Abstract
In the face of the challenges of rising demand and increasing economic pressure, medical service innovations and university hospitals are becoming increasingly important as cornerstones for the continuous development of medical care. Simultaneously, increasing technological complexity, scarce funding, and resource-intensive technology development are forcing university hospitals to open up their internal innovation processes. Numerous studies have highlighted the beneficial effects of cross-sectoral collaboration on the innovation performance of industrial entities, while neglecting the perspective of academic institutions. The impact of industry collaborations on the service innovativeness of university hospitals in particular has not been addressed in previous research. Although the potential for nonlinear effects of university-industry collaborations has been discussed in research, adequate evidence, particularly in the healthcare context, has not been provided. Therefore, this study addresses the questions: (1) What is the impact of university-hospital-industry collaboration (UHIC) on the service innovativeness of university hospitals? (2) Can a nonlinear relationship between UHIC and university hospitals' service innovativeness be empirically verified? The hypotheses are tested based on an unbalanced panel data set, which combines three distinct data sources and comprises annual observations from 2011 until 2019 of all German university hospitals. The findings indicate that the UHIC intensity has a positive effect on university hospitals’ service innovativeness with a one-year time lag. Furthermore, a negative quadratic UHIC effect was found. In doing so, this study complements existing research and opens the black box by uncovering the downside of cross-sectoral collaboration for a more complete understanding of the underlying dynamics of this growing area of research, with a particular focus on university hospitals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
University hospitals are widely recognized as cornerstones of the healthcare system for their medical excellence and key role in the continuous development of medical care (Heyder, 2015; Lehoux et al., 2016; Weigel, 2011). Beyond the increasing competitive and performance pressure on German university hospitals, there is a paradigm shift in the framework conditions both in the context of medical care and in medical university research (Töpfer & Albrecht, 2017). With the introduction of the reimbursement system according to “Diagnosis Related Groups” (DRG), medical services have been reimbursed according to fixed lump sums since 2003, regardless of the actual use of resources. However, this reimbursement system does not take into account the growing costs and scarce financial and human resources in the hospital sector (Busse et al., 2013; Sturm et al., 2019). While the proportion of economically active population is constantly decreasing, the proportion of older and thus, multimorbid patients rises (Laubach & Fischbeck, 2007). According to recent forecasts of case numbers and length of stay in Germany, the number of cases in hospitals is expected to increase from 19.4 million to 22 million by 2030, while the proportion of patients over the age of 60 is expected to increase from 51 to 61%. As a result, university hospitals, as providers of the highest level of care, are under particular pressure to deliver the highest quality of patient care at the lowest cost (Hinkelmann et al., 2017).
In the face of rising challenges in the healthcare system, innovation in medical services has rapidly gained importance in recent years, forcing hospitals, including university hospitals, to adapt the profitability of their service portfolios to increasing competition and cost pressures (Häussler et al., 2010; Savva et al., 2023). While most of the existing literature on innovation focuses on single activities (e.g., the introduction of new specific technology), this study focuses on the portfolio level of service innovation. Given that the benefits of single activities may be short-lived, relying on an innovative service portfolio allows the hospital to strengthen its long-term market position (Cooper et al., 1999; Salge & Vera, 2009; Schultz et al., 2012). Previous empirical studies demonstrate the crucial role of the adoption of medical service innovations, in improving health service providers’ financial performance (Trinh et al., 2008; Zengul et al., 2018), as well as various clinical outcome variables, such as mortality rate (Jiang et al., 2006), readmission rate and average length of hospital stay (Moreira et al., 2017), operational efficiency measured as proportion of outpatient surgeries (Dias & Escoval, 2015), and patient-perceived quality of care (Wu & Hsieh, 2011). Thus, in order to ensure their long-term performance and quality of care, hospitals need to implement medical service innovations that incorporate changes in the technology, design, or delivery of a specific health service or a bundle of such services (Greenhalgh et al., 2004; Mutlu & Sürer, 2015). University hospitals, in particular, as providers of the maximum level of care, are under particular economic pressure and thus are forced to innovate in order to improve their efficiency (Blümel et al., 2020; Hinkelmann et al., 2017; Schultz et al., 2011). This study aims to explain the service innovativeness of university hospitals in particular. Following the literature on service innovation, service innovativeness is defined as the extent to which a service provider (i.e., a university hospital) implements and offers new (medical) procedures within its existing service portfolio (Greenhalgh et al., 2005; Lee et al., 2009; Schultz et al., 2012).
Rising technological complexity, scarcity of funds, and resource-intensive technology development are prompting more and more university hospitals to open up their internal innovation processes (Kesting, 2013; Lester & Sotarauta, 2007). Significant cuts in funding for academic research and teaching, partly as a consequence of the Europe-wide financial crisis, have led to an existential dependence of universities on third-party funding (Heyder, 2015; Kesting, 2013). Consequently, in order to secure their existence and research function in long-term, medical university research needs to intensify innovation-oriented and practice-orientated collaborations with industry partners (Häussler et al., 2010; Lester & Sotarauta, 2007). Despite the rising importance to implement innovative medical services, research about university-industry collaboration (UIC) in the medical field are sparse (Tsuruya et al., 2018). But the potential of collaboration between the industry and medical facilities and health professionals are emphasized in numerous studies. For instance, Chatterji et al. (2008) found that 20% of the approximately 26,000 patents filed in the U.S. medical device industry between 1990 and 1996 were held by practicing physicians. In addition, the study showed that physician patents had a stronger influence on subsequent invention activity than pure industry patents without physician involvement. However, this finding emphasizes the importance of cross-sectoral collaboration in the medical device discovery process (Chatterji et al., 2008). The role of industrial funding of academic research has further grown in the last decades, pinpointing the rising relevance of UIC for innovation (Fischer et al., 2018; Gulbrandsen & Smeby, 2005). Given impede conditions of health care organizations, literature has increasingly emphasized the role of research networks and therefore the sharing of capabilities, resources and competencies with industry to create new service innovations. In this regard, UIC is considered to be a main engine of innovation in the context of the knowledge-intensive economy (Muscio & Pozzali, 2013; Tian et al., 2022; Wirsich et al., 2016).
Despite the extensive and growing literature on UIC and firms’ innovation performance (Gretsch et al., 2019; Kobarg et al., 2018; Tian et al., 2022), little attention has been paid to potential effects of industrial research collaboration in the innovation context from particularly health service providers’ perspective (Dhainaut et al., 2020; Wit-de Vries et al., 2019). No quantitative study exists that has examined the role of industry research collaborations on university hospitals’ service innovativeness. In this regard, this research aims to provide a better understanding of how university hospitals may benefit from industrial research partnerships, and how university hospitals should manage their research collaborations in order to successfully respond to the increasing competitive and economic pressures in healthcare. Following established theoretical frameworks of previous studies in the UIC research field (e.g., the resource-based view (Barney, 1991)), this study argues that university hospitals may use the external knowledge and resources gained from their industry research partners to develop, refine, and implement new medical service innovations. However, to close existing research gaps and complement previous research, this study tests for the existence of a marginal effect of university-hospital-industry collaboration (UHIC). On the one hand, limited capabilities (Muscio, 2010), increasing coordination efforts (D’Este & Patel, 2007), and a growing perceived threat of losing academic freedom (Azagra-Caro et al., 2006; Tartari & Breschi, 2012), as well as an increasing cognitive distance between academic and industrial researchers (D’Este & Perkmann, 2011; Muscio & Pozzali, 2013), may limit the integration of too many external knowledge sources. On the other hand, increasing marginal returns of UHIC intensity might exist because of learning effects and emerging trust toward industry partners (Bruneel et al., 2010; Rajalo & Vadi, 2017).
The proposed hypotheses are tested by applying a panel data of all available German university hospitals for the period between 2011 and 2019. This data allows us to consider objective information about the degree of service innovativeness of hospitals as well as the incorporation of relevant control variables. The UHIC intensity is measured based on extracted publication data from Web of Science (WoS) following the co-authorship concept (Bozeman et al., 2013). To provide valid empirical evidence, this study introduced a set of robustness checks with, for instance, an alternative measure for the hospital service innovativeness and UHIC intensity. This study contributes to the sparse literature on the impact of UIC on the implementation of service innovations in university hospitals and aims to reconcile long-standing conflicting views on the marginal effects of cross-sectoral research collaborations.
