Abstract
Despite concerted efforts to enforce smoke-free laws in various countries, nonsmokers, particularly women and children, continue to be exposed to daily secondhand smoke (SHS), resulting in significant health risks. While existing studies have assessed the health effects of numerous diseases, the quantification of SHS spillovers remains understudied. This research employs choice experiments and contingent valuation techniques to rigorously quantify the attributes of SHS health risks, with a specific emphasis on facilitating cross-country comparisons. Our investigation reveals that nonsmoking individuals in the United Kingdom exhibit an attitude of indifference towards a proposed policy offering increased disposable income as compensation for SHS exposure. Conversely, nonsmoking Americans express a contrary perspective. Furthermore, our study demonstrates that nonsmoking Americans attribute a higher value to SHS health risks compared to their British counterparts. Consequently, this research uncovers a hitherto unexplored dimension of health risk-related behaviors. These findings hold the potential to significantly contribute to the development of future smoke-free policies, offering valuable insights that can inform policy decisions and address the persistent challenges associated with SHS exposure, particularly among vulnerable populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A few countries have enacted various smoke-free laws to protect nonsmokers from exposure to secondhand smoke (SHS). Governments increase tobacco taxes to raise cigarette prices and ultimately discourage smoking. However, tobacco companies counteract this through price discounts. Such laws are helpful but do not eliminate SHS, leaving many nonsmokers at risk in some public and private places (van der Eijk & Porter, 2015). Restricting smoking in some public venues increases smoking in private places as smokers try to make up for the loss of certain outdoor smoking (Agee et al., 2001; WHO, 2023). Studies have shown that indoor exposure to SHS increased in recent years (Ciaccio et al., 2014; de Hollander and Melse, 2006; Yang et al., 2021), especially during COVID-19 lockdown (ASH, 2020; Yach, 2020).
One common feature of smoke-free laws in many countries is that they do not protect nonsmokers in private homes and other public places such as bus stops, building entrances, often-crowded city centers, and other outlets. There is also smoke drift from one apartment to another, especially in multi-unit housing (CDC, 2021b, 2021c). Thus, smoke-free laws are far from fulfilling Article 8 of the WHO Framework Convention on Tobacco Control (WHO, 2013, 2023).
The WHO promotes a smoke-free world because no level of exposure is safe, and using designated areas for smoking and other measures have not been effective in achieving clean air (WHO, 2013). Globally, about one in two children breathes in SHS, and 65,000 die as a result. In total, 1.2 million nonsmokers die prematurely each year (WHO, 2020). In addition, recent evidence shows that children exposed to SHS are vulnerable to sudden infant death syndrome, middle ear disease, and asthma. Also, adults exposed to SHS have a 20–30% risk of suffering stroke, lung cancer (20–30%), and coronary heart disease (25–30%) (CDC, 2020). Emotional distress has also been reported among those exposed to SHS (Bandiera, Richardson, Lee, He and Merikangas, 2011). Furthermore, it is worth noting that exposure to SHS increases the risk for COVID-19 infection (Mendez, Escobar, Encinas and Wojcicki, 2021) and other infectious diseases (Jiang et al., 2020; The Cancer Council, 2019).
Based on the smoking prevalence in the U.S. and U.K., approximately 23% of Americans aged 15 years and above are tobacco users, with 28% of males and 18% of females engaging in tobacco consumption (World Bank, 2023). Consequently, SHS exposure is responsible for over 41,000 deaths among nonsmokers annually. Among these fatalities, approximately 34,000 are attributed to heart disease, 8000 to stroke, and 7300 to lung cancer (CDC, 2021a). These figures underscore the profound health risks nonsmokers face due to SHS exposure and emphasize the urgent need for effective interventions to mitigate its adverse consequences.
In comparison, 15.4% of British aged 15 years and over use tobacco—17% of males and 14% of females (World Bank, 2023). Exposure to SHS accounts for more than 300,000 General Practice (GP) consultations annually with children, about 9,500 are admitted to hospitals, and 40 cot deaths are recorded (SFF, n.d.). In addition, SHS is responsible for around 10,700 deaths among nonsmokers each year (ASH, 2020).
While scientific evidence shows that SHS has enormous health risks, it is unclear how nonsmokers perceive and value these risks. Stated preference methods such as contingent valuation (Andersson et al., 2015; Hammitt & Haninger, 2010; Hollinghurst et al., 2016; Tubeuf et al., 2015), and choice experiments (Adamowicz et al., 2011; Gerard et al., 2003; Hole, 2008; Huang et al., 2018; Johnson et al., 2000) are widely used to value health risks where there is a lack of market data. These techniques involve creating a hypothetical market in which respondents make choices that involve trade-offs between health risks and a certain payoff (Andersson et al., 2019).
However, critical issues need to be considered in valuing spillovers such as SHS. These issues involve deciding whether to elicit willingness to pay (WTP) or willingness to accept (WTA). The choice depends on two factors: (1) the nature of the good and (2) property rights (Carson et al., 2001; Hammitt, 2002; Knetsch, 2007; Kim et al., 2015; Whittington et al., 2017).
Thus, when an individual has the right to a welfare improvement and yet does not obtain it, WTA is appropriate. On the other hand, the individual is expected to pay for the improvement if they are not entitled, in which case, WTP is elicited. The implication is that an individual who has the right to produce negative externalities should be incentivized if the government wants to curtail such activities.
Against this background, valuing SHS health risks is not straightforward because nonsmokers are entitled to clean air free from tobacco smoke (UNEP, 2019a, 2019b; WHO, 2005). At the same time, smokers have the right to smoke in non-smoke-free zones whether or not a nonsmoker is present. This study is the first to give insight into nonsmokers’ perceptions about SHS and quantify its welfare impacts, including the psychological aspect. As a result, it would give policymakers more insight into peoples’ views on this issue and contribute to smoke-free legislation.
The selection of the United States (U.S.) and the United Kingdom (U.K.) as our study focus is based on the intrinsic dissimilarity between their healthcare systems. While the U.S. operates a private healthcare system, the U.K. adopts a publicly-funded approach. This divergence prompts us to investigate how nonsmokers from these two countries value the health risks associated with secondhand smoke differently, drawing on insights from the theory of social preferences and social capital.
The theory of social preferences posits that individuals are not solely driven by self-interest but also exhibit concern for the welfare of others. Consequently, decision-making may extend beyond individual benefits to encompass collective well-being. Social capital, on the other hand, encapsulates the value derived from the interconnected networks of relationships among members of a given society, which fosters effective societal functioning. It comprises robust interpersonal ties, shared identities, mutual understanding, norms, values, trust, cooperation, and reciprocity (Charness & Rabin, 2002; Martikke, 2017; Portes, 1998).
In light of these conceptual frameworks, we posit that the U.S. nonsmokers, accustomed to a privately funded or out-of-pocket medical services system, may exhibit a higher valuation of secondhand smoke health risks compared to their British counterparts, who experience a publicly-funded healthcare system. The difference in healthcare financing mechanisms could influence individuals’ risk perception and response patterns, shaping their willingness to pay to prevent exposure and/or willingness to accept compensation.
In the context of the U.S. private healthcare system, where individuals bear a more direct financial responsibility for their medical expenses, the notion of social preferences may take a back seat, potentially leading to a stronger emphasis on personal well-being. In contrast, the U.K.’s publicly-funded healthcare system may foster a sense of shared responsibility and mutual support.
It is imperative to acknowledge that this argument constitutes a theoretical framework and requires empirical investigation to substantiate the actual differences in how American and British nonsmokers value secondhand smoke health risks. Nevertheless, the exploration of such disparities has the potential to enhance our understanding of the intricate interplay between healthcare system structures, social dynamics, and risk valuation among nonsmokers in these two nations. By shedding light on these aspects, our study endeavors to contribute valuable insights to public health policy formulation, encouraging tailored interventions that address the specific needs and behaviors of nonsmokers in each context.
Literature Review
Although there are no studies directly related to ours, a handful of studies have used stated preference (SP) techniques to elicit willingness to pay to reduce health risks or undergo a diagnostic test. We review these studies to give insights into the types of health-related diseases researchers have evaluated. The WTP values reported in the literature differ significantly depending on the elicitation format and period of study (affected by inflation and exchange rate) and the type of healthcare system practiced in the place of study. Thus, readers should be cautious in comparing WTP values. Furthermore, while some reported median, others presented mean WTP, which is usually greater than the median value due to outliers.
For example, O’Brien and Viramontes (1994) used contingent valuation (CV) to elicit WTP for a possible 99% chance of preventing chronic lung disease and a 1% likelihood of death in Canada. The participants were willing to pay CAN$113 per month to avoid the disease, while Johnson et al. (2000) applied choice experiments (CE) to value the attributes of respiratory and cardiovascular diseases, such as activity restriction, episode duration, and symptom. The estimated marginal WTP ranged from CAN$100 to CAN$225. Similarly, Krupnick et al. (2002) elicited willingness to pay for a reduction in mortality risk. The mean WTP was CAN$417, and the value for a statistical life (VSL) was CAN$1.2–$3.8 million. Adamowicz et al. (2011) applied CV and CE to value reductions in cancer and microbial diseases from drinking water. The attributes were microbial illness and death, cancer illness and death. The marginal WTP for fewer microbial and cancer deaths were CAN$12.61 and CAN$10.43, whereas the marginal WTP for reductions in cancer morbidity and microbial morbidity risks were CAN$2.43 and CAN$0.02. However, CV results show that the mean WTP for reductions in both risks was CAN$294. The VSLs for microbial and cancer deaths were CAN$16-$20 million and CAN$14–$17 million, respectively.
