68Ga]Ga-Exendin-4 (n = 8) assessed by radio-TLC (Fig. 2a–c) using three different solvent systems were, (99.3 ± 0.3)% (0.1 M sodium citrate buffer, pH: 5.0), (99.1 ± 0.6)% (0.1 M EDTA in 0.25 M CH3COONH4, pH: ~ 5.5) and (99.2 ± 0.3)% (1MCH3COONH4 (pH:3.5) /CH3OH: 1/1 v/v) with Rf: 0.01 (Fig. 2a) 0.03 (Fig. 2b) and 0.71 (Fig. 2c) respectively. The RCP derived at by radio-HPLC (n = 8) was (99.1 ± 0.3)% (with Rt: 16.73 min, Fig. 2e).
Radio TLC chromatogram of [68Ga]Ga-Exendin-4: a 0.1 M Sodium citrate buffer (pH ~ 5.0) Rf: 0.01; b 0.1 M EDTA in 0.25 M CH3COONH4 (pH ~ 5.5) Rf: 0.03; c 1M CH3COONH4 (pH: 3.5) /CH3OH: 1/1 (v/v) Rf: 0.71; d Radio TLC of [68Ga]Ga-EDTA (Rf: 0.28) in 0.1 M Sodium Citrate Buffer (pH ~ 5.0) Chromatogram of [68Ga]Ga-Exendin-4; e radio-HPLC (Rt: 16.73 min); f radio-HPLC (Rt: 16.75 min) at 2h post radiolabeling, with stabilizer, on storage at room temperature (25°C); g radio-TLC (Rf: 0.01) after 1h incubation (in healthy human serum, at 37°C) and on further storage up to 1h at 25°C; h radio-TLC of [68Ga]Ga-Exendin-4 (Rf: 0.01) co-spotted with [68Ga]GaCl3 (Rf: 0.94)
In-vitro saline stability (radio-HPLC, Fig. 2f) of the [68Ga]Ga-Exendin-4 (n = 8) was found to be (98.7 ± 0.3)% upto 2 h post-radiolabeling, upon storage at 25°C (room temperature) using 20 mM L-ascorbic acid, as the stabilizer. Radio-TLC chromatogram (Fig. 2g) ascertains the in-vitro serum stability of [68Ga]Ga-Exendin-4 (n = 8) with RCP of (98.2 ± 0.2)% upon 1h post incubation (37°C) with no decrease on further storage for 1h at 25°C. Less than 15% of the activity incubated with serum was found to be bound to the precipitated protein.
For validating the radio-TLC method (solvent system: 0.1 M sodium citrate buffer, pH: 5.0), the [68Ga]Ga-Exendin-4 was spiked with known concentration of [68Ga]GaCl3. Radio-TLC chromatogram (Fig. 2h) exhibits two peaks with Rf 0.01 and 0.94 corresponding to [68Ga]Ga-Exendin-4 and [68Ga]GaCl3 respectively. In order to establish that the adopted radio-TLC method (solvent system: 0.1 M sodium citrate buffer, pH: 5.0) was suitable for separating [68Ga]Ga-EDTA, radiolabeling of EDTA (3.5 µL, 12 nmoles, concentration: 1 µg/µL) with pre-concentrated [68Ga]GaCl3 (515 µL, 1.0 GBq) was performed under similar reaction conditions as employed for radiolabeling of Exendin-4[Lys40(NODAGA)] with [68Ga]Ga3+ (Fig. 2d).
The Endotoxin Limit of [68Ga]Ga-Exendin-4 was found to be < 25 EU/mL (n = 8) with sterility remaining intact for all the batches. The HEPES content in all the produced batches of [68Ga]Ga-Exendin-4 (n = 8) were 7.6 ± 0.2 µg/mL (Fig. 3), while Tween-80 content in the final product was found to be < 0.1%. The specific activity of [68Ga]Ga-Exendin-4 (n = 8) was found to be 105.1 ± 5.2 MBq/nmole, while the Exendin-4[Lys40(NODAGA)] content in the radiolabeled product was found to be 1.36 ± 0.02 µg/mL. [68Ga]Ga-Exendin-4 was eluted from HLB cartridges using absolute ethanol (100%, 0.8 mL), which resulted in the presence of (6.4 ± 0.2)% ethanol in the final product (n = 8). A comparison of the QC parameters of the [68Ga]Ga-Exendin-4 produced in the present study with the specifications stated in the European Pharmacopoeia of gallium (68Ga) Edotreotide Injections presented in Table 2.