2 Theoretical background and hypotheses
2.1 The effect of industry collaboration on university hospitals’ service innovativeness
Collaborative research between universities and industry are recognized to increase the rate of innovation in diverse sectors (Mueller, 2006; Rajalo & Vadi, 2017). Substantial research has been focusing on beneficial effects of UIC, as such positive effects on the quality of new product ideas (Gretsch et al., 2019), technological product newness (Wirsich et al., 2016), commercialization success of novel products (Duysters & Lokshin, 2011; Kobarg et al., 2018), financial outcome and patent count (George et al., 2002; Tian et al., 2022). Many studies have been focusing on innovative performance in the manufacturing industry, but at the same time less attention has been given to the service industry (Hee et al., 2018). Distinctive service quality is essential to service providers, particularly in the healthcare sector (Eiriz et al., 2010; Trinh et al., 2008). However, there is a persistent lack of empirical studies that focus on the relationship between industry research collaborations, and the introduction of service innovations, particularly in the hospital sector (Dhainaut et al., 2020; Tsuruya et al., 2018).
Since healthcare systems are facing greater scarcity of financial and human resources, high quality and efficient medical treatment can be ensured by implementing new service innovations (Lehoux et al., 2016; Preker & Harding, 2003). Recent literature emphasizes three major innovation-related benefits that can accrue to both sides in the course of UIC. First, ideally, all parties involved gain valuable access to complementary resources. According to the “resource-based view” (RBV), internal resources alone are often insufficient for the development of new products and/or services to cope with the increasing environmental complexity and the speed of technological change (Barney, 1991; Peteraf, 1993; van Rijnsoever et al., 2008). According to this view, in an increasingly dynamic environment, organizations rely more and more on external sources of knowledge and resources, which can provide a significant portion of the inputs required to develop successful innovations. Therefore, research collaboration has become an important vehicle in this knowledge sourcing process, and thus firms, but also academic institutions, engage in UIC collaboration (Belderbos et al., 2015; Enkel et al., 2009; Schultz et al., 2021).
Second, collaborative research is also associated with cost and risk sharing, which can be particularly valuable for both sides, especially in the context of increasing technological complexity and investment-intensive research and development (Kobarg et al., 2018; Wirsich et al., 2016). This is particularly true if the organization intends to introduce services that are new to the organization, and if the organization plans to target new market segments with either limited or no previous experience (Kock et al., 2011). Furthermore, this is also important in the case of complex medical service innovations, where an imitation of innovation activities reduces uncertainty during the innovation process (Kennedy & Fiss, 2009; Trinh et al., 2008).
Finally, UIC literature often emphasizes the potential synergy effects underlying the merging of basic academic research with the practice-oriented research of industrial entities. In the context of knowledge translation, i.e., the transfer of findings from basic research into practice, companies benefit through an appropriate share of the profits, for instance, involving patenting and licensing of inventions as well as academic entrepreneurship (Ortiz, 2013; Wit-de Vries et al., 2019). On the other hand, knowledge translation is for academic research also a major motive to engage in UIC, for instance, to test novel ideas and/or theories and apply them in practice-related settings (Ankrah et al., 2013; Tseng et al., 2020). Thus, for university research, which is often seen as a driver of basic research (Bruneel et al., 2010; Kesting, 2013; Ponds et al., 2010), the opportunity arises for the application and timely implementation of applied research (D’Este & Perkmann, 2011; Lang, 2013). It is also plausible to assume that university medicine strives for a more effective translation of knowledge from basic medical research into clinical practice. So, it should be underlined that research collaborations are not only driven by financial incentives (Colyvas et al., 2002; Tartari & Breschi, 2012). Universities also devote many of their own resources to most collaborative research projects (Lester & Sotarauta, 2007; van Rijnsoever et al., 2008). In this context, D'Este and Perkmann (2011) were able to show in their qualitative study in the United Kingdom that it is not the economic aspects that are decisive for academic scientists, but rather the opportunity to advance their own research through an exchange of content with industrial research. Given the high demand for medical service innovations to improve the quality and efficiency of their own hospital operations (Greenhalgh et al., 2005; Labitzke et al., 2014; Lehoux et al., 2016), this also seems plausible for German university medicine. In addition, the gap between academic laboratories and the industrial marketplace has shrunk, and therefore universities, teaching hospitals, and other academic institutions have become more adept at commercializing academic research (Lehoux et al., 2016; Lester & Sotarauta, 2007).
Within the large number of studies that have focused on the potential positive effects of UIC on innovation at the organizational level, many previous studies have neglected the possible time-lag effect of research collaborations (Wirsich et al., 2016). In fact, research results in the form of new products, processes, or services usually cannot be introduced into practice immediately after the development process or the publication of the knowledge base (Ponds et al., 2010). In the medical field, the introduction of innovations is related with a high level of uncertainty and thus, can be very time-consuming (Angst et al., 2010; Schultz et al., 2011; Weigel, 2011). First, new medical services have to be checked with the Institute for Hospital Payment Systems to see if they already exist in the existing DRG system. If this is not the case, the concrete fees for the new medical procedure must be negotiated with the statutory health insurers, which are often rejected in the initial application rounds (Blümel et al., 2020; Häussler et al., 2010). In this regard, it is conceivable that research collaborations with industry partners may have a delayed impact on the introduction of new medical services in university hospitals. In summary, university hospitals can gain valuable complementary resources from UHIC, as well as the opportunity for knowledge translation and risk sharing during the innovation process, which overall facilitates the implementation of new medical service innovations. Based on these arguments, the following hypothesis is derived:
Hypothesis 1
University-hospital-industry collaborations have a positive impact on the service innovativeness of university hospitals.
2.2 Nonlinear effects of industry collaboration on university hospitals’ service innovativeness
According to recent research, the effects associated with UIC on the creation of new knowledge and innovations are not strictly linear (Cheng et al., 2020; Melnychuk et al., 2021; Wirsich et al., 2016). At the same time, however, the results of studies in this area of research are not consistent as to whether UIC has diminishing or increasing marginal effects (Banal-Estañol et al., 2015).
Scholars have argued that both university and industry actors are interested in building long-term relationships with each other to take advantage of their complementary organizational strengths (Arundel & Geuna, 2004; Azagra-Caro et al., 2006; Bruneel et al., 2010; Mueller, 2006). However, the formation of ties and interactions for efficient knowledge transfer in cross-sectoral research collaborations requires many different prerequisites, such as familiarity, trust, common understanding and language, and a long-term commitment to the collaboration (Muscio & Pozzali, 2013; Ortiz, 2013; Thune, 2007). For example, a recent UIC review by Wit-de Vries et al. (2019) shows that interpersonal interactions are often emphasized in studies by university and industry actors as the main mechanisms for bilateral knowledge flows. By intensifying interactions, involved research partners can learn about each other's needs, capabilities, and competencies, and this can also lead to internal capabilities to better coordinate and improve the required processes in collaborative research (Ankrah et al., 2013; Tartari & Breschi, 2012). This, in turn, increases the available (slack) resources and capabilities that would otherwise have to be invested in the costly management of UIC and can thus be invested instead in internal innovation activities. To summarize, an increasing number of research collaborations and more intensive networking activities can lead to a higher exchange of knowledge and resources due to the growing trust and the emergence of informal relationships and learning effects between university and industry actors. This leads to the suggestion that the effects of UHIC are not linear, but may have an increasing marginal effect on the service innovativeness of university hospitals:
Hypothesis 2a
The positive effect of university-hospital-industry collaborations on service innovativeness of university hospitals will show an increasing marginal effect.
Despite the often emphasized positive influence of UIC on service innovation, negative aspects and potential decreasing marginal (nonlinear) effects of UIC are still poorly explored (Lin, 2017; Wit-de Vries et al., 2019). Literature often highlights that organizations struggle to apply externally generated resources and knowledge due to limited internal capabilities, since assimilation and integration of novel knowledge required an immense amount of available resources and need to overcome different knowledge barriers (Hee et al., 2018). Organizational theory has often emphasized that an organization's capacity, also known as its "absorptive capacity," to integrate information and knowledge from external sources to generate or implement innovations is limited by its available resources and knowledge base (Azagra-Caro et al., 2006; Kobarg et al., 2018). According to this view, the limited organizational capacity to digest new external knowledge will also limit the potential impact of UHIC on the service innovativeness of university hospitals to a certain extent. As the number of research partners increases, so does the complexity of managing a diverse portfolio of collaborations and the need to allocate limited internal resources to managing them. As a result, UIC can be disproportionately costly and strategically challenging, and potential problems arise from being "too open" and overweighting the beneficial effects (Faems et al., 2010; George et al., 2002; Wirsich et al., 2016). For instance, Duysters and Lokshin (2011) show that alliance complexity has an inverse U-shaped relationship with innovation performance (i.e., introduction of new products to the market). The results the study of Lin (2017) complements this view by revealing that the number of industry collaborations has an inverted U-shaped relationship with the academic innovation of universities, measured as the number of citations of the scientific publications. Although these empirical studies do not focus on the perspective of university hospitals and service innovation, they explain the diminishing marginal effect of UIC by emphasizing the increasing complexity with increasing number of cross-sectoral collaborators. Besides complexity, coordination, decision-making, and monitoring efforts may increase disproportionately with the number of collaborations, leading to redundancies (Bruneel et al., 2010). As a result, the intensity of UIC may have diminishing marginal effects on the service innovativeness of university hospitals.