Arana and León (2006) estimated the WTP to reduce the risk of an episode of respiratory disease in Spain. The participants’ WTP was €41.70. Hammitt and Haninger (2010) estimated WTP to reduce fatal diseases and trauma such as cancer and other chronic diseases to children and adults. The VSL for children was $12–$15 million and US$6–$10 million for adults. Similarly, Andersson et al. (2015) studied Swedish respondents’ willingness to pay to reduce foodborne morbidity risks. The WTP was US$14,000-$17,700, and the VSL in a split-sample were US$710 million and US$695 million (Andersson,Hole and Svensson, 2016).
A few studies focus on China’s air quality, such as Hammitt and Zhou (2006), who estimated air pollution’s health risks such as cold, chronic bronchitis, and fatality. The median WTP was between US$3 and US$6 to prevent the risk of catching a cold, and US$500–$1000 for chronic bronchitis. The VSL was US$4000–$17,000. This is small because the authors used the median value instead of the mean, which is about thirteen times higher. Also, this result is about 10–1000 times smaller than the US’s and Taiwan’s at the exchange rate during the study. Likewise, Guo et al. (2006) investigated a similar problem (reduction in the risks of asthma and mortality) by considering three scenarios: when the policy aimed at reducing health risks is publicly or privately provided; how WTP changes with a change in the magnitude of the health risk; and the degree of sensitiveness of the WTP in the first scenario. The estimated median WTP for a reduction in asthma was US$1,711.
However, in an earlier study, Peng and Tian (2003) reported US$2717 as the WTP for reducing the risk of asthma. Huang et al. (2018) quantified the attributes of air pollution health risks, such as cold, respiratory, and cardiovascular diseases, and the probability of dying from those diseases. The VSL was US$774,000. Generally, the WTP to avoid pollution-related diseases in China is high because exposure to industrial air pollution is a severe unavoidable problem in many Chinese megacities.
Others have focused on the U.K. For instance, Frew et al. (2001) investigated the WTP for two types of colorectal cancer screening. Patients were willing to pay between £30 and £50. It was found that male respondents and those that had an experience of a health condition were willing to pay more. Also, Tubeuf et al. (2015) studied respondents’ willingness to pay for an inherited retinal disease test. Three scenarios were presented to participants: a test that would reveal the disease’s inheritance nature; a test that would provide information about the future’s visual function; and a new treatment that would improve patients’ condition. The mean WTP in those scenarios were £539, £1516, and £6895. In all the scenarios, patients were willing to undertake the tests. WTP decreased with the female respondents.
Similarly, Hollinghurst et al. (2016) examined whether patients were willing to undergo diagnostic testing for pancreatic, colorectal, and lung cancer. The first part of the survey used a binary question format to ask patients to show whether they would accept a test, and the second asked how much they were willing to pay. The results were conflicting because most of the respondents who answered yes to the first question were unwilling to pay. The WTP for a chest X-ray was £365 if the risk was 10% high and £305 if it was 1% low. Using choice experiments, Hole (2008) quantified the attributes of a general practitioner’s choice, such as doctors’ knowledge of the patient, the doctor’s interpersonal manner, and thoroughness of the physical examination, flexibility of time of appointment, and appointment waiting days. The author included a cost variable even though these services are free at the point of delivery. The patients were willing to pay £1.71, £4.48, £2.53, £4.13, and £13.82 for those attributes.
The way people perceive health risks varies across healthcare systems. Also, perceptions about other people’s health-risk behaviors differ. For example, Shickle (1997) showed that when British respondents were asked to choose between giving treatment priority to a patient responsible for their illness and another who cannot be blamed, an overwhelming 74% of the respondents chose a nonsmoker over a smoker. Further, 80% of the respondents chose a patient with low alcohol consumption over a heavy drinker; 60% favored giving life-saving treatment to a patient with an inherited disease over an identical patient with diet-related disease. Similarly, Miraldo et al. (2014) investigated respondents’ behaviors toward the National Health Service (NHS), bearing the costs of risky behaviors such as smoking, alcohol consumption, sedentary life, unhealthy diet, and overeating. Half of the respondents agreed that the NHS should cover risky behaviors such as smoking, sedentary life, and heavy drinking. Those who engage in those behaviors were more likely to favor the NHS covering those costs. Further, they were more likely to support covering other people’s risky behaviors too.
Also, in the Netherlands, the respondents showed low solidarity with smokers and overweight people (Bonnie,van den Akker,van Steenkiste and Vos, 2010). Likewise, Van der Star and Van den Berg (2011) estimated Dutch respondents’ WTP to cover health-risk behavior such as smoking and non-lifestyle chronic disease in the primary health insurance package. About 80% of the respondents voted for a flat insurance premium regardless of healthcare utilization. The respondents were willing to pay €11.29 to include smoking behavior in the package compared to €42.39 for a chronic disease independent of their lifestyle.
In the U.S., Berk et al. (2006) reported that 52% of the respondents favored mandatory health insurance, 87% believed that health premiums should be flat and not vary with the health status of patients, 60% believed that people who engage in risky health behaviors such as smoking should pay higher premiums. About two-thirds of the respondents wanted the healthcare system to be publicly-funded. Jonas et al. (2010) elicited willingness to pay to avoid discomfort and time related to colposcopy. Participants were willing to pay US$263 to avoid those situations. On the other hand, using the 1991 National Maternal and Infant Health Survey (NMIHS), Agee et al. (2001) estimated smokers’ valuation of own and child’s health. The results suggest that smokers were willing to pay US$494.48 for a 10% increase in their child’s health annually. At the same time, they were willing to pay US$10.12 for a 1% reduction in their child’s exposure to ETS. However, the respondents were willing to pay US$198.29 for a 10% increase in their health. It was reported that WTP increased with the frequency of smoking and child exposure. Thus, smokers value their child’s health two times more than theirs. Neumann et al. (2012) studied respondents’ willingness to pay for Alzheimer’s, prostate cancer, arthritis, and breast cancer diagnostic tests. The median WTP was US$109–$263. Further, WTP declined with the female respondents.
First, prior research in this domain has predominantly focused on examining how individuals value the health risks of their behaviors. Surprisingly, the effects of other individuals’ health-risk behaviors on public health have been largely overlooked. By directing our investigation toward understanding how nonsmokers value the health risks associated with secondhand smoke and considering its impact on the wider public, our study brings attention to this novel behavioral aspect that has yet to be explored in the literature.
Second, a cross-country comparison is imperative to discern potential disparities in the valuation of secondhand smoke health risks between American and British nonsmokers. By juxtaposing the privately-funded healthcare system in the United States and the publicly-funded healthcare system in the United Kingdom, our study endeavors to fill this gap and shed light on how different healthcare financing structures may influence the perception and valuation of secondhand smoke health risks.
As a result, this research intends to unravel unique insights into the behavioral aspects of health-risk valuation concerning secondhand smoke, particularly concerning the consideration of its impact on public health and the comparative analysis across two countries with distinct healthcare systems. By addressing these unexplored dimensions, our study aims to contribute valuable knowledge to the existing literature and provide a more comprehensive understanding of how individuals from different healthcare contexts value the health risks associated with secondhand smoke exposure.
Methodology
Overview
We estimate both respondents’ willingness to accept health harm compensation due to SHS and willingness to pay to prevent exposure. Here, WTA is the amount of money that will keep an individual on a higher indifference curve (or the amount of money required to compensate the individual for health harms or losses) but on the same health risk level (\(\hbox {R}_{0}\)). Conversely, WTP is the amount that will be taken from the individual for a change from the status quo risk level (\(\hbox {R}_{0}\)) to an improved health level (\(\hbox {R}_{1}\)), while they are as well off as before.
We show the framework as follows: Assume an agent n with wealth \(w_{0}\) and status quo health risk \(R_{0}\). The utility functions of n are given as
where WTP is the amount of money n is willing to pay to prevent exposure to SHS, WTA is the amount n is willing to accept as compensation for health losses or harms due to SHS, and \(R_{1}\) is an improved health profile.
Contingent Valuation
We asked respondents to imagine a policy that would change their current level of SHS exposure. The payment vehicle was a one-off increment in their 1-year income tax. The question asked them to state the minimum and maximum WTP to prevent SHS exposure. It is a common practice to elicit maximum WTP only, but we included the minimum to ensure that zero responses in both cases signify a protest. We provided a cheap talk that reminded respondents to take the scenario as real and to be honest.
Survey and Data Collection
Besides the first part that provided a brief introduction of the study to respondents and the second that contained the University of Exeter’s generic consent questions, the survey had five blocks.
In part one, we asked questions relating to respondents’ knowledge and perceptions about SHS. Part two contained a few questions about their health status. Part three had WTP elicitation questions, including a question that asked respondents who indicated a zero WTP to state their reasons. Those who indicated a positive value were also asked to show how sure they were to pay the amount in reality on a ten-point Likert scale, ranging from not sure to very sure. In block four, we presented sixteen choice sets in two blocks of eight each. Respondents were randomly assigned these evenly. We asked a few socio-demographic questions in part five, including two debriefing questions that elicited respondents’ general views about SHS and the survey. The study terminated with a further explanation about SHS and how respondents can access the study’s findings in the future.
Participants were recruited and remunerated through the Prolific platform, a polling consultancy based in the United Kingdom. The sample consisted of individuals aged 18 years and above residing in the United States and the United Kingdom. Non-smokers were exclusively selected as participants in both countries, with an additional criterion for U.S. respondents requiring possession of health insurance. Prior to the primary survey, two pilot studies were conducted, encompassing both U.S. and U.K. populations. Subsequent to these preliminary investigations, adjustments to the questionnaire were made, involving the inclusion or removal of specific questions. A total of approximately 600 participants were surveyed in each country. The data collection period extended from September 14, 2020, to January 9, 2021. Following meticulous data cleaning procedures, 541 and 554 choice experiment responses from the U.S. and U.K. were employed in the estimation process, resulting in 8,656 and 8,864 observations, respectively. Notably, zero responses from the contingent valuation (CV) data were excluded, leading to the utilization of 364 and 363 observations from the U.S. and U.K., respectively.