In-vitro pharmacokinetic studies of [68Ga]Ga-Exendin-4
In-vitro cell binding studies carried out in INS-1cells showed a rapid and specific binding of (34.4 ± 2.8)% with [68Ga]Ga-Exendin-4 (0.15 pmol) at 30 min (n = 3). The curve of cell binding verses time of incubation gradually plateaus off after 60 min [% cell binding (50.8 ± 2.4)% at this point] of cells incubation with the radiotracer, with slight elevation of the slope for the time > 60 min. The curve attained a maximum total cell binding of (59.8 ± 3.1)% at 150 min. The cell binding reduced to (1.4 ± 0.2)% when incubated with an addition of 0.2 nmol of cold Exendin-4[Lys40(NODAGA)], indicating the specificity of the radiotracer for GLP1 antigen. Non-specific MCF7 cells showed only background counts. Figure 4 shows the total binding at different incubation times.
In-vivo pharmacological behaviour of [68Ga]Ga-Exendin-4 in SCID mice
Biodistribution studies in xenografted SCID mice and normal Wistar rats showed high non-specific uptake of [68Ga]Ga-Exendin-4 in the kidneys. Uptake in the kidneys was (56.6 ± 4.6)% IA/g post 1 h of administration, however, the uptake was found to be reduced by 1.5 times (37.1 ± 5.8)% IA/g by pre-administration of Gelofusine (Fig. 5a). PET/CT image result in Wistar rats (Fig. 5d, e) was in concordance with biodistribution study in mice. A moderate uptake was observed in GLP1 positive organs in xenografted SCID mouse at 1 h of administration, which includes pancreas (3.0 ± 0.5)% IA/g, lungs (8.8 ± 2.1)% IA/g and stomach (3.3 ± 0.7)% IA/g [3, 10, 30]. In the biodistribution studies of xenografted SCID mouse, the tumour uptake of the radiotracer was found to be (14.3 ± 1.9)% IA/g post 2 h of administration, which was 12.5 fold higher (Fig. 5b) compared to that of uptake in blood (1.1 ± 0.2)% IA/g, the uptake in tumor was statistically significant (p < 0.01). At 1 h of post administration of radiotracer, very low uptake was observed in spleen (1.4 ± 0.2)%IA/g and bone (1.5 ± 0.7)% IA/g. Negligible uptake was observed in other organs especially in muscle, brain and heart.
a Biodistribution data of [68Ga]Ga-Exendin-4 in SCID mice. The radiotracer (3–3.7 MBq/mice) was injected through tail vein (n = 3) (*with administration of kidney protectant gelofusine); b Tumor to organ ratio, 2h post-injection; c PET/CT image of SCID mice INS1 xenograft in the left neck, 2h post- injection; d, e PET/CT image of Wistar rat without and with gelofusine respectively, injected with [68Ga]Ga-Exendin-4 and imaged 1 h post-injection
PET/CT image analysis in xenografted SCID mouse and normal wistar rat
A reduction in radiotracer uptake induced by administration of kidney protection agent was observed using in-vivo PET/CT imaging of animals. PET/CT scintigraphy carried out in SCID mouse bearing tumor xenografts (induced with rat insulinoma cells INS-1 832/13), showed tumor uptake of the tracer (Fig. 5c). Pre-administration of ~ 320 mg/Kg dose of gelofusine in normal Wistar rat model, induced about 35% reduction in kidney uptake. PET/CT scan of left kidney (in Wistar rat) exhibited SUVmean of 4.0 (Fig. 5d) without gelofusine administration while the SUVmean was reduced to 2.6 (Fig. 5e) with gelofusine pre-administration.
Preclinical dosimetry
The mean organ-absorbed dose coefficient was found to be the highest in kidneys (0.186 ± 0.015) mGy MBq−1 due to non-receptor specific uptake, followed by uptake in the GLP1 positive organs which include lungs (0.022 ± 0.005) mGy MBq−1 and pancreas (0.019 ± 0.012) mGy MBq−1. Lesser absorbed doses were estimated for organs like stomach (0.015 ± 0.004) mGy MBq−1 and other organs and the results are given in Table 3. The kinetics value (number of nuclear transformations per unit of administered activity) for [68Ga]Ga-Exendin-4 in mouse species (pre-injected with kidney protectant i.e. gelofusine) extrapolated to reference adult male (ICRP-89) are shown in Fig. 6. The total body effective dose coefficient for this radiotracer was estimated to be (0.0056 ± 0.0031) mSv MBq−1.