A frequently highlighted resistance to knowledge from external sources, known as the "not invented here" syndrome (R. Katz & Allen, 1982), may also lead to a reduced effect of UHIC on service innovation in university hospitals. According to this view, individuals generally have negative attitudes toward knowledge, ideas, or technologies from external sources that may affect their status quo at work (Burcharth et al., 2014). In particular, health professionals (e.g., physicians and nurses) may develop greater negative attitudes toward ideas and innovations from external sources if they feel dominated and perceive a threat to their professional role (Huynh et al., 2023). This may result from health professionals' identity as caretakers of their patients’ lives, which may lead them to rely more on their own expertise (Maccoby et al., 2013; McNeill, 2013). This mentality may foster the not-invented-here resistance, which is intensified by the increasing number of industry collaborations (Nissen et al., 2015). In this regard, Tartari and Breschi (2012) showed in a large survey of university researchers that the decision to collaborate with industry partners is crucially influenced by the perceived threat to the academic freedom of the researcher. As the number of industry collaborations increases, the perceived threat reinforces the overemphasis on external knowledge and ideas in the implementation of innovations. As a result, too many collaborations and a substantial amount of external knowledge mitigate the efficiency of UHIC and thus potential benefits on the innovation performance. As such, the influence of UHIC on service innovativeness may be nonlinear, reflecting decreasing marginal effects over the continuum of UHIC intensity:
Hypothesis 2b
The positive effect of university-hospital-industry collaborations on the service innovativeness of university hospitals will show a decreasing marginal effect.
3 Methodology
3.1 Data sources
The empirical approach to test the hypotheses is based on an unbalanced panel dataset, which combines three distinct data sources and comprises annual observations from 2011 until 2019 of 32 German university hospitals. As a first data source, this research processes structural hospital and medical department data (e.g., number of beds, number of physicians, disease and procedural case numbers) from publicly available hospital quality management reports. These report cards are part of the mandatory external quality monitoring system operated by the executive authority in the German healthcare system, the “Federal Joint Committee” (Gemeinsamer Bundesausschuss). As a second data source, regional district-level data on the population and the district’s gross domestic product (GDP) are used from the “Regionaldatenbank Deutschland – GENESIS” database, which is administered by the statistical office of North Rhine-Westphalia. And as a third data source, this study uses data from the WoS publication database in order to capture all research collaborations of the examined university hospitals with industry partners (i.e., UHIC) based on the co-authorship concept (for a similar approach, see Bozeman et al., 2013).
The dataset includes comprehensive information on all German university hospitals available for the period 2011—2019, with the exception of the privately owned "University Hospital Giessen and Marburg", which was excluded from the analysis to maintain the rigor of the study (Busse & Blümel, 2014). Thus, this study utilized a representative sample of all German university hospitals, which are crucial components of medical research and providers of maximum care, representing approximately 10% of all hospital beds in the country (Blümel et al., 2020).
3.2 Measurement
Service innovativeness as dependent variable. Based on service innovation literature (Greenhalgh et al., 2005; Lee et al., 2009; Schultz et al., 2012), a health provider’s service innovativeness is defined as its ability to implement a variety of new health services for patient treatment in a timely manner. Medical progress and changing demands force hospitals to regularly adapt their portfolio of medical services to be able to provide high quality health services (Eiriz et al., 2010; Greenhalgh et al., 2004; Trinh & Begun, 2019). In this study a university hospital’s service innovativeness (ServiceInno1) is therefore measured based on the share of patients that are treated with medical operational procedures that are newly implemented in the German health system in that particular year. In Germany, medical procedures are officially classified by the so-called “Operationen- und Prozedurenschlüssel” (OPS), which is the German classification system for operations, procedures, and general medical activities, based on the International Classification of Procedures in Medicine from the World Health Organization (Blümel et al., 2020). Newly implemented OPS codes are registered in annual, publicly accessible reports of the German Federal Institute for Drugs and Medical Devices. The new OPS codes were manually extracted from these reports for each year from 2012 to 2019. Only new OPS codes that represent genuinely new medical procedures were included in the analysis (e.g., OPS codes that were introduced as a result of splitting existing medical procedures into new subsidiary codes were excluded).
As a robustness check, this study applied a second measurement for the dependent variable (ServiceInno2). A university hospital’s service innovativeness is alternatively operationalized based on the share of patients that are treated with newly applied medical procedures in the focal university hospital in a particular year. By comparing the OPS codes reported annually by each university hospital with those from the previous year, newly applied medical procedures were identified for each considered university hospital. To meet the assumption of a normally distributed dependent variable, both service innovativeness measures are transformed using their natural logarithms.
UHIC intensity as independent variable. In this study, the UHIC intensity is operationalized as the share of industry publications relative to all scientific publications of a considered university hospital per year. A publication is defined as an industry publication if at least one company is listed as an author organization. All research collaborations were identified based on the publication data extracted from the WoS database according to the principle of co-authorship. Although the co-authorship is a partial indicator for all research collaboration, this concept is widely established and provides several advantages, including verifiability, stability over time, data availability, and ease of measurement (Bozeman et al., 2013; Chen et al., 2019; Katz, 1997). All relevant information about all industrial and non-industrial research partners (e.g., organization names and addresses) were also retrieved from the biometric data. Due to the fact that certain university hospitals use particular organizational names and abbreviations in their publications, a specific search string was created for each university hospital to identify all publications in the WoS database.
As robustness check, a second measurement for the independent variable was applied. The intensity of UHIC is also measured as the share of industrial partners relative to all partners in all published research (Share of industrial partners). This was done by counting the distinct number of companies listed in the authors’ address information. Special care was taken to ensure that a listed company was counted only once per publication. During the initial data analysis, it was frequently found that numerous companies were listed more than once in a publication, for example due to the naming of different departments, projects or due to data entry errors. In order to avoid double counting, the number of companies was recorded on the basis of the institute name, as this does not contain any additional information, such as the project name or the department notation. Addresses with the same company name but a different country addresses were considered as two different industrial partners.
Control variables. The empirical model includes other hospital characteristics and environmental variables that may affect an organization’s service innovativeness. To account for each university hospital's regional competitive pressure, the Herfindahl–Hirschman Index (HHI within 30 km radius) was measured based on a university hospital's share of patients relative to other hospitals within a 30 km radius (Möllenkamp et al., 2022). The number of beds (Total beds) is used to control for the size of the hospitals (Mutlu & Sürer, 2015; Rye & Kimberly, 2007). Considering the fact that the top management is responsible for (re-)allocating resources for innovation activities (Greenhalgh et al., 2004; Schultz et al., 2012), this study controls for potential changes in the university hospital’s senior management. The tested models differentiate between changes of the administrative (Δ AdminHead), medical (Δ MedicalHead), and care (Δ CareHead) leadership. These changes are measured respectively as binary dummy variables (0 = not new; 1 = new). Available physician supply in the hospitals is often emphasized as a potential factor in their innovation behavior (Labitzke et al., 2014; Schultz et al., 2012). To control for this, the number of physicians per 1000 cases (PhysPer1000cases) is included. In order to account the general effect of research collaborations, the number of all publications (Number of all publications) and mean number of research partners per publication with a one-year time lag (Mean number of research partners) were both included as controls (Greenhalgh et al., 2005). In addition, healthcare management literature increasingly highlights spatial knowledge spillovers which can determine the uptake of novel medical devices and service innovations (Hughes & Luft, 1991; Möllenkamp et al., 2022). The geographic proximity to neighboring hospitals, helps focal hospitals to evaluate and assess the relative advantage of new service innovations (Angst et al., 2010; Trinh et al., 2008). In this regard, all tested models control for the average service innovativeness of neighboring hospitals within a radius of 30 km (Neighbors’ service innovation 30 km radius). Finally, exogenous socioeconomic factors are also often considered to be determinants of organizations’ service innovativeness (Lee et al., 2009; Preker & Harding, 2003); and thus this model controls for the district’s GDP per capita in 2012 prices (GDP). Some of the regressors introduced (Beds and GDP) are measured in natural logarithms to account for unequal variation.