The Choice Experimental Design
Table 1 contains the attributes and their levels. The choice of attributes and levels were informed by extensive literature review and pilot studies. The attributes relate to sufficient evidence of health effects of SHS to adults, such as stroke, lung cancer, and coronary heart disease (see CDC, 2020, The Tobacco Atlas, 2021). Other attributes used are emotional distress and monetary payoffs (reduction in health insurance premium or tax as the case may be).
These attributes and their levels in the full factorial design yield 512 \((2 \times 4^4)\) different alternatives. These would be \(512 \times 511/2 = 130,816\) pairs of choice sets, which will be too much for each respondent to complete. Thus, we constructed sixteen choice sets blocked into two pairs of eight choices using the D-efficient design. Without priors, and following the best practice guidelines, we set the attributes coefficients at zero (see Hole, 2008, 2017, Lancsar et al., 2017).
First, we designed the efficient experiment in Stata. Second, we transformed it into an Excel spreadsheet. Third, we wrote a Stata command in advanced format TXT files and constructed the CE tables using a hypertext markup language (HTML). Fourth, we randomized the order in which the choice sets were presented to participants within and across blocks using the advanced randomization option in Qualtrics. Finally, we wrote another Stata code that automatically transformed the collected data and made it ready for use (see Weber, 2019).
The choice experiment scenario asked participants to imagine that they had to choose between two bundles of potential health risk levels due to SHS exposure, including a monetary payoff. Respondents were given a general introduction about the sources, effects, and meaning of each disease associated with SHS. Also, a brief country-specific statistics on the risk levels of the respective diseases were provided. This was to ensure that respondents focus on the subject. We provided a question that asked respondents to rank the attributes to their order of dislike before proceeding with the choice tasks. Figure 1 represents one of the choice sets presented to participants from the United Kingdom during the study.
CV Models
One variant of CV uses open-ended questions that ask respondents to state their maximum WTP for an improvement in health conditions (see Contu & Mourato, 2020; Donaldson et al., 1998, Jonas et al., 2010). It is common to use ordinary least squares (OLS) regression to analyze the data in such a situation. However, this becomes problematic if the data set contains a substantial amount of zeros (Donaldson, Jones, Mapp and Olson, 1998) because of protest against paying for others’ health-risk behavior. It may be advisable to exclude the protest responses (Adamowicz et al., 2011; Johnston et al., 2017). The OLS regression is given by
where \({WTP}_{n}\) is the willingness to pay for respondent n, \(X_{n}\) is a vector of the explanatory variables, \(\beta\) is the vector of coefficients, \(\epsilon _{n}\) is the error term. Equation 3 is estimated by minimizing \(\sum _{n}\epsilon ^{2}_{n}\).
This model’s limitation is that it only gives the average relationship between the conditional mean of the dependent variable and a set of regressors, giving only a partial insight into the relationship (Cameron & Trivedi, 2010). Furthermore, even when the protest responses are removed from the estimation, there may still be some outliers, and because of the asymmetric distribution of the WTP, it is best practice to use the natural logarithm of WTP. Moreover, when such is done, if the smallest value of WTP is 1, it becomes 0.
The ensuing argument invokes the use of a censoring model such as the Tobit model. It assumes that the error term follows a censored normal distribution. The model is specified as:
where \(\Phi\) and \(\phi\) are the cumulative density function and standard normal density function, respectively, and \(\sigma\) is the standard deviation of \(\epsilon _{n}\). Here, the conditional mean function depends on the relationship between the dependent variable and a set of regressors and also on the probability that the dependent variable has a value that is greater than zero (Donaldson et al., 1998).
Another model favored over the OLS is quantile or median regression. It gives a complete view of the relationship between the dependent and independent variables at different quantiles in WTP distribution. Unlike the OLS regression, this model provides more robust results because it handles outliers efficiently. It is a semiparametric method, which does not make assumptions about the distribution of the error term (Cameron et al., 2005; Cameron & Trivedi, 2010). It is given by
where \(q \in (0,1)\) represents the quantile specified, the coefficients \(\beta ^{q}\) are realized by minimizing the weighted sum of the absolute values of \(\epsilon _{n}^{q}\).
To account for possible confounding effects, we include independent variables and specify the general form equation as:
Hence, we are interested in the sign and statistical significance level of the independent variables on willingness to pay.
CE Models
It is plausibly assumed that each decision-maker interprets utility in terms of attributes through a common functional form (Hensher et al., 2005). Suppose an individual n faces a set of alternative health scenarios denoted as J and \(j = 1,\ldots ,J\). Let \(U_{njt}\) represents the utility the n th individual derives from choosing the jth alternative in choice set t.
The individual’s utility is decomposed into representative (deterministic) and random parts. While the econometrician observes the representative part via estimation of model parameters, she is not aware of the random part (Train, 2009). The model can be specified in the additive form as:
where \(\beta _{1}\) to \(\beta _{5}\) are the parameters to be estimated; \(stroke_{njt}\) is stroke risk, \(cancer_{njt}\) is lung cancer risk, \(hrtdisease_{njt}\) is coronary heart disease risk, \(emodistress_{njt}\) is the risk of having emotional distress, \(payoff_{njt}\) is the reduction in health insurance premium or tax as the case may be, and \(\epsilon _{njt}\) is the random error term.
Suppose we assume that the random terms are independently and identically distributed (IID) type I extreme value. In that case, this yields the conditional logit model of McFadden (1974).
This model makes strong assumptions that the errors are IID, which leads to the second assumption of independence of irrelevant alternatives (IIA). This assumption states that the ratio of the probabilities of choosing any option over another \((\frac{P{_j}}{P{_i}})\) is not affected by the presence or absence of any other alternatives in the choice set. Thus, it treats respondents’ preferences and taste as homogeneous. However, in reality, the deterministic and random attributes of utility may depend on each other, and this correlation leads to the bias of the utility parameters.
As a result, more advanced models such as mixed logit (MXL) or random parameters logit (RPL), and generalized multinomial logit (G-MNL) are applied. The mixed logit model is highly flexible and guarantees a wide range of choices to specify individual-specific unobserved heterogeneity, although being fully parametric (Hensher & Greene, 2003). It overcomes the IIA assumption by treating the coefficients that enter the model as varying across individuals but being constant across choice occasions for each decision-maker (Train, 2009). In the mixed logit model, the unobserved part, \(\epsilon _{nit}\) is independently and identically distributed extreme value over people and alternatives. The \(\beta _{n}\) is a vector of coefficients [vector of parameter weights] representing individual-specific tastes with density \(f(\beta /\theta )\), where \(\theta\) represents, say, mean and covariance of the \(\beta ^{\prime }\)s in the population (Train, 2009). These conditional parameter estimates are strictly same-choice-specific parameters or the subpopulation’s mean that makes similar choices when faced with the same choice scenarios. It is an important distinction since it is impossible to establish every individual’s distinct set of estimates. Rather a mean estimate for the subpopulation who made the same set of choices is identified (Czajkowski et al., 2017; Hensher et al., 2005). It is worth noting that the MXL model collapses to the CL model if there is no unobserved heterogeneity. In which case, the CL can be reliable.
The probability that the decision-maker (n) makes a sequence of choices conditional on observing \(\beta\) is the product of the logit formula as:
where \(y_{njt}\) is equal to 1 if j alternative is chosen and to 0 otherwise, and \(\beta = (\beta _{1}, \beta _{2}, \beta _{3}, \beta _{4}, \beta _{5})\). The econometrician determines \(\beta\)’s distribution through intuition and statistical tests. While parameters in Eq. 8 can be estimated using the maximum likelihood (ML) method, the integral in Eq. 9 can only be simulated. Despite the MXL model’s appealing qualities and its wide application, it is not free from criticisms. The model still assumes that the random error is IID.
The G-MNL models heterogeneity in taste as scale heterogeneity. This means that the scale of the error term is more significant for some respondents than others. In other words, the idiosyncratic error terms are more critical to some decision-makers than the observed attributes. Thus, it accounts for some respondents’ random behavior by treating the attributes coefficients as a continuous mixture of scaled normals (Fiebig et al., 2010; Lancsar et al., 2017). However, the MXL model with correlated coefficients may provide a better fit. It is best practice to estimate all the models and choose the best using AIC and BIC criteria.
For convenience, we will specify the G-MNL as (Lancsar et al., 2017):
where \(X^{\prime }_{njt}\) is a vector of respondent n observed attributes, and \(\beta _{n}\) is a vector of respondent-specific coefficients.
No scale heterogeneity assume \(\lambda _{n} = \lambda\), and G-MNL collapses to MXL. Further, there is no preference heterogeneity if \(\eta _{n}\) = 0, thus, \(\beta _{n} = \lambda _{n}\beta\). Two variants of G-MNL emerge if \(\gamma\) is restricted to either zero (scaled random coefficients) or one (scaled means of the coefficients). In both cases, we will have \(\beta _{n} = \lambda _{n}(\beta + \eta _{n})\) and \(\beta _{n} = \lambda _{n}\beta + \eta _{n}\).