Discussion
Modification in automated radiochemistry module and radiolabeling protocol
In the EZ Modular-Lab Standard radiochemistry module with constraints of five reservoirs, the automated radiochemical synthesis of [68Ga]Ga-Exendin-4 poses several operational challenges. Inorder to overcome the challenges, two strategies were adopted (i) making provision for extra reservoir (sixth), further integrating the time list for operation of the sixth reservoir with associated solenoid valves through GUI software and (ii) modification in the radiosynthetic process.
In the modified protocol, 20 mM EDTA (400 µL), 10% Tween-80 (30 µL) along with 1 mL ultrapure water were loaded in the 3rd reservoir for cooling the reaction mixture, which otherwise is not being done for the automated radiosynthesis of [68Ga]Ga-Exendin-4 in the cassette-based automated synthesizer. The volume and concentration of mixture (20 mM EDTA, 10% Tween-80 and UPW) were optimized to the extent such that the final concentration of EDTA and Tween-80 in the reaction mixture were maintained at 3 mM and 0.11% respectively.
In the cassette-based automated commercial synthesizer (Modular PharmLab, Modular-Lab PharmTracer and Scinotmics GRP®) as described in reported literature, each of the reagents (HEPES, 1 M CH3COONa buffer, 1 M NaOH, ascorbic acid, EDTA, Polysorbate-80, ethanol) of required concentration and volume, essential for radiosynthesis of [68Ga]Ga-Exendin-4, were aseptically filled and packed in separate customized plastic reagent bottle or syringe. These customized reagents in separate bottle or syringe (with specific volume and concentration) were fitted in the designated slots of cassette prior to radiosynthesis [8,9,10]. Each of these reagents were passed through the reaction vessel one after the other in sequential manner as defined in the time list. Hence, requirement for mixing two or three reagents in optimum concentration and further loading the reagents mixture in the 3rd reservoir as described in our optimized protocol (on using EZ Modular-Lab Standard) is not required in the cassette-based system. Also in our modified protocol, the 4th reservoir was loaded with 6.5 mL of UPW. Post acidified HEPES washing of HLB cartridge, 1.5 mL UPW was passed through the HLB cartridge in order to remove the residual HEPES, so as the HEPES content in the final product is ≤ 20 µg/mL.
After eluting the [68Ga]Ga-Exendin-4 into the final product vial from HLB cartridge (using 0.8 mL of 100% ethanol) the remaining 5.0 mL of UPW from 4th reservoir was passed through HLB cartridge and PES membrane filter to elute residual [68Ga]Ga-Exendin-4 from the PES membrane filter. Also, the final product was diluted to maintain the residual ethanol content less than the permissible limit of 10% V/V. The precise elution of UPW from single reservoir (4th) at different sequence of purification was facilitated only after modifying the existing time list and program operated through GUI software. However, such modification in purification protocol was not required on using cassette based automated synthesizer as described in the reported literature [8,9,10].
The 6th reservoir was loaded with 3 mL of acidified HEPES buffer (0.1N HCl/2.5 M HEPES buffer in 8/1 v/v) to wash the HLB cartridge (post loading of reaction mixture into the HLB cartridge) to remove the free [68Ga]Ga3+in the form of 68Ga]Ga-EDTA as shown in Fig. 1a. In cassette-based module, making modifications in the time list either operating through GUI or human machine interface (HMI) software from user-end is restricted, since the software control of these cassettes worked on radiofrequency identification (RFID) chip scanner which is not the case with fixed-tubing based module (EZ Modular-Lab Standard) [31].
Till date, the modification in fixed tubing or non-cassette based EZ Modular-Lab Standard (making provision for 6th reservoir), followed by synchronizing the modified protocol and the operation of the 6th reservoir after modifying the GUI interfaced existing time list for clinical dose preparation of [68Ga]Ga-Exendin-4, has not yet been reported. The stepwise modification of the radiochemical synthesis protocol for clinical dose preparation of [68Ga]Ga-Exendin-4 in EZ Modular-Lab Standard has been detailed and compared to that of [68Ga]Ga-DOTATATE (Fig. 1b). Additionally, Table 1 describes the position and purpose of various reservoirs containing different reagents required in the present modified radiosynthesis protocol of [68Ga]Ga-Exendin-4, using the EZ Modular-Lab Standard.