3.3 Statistical analysis
Given the underlying dataset consists of i = 1, 2, … N study units (i.e., university hospitals) and whose observed characteristics are available for t = 1, 2, …T at different time points (i.e., observation years), panel regression analysis is particularly suitable (Cameron & Trivedi, 2005). The standard linear panel regression equation is as follows:
The term \({y}_{it}\) represents the dependent variable, in this case the service innovativeness of the i-th university hospital at time t. \({x}_{it}\) represents all observable independent variables included in the model that may influence the dependent variable. While \(\ss\) represents the marginal effect of a specific independent variable, such as the UHIC intensity, on the dependent variable. Thus, it can be used to test Hypothesis 1 (if \(\ss\) > 0). The expression \({\alpha }_{i}\) includes all these unobserved time-constant factors that affect the dependent variable but were not included in the analysis. It accounts for individual heterogeneity of the i-th university hospital that does not change over time. Whereas \({u}_{it}\) is the collective term for unobserved factors (e.g., random shocks) that affect the dependent variable for the i-th university hospital at time t (Biørn, 2017).
Panel regression analysis is a powerful method for studying datasets with both temporal and cross-sectional dimensions. It allows for the inclusion of entity-specific effects and dynamic relationships over time, and enhances the researcher's capacity for causal inference and efficiency gains in statistical estimation (Bell & Jones, 2015; Biørn, 2017). Two common methods for analyzing panel datasets are the "fixed effect model" and the "random effect model". Both models differ with respect to the basic assumption that there is a correlation between the unobserved time-constant factors \({\alpha }_{i}\) and the observed explanatory variables \({x}_{it}\) (Aljandali & Tatahi, 2018). To determine whether to use a fixed or random effects model, a “Hausman Test” was performed, with the null hypothesis that the preferred model is random effects and the alternative is fixed effects (Hausman, 1978; Hsiao, 2022). The conducted Hausman Test indicated that the random effects model is the appropriate approach for the given panel dataset. The “Breusch–Pagan Lagrange Multiplier Test” was also performed to test for heteroskedasticity in a linear panel regression model and to further validate the suitability of the random effect model (Breusch & Pagan, 1980). In panel data analysis, heteroskedasticity (i.e., the variance of the error term is not constant across the observed university hospitals) can violate an underlying assumption of a linear regression model. This can lead to inefficient estimates and biased standard errors, which affects the validity of statistical conclusions (Biørn, 2017). The test statistic shown for all tested models p-values below an appropriate threshold (i.e., p < 0.05). Thus, the required assumption (i.e., homoskedasticity) can be assumed (Bell & Jones, 2015). This study applies common model selection quality criteria as the “Akaike Information Criterion” (AIC) and “Bayesian Information Criterion” (BIC) and the “Log-Likelihood Ratio Test” (LRT) to verify for significant differences in the fit between the different estimated models (Hsiao, 2022).
4 Results
4.1 Descriptive statistics
The examination of the descriptive statistics and correlations of the underlying variables revealed that most correlations among the explanatory variables have a moderate value (see Table 1). However, because this study controls for organization-specific effects in the random effects panel model, high correlations among the “raw” variables will not (inevitably) cause problems of multicollinearity in the estimation.
The results of the descriptive analysis of the past UHIC for the period 2011 to 2019 show that networking activities between university hospitals and industrial entities have grown significantly each year. As for instance, the average number of industry partners per university hospital grew from 90.22 in 2011 to 418.8 in 2019, an increase of 363.73%. The average number of all research partners per publication, regardless of industry or non-industry background, also shows an increase of 315.09% between 2011 and 2019. In addition to the increasingly dense network structures (larger research groups), the results show that university medical research in general has not only opened up its internal innovation processes more to industry, but has also formed research communities much more frequently overall (see Appendix Table 3).
4.2 Random effects panel regression results
Table 2 reports the results of the linear and quadratic effect for both innovation measures, ServiceInno1 and ServiceInno2. In order to take account of whether the size and statistical significance of any of the results might depend on the inclusion or exclusion of some of the variables from the regression, the independent variables were added step by step in the regression analysis. Parameter estimates for the year dummies (2012 to 2019) are not shown to economize on space. In Model (1) and (4), only the control variables are considered.
The results in Model (1) and (4) indicate that different control variables have a statistically significant effect on university hospitals’ service innovativeness, depending on how service innovativeness is measured. As such, the covariates GDP (ln), total number of beds, and HHI within 30 km radius (ln) have a positive significant influence on the service innovativeness measured as ServiceInno1. With ServiceInno2 as the dependent variable, the control variables Physicians Per 1000 cases and change of medical department heads show a positive effect on the service innovativeness of university hospitals.
When considering the LOGLIKE, AIC and BIC statistics, all tested models with the linear and quadratic UHIC effect obtain a higher model fit compared to the estimations of the basic model (Model (1) and (4)). These improvements are highly statistically significant (p < 0.01), as indicated by the conducted LRT.
The results of Model (2) and (5) show that UHIC intensity has a significant positive impact on the service innovativeness of university hospitals (Model (2), ß = 5.597, p < 0.01, Model (5), ß = 5.451, p < 0.01). Interestingly, both coefficients are quite similar and both are statistically significant at 1% level. The findings therefore support Hypothesis 1.
Finally, the estimation results in Model (3) and (6) show both a negative significant quadratic effect of UHIC (Model (3), ß = − 44.366, p < 0.05 and Model (6), ß = − 42.656, p < 0.05) and provide support for Hypothesis 2b. Thus, this observation suggests that industry collaborations have a positive effect on the innovativeness of university hospitals only up to a critical level. Beyond this critical value, the UHIC effect is reversed, implying that as the UHIC intensity (i.e., share of industry publications) increases, the service innovativeness of university hospitals decreases. In the following, the quadratic effect is analyzed and discussed in more detail.
4.3 Quadratic effect of industry collaboration on university hospitals’ service innovativeness
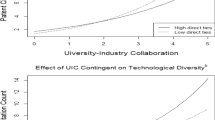
To further illustrate the marginal UHIC effect, the following Fig. 1 shows the marginal effect plot for both service innovativeness measures integrated with the histogram showing the frequency distribution of the independent variable (UHIC intensity). For a better interpretation of the results, the plotted values of both service innovativeness measures on the y-axis are the exposed (non-logarithmized) values. The upper plot depicts the negative marginal effect with ServiceInno1 as the dependent variable. Both plots show the decreasing marginal effect of UHIC and a similar trend.
With the innovation measure ServiceInno1, the calculated optimum is equal to 0.168 and with the variable ServiceInno2, the optimum of the marginal UHIC effect lies at 0.169. Both optimum values are very similar.
This suggests, for example, that if a university hospital exceeds the critical value of 16.83% in its share of industry collaborations, it can expect a negative, rather than a positive, effect of UIC on its service innovativeness. Looking at the given frequency distribution of UHIC, it becomes apparent that most of the university hospitals in the sample are below the estimated critical thresholds. Thus, it can be presumed that none of the considered university hospitals have observed negative effects on their innovation performance so far. It can also be assumed that university hospitals may be aware of the critical threshold and therefore manage their collaborations with industry in a targeted manner.
4.4 Robustness checks
All above presented random effect regression models were also conducted with share of industry partners (i.e., share of industry research partners in proportion to all research partners) as alternative independent variable. The results are consistent with the findings in case of the proposed positive linear UHIC effect and thus provide support for Hypothesis 1 (see Appendix 4 Model (8) and (11)). However, the results of this additional robustness check provide only partial support for Hypothesis 2b, as only a statistically significant decreasing marginal UHIC effect on the service innovativeness of university hospitals, measured as ServiceInno2, was found (Model (12); ß = − 561.958, p < 0.1). Considering these results, the critical threshold is estimated to be x = 0.039. In particular, this means that a university hospital with up to 3.91% industry partners in its collaboration portfolio can expect a positive UHIC effect on its service innovativeness, but after this threshold is exceeded, the UHIC effect will reverse. It should be noted, however, that these results should be treated with the highest degree of caution, as this study was only able to provide statistically significant results for this quadratic effect at the 10% significance level and for only one of the two service innovativeness measures.
To further bolster the study findings, all original models presented in Table 2 were also tested with alternative service innovativeness measures. As such, Alternative ServiceInno1 measures the percentage of OPS codes (instead of the number of treated patients) used by the focal university hospital that are newly implemented in the system. While Alternative ServiceInno2 represents the percentage of OPS codes that are new to the focal university hospital's service portfolio for each considered year. The results of the estimated random effect models provide also empirical support for Hypothesis 1 and thus, suggest that university hospitals likely are able to utilize the UHIC to improve their service innovativeness by implementing new medical procedures (see Appendix Table 5 Model (14) and (17)). Considering the log-likelihood, BIC and AIC statistics, the inclusion of the linear and quadratic UHIC effect improves the model fit in comparison to the basic model.