Another model that captures heterogeneity differently is the latent class logit model (LCM), because in modeling taste heterogeneity, corner solution may arise when a significant subpopulation of the population places a zero weight on some attributes and not accounting for this may not reveal the true nature of heterogeneity (Hensher, 2014). In modeling spatial heterogeneity, individuals are assumed to be sorted into a set of different classes or clusters (c), with the researcher not having prior knowledge of the cluster each belongs. Thus, preferences are homogeneous within classes but differ across classes (Greene & Hensher, 2003).
The difference between MXL and LCM is that in the former, parameters are individual-specific, while in the latter, it is class-specific. The utility is assigned a number based on the class to which a respondent belongs (Czajkowski et al., 2017). Further, while the MXL model assumes a full parametric distribution of the parameters, the LCM is semiparametric. This gives the analyst liberty not to make any distributional assumptions about individual heterogeneity (Greene & Hensher, 2003). While in the MXL, the coefficients are continuously distributed, they follow a discrete distribution in the LCM. Furthermore, although the two models can account for correlations between the coefficients, the analyst needs to specify this option in MXL while the LCM implicitly allows the coefficients to correlate. Thus, the choice of the distribution of \(\beta\) in the LCM is not controversial. Finally, the MXL model is estimated through maximum simulated likelihood (SML), while the LCM is estimated via the ML approach (Hole, 2008).
The LCM probability that n makes a sequence of choices is specified as:
where \(H_{nc}\) is the probability that n belongs to class c, which gives the multinomial logit:
where \(Z_{n}\) is a vector of observed characteristics of respondent n and \(\gamma _{c}\) parameter is normalized to zero for model identification (Andersson et al., 2019; Greene & Hensher, 2003; Yoo, 2020).
The marginal WTA compensation for SHS exposure is derived by partially differentiating Eq. 7 with respect to each of the attributes and dividing each by the monetary attribute. As per the LCM, this is simulated using the class-specific marginal utilities.
Results
Descriptive Statistics
Table 2 presents the key variables used in the analyses. We present the sample statistics of the pooled data, U.S., and U.K. data. For simplicity, we will focus on comparing U.S. and U.K. figures. In most cases, the samples are identical. The majority of the U.S. sample are males (55%) compared to 36%. More respondents are exposed to SHS at home and in private vehicles in the U.K. (35%) than in the U.S. (16%). Nearly half of respondents (48%) are living with a partner/spouse in the U.S. compared to 53% in the U.K. Only 4% of U.S. respondents’ partner/spouse smoke relative to 6% in the U.K. While 38% of U.S. respondents have/had serious ill-health, it is 40% in the U.K. The majority of respondents in the U.S. (82%) and U.K. (78%) indicated that SHS causes them distress. Respondents were asked to show on a ten-scale Likert of poor to excellent their knowledge about SHS effects. Most of the respondents (58%) in the U.S. and 53% of U.K. respondents reported having good knowledge, only 19% compared to 13% of respondents indicated that they have excellent knowledge. The income distributions of both samples are similar. The vast majority of respondents (64%) in the U.S. relative to 69% of U.K. respondents fall within the $1,100-$5,600 band.
Other variables not used in the estimations but provide more insight into our samples’ characteristics are presented in Table 14. The average age of U.S. respondents is 31.4 compared to 32.1 years. Only 24% (23%) of respondents have university degree; and 73% (69%) are in full employment; 63% (81%) are whites. It is worth noting that most U.K. respondents (72%) are exposed to SHS between four to seven times a week compared to 45% of U.S. participants. As per health-risk behaviors, more U.K. respondents (80%) consume alcohol compared to 56% of U.S. respondents. Further, they consume 3.4 glasses per week on average compared to 2.1 glasses reported by U.S. respondents.
Perceptions About Smoking Control
For exploratory reasons, we elicited respondents’ attitudes towards smoking. First, we asked: “Should governments ban smoking at home and in private vehicles when a nonsmoker is present?” An equal proportion of U.S. respondents (37%) voted yes and no, respectively. At the same time, 26% did not care. In the U.K., 60% of respondents answered in affirmative, only 16% voted no, and 24% did not care. Finally, we asked: “Should governments empower kids exposed to secondhand smoke at home to sue the smoker when they become adults?” Again, there were cross-country discrepancies. Only 23% of U.S. respondents answered yes, 32% indicated no, and 45% did not care. In comparison, 33% of U.K. respondents supported the law, 27% were against it, and the majority 40% did not care. These discrepancies could be because more U.K. respondents are exposed to SHS in those places than U.S. participants.
It is important to note that the statistical information presented herein pertains to a subset of the sample, as not all respondents responded to the open-ended questions. Consequently, to mitigate the potential for a substantial amount of missing data, which could compromise the robustness of the outcomes, we opted to avoid incorporating perceptions as an independent predictor in the models. Nonetheless, the descriptive analysis yields valuable insights into nonsmokers’ perceptions regarding smoking control in both countries.
CV Results
Diagnostic tests reveal that the distribution of WTP skewed to the left, and using it at levels can lead to biased predictions because it forces the effects of the independent variables to be additive (Cameron & Trivedi, 2010). Thus, we conduct the Box-Cox specification test on the log of WTP. The test favors the log-linear specification. We further test the functional form of the conditional mean of ln(WTP) using the Ramsey RESET test. The results show that the conditional mean of ln(WTP) is correctly specified. Although the standard errors are specified as robust, we formally test for the presence of heteroskedasticity using the Breusch-Pagan/Cook-Weisberg test. We conduct robustness checks using quantile regression (median regression).
We pooled the U.S. and U.K. data and estimate the difference using a dummy variable and further estimate separate models using country-specific data. The coefficient of the dummy variable in Table 3 is positive and statistically significant. This shows that U.S. respondents value SHS health risks more than their U.K. counterparts. In both countries, WTP declines with female respondents. Suspecting that the income effects might be responsible for this, we interact income with gender, but it is consistently negative and insignificant. The results are presented in Table 15. U.S. respondents who are living with a partner or spouse value SHS health risks less. However, those whose partner/spouse smokes in both countries are willing to pay more to prevent further SHS exposure. U.K. respondents suffering from or have experienced a serious ill-health are willing to pay more to avert SHS exposure. Also, U.K. respondents exposed to SHS at home/vehicle and are distressed by it value it more than their counterparts. In terms of knowledge, only U.S. respondents with excellent knowledge about SHS health effects are willing to pay more to prevent exposure. Furthermore, income is a significant predictor of WTP.
Table 4 presents the results of the quantile or median regression, using the 50th and 75th percentiles. It is worthy of note here that the gender discrepancy still holds in both countries. Thus, it is sufficient to conclude that female respondents value SHS risks less than men. In most cases, the signs of the coefficients are not different from those in Table 3.
We present the mean and median WTP of respondents in Table 5. U.S. respondents are willing to pay $521.63 to prevent SHS exposure compared to $242.96 by U.K. respondents. The difference is statistically significant (\(p<0.01\)). The median WTP is $100 compared to $68.57. We extrapolate these figures to the population to derive the economic cost of secondhand smoke. The costs are $173.123 billion and $16.357 billion in the U.S. and U.K., respectively.
CE Results
To ensure that respondents did not engage in unethical practices, we checked the possibility of consistently choosing a particular option before the estimation (see Viscusi et al., 1991). We did not find any abnormal responses, but incomplete responses were deleted. Following best practice guidelines (see Johnston et al., 2017, Lancsar et al., 2017), we started with a simple model such as the conditional logit (or fixed effect model) in Eq. 8 and estimated more advanced ones like the mixed logit/random parameters logit specified in Eq. 9, and generalized multinomial logit (G-MNL) in Eq. 11. While the conditional logit model treats individual preferences as homogeneous, the more advanced models account for heterogeneity in taste and scale. We model all the variables as continuous, except the emotional distress variable coded as a dummy. See Tables 12 and 13 for the summary statistics of the choice models variables.
In MXL I, we treat all parameters as normally distributed, except the payoff parameter, whereas all parameters are normally distributed in MXL II. MXL III accounts for correlation among the random coefficients. Since each respondent completed eight tasks, we anticipate correlated responses. Failure to account for this could bias the results (see Carlsson et al., 2010).
In the G-MNL specification, we restrict gamma to zero to account for scale heterogeneity (differences in error variance). Failure to account for this could produce biased estimators (Fiebig et al., 2010; Haab et al., 1999; Johnston et al., 2017). This model collapses to MXL if the coefficient of the scale parameter turns out to be statistically insignificant. The MXL and G-MNL models were estimated through maximum simulated likelihood with 500 Halton draws. We circumvent confounding effects on our results by not including covariates.
Concerning the coefficients’ interpretation of the results in Tables 6 and 7, it should be noted that signs of the attributes’ coefficients relate to how each affects the dependent variable (choice probability). A negative coefficient shows the probability of a decrease in utility. Overall, the signs of the coefficients are consistent with a priori expectation. All the coefficients are statistically significant. U.S. respondents prefer policies with a higher reduction in health insurance premiums and lower SHS health risks. However, the coefficient of a tax reduction in Table 7 is not statistically different from zero. It is worthy to note that respondents prefer a higher probability of reducing the risk of emotional distress than other risks.
It can be seen that the standard deviation coefficients are significant, meaning that there is evidence of heterogeneity in taste across our samples. Further, the scale parameter in the G-MNL is significant, indicating scale heterogeneity. In Table 6, the AIC and BIC favor MXL II, where all the coefficients are treated as random. However, the outcome is mixed in Table 7, where the AIC favors MXL III, while BIC prefers MXL II. The log-likelihood function is higher in MXL III. Revelt and Train (1998) recommended modeling the monetary variable as fixed; however, like our results, Meijer and Rouwendal (2006) and Hole (2008) found that allowing it to vary fits their data better.