After modifying the EZ Modular-Lab Standard, three different gallium-68 based radiotracers, viz. ([68Ga]Ga-DOTATATE, [68Ga]Ga-PSMA-11 and [68Ga]Ga-Exendin-4), were carried out on a single day, in the same module, without any cross-contamination, at every 3–4 h interval. The decay-corrected RCY [(78.73 ± 0.78)%] and RCP [(98.54 ± 0.34)%] were consistent, reliable and reproducible for automated routine preparation of clinical dose of [68Ga]Ga-Exendin-4. The ndc RCY of produced [68Ga]Ga-Exendin-4 by the present methodology, in the modified automated EZ Modular-Lab Standard was ~ 1.22 times higher than that of reported procedures which make use of cassette-based automated synthesizer [8,9,10].
This demonstrates the enhanced utility of the EZ Modular-Lab Standard in a hospital radiopharmacy set-up, with the additional advantage of obviating the dependence on dedicated and costly disposable radiotracer specific cassettes. A comparison of the automated radiochemical synthesis of [68Ga]Ga-Exendin-4 described in the earlier reports vis-a-vis the one standardized by us using EZ Modular-Lab Standard is presented in Table 4.
Radiolabeling buffer
The initial optimization process for radiolabeling of Exendin-4[Lys40(NODAGA)] with [68Ga]Ga3+ was carried out in 1N CH3COONa buffer at pH ~ 4.0. At pH ~ 4.0 (1N CH3COONa buffer) the reaction kinetics is fast and effective radiocomplexation, to give the desired product is favored by reducing the possibility of formation of the [68Ga]Ga-colloid. The Na+ ions of the inorganic buffer (1N CH3COONa buffer, pH ~ 4.0) competes during radiocomplexation of Exendin-4[Lys40(NODAGA)] with [68Ga]Ga3+, thereby reducing the non-decay corrected RCY of the final product, post -SPE (tC18) purification to ~ 49% [32].
In an attempt to increase the RCY of [68Ga]Ga-Exendin-4, the radiolabeling reaction was carried out in an organic buffer (2.5 M HEPES buffer, pH ~ 5.0), wherein the non decay corrected RCY of the final product, post SPE (HLB) purification was increased to ~ 61%. The HEPES with a higher pH value (~ 5.0) was preferred over CH3COONa for radiocomplexation of NODAGA chelator in Exendin-4[Lys40(NODAGA)] with [68Ga]Ga3+. Generally at slightly higher pH (~ 5.0) the pendant donor acid groups of the NODAGA chelator was readily deprotonated for radiocomplexation [33, 34].
In our optimized automated protocol, radiolabeling was carried out with 10.70 nmoles of Exendin-4[Lys40(NODAGA)] in order to prevent the saturation of GLP1. For radiolabeling, a low concentration of Exendin-4[Lys40(NODAGA)] (50 µg or 10.70 nmoles) resulted in a non decay corrected RCY of ~ 61% on using HEPES buffer as the reaction medium. However, when same quantity of Exendin-4[Lys40(NODAGA)] (50 µg) was used for radiolabeling in sodium acetate reaction medium (using CH3COONa.3H2O with > 99.5% purity), the non decay corrected RCY was reduced to ~ 49%. This is attributed to the (i) absence of metallic impurities in HEPES buffer (organic buffer) and (ii) chelation of acetate ions (CH3COO−) with [68Ga]Ga3+. [35, 36]. The variation in RCP and decay corrected RCY of [68Ga]Ga-Exendin-4 in HEPES and CH3COONa buffer system at different pH is depicted in Fig. 7.
In order to avoid the usage of HEPES buffer as reaction medium and subsequent quantification of HEPES content in the final product, numerous experiments were carried out to standardize a radiosynthetic protocol using CH3COONa buffer, so as the final product could be obtained with reasonable ndc RCY (~ 60%). Towards achieving this, radiolabeling of Exendin-4[Lys40(NODAGA)] was carried out with pre-concentrated [68Ga]GaCl3 using two different concentration of CH3COONa buffer (1 M and 2 M). However, in none of the experiments, the dc RCY of the final product obtained was more than 65%. The RCP and dc RCY of the final product i.e. [68Ga]Ga-Exendin-4, in different buffer concentrations is depicted in Fig. 8.
Quantification of HEPES and its permissible limit
The allowed limit of HEPES content in the final product as described in European pharmacopoeia shall be ≤ 200 µg/V, where V is the maximum volume of injection. The limit of HEPES content in the [68Ga]Ga-Exendin-4 obtained by the present method has been evaluated by considering the maximum volume of injection (7–10 mL). Towards this, the HEPES content in the product [68Ga]Ga-Exendin-4 was found to be 7.56 µg/mL as estimated by our developed methodology and depicted in Fig. 3. This value translates to 53–75 µg of HEPES in a single intravenous administration of [68Ga]Ga-Exendin-4 (considering 70 kg as standard body weight of the patient, which corresponds to 0.75–1.02 µg/kg of body weight). The HEPES content in all the batches of [68Ga]Ga-Exendin-4 were found to be much below the permissible limit and in accordance with European Pharmacopoeia [23, 37].