It was additionally examined whether the linear as well as the quadratic effect of UHIC could be found statistically significant without the proposed time lag of one year. However, the findings confirm that UHIC do not show a statistically significant effect on the service innovativeness of university hospitals without a respective time lag. Only when the ServiceInno2 measure is considered as the dependent variable, the robustness check reveals a weakly significant quadratic at the 10% significance level (see Appendix Table 6 Model (21); ß = − 49.643).
5 Discussion
5.1 Theoretical implications
The study provides empirical evidence on the relationship between UIC and service innovativeness from the perspective of university organizations. The research findings show that the intensity of UHIC has a positive impact on the service innovativeness of university hospitals. This suggests that university hospitals engaging in collaborations with industry partners are more likely to exhibit higher levels of service innovativeness. The study provides empirical evidence that such collaborations can positively influence innovation adoption in service-based organizations, expanding the understanding of innovation adoption beyond product-centric contexts. To the best of my knowledge, no other study has adopted so far, a similar, rigorous quantitative approach to empirically investigate the effect of UHIC and university hospitals’ service innovativeness. In doing so, the results of this study add valuable evidence to the existing literature on healthcare innovation and UIC by highlighting the relevance of a relatively new and often neglected form of cross-sector collaboration for the service innovativeness of university hospitals. The study utilizes panel data regression analysis with random effects, providing a robust methodological approach to analyze objective longitudinal data from 2011 to 2019. It also conducts a great set of robustness checks, strengthening the reliability of the research findings. Furthermore, the additional robustness check confirms the relevance of considering a time lag of the effect of industry collaborations on the service innovativeness of university hospitals. As the time lag is often neglected in empirical studies, the results of this study help to improve the understanding for future studies and enrich the sparse literature on university-industry knowledge transfer in the healthcare context. This study introduces also two alternative measures of service innovativeness following existing service innovation definition in literature (e.g., Lee et al., 2009; Schultz et al., 2012) and finds consistent results with the main analysis. This expands the understanding of service innovativeness and confirms the robustness of the findings. In addition, these measurement approaches can inspire the development of more precise and context-specific metrics for service innovation in further sectors.
Although no comparative studies are available, it can be claimed that the finding that industry collaborations have a positive effect on the innovation performance of academic organizations is consistent with the results of other recent studies. For example, the comprehensive literature review by Ankrah et al. (2013) shows that most of the studies in this area found consistent results that one of the main motivations of university actors to engage in UIC is to facilitate the implementation of innovation through knowledge/technology transfer. The findings of this study also complement existing evidence of recent research, as for example, the study of Tseng et al. (2020) which revealed that UIC positively impact universities’ technology innovation performance.
Moreover, this study also examined potential nonlinear effects of UHIC on service innovativeness. It was observed that the positive impact of UHIC on service innovativeness reaches a critical point, beyond which the UHIC effect becomes negative. In other words, while collaborations with industry partners initially lead to increased service innovativeness, excessively high levels of such industry collaborations may hinder or decrease the university hospitals' ability to introduce new medical services in their portfolio. By identifying this negative quadratic UHIC effect on service innovativeness, this research emphasizes the nuanced nature of UIC dynamics in healthcare. These finding challenges existing assumption of linear relationships and between UIC and innovation adoption in the healthcare context, emphasizing the need for more context-specific theories and research. Furthermore, it helps to reconcile conflicting views in UIC research on diminishing and/or increasing marginal effects of UIC. By doing so, this study sheds light on the underexplored area of cross-sectoral collaboration in healthcare and highlights the importance of considering both the positive and negative consequences of industry collaboration on innovation adoption from the perspective of university actors. This, in turn, can be incorporated into existing theories of UIC and innovation management.
5.2 Managerial implications
A large number of previous empirical studies (e.g., Jiang et al., 2006; Moreira et al., 2017; Zengul et al., 2018) have shown that the introduction of new medical services has a very high practical relevance for the performance of health service providers and thus for their long-term competitiveness. Thus, the study's findings can support evidence-based decision-making for university hospital managers, healthcare policymakers, and researchers seeking to improve the quality of healthcare services, patient outcomes, and the overall innovation ecosystem. For example, university hospital leaders should recognize the potential benefits of collaborating with industry partners to access knowledge, resources and technologies that can enhance the adoption of new medical services. In addition, university hospital managers should recognize the importance of organizational policies that support efficient knowledge transfer with cross-sectoral research partners. They should foster an environment that encourages the exchange of knowledge and expertise between academic and industry partners. Implementing practical measures, such as establishing research hubs for cross-sectoral teamwork, implementing key performance indicators to measure the impact of collaborative research, and creating clear policies on intellectual property issues, can create an environment for successful and mutually beneficial research collaborations between academic and industry actors. This, in turn, supports the implementation of innovative medical services in the operations of university hospitals, ultimately enhancing patient care.
At the same time, however, university hospital managers should be wary of the risks associated with too much collaboration with industry, which can lead to a decline in the university hospital's own capacity for innovativeness. University hospital managers and policymakers must strive to find a proper balance between collaboration and maintaining the hospital's internal capacity for its core practices. Thus, this research highlights the importance of a continuous monitoring and evaluation system to assess the impact of collaborations over time in order to maintain an optimal level of collaborations to avoid potential diminishing returns on internal innovation activities.
Policymakers should consider supporting and incentivizing strategic collaborations between universities, hospitals and industry, while also encouraging internal research and innovation initiatives within university hospitals. Policymakers can also support the effectiveness of UHIC by establishing policies that specify the goals, scope, and intensity of collaborations that are aligned with the innovation goals and strategic priorities of the actors involved.
6 Conclusion
In conclusion, this study has provided valuable insights into the relationship between UHIC and service innovativeness in German university hospitals. By analyzing objective panel data from 2011 to 2019 and employing robust regression models including a set of robustness checks, the study has demonstrated that UHIC has a significant positive impact on university hospitals’ service innovativeness. This finding emphasizes the importance of fostering collaborations between academia and industry in the healthcare sector to drive service innovation and improve patient care. Moreover, the study's exploration of the quadratic effect of UHIC on service innovativeness has revealed a critical point beyond which the positive impact diminishes and may even become negative. This nonlinear relationship underscores the need for thoughtful management of industry collaborations and highlights the potential risks of overburdening the coordination of industry partnerships.
As with any other research, this study has some limitations that provide avenues for future research. The investigation focused on German university hospitals, and thus the generalizability of the findings to other healthcare systems and settings requires further research.
This study examined a particular part of the overall innovation ecosystem in healthcare. The innovation ecosystem encompasses a broader network of organizations, stakeholders and factors that contribute to the innovation process. For example, it includes collaboration between industry partners, other academic institutions, regulatory bodies, and individual users, such as health professionals and patients, who influence or are influenced by the innovations introduced (Dedehayir et al., 2018; Kapoor & Lee, 2013; Schiavone, 2020). In this study, the number of all research publications and the average number of research partners were included as control variables to capture the potential role of collaborations with other relevant partners of university hospitals, such as other hospitals and academic medical intuitions. The results did not statistically prove that these factors have a significant impact on university hospitals’ service innovativeness. However, the role of collaboration mechanisms with other relevant stakeholders and users on the service innovativeness of university hospitals should be explored in broader future studies. This can inform not only the specific outcomes of collaborative research projects between different types of stakeholders, but also the implications for how to promote the diffusion of service innovations in the healthcare ecosystem.
Moreover, it is conceivable that further contextual factors may drive the relationship between UHIC and service innovativeness of university hospitals. In particular, UIC research often suggests that certain characteristics of the research collaboration itself, such as the degree of diversification of collaboration areas, may moderate the impact on innovation activities (e.g., Melnychuk et al., 2021; Wirsich et al., 2016). In this regard, a number of additional moderation analyses were conducted in this study, such as testing the UHIC diversification, measured as the number of different disciplines in university hospitals' publications with industry partners based on the “Web of Science Categories”, as a moderator variable for both service innovativeness measures. The analyses do not confirm any significant moderation effects. However, to further improve the understanding of the complex relationship between UHIC and service innovativeness of university hospitals, future research should focus more on the characteristics of research collaborations and their potential impact on innovation outcomes.