Latent Class Model Results
Since the MXL model results show heterogeneity in our samples, we use a latent class logit model to sort respondents into different groups comprising identical preferences. We estimate three classes, which are determined using AIC and BIC. It is assumed that preferences are homogeneous within a class but heterogeneous across classes (Greene and Hensher, 2003). Ultimately, the model allows us to see how respondents in each class value the attributes. In our latent class model, class membership is explained by a constant. Thus, the likelihood of belonging to each group is constant across respondents (see also Adamowicz et al., 2011, Hole, 2008).
We model the payoff as homogeneous in Table 8, while we allow it to vary in Table 9. Specifying it this way gives our data a better fit. All the coefficients in Table 8, have the expected signs and are statistically significant, except the coefficient of emotional distress in class 3. This shows that emotional risk is not paramount to about 30% of respondents. Indeed, SHS may not cause emotional distress to a nonsmoker, depending on where their exposure takes place and the frequency. Furthermore, the log-likelihood is similar to the mixed logit model in Table 8, where all the coefficients are allowed to vary. This is consistent with the findings of Hole (2008). The majority of respondents belong to class 1, followed by classes 3 and 2, respectively.
As per the U.K. results, Table 9 shows that all the coefficients have the expected signs, except in class 2, where the tax coefficient is negative. It can be seen that the results vary substantially across classes. Most of the coefficients in class 2 are statistically significant, while only coronary heart disease risk and emotional distress are significant in class 1. In class 3, stroke and lung cancer risks are significant. The vast majority of respondents belong to class 1, followed by classes 2 and 3, respectively. Although the results of CL, MXL, and G-MNL presented in Table 7 show that the tax coefficient is not significant, the latent class model helps us see that it is significant for class 3 respondents.
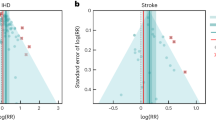
Table 10 presents the estimated WTA and 95% confidence intervals. The WTA estimates derived from the MXL II model are $3,067.57 for a potential stroke risk, $4,138.16 for lung cancer risk, $2,677.89 for coronary heart disease risk, and $28,939.14 for emotional distress risk. Comparing the estimates of the three classes in the latent class model, the WTA are $6,410.28, $1,912.11, and $2,606.68 for stroke risk; $4,809.25, $668.09, and $18,606.71 for lung cancer risk; $5,114.62, $515.28, and $2,822.96 for coronary heart disease; $60,766.10 and $13,210.01 for emotional distress, respectively.
Regarding the U.K. results presented in Table 11, we estimate the WTA of class 3 only because the tax coefficient is either not in line with theory or not statistically significant in other classes. The WTA is $3,424.69 for stroke risk and $12,731.80 for lung cancer risk.
Discussion and Conclusion
Several noteworthy insights emerge from our study findings. Regarding the contingent valuation (CV) results, as presented in Table 3, it is evident that American respondents exhibit a higher WTP than their British counterparts. The underlying determinants for this divergence are multifaceted. One plausible explanation is rooted in the premise that American respondents may possess a higher degree of health risk aversion relative to their British counterparts. This observation aligns with established research indicating that individuals with heightened risk aversion tendencies tend to manifest a greater WTP in order to mitigate health risks (Congress, 1997; Eeckhoudt & Hammitt, 2004; Fuchs & Zeckhauser, 1987; Liu et al., 1997; Smith et al., 2004).
These outcomes carry substantial implications for public policy formulation and regulatory measures. Recognizing the variances in risk aversion between American and British nonsmokers prompts a nuanced approach to shaping smoke-free policies in both countries. In the United States, policy interventions that effectively communicate the tangible health risks of secondhand smoke exposure may resonate more deeply with the population, particularly those inclined towards risk aversion. Enhancing awareness campaigns and disseminating information regarding the heightened health risks of secondhand smoke could garner more public support for stringent smoking control measures.
Conversely, while the general WTP appears lower in the British context, policy strategies could be tailored to resonate with the prevailing societal norms and preferences. Since policy preferences often reflect broader socio-cultural contexts, initiatives emphasizing the collective benefits of reduced secondhand smoke exposure within the British populace may resonate more strongly. Acknowledging these contrasting psychological drivers can inform the design and implementation of culturally relevant anti-smoking campaigns and public health interventions.
Our findings not only underscore the disparities in WTP for secondhand smoke health risks between American and British nonsmokers but also underscore the role of risk aversion as a potential underlying factor. These insights substantiate the significance of tailored policy approaches grounded in the nuanced psychological predispositions of the respective populations, thus facilitating the development of more effective and resonant smoke-free policies in both countries.
Our research findings indicate that male respondents are willing to allocate a higher monetary value in comparison to their female counterparts for mitigating the health risks associated with secondhand smoke. A plausible explanation for this disparity might be that male nonsmokers demonstrate a higher degree of health risk aversion compared to female nonsmokers. Nevertheless, it is important to note that the literature on valuation of health risks presents a mixed array of results. Some studies align with our observations (Adamowicz et al., 2011; Frew et al., 2001; Neumann et al., 2012; Tubeuf et al., 2015), while others contradict these outcomes (Andersson et al., 2015; Condliffe & Fiorentino, 2014; Viscusi & Huber, 2012).
Initially, we considered the possibility that other underlying factors, such as income level, might account for these divergent findings. However, after incorporating interaction terms in the analytical model (as presented in Table 15), we found no significant evidence to support such a relationship. The coefficients associated with the interaction terms were statistically insignificant, albeit displaying counterintuitive signs.
This insight into gender-based variations in the valuation of secondhand smoke health risks holds significant implications for public policy and regulatory decisions in both the United States and the United Kingdom. Understanding the differential willingness to pay for mitigating secondhand smoke health risks between male and female nonsmokers can aid policymakers in designing more targeted and effective interventions.
For instance, if male nonsmokers are indeed more risk-averse and willing to allocate higher financial resources for reducing their exposure to secondhand smoke, policymakers might consider tailoring educational campaigns and health initiatives specifically towards this demographic. Moreover, it could warrant a closer examination of the factors influencing risk perception and aversion in each gender group to address potential gender-specific barriers and concerns.
Additionally, by recognizing the mixed findings in the existing valuation literature, policymakers must approach this matter with caution and ensure that regulations and policies are well-informed by robust scientific evidence. Continued research and validation of these findings through longitudinal studies could provide a more comprehensive understanding of the underlying mechanisms influencing gender disparities in risk perception and willingness to pay for health protections.
In summary, this results shed light on the differential valuation of secondhand smoke health risks between male and female nonsmokers. The understanding of such gender-based disparities can contribute to the formulation of more targeted and effective public health policies, leading to better protection for both nonsmokers and the general population from the adverse effects of secondhand smoke exposure in the U.S. and U.K.
Notably, respondents with a smoker partner or spouse demonstrate a higher WTP, consistent with existing literature. Noteworthy studies have demonstrated that nonsmokers living with a partner or spouse who smokes face a substantially 30% higher risk of developing lung cancer than their counterparts residing with non-smoking partners or spouses (Hirayama, 1984; Pressman, 1993). Although complex, this association underscores the direct impact of exposure to secondhand smoke within intimate settings on perceived health risks and, subsequently, the corresponding valuation of strategies to reduce such risks.
Furthermore, our findings underscore a distinct trend within the British context. British respondents who have encountered episodes of significant ill health in their lives exhibit an increased willingness to pay to mitigate secondhand smoke risks. This inclination can be attributed to a heightened awareness of health vulnerabilities and a consequential desire to avoid exacerbating existing health conditions. Similar observations have been reported in prior research, supporting the notion that individuals who have experienced health setbacks are more attuned to the potentially detrimental effects of environmental factors such as SHS (Andersson et al., 2015; Frew et al., 2001; Hammitt & Zhou, 2006).
These discernible trends within our results carry pivotal implications for policy formulation and public health interventions. The elevated WTP among respondents cohabiting with smoker partners or spouses emphasizes the imperative for tailored campaigns and strategies that address not only the health risks of the smokers themselves but also those imposed on their non-smoking counterparts within shared living environments. Awareness initiatives targeting smokers and their cohabitants, emphasizing the dangers of secondhand smoke, may drive behavior change and incentivize more stringent smoke-free household policies.
Moreover, recognizing the augmented valuation of SHS risk mitigation strategies among British respondents who have faced health adversities underscores the potential effectiveness of targeted health communication campaigns. Designing public health messages that resonate with individuals who have experienced ill health can reinforce the importance of minimizing environmental health risks, fostering a greater willingness to support measures to reduce SHS exposure financially.
Our study’s identification of these distinct trends in WTP among respondents with smoker partners or spouses and those with previous experiences of ill health provides valuable insights for shaping policies that more effectively address secondhand smoke health risks. Tailored interventions, taking into account these nuanced factors, hold the potential to instigate behavioral shifts and promote healthier living environments, thereby contributing to enhanced public health outcomes.
Individuals exposed to SHS within their residences and private vehicles exhibit an elevated WTP to evade such exposure. However, it is notable that the statistical significance of this result is not observed within the U.S. context. This lack of significance could be attributed to the disparity in exposure prevalence, with 35% of U.K. respondents experiencing SHS exposure in these environments, in contrast to 16% of their U.S. counterparts. This variance in exposure rates underscores the intricate interplay between personal exposure experiences and the valuation of risk mitigation strategies.
Moreover, within the U.S. context, respondents demonstrating a heightened awareness of the health effects of SHS exhibit a higher WTP. This trend resonates with the findings of Kenkel (1991), who observed a decrease in health-risk behaviors among Americans possessing comprehensive health knowledge. This alignment highlights the pivotal role of knowledge dissemination in influencing individuals’ risk perceptions and willingness to allocate resources for health risk abatement.