The HEPES quantification methodology described in our studies constitutes the first of its kind report. However, till date, the sensitive quantification of HEPES in various [68Ga]Ga-radiotracers has been estimated employing high performance liquid chromatography (HPLC) system equipped with UV detector using either C-18 reversed phase column or N analytical column [34]. In all these reports, the minimum limit of quantification (LOQ) involved was ≥ 3 µg/mL. Among all those reported studies, the fastest Rt for HEPES was 2.4 min [24, 38,39,40]. Also, poor separation of the HEPES and dilution buffer (NaCl or PBS) peak in the HPLC methodology was observed in two of the reported studies [24, 40]. To circumvent such limitations in detection of HEPES in the final product, the adopted method using microvolume spectrophotometer, in the present study has demonstrated the LOQ > 2.5 µg/mL. Additionally, the described procedure allows to carry out the quantification in a very short time (within 75 s). The rapid and consistent quantification of HEPES thus allowscompletion of the test prior to release of the product for patient use, alongwith minimization of the decay time of [68Ga]Ga-Exendin-4.
Choice of SPE resin for purification of [68Ga]Ga-Exendin-4
The choice of suitable SPE resin for purification post radiolabeling, directly reflects on the RCP and the RCY of the final product. In our methodology, process optimization of the initial SPE-based purification was carried out with light C18 (130 mg) and light tC18 (145 mg) SPE resin, when the reaction medium was CH3COONa buffer. The RCP of the produced [68Ga]Ga- Exendin-4 batches were found to be consistent and > 98%, albeit with variation in RCY. The tC18 SPE resin purification resulted in better RCY compared to the use of C18 SPE column as depicted in Fig. 9. This is attributed to the trifunctional binding affinity of analytes, with better hydrolytic stability, on using tC18 SPE resin compared to that of C18 [18].
The ndc RCY of the final product ([68Ga]Ga-NODAGA-Exendin-4) obtained was < 50% on carrying out tC18 SPE based purification. This necessitates the development, optimization and adoption of a different SPE based purification methodology, where the RCY of the final product could be increased considerably. Towards this goal, SPE purification post-radiolabeling were carried using plus HLB resin (225 mg), while the reaction was carried out in HEPES medium. This protocol resulted in non decay corrected RCY of ~ 61% (Fig. 9). This is attributable to the use of HLB resin which is composed of [poly(divinylbenzene-co–N-vinylpyrrolidone} as functional groups having high retention capacity of the hydrophilic peptide, which otherwise was not the case while using C18 or tC18 resin [18].
Requirement for detailed pre-clinical investigations
The in-vitro and in-vivo studies were carried out to determine the pharmacokinetics of [68Ga]Ga-Exendin-4. The results indicate the specific binding of the agent to GLP1 in INS-1 cell line. In-vivo distribution and PET/CT studies in SCID mice with insulinoma-induced tumors revealed substantial radiotracer uptake. In line with reported literature, notable kidney uptake was observed, which is well mitigated by gelofusine pre-treatment. The radiotracers exhibited moderate uptake in GLP1 positive organs such as the pancreas and lungs. Preclinical dosimetry shows mean total body effective dose coefficient 0.0056 mSv MBq−1, which is 20% lesser than the value of 0.0071 mSv MBq−1 estimated by M. Boss et al. from PET-based dosimetry in patient (Table 3) [41]. This difference can be attributed to lesser kidney uptake in the present study by pre-administration of kidney protectant gelofusine in mice [27]. Kidneys being the organ wherein highest uptake of this radiotracer could be observed, a co-administration of kidney protectant can decrease the kidney adsorbed dose and thereby reduce the total body effective dose from this product. Mean absorbed dose coefficient to kidneys observed in the present study was 0.186 mGy MBq−1 which is 39% lesser than the value of 0.472 mGy MBq−1 as estimated by M. Boss et al. and 33% lesser than the value of 0.276 mGy MBq−1 as estimated by Selvaraju et. al. (Table 3). Absorbed dose to lungs was 0.026 ± 0.005 mGy MBq−1, which is 1.66 times higher than the value 0.013 mGy MBq−1 reported by Selvaraju et.al., but is acceptably low since the tissue tolerance dose (TD5/5) for lungs is 17.5 Gy [42]. Dose to pancreas and liver were within ± 20% deviation from the values reported by M. Boss et al. For a standard ~ 100 MBq PET injection dose, the estimated mean absorbed dose to the dose limiting organ kidneys was 18.57 ± 1.51 mGy/ 100 MBq for adult, which is far below the toxicity limit of 23 Gy (TD 5/5) for the organ [43]. The estimated total body effective dose in the present study with co-administration of gelofusine (~ 0.3 g/Kg adult) was 0.56 ± 0.31 mSv/ 100 MBq, which is low as well as the acceptable level of medical radiation exposure in diagnostic procedures. This study documents the potential of [68Ga]Ga-Exendin-4 in the diagnosis of insulinoma and other related disorders.