Although numerous studies have demonstrated the impact of service innovativeness on hospitals’ performance (e.g., Moreira et al., 2017; Zengul et al., 2018), future research should still investigate the effects of UHIC on different healthcare performance indicators, including patient satisfaction, cost-effectiveness, and clinical outcomes in university hospitals. Understanding how medical service innovations resulting from UHIC translate into improved patient care and health outcomes can provide crucial insights for healthcare policy and management. Unfortunately, the underlying dataset does not provide information to assess efforts to improve care efficiency and patient satisfaction.
In addition, it is important to note that the quantitative approach using bibliometric data in this study may not fully capture the depth and diversity of research collaborations between industry partners and university hospitals. This approach may miss valuable information such as informal interactions and knowledge sharing, discrete mistakes and failures during the collaboration. In this regard, complementing the rigorous quantitative analysis of this study with qualitative research methods, such as interviews and case studies, can provide a deeper understanding of the mechanisms and processes underlying successful UHIC, but also how health professionals and patients can benefit from UHIC and service innovations. This could provide practice-relevant insights into the expected benefits, as well as the factors that facilitate or hinder effective knowledge exchange and innovation between university hospitals and industry. In doing so, further qualitative research could also help to explore hidden mechanisms and factors (e.g., openness to change) that mediate the relationship between UHIC and service innovativeness.
Extending the research to include a cross-country comparative analysis of UHIC in different healthcare systems could offer insights into the role of contextual factors in shaping innovation outcomes. Comparing the findings across countries with varying healthcare policies and structures may reveal best practices and policy implications. Focusing on specific medical service innovations and their development through UHIC could provide a more targeted analysis of the impact of such cross-sectoral collaborations on different aspects of healthcare delivery. For example, exploring the adoption and implementation of telemedicine or digital health solutions through industry collaborations could be a valuable research direction.
References
Aljandali, A., & Tatahi, M. (2018). Panel data analysis. In A. Aljandali & M. Tatahi (Eds.), Statistics and econometrics for finance economic and financial modelling with eviews (pp. 237–260). Cham: Springer International Publishing.
Angst, C. M., Agarwal, R., Sambamurthy, V., & Kelley, K. (2010). Social contagion and information technology diffusion: The adoption of electronic medical records in U.S. Hospitals. Management Science, 56(8), 1219–1241. https://doi.org/10.1287/mnsc.1100.1183
Ankrah, S. N., Burgess, T. F., Grimshaw, P., & Shaw, N. E. (2013). Asking both university and industry actors about their engagement in knowledge transfer: What single-group studies of motives omit. Technovation, 33(2–3), 50–65. https://doi.org/10.1016/j.technovation.2012.11.001
Arundel, A., & Geuna, A. (2004). Proximity and the use of public science by innovative European firms. Economics of Innovation and New Technology, 13(6), 559–580. https://doi.org/10.1080/1043859092000234311
Azagra-Caro, J. M., Archontakis, F., Gutiérrez-Gracia, A., & Fernández-de-Lucio, I. (2006). Faculty support for the objectives of university–industry relations versus degree of R&D cooperation: The importance of regional absorptive capacity. Research Policy, 35(1), 37–55. https://doi.org/10.1016/j.respol.2005.08.007
Banal-Estañol, A., Jofre-Bonet, M., & Lawson, C. (2015). The double-edged sword of industry collaboration: Evidence from engineering academics in the UK. Research Policy, 44(6), 1160–1175. https://doi.org/10.1016/j.respol.2015.02.006
Barney, J. (1991). Firm Resources and Sustained Competitive Advantage. Journal of Management, 17(1), 99–120. https://doi.org/10.1177/014920639101700108
Belderbos, R., Carree, M., Lokshin, B., & Fernández Sastre, J. (2015). Inter-temporal patterns of R&D collaboration and innovative performance. The Journal of Technology Transfer, 40(1), 123–137. https://doi.org/10.1007/s10961-014-9332-4
Bell, A., & Jones, K. (2015). Explaining fixed effects: random effects modeling of time-series cross-sectional and panel data. Political Science Research and Methods, 3(1), 133–153. https://doi.org/10.1017/psrm.2014.7
Biørn, E. (2017). Econometrics of panel data: Methods and applications (1st ed.). Oxford: Oxford University Press.
Blümel, M., Spranger, A., Achstetter, K., Maresso, A., & Busse, R. (2020). Germany: Health system review. Health Systems in Transition, 22(6), 1–272.
Bozeman, B., Fay, D., & Slade, C. P. (2013). Research collaboration in universities and academic entrepreneurship: The-state-of-the-art. The Journal of Technology Transfer, 38(1), 1–67. https://doi.org/10.1007/s10961-012-9281-8
Breusch, T. S., & Pagan, A. R. (1980). The Lagrange Multiplier Test and its Applications to Model Specification in Econometrics. The Review of Economic Studies, 47(1), 239. https://doi.org/10.2307/2297111
Bruneel, J., D’Este, P., & Salter, A. (2010). Investigating the factors that diminish the barriers to university–industry collaboration. Research Policy, 39(7), 858–868. https://doi.org/10.1016/j.respol.2010.03.006
Busse, R., & Blümel, M. (2014). Germany: Health system review. Health Systems in Transition, 16(2), 1–296.
Busse, R., Geissler, A., Aaviksoo, A., Cots, F., Häkkinen, U., Kobel, C., Mateus, C., Or, Z., O’Reilly, J., Serdén, L., Street, A., Tan, S. S., & Quentin, W. (2013). Diagnosis related groups in Europe: Moving towards transparency, efficiency, and quality in hospitals? British Medical Journal, 346, f3197. https://doi.org/10.1136/bmj.f3197
Cameron, A. C., & Trivedi, P. K. (2005). Microeconometrics: Methods and applications. Cambridge: Cambridge University Press.
Chatterji, A. K., Fabrizio, K. R., Mitchell, W., & Schulman, K. A. (2008). Physician-industry cooperation in the medical device industry. Health Affairs (project Hope), 27(6), 1532–1543. https://doi.org/10.1377/hlthaff.27.6.1532
Chen, K., Zhang, Y., & Fu, X. (2019). International research collaboration: An emerging domain of innovation studies? Research Policy, 48(1), 149–168. https://doi.org/10.1016/j.respol.2018.08.005
Cheng, H., Zhang, Z., Huang, Q., & Liao, Z. (2020). The effect of university–industry collaboration policy on universities’ knowledge innovation and achievements transformation: Based on innovation chain. The Journal of Technology Transfer, 45(2), 522–543. https://doi.org/10.1007/s10961-018-9653-9
Colyvas, J., Crow, M., Gelijns, A., Mazzoleni, R., Nelson, R. R., Rosenberg, N., & Sampat, B. N. (2002). How do university inventions get into practice? Management Science, 48(1), 61–72. https://doi.org/10.1287/mnsc.48.1.61.14272
Cooper, R., Edgett, S. J., & Kleinschmidt, E. J. (1999). New product portfolio management: Practices and performance. Journal of Product Innovation Management, 16(4), 333–351. https://doi.org/10.1016/S0737-6782(99)00005-3
D’Este, P., & Patel, P. (2007). University–industry linkages in the UK: What are the factors underlying the variety of interactions with industry? Research Policy, 36(9), 1295–1313. https://doi.org/10.1016/j.respol.2007.05.002
D’Este, P., & Perkmann, M. (2011). Why do academics engage with industry? The entrepreneurial university and individual motivations. The Journal of Technology Transfer, 36(3), 316–339. https://doi.org/10.1007/s10961-010-9153-z
de Araújo Burcharth, A. L., Knudsen, M. P., & Søndergaard, H. A. (2014). Neither invented nor shared here: The impact and management of attitudes for the adoption of open innovation practices. Technovation, 34(3), 149–161. https://doi.org/10.1016/j.technovation.2013.11.007
de Wit-de Vries, E., Dolfsma, W. A., van der Windt, H. J., & Gerkema, M. P. (2019). Knowledge transfer in university–industry research partnerships: A review. The Journal of Technology Transfer, 44(4), 1236–1255. https://doi.org/10.1007/s10961-018-9660-x
Dedehayir, O., Mäkinen, S. J., & Roland Ortt, J. (2018). Roles during innovation ecosystem genesis: A literature review. Technological Forecasting and Social Change, 136, 18–29. https://doi.org/10.1016/j.techfore.2016.11.028