The influence of socioeconomic status on WTP is also notable. Wealthier respondents showcase a higher WTP, a pattern congruent with existing research (Andersson et al., 2015, 2019; Adamowicz et al., 2011; Eeckhoudt & Hammitt, 2004; Viscusi & Huber, 2012). This phenomenon can be attributed to the recognition that individuals with greater economic resources possess more to lose in the event of health afflictions, thus motivating a more pronounced willingness to invest in averting potential health risks.
The substantial discrepancy between U.S. and U.K. respondents’ mean WTP is a striking outcome. U.S. respondents exhibit a WTP that is double that of their U.K. counterparts. The magnitude of this discrepancy is accentuated when contextualized against previous studies. U.S. nonsmokers’ mean WTP surpasses the $494 that American smokers were willing to pay annually to shield their children from SHS exposure (Agee et al., 2001). Additionally, U.S. respondents’ WTP surpasses the respective CAN$100 and CAN$225 values Canadians were willing to pay to reduce respiratory and cardiovascular diseases (Johnson et al., 2000). When compared internationally, Chinese respondents demonstrated a notably higher valuation of risks associated with chronic bronchitis and asthma due to air pollution (Guo et al., 2006; Hammitt & Zhou, 2006; Peng & Tian, 2003).
In this scenario, where current partial smoke-free laws persist, our analysis reveals significant disparities in the projected costs of SHS between the United States and the United Kingdom. Specifically, the estimated cost of SHS exposure is calculated to amount to $173.123 billion in the U.S., in stark contrast to $16.357 billion in the U.K.
These substantial variations in estimated costs can be attributed to several underlying factors. Firstly, the dissimilarity in population size between the two countries inevitably contributes to the stark contrast in absolute cost estimates. The larger population in the U.S. and the higher smoking prevalence rates result in an escalated burden of SHS-related health risks and their attendant costs. Moreover, disparities in SHS exposure prevalence and intensity within different societal contexts are pivotal contributors. In the U.S., despite partial smoke-free laws, a notable prevalence of SHS exposure persists due to localized variations in regulatory stringency and compliance. Conversely, the U.K.’s more comprehensive smoke-free legislation has significantly reduced smoking, leading to correspondingly lower projected costs.
These findings possess profound implications for policy formulation and public health interventions. The stark contrast in projected SHS costs between the U.S. and the U.K. underscores the potency of stringent smoke-free legislation in effectuating meaningful reductions in smoking-related health burdens. Robust smoke-free laws in the U.K. have successfully curtailed SHS exposure, yielding substantial health and economic dividends (WHO, 2023). This phenomenon underscores the imperative for the U.S. to consider augmenting its existing regulatory framework to encompass more comprehensive smoke-free policies, thereby mitigating the projected economic burden of SHS exposure.
Furthermore, our study underscores the latent economic value of bolstered anti-smoking policies. The pronounced cost disparities underscore the potential for substantial savings that can be realized by adopting measures to reduce SHS exposure. By integrating these economic insights into policy dialogues, public health advocates and policymakers can articulate the fiscal merits of comprehensive smoke-free legislation, fostering political will and facilitating informed decision-making.
In sum, the estimated economic costs of SHS exposure within a business-as-usual context are a stark reminder of insufficient smoke-free regulations’ tangible health and economic ramifications. The disparities in cost projections between the U.S. and the U.K. underscore the pivotal role of stringent regulatory measures in ameliorating SHS-related health burdens. These findings advocate for prioritizing robust smoke-free legislation, offering substantial economic benefits while safeguarding public health on both sides of the Atlantic.
The examination of the choice experiment results, as delineated in Table 7, elucidates a discernible contrast in the responses of U.K. and U.S. respondents. Specifically, U.K. respondents exhibit a stance of indifference towards a prospective policy entailing a guaranteed augmentation in disposable income as compensation for exposure to secondhand smoke (SHS). Conversely, U.S. respondents manifest an opposing inclination, displaying a preference for such compensation. This dichotomy of response can be explicated through the prism of several intricate factors, including variances in healthcare systems, as well as considerations of altruism, warm glow, and social preferences.
The observed distinctions in response may partly be attributed to the divergent healthcare systems in place. The U.S. healthcare framework, characterized by a greater emphasis on individualism and private provision, could foster a heightened valuing of individual compensation. Conversely, the publicly funded healthcare system in the U.K. may cultivate a sense of collectiveness and community well-being, thereby attenuating the perceived necessity for individual financial recompense. This perspective resonates with the observations of Bridges (2003), who linked social preferences to the concept of social capital-a construct encompassing shared communal values in contrast to individualistic paradigms.
Additionally, the propensity of U.K. respondents to favor mitigation measures over compensation merits consideration. This phenomenon aligns with the findings of Knetsch (1990), who established a preference for direct action to alleviate environmental concerns rather than material compensation. Furthermore, insights from Hollinghurst et al. (2016) highlight the intricacy of risk perception within the U.K. context. As indicated by Hollinghurst and colleagues, the inconsistency in participant responses underscores the nuanced and multifaceted nature of how U.K. individuals appraise and engage with risk-related scenarios.
These nuanced findings offer pertinent implications for policy formulation and strategic interventions. The preference divergence between U.K. and U.S. respondents underscores the imperative of contextually tailored policy approaches. For the U.S., where compensation is favored, policy strategies that offer material incentives could align with the prevailing individualistic ethos. In contrast, in the U.K., where mitigation is seemingly valued, policies prioritizing comprehensive smoke-free initiatives and health promotion measures may find greater resonance. Recognizing the interconnectedness between healthcare frameworks, societal norms, and valuation mechanisms is critical in crafting strategies that effectively cater to distinct preferences.
The juxtaposition of U.K. and U.S. respondent responses underscores the intricate interplay of healthcare systems, cultural inclinations, and valuation paradigms. These findings impel policymakers to adopt strategies that resonate with the prevailing societal ethos, facilitating more effective policy implementation. By aligning interventions with the nuanced preferences of each context, opportunities for fostering healthier environments and mitigating secondhand smoke-related health risks can be optimally harnessed.
The analysis of the findings, as elucidated in Table 9, engenders a deeper comprehension of the respondent preferences. This stratification of individuals into three distinct segments offers valuable insights into the multifaceted landscape of preferences exhibited by the study participants. The outcomes notably highlight the emergence of discrete segments characterized by unique valuation patterns, delineating three specific respondent groups.
Firstly, our analysis discerns a segment within the U.K. nonsmoking population that attributes a tangible monetary value to the health risks associated with stroke and lung cancer. This notable segment may encompass individuals who possess private health insurance or lack registration with a General Practice (GP), thus relying on direct out-of-pocket expenditures to access healthcare services. Alternatively, it is plausible that a significant proportion of respondents exposed to SHS within private settings align with this segment.
Parallel to our findings, extant literature has reported analogous class distinctions in respondents’ valuations of cancer disease attributes (Adamowicz et al., 2011; Andersson et al., 2016). These collective findings underscore the consistency of such segmental differentiation across different study contexts and settings, thus emphasizing the generalizability of the observed phenomenon. Informed by these consistent trends, policymakers can derive insights for formulating targeted communication strategies and policy frameworks that resonate with the distinct valuation patterns exhibited by these segments.
Examining emotional distress, an aspect hitherto underrepresented within the health valuation literature, introduces a fresh and noteworthy dimension to our study. Evidentiary support for emotional distress among Americans exposed to SHS has been documented (Bandiera et al., 2011), thereby elevating the pertinence of its inclusion in the valuation framework.
The outcomes articulated in Table 10 illuminate a distinctive tendency among American respondents to attribute a higher monetary value to emotional distress when compared to other associated attributes. The rationale underpinning this pronounced valuation preference warrants exploration. The precise factors engendering this elevated valuation for emotional distress in contrast to other attributes remain unresolved. However, insights from the American Psychiatric Association (APA) provide valuable context.
Indeed, the American Psychiatric Association’s assertion that mental health issues manifest as a substantial societal concern within the U.S., impacting nearly one in five adults (APA, 2018), offers a vantage point for comprehending the observed valuation patterns. The omnipresence of mental health struggles underscores the palpable influence of emotional well-being on the broader fabric of American society. The potential link between SHS exposure and subsequent emotional distress within a nation grappling with a significant mental health landscape signifies a salient policy consideration.
Policy insights stemming from these findings advocate for multifaceted interventions. Firstly, recognizing the distinct valuation of emotional distress positions the imperative for public health policies that encompass mental health considerations. Comprehensive smoke-free legislation that not only safeguards physical health but also attends to the emotional well-being of nonsmokers could be pivotal. Moreover, identifying emotional distress as a valued attribute can serve as an advocacy tool, underscoring the urgency of strategies targeting the mitigation of SHS exposure.
Incorporating these insights into the broader health policy landscape fosters the construction of more holistic policy frameworks. The elevation of mental health considerations within the context of SHS exposure aligns with the growing societal recognition of mental well-being as an integral component of public health. As the valuation of emotional distress offers novel insights into SHS-related health risks, its incorporation into policy narratives can invigorate the discourse surrounding smoke-free initiatives.
The heightened valuation of emotional distress among American respondents in the context of SHS health risks affords a compelling perspective on the interplay between mental health, societal consciousness, and policy interventions. The convergence of these factors underscores the significance of crafting policy measures that holistically address nonsmokers’ physical and emotional well-being. Integrating mental health considerations into the fabric of smoke-free policies can cultivate a broader and more inclusive approach to public health.