Conclusion
An efficient, reliable and consistent method was developed for the automated radiochemical synthesis for clinical dose preparation of [68Ga]Ga-Exendin-4 with high decay corrected RCY of (78.7 ± 0.8)% and RCP of > 98%, using fixed tubing-based or non-cassette based EZ Modular-Lab Standard. The quality of the produced [68Ga]Ga-Exendin-4 was in accordance with European Pharmacopoeia of gallium (68Ga) Edotreotide® Injections. The highest radiochemical yield was obtained when using HEPES as the reaction medium and HLB resin for post-radiolabeling purification. The rapid and specific binding of the radiotracer to INS-1 cells, demonstrate the affinity and specificity of the radiotracer towards GLP-1 receptors. PET/CT imaging carried out in SCID mice bearing tumor xenografts [induced with rat insulinoma cells INS-1 832/13], at 60 min post [68Ga]Ga-NODAGA-Lys40-Exendin-4 injections, showed uptake of the tracer in tumor, and was observed to be in concordance with the tissue distribution kinetics of SCID mice tumor model. Biodistribution analysis in SCID mice and Wistar rats with pre-administration of kidney protectant Gelofusine (~ 0.3 g/Kg body weight), showed ~ 35% reduction in the non-receptor-specific kidney uptake of the radiotracer. In order to carry out pre-clinical dosimetry estimations, the biodistribution data of normal SCID mice (pre administrated with Gelofusine as kidney protectant), was extrapolated to reference adult human (ICRP 89). Mean organ absorbed dose coefficient was estimated to be highest for kidneys (~ 1.86E-01 mGy MBq−1), which is lesser than the values reported without pre-administration of kidney protectant as reported by M. Boss et. al. and Selvaraju et. al. [38, 39]. The pre-clinical results establish the diagnostic efficacy of the product towards clinical translation. The modification in the EZ Modular-Lab Standard described in the present study, enabled the production of three different gallium-68 based radiotracers, viz. ([68Ga]Ga-DOTATATE, [68Ga]Ga-PSMA-11 and [68Ga]Ga-Exendin-4), on a single day, in the same module, without any cross-contamination, at every 3–4 h interval, which offered a definitive advantage to the hospital radiopharmacy unit catering to a high-volume nuclear medicine facility.
Data availability
The raw data supporting this study will be available upon request from the corresponding author.
References
Mehrabi A, Fischer L, Hafezi M et al (2014) A systematic review of localization, surgical treatment options, and outcome of insulinoma. Pancreas 43(5):675–686
Jansen TJP, van Lith SAM, Boss M et al (2019) Exendin-4 analogs in insulinoma theranostics. J Label Comp Radiopharm 62(10):656–672
Wild D, Wicki A, Mansi R et al (2010) Exendin-4-based radiopharmaceuticals for glucagonlike peptide-1 receptor PET/CT and SPECT/CT. J Nucl Med 51(7):1059–1067
Velikyan I, Bulenga TN, Selvaraju R et al (2015) Dosimetry of [177Lu]-DO3A-VS-Cys 40-Exendin-4-impact on the feasibility of insulinoma internal radiotherapy. Am J Nucl Med Mol Imaging 5(2):109–126
Nock BA, Kanellopoulos P, Joosten L et al (2023) Peptide radioligands in cancer theranostics: agonists and antagonists. Pharmaceuticals 16(5):674
Felber VB, Wester HJ (2021) Small peptide-based GLP-1R ligands: an approach to reduce the kidney uptake of radiolabeled GLP-1R-targeting agents? EJNMMI Radiopharm Chem. https://doi.org/10.1186/s41181-021-00136-x
Joosten L, Brom M, Peeters H et al (2018) Enhanced specific activity by multichelation of Exendin-3 leads to improved image quality and in vivo beta cell imaging. Mol Pharm 15(2):486–494