Dhainaut, J.-F., Blin, O., Herry, F., Benito, S., Bilbault, P., Cauterman, M., Favrel-Feuillade, F., Fazi-Leblanc, S., Germain, C., Goehrs, C., Grosskopf, C., Labarthe, B., Lechat, P., Malciu, C., Marquet, P., Miceli-Richard, C., Peyret, O., Rattenbach, R., & de Saint-Exupéry, E. (2020). Health research and innovation: Can we optimize the interface between startups/pharmaceutical companies and academic health care institutions or not? Theriogenology, 75(1), 113–123. https://doi.org/10.1016/j.therap.2019.11.010
Dias, C., & Escoval, A. (2015). Hospitals as learning organizations: Fostering innovation through interactive learning. Quality Management in Health Care, 24(1), 52–59. https://doi.org/10.1097/QMH.0000000000000046
Duysters, G., & Lokshin, B. (2011). Determinants of alliance portfolio complexity and its effect on innovative performance of companies. Journal of Product Innovation Management, 28(4), 570–585. https://doi.org/10.1111/j.1540-5885.2011.00824.x
Eiriz, V., Barbosa, N., & Figueiredo, J. (2010). A conceptual framework to analyse hospital competitiveness. The Service Industries Journal, 30(3), 437–448. https://doi.org/10.1080/02642060802236137
Enkel, E., Gassmann, O., & Chesbrough, H. (2009). Open R&D and open innovation: Exploring the phenomenon. R&D Management, 39(4), 311–316. https://doi.org/10.1111/j.1467-9310.2009.00570.x
Faems, D., de Visser, M., Andries, P., & van Looy, B. (2010). Technology alliance portfolios and financial performance: Value-enhancing and cost-increasing effects of open innovation. Journal of Product Innovation Management, 27(6), 785–796. https://doi.org/10.1111/j.1540-5885.2010.00752.x
Fischer, B. B., Schaeffer, P. R., Vonortas, N. S., & Queiroz, S. (2018). Quality comes first: University-industry collaboration as a source of academic entrepreneurship in a developing country. The Journal of Technology Transfer, 43(2), 263–284. https://doi.org/10.1007/s10961-017-9568-x
George, G., Zahra, S. A., & Wood, D. (2002). The effects of business–university alliances on innovative output and financial performance: A study of publicly traded biotechnology companies. Journal of Business Venturing, 17(6), 577–609. https://doi.org/10.1016/S0883-9026(01)00069-6
Greenhalgh, T., Robert, G., Bate, P., Macfarlane, F., & Kyriakidou, O. (2005). Diffusion of innovations in health service organisations. Blackwell Publishing Ltd. https://doi.org/10.1002/9780470987407
Greenhalgh, T., Robert, G., Macfarlane, F., Bate, P., & Kyriakidou, O. (2004). Diffusion of innovations in service organizations: Systematic review and recommendations. The Milbank Quarterly, 82(4), 581–629. https://doi.org/10.1111/j.0887-378X.2004.00325.x
Gretsch, O., Salzmann, E. C., & Kock, A. (2019). University-industry collaboration and front-end success: The moderating effects of innovativeness and parallel cross-firm collaboration. R&D Management, 49(5), 835–849. https://doi.org/10.1111/radm.12385
Gulbrandsen, M., & Smeby, J.-C. (2005). Industry funding and university professors’ research performance. Research Policy, 34(6), 932–950. https://doi.org/10.1016/j.respol.2005.05.004
Hausman, J. A. (1978). Specification Tests in Econometrics. Econometrica, 46(6), 1251–1271. https://doi.org/10.2307/1913827
Häussler, B., Isenberg, T., & Klusen, N. (2010). Ökonomie Jahrbuch der medizinischen Innovationen: Band 6: Innovation und Gerechtigkeit (A. Penk, Ed.). Schattauer GmbH Verlag für Medizin und Naturwissenschaften.
Hee, O. C., Hui, O. K., Rizal, A. M., Kowang, T. O., & Fei, G. C. (2018). Determinants of innovative performance in the service industry: A review. International Journal of Academic Research in Business and Social Sciences. https://doi.org/10.6007/IJARBSS/v8-i6/4229
Heyder, R. (2015). Die Bedeutung der Universitätskliniken in der regionalen und überregionalen Versorgung. In Schwerpunkt: Strukturwandel. Schattauer, 2015.
Hinkelmann, J., Hasebrook, J. P., Volkert, T., & Hahnenkamp, K. (2017). Growing pains at hospitals: Opportunities and issues of service expansion in maximum care. Frontiers in Medicine. https://doi.org/10.3389/fmed.2017.00090
Hsiao, C. (2022). Analysis of panel data. Cambridge University Press, Cambridge: Econometric Society monographs series.
Hughes, R. G., & Luft, H. S. (1991). Service patterns in local hospital markets: Complementarity or medical arms race? Health Services Management Research, 4(2), 131–139. https://doi.org/10.1177/095148489100400206
Huynh, T., Kroh, J., & Schultz, C. (2023). Overcoming the not-invented-here syndrome in healthcare: The case of German ambulatory physiotherapists’ adoption of digital health innovations. PLoS ONE, 18(12), e0293550. https://doi.org/10.1371/journal.pone.0293550
Jiang, H. J., Friedman, B., & Begun, J. W. (2006). Sustaining and improving hospital performance: The effects of organizational and market factors. Health Care Management Review, 31(3), 188–196. https://doi.org/10.1097/00004010-200607000-00004
Kapoor, R., & Lee, J. M. (2013). Coordinating and competing in ecosystems: How organizational forms shape new technology investments. Strategic Management Journal, 34(3), 274–296. https://doi.org/10.1002/smj.2010
Katz, J. S. (1997). What is research collaboration? Research Policy, 26(1), 1–18. https://doi.org/10.1016/S0048-7333(96)00917-1
Katz, R., & Allen, T. J. (1982). Investigating the not invented here (NIH) syndrome: A look at the performance, tenure, and communication patterns of 50 R&D Project Groups. R&D Management, 12(1), 7–20. https://doi.org/10.1111/j.1467-9310.1982.tb00478.x
Kennedy, M. T., & Fiss, P. C. (2009). Institutionalization, framing, and diffusion: The logic of TQM adoption and implementation decisions among U.S. hospitals. Academy of Management Journal, 52(5), 897–918. https://doi.org/10.5465/AMJ.2009.44633062
Kesting, T. (2013). Wissens- und Technologietransfer durch Hochschulen aus einer marktorientierten Perspektive: Ansatzpunkte zur Gestaltung erfolgreicher Transferprozesse an Universitäten und Fachhochschulen. Springer Gabler. https://doi.org/10.1007/978-3-658-00719-5
Kobarg, S., Stumpf-Wollersheim, J., & Welpe, I. M. (2018). University-industry collaborations and product innovation performance: The moderating effects of absorptive capacity and innovation competencies. The Journal of Technology Transfer, 43(6), 1696–1724. https://doi.org/10.1007/s10961-017-9583-y
Kock, A., Gemünden, H. G., Salomo, S., & Schultz, C. (2011). The mixed blessings of technological innovativeness for the commercial success of new products. Journal of Product Innovation Management, 28(s1), 28–43. https://doi.org/10.1111/j.1540-5885.2011.00859.x
Labitzke, G., Svoboda, S., & Schultz, C. (2014). The role of dedicated innovation functions for innovation process control and performance: An empirical study among hospitals. Creativity and Innovation Management, 23(3), 235–251. https://doi.org/10.1111/caim.12068
Lang, H. (2013). Forschungskooperationen zwischen Universitäten und Industrie. Springer Fachmedien Wiesbaden. https://doi.org/10.1007/978-3-658-02759-9
Laubach, W., & Fischbeck, S. (2007). Job satisfaction and the work situation of physicians: A survey at a German university hospital. International Journal of Public Health, 52(1), 54–59. https://doi.org/10.1007/s00038-006-5021-x
Lee, R. P., Ginn, G. O., & Naylor, G. (2009). The impact of network and environmental factors on service innovativeness. Journal of Services Marketing, 23(6), 397–406. https://doi.org/10.1108/08876040910988183
Lehoux, P., Roncarolo, F., Rocha Oliveira, R., & Pacifico Silva, H. (2016). Medical innovation and the sustainability of health systems: A historical perspective on technological change in health. Health Services Management Research, 29(4), 115–123. https://doi.org/10.1177/0951484816670192
Lester, R. K., & Sotarauta, M. (2007). Innovation, universities, and the competitiveness of regions editors: Richard K. Lester and Markku Sotarauta. Technology review: Vol. 214. Tekes.
Lin, J.-Y. (2017). Balancing industry collaboration and academic innovation: The contingent role of collaboration-specific attributes. Technological Forecasting and Social Change, 123, 216–228. https://doi.org/10.1016/j.techfore.2016.03.016
Maccoby, M., Norman, C. L., Norman, C. J., & Margolies, R. (2013). Transforming health care leadership: A systems guide to improve patient care, decrease costs, and improve population health. Wiley.