Even with the valuable insights derived from our study concerning the valuation of secondhand smoke (SHS) health risks among American and British nonsmokers, certain limitations merit consideration in interpreting our findings. While informative, the assumptions underpinning our valuation results do not comprehensively account for underlying differentials in healthcare access, encompassing variables such as user costs and service choice. Moreover, the intricate fabric of legislative frameworks, spanning the nature of jurisdiction and the coexistence of federal and state laws in the U.S., and the nuanced applications within the unitary system of the U.K. across its constituent nations, introduce complexities that could potentially influence the generalizability of certain conclusions based on the evidence obtained.
This study stands as a pioneering endeavor, offering unprecedented insights into the valuation of secondhand smoke health risks from the vantage point of nonsmokers. The revealed outcomes augur the impetus for further scholarly inquiry. This research direction holds salience in informing the trajectory of future smoke-free legislation, particularly within the evolving landscape following the COVID-19 pandemic. Delving deeper into the dynamics of political and legislative systems, particularly concerning their potential to facilitate health objectives and universal coverage, presents a fertile terrain for subsequent investigation.
Moreover, the discernible divergence in willingness to pay (WTP) between U.S. residents and counterparts from other regions engenders intriguing questions regarding the intricate interplay between perceptions of personal freedom and the attendant financial contributions. The formulation of future investigations aimed at unraveling these complexities, examining their implications for public health policies, and dissecting the societal constructs that shape such valuation patterns, holds the promise of yielding a more profound understanding of the intricate tapestry surrounding this topic.
While acknowledging the limitations of our current study, our findings serve as a catalyst for further scholarly engagement. Exploring uncharted territories in healthcare access, legislative systems, and societal perceptions can enrich our comprehension of the valuation of secondhand smoke health risks and their ramifications. These potential avenues of research can furnish critical insights that will significantly contribute to the refinement of public health strategies, thereby navigating the complexities of a post-COVID-19 era and advancing the discourse surrounding smoke-free legislation.
References
Adamowicz, W., Dupont, D., Krupnick, A., & Zhang, J. (2011). Valuation of cancer and microbial disease risk reductions in municipal drinking water: An analysis of risk context using multiple valuation methods. Journal of Environmental Economics and Management, 61(2), 213–226.
Agee, M. D., Crocker, T. D., & Altoona, P. (2001). Smoking parents’ valuations of own and children’s health economic valuation of mortality risk reduction: Assessing the state of the art for policy applications, 27.
Andersson, H., Hammitt, J. K., & Sundström, K. (2015). Willingness to pay and QALYs: What can we learn about valuing foodborne risk? Journal of Agricultural Economics, 66(3), 727–752.
Andersson, H., Hole, A. R., & Svensson, M. (2016). Valuation of small and multiple health risks: A critical analysis of sp data applied to food and water safety. Journal of Environmental Economics and Management, 75, 41–53.
Andersson, H., Hole, A.R. & Svensson, M. (2019) Valuation of health risks. In Oxford research encyclopedia of economics and finance Oxford.
APA (2018) What is mental illness? https://www.psychiatry.org/patients-families/what-is-mental-illness#:~:text=Mental%20illness%20is%20treatable.,function%20in%20their%20daily%20lives. &text=Mental%20health%20is%20the%20foundation,%2C%20resilience%20and%20self%2Desteem
Arana, J. E., & León, C. J. (2006). Modelling unobserved heterogeneity in contingent valuation of health risks. Applied Economics, 38(19), 2315–2325.
ASH (2020) Secondhand smoke https://ash.org.uk/wp-content/uploads/2020/03/SecondhandSmoke.pdf.
Bandiera, F. C., Richardson, A. K., Lee, D. J., He, J. P., & Merikangas, K. R. (2011). Secondhand smoke exposure and mental health among children and adolescents. Archives of Pediatrics & Adolescent Medicine, 165(4), 332–338.
Berk, M. L., Gaylin, D. S., & Schur, C. L. (2006). Exploring the public’s views on the health care system: A national survey on the issues and options—Americans want to see coverage expanded, but their beliefs about the relative roles of government, employers, and consumers vary. Health Affairs, 25(Suppl1), W596–W606.
Bonnie, L. H., van den Akker, M., van Steenkiste, B., & Vos, R. (2010). Degree of solidarity with lifestyle and old age among citizens in the Netherlands: Cross-sectional results from the longitudinal smile study. Journal of Medical Ethics, 36(12), 784–790.
Bridges, J., et al. (2003). Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Applied Health Economics and Health Policy, 2(4), 213–224.
Cameron, A. C., & Trivedi, P. K. (2005). Microeconometrics: Methods and applications. Cambridge university Press.
Cameron, A. C., & Trivedi, P. K. (2010). Microeconometrics Using Stata (Vol. 2). Stata press College Station.
Carlsson, F., Daruvala, D., & Jaldell, H. (2010). Value of statistical life and cause of accident: A choice experiment Risk Analysis: An. International Journal, 30(6), 975–986.
Carson, R. T., Flores, N. E., & Meade, N. F. (2001). Contingent valuation: Controversies and evidence. Environmental and Resource Economics, 19(2), 173–210.
CDC 2020 Health effects of secondhand smoke https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/index.htm#:~:text=Even%20brief%20secondhand%20smoke%20exposure,the%20cancer%20process%20in%20motion. &text=As%20with%20active%20smoking%2C%20the,risk%20of%20developing%20lung%20cancer
CDC (2021a) Health effects of secondhand smoke https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/
CDC (2021b) Prohibiting smoking in public housing nationally would save lives and: \$153 million annually https://www.cdc.gov/tobacco/infographics/secondhand-smoke/pdfs/p1002-smoke-free-housing.pdf
CDC (2021c) Secondhand smoke https://www.cdc.gov/tobacco/basic_information/secondhand_smoke/.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/
Charness, G., & Rabin, M. (2002). Understanding social preferences with simple tests. The Quarterly Journal of Economics, 117(3), 817–869.
Ciaccio, C. E., DiDonna, A., Kennedy, K., Barnes, C. S., Portnoy, J. M., & Rosenwasser, L. J. (2014). Secondhand tobacco smoke exposure in low-income children and its association with asthma in. Allergy and Asthma Proceedings, 35, 462.
Condliffe, S., & Fiorentino, G. T. (2014). The impact of risk preference on health insurance and health expenditures in the united states. Applied Economics Letters, 21(9), 613–616.
Congress, U. (1997). The benefits and costs of the clean air act, 1970–1990. Environ Prot, 7–58.
Contu, D., & Mourato, S. (2020). Complementing choice experiment with contingent valuation data: Individual preferences and views towards iv generation nuclear energy in the UK. Energy Policy, 136, 111032.
Czajkowski, M., Budziński, W., Campbell, D., Giergiczny, M., & Hanley, N. (2017). Spatial heterogeneity of willingness to pay for forest management. Environmental and Resource Economics, 68, 705–727.
de Hollander, A. E., & Melse, J. M. (2006). Valuing the health impact of air pollution: Deaths. DALYs or dollars Air pollution and health: Imperial College Press.
Donaldson, C., Jones, A. M., Mapp, T. J., & Olson, J. A. (1998). Limited dependent variables in willingness to pay studies: Applications in health care. Applied Economics, 30(5), 667–677.
Eeckhoudt, L. R., & Hammitt, J. K. (2004). Does risk aversion increase the value of mortality risk? Journal of Environmental Economics and Management, 47(1), 13–29.
Fiebig, D. G., Keane, M. P., Louviere, J., & Wasi, N. (2010). The generalized multinomial logit model: Accounting for scale and coefficient heterogeneity. Marketing Science, 29(3), 393–421.
Frew, E., Wolstenholme, J., & Whynes, D. (2001). Willingness-to-pay for colorectal cancer screening. European Journal of Cancer, 37(14), 1746–1751.
Fuchs, V. R., & Zeckhauser, R. (1987). Valuing health: A priceless commodity. The American Economic Review, 77(2), 263–268.
Gerard, K., Shanahan, M., & Louviere, J. (2003). Using stated preference discrete choice modelling to inform health care decision-making: A pilot study of breast screening participation. Applied Economics, 35(9), 1073–1085.
Greene, W. H., & Hensher, D. A. (2003). A latent class model for discrete choice analysis: Contrasts with mixed logit. Transportation Research Part B, 37, 681–698.
Guo, X., Haab, T. C. &Hammitt, J. K. (2006) Contingent valuation and the economic value of air-pollution-related health risks in China Technical report
Haab, T. C., Huang, J. C., & Whitehead, J. C. (1999). Are hypothetical referenda incentive compatible? A comment. Journal of Political Economy, 107(1), 186–196.
Hammitt, J. K. (2002). Qalys versus wtp risk analysis: An. International Journal, 22(5), 985–1001.
Hammitt, J. K., & Haninger, K. (2010). Valuing fatal risks to children and adults: Effects of disease, latency, and risk aversion. Journal of Risk and Uncertainty, 40(1), 57–83.
Hammitt, J. K., & Zhou, Y. (2006). The economic value of air-pollution-related health risks in China: A contingent valuation study. Environmental and Resource Economics, 33(3), 399–423.
Hensher, D. (2014). Attribute processing as a behavioural strategy in choice making. In: Handbook of choice modelling, Edward Elgar Publishing
Hensher, D. A., & Greene, W. H. (2003). The mixed logit model: The state of practice. Transportation, 30, 133–176.
Hensher, D. A., Rose, J. M., & Greene, W. H. (2005). Applied Choice Analysis: A Premier. Cambridge University Press.
Hirayama, T. (1984). Cancer mortality in nonsmoking women with smoking husbands based on a large-scale cohort study in Japan. Preventive Medicine, 13(6), 680–690.
Hole, A. R. (2008). Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. Journal of Health Economics, 27, 1078–1094.