Migliari S, Sammartano A, Boss M et al (2022) Development and validation of an analytical HPLC method to assess chemical and RADIOCHEMICAL purity of [68Ga]Ga-NODAGA-Exendin-4 produced by a fully automated method. Molecules. https://doi.org/10.3390/molecules27020543
Kraihammer M, von Guggenberg E, Hörmann AA et al (2023) Automated production of [68Ga]Ga-DOTA-Exendin-4 via fractionated radionuclide generator elution on a cassette based synthesis module. Nucl Med Biol. https://doi.org/10.1016/j.nucmedbio.2023.108381
Velikyan I, Rosenstrom U, Eriksson O (2017) Fully automated GMP production of [68Ga]Ga-DO3A-VS-Cys40-Exendin-4 for clinical use. Am J Nucl Med Mol Imaging 7(3):111–125
Bandara N, Zheleznyak A, Cherukuri K et al (2016) Evaluation of Cu-64 and Ga-68 radiolabeled glucagon-like peptide-1 receptor agonists as PET tracers for pancreatic β cell imaging. Mol Imaging Biol 18(1):90–98
Brom M, Franssen GM, Joosten L et al (2016) The effect of purification of Ga-68-labeled Exendin on in vivo distribution. EJNMMI Res. https://doi.org/10.1186/s13550-016-0221-8
Migliari S, Sammartano A, Scarlattei M et al (2022) Feasibility of a scale-down production of [68Ga]Ga-NODAGA-Exendin-4 in a hospital based radiopharmacy. Curr Radiopharm 15(1):63–75
Garcia-Arguello SF, Lopez-Lorenzo B, Ruiz-Cruces R (2019) Automated production of [68Ga]Ga-DOTANOC and [68Ga]Ga-PSMA-11 using a TRACERlab FXFN synthesis module. J Label Comp Radiopharm 62(3):146–153
Boschi S, Lodi F, Malizia C et al (2013) Automation synthesis modules review. Appl Radiat Isot 76:38–45
Boschi S, Malizia C, Lodi F (2013) Overview and perspectives on automation strategies in 68Ga radiopharmaceutical preparations. Recent Results Cancer Res 194:17–31
Huang YP, Robinson RC, Dias FFG et al (2022) Solid-phase extraction approaches for improving oligosaccharide and small peptide identification with liquid chromatography-high-resolution mass spectrometry: a case study on proteolyzed almond extract. Foods. https://doi.org/10.3390/foods11030340
Guo X, Kristal BS (2012) The use of underloaded C18 solid-phase extraction plates increases reproducibility of analysis of tryptic peptides from unfractionated human plasma. Anal Biochem 426(1):86–90
Stabin MG, Sparks RB, Crowe E (2005) OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 46(6):1023–1027
Howell RW, Wessels BW, Loevinger R et al (1999) The MIRD perspective 1999. J Nucl Med 40(1):3s–10s
Eckerman KF, Endo A (2007) [Book] MIRD: Radionuclide Data and Decay Schemes. The Society of Nuclear Medicine, Reston
Repetto-Llamazares AHV, Larsen RH, Mollatt C et al (2013) Biodistribution and dosimetry of 177Lu-Tetulomab, a new radioimmuno-conjugate for treatment of non-Hodgkin lymphoma. Curr Radiopharm 6(1):20–27
European Pharmacopoeia (2011) Gallium (68Ga) Edotreotide Injection Monograph. PA/PH/Exp. 14/T(07) 12 ANP 2R: 2482, Pharmeuropa 23(2)
Antunes IF, Franssen GM, Zijlma R et al (2020) New sensitive method for HEPES quantification in 68Ga-radiopharmaceuticals. EJNMMI Radiopharm Chem. https://doi.org/10.1186/s41181-020-00093-x
Satpati D, Vats K, Sharma R et al (2020) 68Ga-labeling of internalizing RGD (iRGD) peptide functionalized with DOTAGA and NODAGA chelators. J Pept Sci. https://doi.org/10.1002/psc.3241
Bhadwal M, Das T, Dev Sarma H et al (2015) “Radiosynthesis and bioevaluation of [68Ga]-Labeled 5,10,15,20-Tetra(4-methylpyridyl)-porphyrin for possible application as a PET radiotracer for tumor imaging. Mol Imaging Biol 17(1):111–118
Luo Y, Pan Q, Li F (2020) Decreased 68Ga-NOTA-Exendin-4 renal uptake in patients pretreated with Gelofusine infusion: a randomized controlled study. J Pancreatol 3(3):161–166
Dewaraja YK, Frey EC, Sgouros G et al (2012) MIRD pamphlet no. 23: Quantitative SPECT for patient-specific 3-dimensional dosimetry in internal radionuclide therapy. J Nucl Med 53(8):1310–1325