McNeill, D. (2013). A framework for applying analytics in healthcare: What can be learned from the best practices in retail, banking, politics, and sports. Pearson.
Melnychuk, T., Schultz, C., & Wirsich, A. (2021). The effects of university–industry collaboration in preclinical research on pharmaceutical firms’ R&D performance: Absorptive capacity’s role. Journal of Product Innovation Management, 38(3), 355–378. https://doi.org/10.1111/jpim.12572
Möllenkamp, M., Pongiglione, B., Rabbe, S., Torbica, A., & Schreyögg, J. (2022). Spillover effects and other determinants of medical device uptake in the presence of a medical guideline: An analysis of drug-eluting stents in Germany and Italy. Health Economics, 31(1), 157–178. https://doi.org/10.1002/hec.4587
Moreira, M. R. A., Gherman, M., & Sousa, P. S. A. (2017). Does innovation influence the performance of healthcare organizations? Innovation, 19(3), 335–352. https://doi.org/10.1080/14479338.2017.1293489
Mueller, P. (2006). Exploring the knowledge filter: How entrepreneurship and university–industry relationships drive economic growth. Research Policy, 35(10), 1499–1508. https://doi.org/10.1016/j.respol.2006.09.023
Muscio, A. (2010). What drives the university use of technology transfer offices? Evidence from Italy. The Journal of Technology Transfer, 35(2), 181–202. https://doi.org/10.1007/s10961-009-9121-7
Muscio, A., & Pozzali, A. (2013). The effects of cognitive distance in university-industry collaborations: Some evidence from Italian universities. The Journal of Technology Transfer, 38(4), 486–508. https://doi.org/10.1007/s10961-012-9262-y
Mutlu, H. M., & Sürer, A. (2015). Effects of market, E-marketing, and technology orientations on innovativeness and performance in Turkish health organizations. Health Marketing Quarterly, 32(4), 313–329. https://doi.org/10.1080/07359683.2015.1093879
Nissen, H. A., Evald, M. R., & Clarke, A. H. (2015). Firms’ reshaping of commercialization practices to overcome the ‘not invented here’ phenomenon in public healthcare organizations. The Innovation Journal, 20(3), 1–27.
Ortiz, A. (2013). Kooperation zwischen Unternehmen und Universitäten. Springer Fachmedien Wiesbaden. https://doi.org/10.1007/978-3-8349-3644-8
Peteraf, M. A. (1993). The cornerstones of competitive advantage: A resource-based view. Strategic Management Journal, 14(3), 179–191. https://doi.org/10.1002/smj.4250140303
Ponds, R., Oort, F. V., & Frenken, K. (2010). Innovation, spillovers and university-industry collaboration: an extended knowledge production function approach. Journal of Economic Geography, 10(2), 231–255. https://doi.org/10.1093/jeg/lbp036
Preker, A. S., & Harding, A. (2003). Innovations in health service delivery. The World Bank. https://doi.org/10.1596/0-8213-4494-3
Rajalo, S., & Vadi, M. (2017). University-industry innovation collaboration: Reconceptualization. Technovation, 62–63, 42–54. https://doi.org/10.1016/j.technovation.2017.04.003
Rye, C. B., & Kimberly, J. R. (2007). The adoption of innovations by provider organizations in health care. Medical Care Research and Review, 64(3), 235–278. https://doi.org/10.1177/1077558707299865
Salge, T. O., & Vera, A. (2009). Hospital innovativeness and organizational performance: Evidence from English public acute care. Health Care Management Review, 34(1), 54–67. https://doi.org/10.1097/01.HMR.0000342978.84307.80
Savva, N., Debo, L., & Shumsky, R. A. (2023). Hospital reimbursement in the presence of cherry picking and upcoding. Management Science, 69(11), 6777–6799. https://doi.org/10.1287/mnsc.2023.4752
Schiavone, F. (2020). User innovation in healthcare. Springer Nature. https://doi.org/10.1007/978-3-030-44256-9
Schultz, C., Zippel-Schultz, B., & Salomo, S. (2011). Innovationen im Krankenhaus sind machbar! Innovationsmanagement als Erfolgsfaktor (1st ed.). Management von Innovationen im Gesundheitswesen. Kohlhammer.
Schultz, C., Gretsch, O., & Kock, A. (2021). The influence of shared R&D-project innovativeness perceptions on university-industry collaboration performance. The Journal of Technology Transfer, 46(4), 1144–1172. https://doi.org/10.1007/s10961-020-09818-1
Schultz, C., Zippel-Schultz, B., & Salomo, S. (2012). Hospital innovation portfolios: Key determinants of size and innovativeness. Health Care Management Review, 37(2), 132–143. https://doi.org/10.1097/HMR.0b013e31822aa41e
Sturm, H., Rieger, M. A., Martus, P., Ueding, E., Wagner, A., Holderried, M., & Maschmann, J. (2019). Do perceived working conditions and patient safety culture correlate with objective workload and patient outcomes: A cross-sectional explorative study from a German university hospital. PLoS ONE, 14(1), e0209487. https://doi.org/10.1371/journal.pone.0209487
Tartari, V., & Breschi, S. (2012). Set them free: Scientists’ evaluations of the benefits and costs of university-industry research collaboration. Industrial and Corporate Change, 21(5), 1117–1147. https://doi.org/10.1093/icc/dts004
Thune, T. (2007). University–industry collaboration: The network embeddedness approach. Science and Public Policy, 34(3), 158–168. https://doi.org/10.3152/030234207X206902
Tian, M., Su, Y., & Yang, Z. (2022). University-industry collaboration and firm innovation: An empirical study of the biopharmaceutical industry. The Journal of Technology Transfer, 47(5), 1488–1505. https://doi.org/10.1007/s10961-021-09877-y
Töpfer, A., & Albrecht, D. M. (2017). Konsequenzen für das strategische und operative Management von Kliniken bei sich verändernden und verschärfenden Rahmenbedingungen. In Handbuch Changemanagement im Krankenhaus. Springer
Trinh, H. Q., & Begun, J. W. (2019). Strategic differentiation of high-tech services in local hospital markets. Inquiry A Journal of Medical Care Organization, Provision and Financing,. https://doi.org/10.1177/0046958019882591
Trinh, H. Q., Begun, J. W., & Luke, R. D. (2008). Hospital service duplication: Evidence on the medical arms race. Health Care Management Review, 33(3), 192–202. https://doi.org/10.1097/01.HMR.0000324903.19272.0c
Tseng, F.-C., Huang, M.-H., & Chen, D.-Z. (2020). Factors of university–industry collaboration affecting university innovation performance. The Journal of Technology Transfer, 45(2), 560–577. https://doi.org/10.1007/s10961-018-9656-6
Tsuruya, N., Kawashima, T., Shiozuka, M., Nakanishi, Y., & Sugiyama, D. (2018). Academia-industry cooperation in the medical field: Matching opportunities in Japan. Clinical Therapeutics, 40(11), 1807–1812. https://doi.org/10.1016/j.clinthera.2018.10.010
van Rijnsoever, F. J., Hessels, L. K., & Vandeberg, R. L. (2008). A resource-based view on the interactions of university researchers. Research Policy, 37(8), 1255–1266. https://doi.org/10.1016/j.respol.2008.04.020
Weigel, S. (2011). Medical technology’s source of innovation. European Planning Studies, 19(1), 43–61. https://doi.org/10.1080/09654313.2011.530391
Wirsich, A., Kock, A., Strumann, C., & Schultz, C. (2016). Effects of university-industry collaboration on technological newness of firms. Journal of Product Innovation Management, 33(6), 708–725. https://doi.org/10.1111/jpim.12342
Wu, I.-L., & Hsieh, P.-J. (2011). Understanding hospital innovation enabled customer-perceived quality of structure, process, and outcome care. Total Quality Management & Business Excellence, 22(2), 227–241. https://doi.org/10.1080/14783363.2010.532343
Zengul, F. D., Weech-Maldonado, R., Ozaydin, B., Patrician, P. A., & O’Connor, S. J. (2018). Longitudinal analysis of high-technology medical services and hospital financial performance. Health Care Management Review, 43(1), 2–11. https://doi.org/10.1097/HMR.0000000000000124
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables
3,
4,
5 and
6.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huynh, T. Collaborative research in healthcare: uncovering the impact of industry collaboration on the service innovativeness of university hospitals. J Technol Transf (2024). https://doi.org/10.1007/s10961-024-10083-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10961-024-10083-9
Keywords
- University hospital
- University-industry collaboration
- Service innovativeness
- Research collaboration
- Knowledge transfer