Cona MM, Koole M, Feng Y et al (2014) Biodistribution and radiation dosimetry of radioiodinated hypericin as a cancer therapeutic. Int J Oncol 44(3):819–829
Janota B, Karczmarczyk U, Laszuk E et al (2016) Oxidation of methionine - Is it limiting the diagnostic properties of 99mTc-labeled Exendin-4, a glucagon-like peptide-1 receptor agonist? Nucl Med Rev 19(2):104–110
Nader M, Valla DF, Vriamont C et al (2022) [68Ga]/[90Y]FAPI-46: Automated production and analytical validation of a theranostic pair. Nucl Med Biol 110–111:37–44
Tsionou MI, Knapp CE, Foley CA et al (2017) Comparison of macrocyclic and acyclic chelators for gallium-68 radiolabelling. RSC Adv. https://doi.org/10.1039/c7ra09076e
Velikyan I, Beyer GJ, Bergström-Pettermann E et al (2008) The importance of high specific radioactivity in the performance of 68Ga-labeled peptide. Nucl Med Biol 35(5):529–536
Suthiram J, Ebenhan T, Marjanovic-Painter B et al (2021) Article towards facile radiolabeling and preparation of gallium-68-/bismuth-213-dota-[thi8, met(O2)11]-substance p for future clinical application: First experiences. Pharmaceutics. https://doi.org/10.3390/pharmaceutics13091326
Velikyan I, Beyer GJ, Långström B (2004) Microwave-supported preparation of 68Ga bioconjugates with high specific radioactivity. Bioconjug Chem 15(3):554–560
Bauwens M, Chekol R, Vanbilloen H, Bormans G, Verbruggen A (2010) Optimal buffer choice of the radiosynthesis of 68Ga–Dotatoc for clinical application. Nucl Med Commun 31(8):753–758
le Roux J, Kleynhans J, Rubow S et al (2021) The use of HEPES-buffer in the production of gallium-68 radiopharmaceuticals—Time to reconsider strict pharmacopoeial limits? EJNMMI Radiopharm Chem. https://doi.org/10.1186/s41181-021-00129-w
Sasson R, Vaknin D, Bross A et al (2010) Determination of HEPES in 68Ga-labeled peptide solutions. J Radioanal Nucl Chem 283(3):753–756
Migliari S, Scarlattei M, Baldari G et al (2022) A specific HPLC method to determine residual HEPES in [68Ga]Ga-radiopharmaceuticals: development and validation. Molecules. https://doi.org/10.3390/molecules27144477
Pfaff S, Nehring T, Pichler V et al (2018) Development and evaluation of a rapid analysis for HEPES determination in 68Ga-radiotracers. EJNMMI Res. https://doi.org/10.1186/s13550-018-0449-6
Boss M, Buitinga M, Jansen TJP et al (2020) PET-based human dosimetry of 68Ga-NODAGA-Exendin-4, a tracer for β-cell imaging. J Nucl Med 61(1):112–116
Selvaraju RK, Bulenga TN, Espes D et al (2015) Dosimetry of [68Ga]Ga-DO3A-VS-Cys 40-Exendin-4 in rodents, pigs, non-human primates and human-repeated scanning in human is possible. www.ajnmmi.us/ISSN:2160-8407/ajnmmi0007362
Emami B, Lyman J et al (1991) Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21:109–122
Acknowledgements
The authors thank the staff of the Hospital Radiopharmacy Section, Radiopharmaceutical Evaluation Section, Radiation Hazard Control Unit and the Animal House Facility of RMC, BARC, for providing the facilities to carry out the work. The authors also thank Shri Arnab Mitra, UG-Student, IIT(ISM), Dhanbad, India for formatting the figures. The support and encouragement of Head, Radiation Medicine Centre, BARC is being gratefully acknowledged.
Funding
Open access funding provided by Department of Atomic Energy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Menon, S.R., Mitra, A., Chakraborty, A. et al. Automated radiosynthesis of pharmaceutical grade [68Ga]Ga-NODAGA-Lys40-Exendin-4 and demonstration of its efficacy for use in patients. J Radioanal Nucl Chem (2024). https://doi.org/10.1007/s10967-024-09535-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10967-024-09535-1