Hole, A. R. (2017). Dcreate: Stata module to create efficient designs for discrete choice experiments Boston College Department of Economics
Hollinghurst, S., Banks, J., Bigwood, L., Walter, F. M., Hamilton, W., & Peters, T. J. (2016). Using willingness-to-pay to establish patient preferences for cancer testing in primary care. BMC Medical Informatics and Decision Making, 16(1), 1–13.
Huang, D., Andersson, H., & Zhang, S. (2018). Willingness to pay to reduce health risks related to air quality: Evidence from a choice experiment survey in Beijing. Journal of Environmental Planning and Management, 61(12), 2207–2229.
Jiang, C., Chen, Q., & Xie, M. (2020). Smoking increases the risk of infectious diseases: A narrative review. Tobacco Induced Diseases, 1, 10. https://doi.org/10.18332/tid/123845
Johnson, F. R., Banzhaf, M. R., & Desvousges, W. H. (2000). Willingness to pay for improved respiratory and cardiovascular health: A multiple-format, stated-preference approach. Health Economics, 9(4), 295–317.
Johnston, R. J., Boyle, K. J., Adamowicz, W., Bennett, J., Brouwer, R., Cameron, T. A., Hanemann, W. M., Hanley, N., Ryan, M., Scarpa, R., et al. (2017). Contemporary guidance for stated preference studies. Journal of the Association of Environmental and Resource Economists, 4(2), 319–405.
Jonas, D. E., Russell, L. B., Chou, J., & Pignone, M. (2010). Willingness-to-pay to avoid the time spent and discomfort associated with screening colonoscopy. Health Economics, 19(10), 1193–1211.
Kenkel, D. S. (1991). Health behavior, health knowledge, and schooling. Journal of Political Economy, 99(2), 287–305.
Kim, Y., Kling, C. L., & Zhao, J. (2015). Understanding behavioral explanations of the wtp-wta divergence through a neoclassical lens: Implications for environmental policy. Annual Reviews, 7(1), 169–187.
Knetsch, J. L. (1990). Environmental policy implications of disparities between willingness to pay and compensation demanded measures of values. Journal of Environmental Economics and Management, 18(3), 227–237.
Knetsch, J. L. (2007). Biased valuations, damage assessments, and policy choices: The choice of measure matters. Ecological Economics, 63(4), 684–689.
Krupnick, A., Alberini, A., Cropper, M., Simon, N., O’Brien, B., Goeree, R., & Heintzelman, M. (2002). Age, health and the willingness to pay for mortality risk reductions: A contingent valuation survey of Ontario residents. Journal of Risk and Uncertainty, 24(2), 161–186.
Lancsar, E., Fiebig, D. G., & Hole, A. R. (2017). Discrete choice experiments: A guide to model specification, estimation and software. PharmacoEconomics, 35, 697–716.
Liu, J. T., Hammitt, J. K., & Liu, J. L. (1997). Estimated hedonic wage function and value of life in a developing country. Economics Letters, 57(3), 353–358.
Martikke, S. (2017). Social capital: an overview. Greater Manchester Centre for Voluntary Organisation.
McFadden, D. L. (1974). Conditional logit analysis of qualitative choice behaviour. In P. Zamrebka (Ed.), Frontiers in econometrics. Academic Press.
Meijer, E., & Rouwendal, J. (2006). Measuring welfare effects in models with random coefficients. Journal of Applied Econometrics, 21(2), 227–244.
Mendez, A. D., Escobar, M., Encinas, M. R., & Wojcicki, J. (2021). Overcrowding and exposure to secondhand smoke increase risk for Covid-19 infection among latinx families in greater San Francisco bay area. medRxiv.
Miraldo, M., Galizzi, M. M., Merla, A., Levaggi, R., Schulz, P. J., Auxilia, F., Castaldi, S., & Gelatti, U. (2014). Should I pay for your risky behaviours? Evidence from London. Preventive Medicine, 66, 145–158.
Neumann, P. J., Cohen, J. T., Hammitt, J. K., Concannon, T. W., Auerbach, H. R., Fang, C., & Kent, D. M. (2012). Willingness-to-pay for predictive tests with no immediate treatment implications: A survey of US residents. Health Economics, 21(3), 238–251.
O’Brien, B., & Viramontes, J. L. (1994). Willingness to pay: a valid and reliable measure of health state preference? Medical Decision Making, 14(3), 289–297.
Peng, X., & Tian, W. (2003). Wtp study on the economic loss of the air-pollution-related diseases in Shanghai World. Economic Forum, 2, 32–43.
Portes, A. (1998). Social capital: Its origins and applications in modern sociology. Annual Review of Sociology, 24(1), 1–24.
Pressman, C. L. (1993). no smoking please. a proposal for recognition of non-Smokers’rights through tort law. NYLS Journal of Human Rights, 10(2), 8.
Revelt, D., & Train, K. (1998). Mixed logit with repeated choices: Households’ choices of appliance efficiency level. Review of Economics and Statistics, 80(4), 647–657.
SFF (n.d.) Facts about secondhand smoke http://www.smokefreefamilies.co.uk/facts#:~:text=Every%20year%2C%209%2C500%20children%20in,natal%20or%20sudden%20infant%20death
Shickle, D. (1997). Public preferences for health care: Prioritisation in the united kingdom. Bioethics, 11(3–4), 277–290.
Smith, V. K., Evans, M. F., Kim, H., & Taylor, D. H., Jr. (2004). Do the near-elderly value mortality risks differently? Review of Economics and Statistics, 86(1), 423–429.
The Cancer Council (2019) Secondhand smoke and increased risk of infectious disease https://www.tobaccoinaustralia.org.au/chapter-4-secondhand/4-12-secondhand-smoke-and-increased-risk-of-infect
The Tobacco Atlas (2021) Secondhand smoke https://tobaccoatlas.org/topic/secondhand/
Train, K. E. (2009). Discrete Choice Methods with Simulation. Cambridge University Press.
Tubeuf, S., Willis, T. A., Potrata, B., Grant, H., Allsop, M. J., Ahmed, M., Hewison, J., & McKibbin, M. (2015). Willingness to pay for genetic testing for inherited retinal disease. European Journal of Human Genetics, 23(3), 285–291.
UNEP (2019a) Clean air as a human right https://www.unep.org/news-and-stories/story/clean-air-human-right
UNEP (2019b) Clean air is a human right - un special rapporteur https://unfccc.int/news/clean-air-is-a-human-right-un-special-rapporteur#:~:text=Clean%20Air%20is%20a%20Human%20Right%20%2D%20UN%20Special%20Rapporteur%20%7C%20UNFCCC
Van der Star, S. M., & Van den Berg, B. (2011). Individual responsibility and health-risk behaviour: A contingent valuation study from the ex ante societal perspective. Health Policy, 101(3), 300–311.
van der Eijk, Y., & Porter, G. (2015). Human rights and ethical considerations for a tobacco-free generation. Tobacco Control, 24(3), 238–242.
Viscusi, W. K., & Huber, J. (2012). Reference-dependent valuations of risk: Why willingness-to-accept exceeds willingness-to-pay. Journal of Risk and Uncertainty, 44(1), 19–44.
Viscusi, W. K., Magat, W. A., & Huber, J. (1991). Pricing environmental health risks: Survey assessments of risk-risk and risk-dollar trade-offs for chronic bronchitis. Journal of Environmental Economics and Management, 21(1), 32–51.
Weber, S. (2019). A step-by-step procedure to implement discrete choice experiments in qualtrics. Social Science Computer Review, 39.5(2021), 903–921.
Whittington, D., Adamowicz, W., & Lloyd-Smith, P. (2017). Asking willingness-to-accept questions in stated preference surveys: a review and research agenda. Annual Review of Resource Economics, 9, 317–336.
WHO (2005). Convention on tobacco control https://www.who.int/tobacco/framework/WHO_FCTC_english.pdf
WHO (2013). WHO framework convention on tobacco control: Guidelines for implementation of article 5. 3, Articles 8 To 14 World Health Organization
WHO (2020). Tobacco [online] https://www.who.int/news-room/fact-sheets/detail/tobacco
WHO (2023). Who report on the global tobacco epidemic, 2023 protect people from tobacco smoke https://www.who.int/publications/i/item/9789240077164
World Bank (2023). Prevalence of current tobacco use (% of adults) https://data.worldbank.org/indicator/SH.PRV.SMOK
Yach, D. (2020). Tobacco use patterns in five countries during the Covid-19 lockdown. Nicotine & Tobacco Research, 22(9), 1671–1672.
Yang, X., Yan, Z., Xu, G., Tan, Y., & Zhu, J. (2021). How secondhand smoke exposure affects tobacco use and smoking susceptibility of adolescents: Sex and school differences. Tobacco Induced Diseases, 19, 68.
Yoo, H. I. (2020). Lclogit2: An enhanced command to fit latent class conditional logit models. The Stata Journal, 20(2), 405–425.
Acknowledgements
The author is grateful to his kind and supportive supervisors, Professor SC and Prof. BG. He also thanks the following for answering his questions: Prof. ARH and Prof. SW.
Funding
This study was funded by the University of Exeter.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares none
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Although this study was conducted when the author was at the University of Exeter, he is now a Teaching Fellow at the Department of Economics, University of Warwick. Note: This paper is available as a working paper with the title “Willingness to pay or willingness to accept? An experimental study on secondhand smoke”.
A Appendix
A Appendix
We present other summary statistics not used in the models in Table 14.
Robustness checks
See Table 15.
The proportion of zero responses presented in Table 16 reveals that approximately 33% of respondents from the United States and 34% from the United Kingdom provided zero values. This phenomenon is interpreted as a form of protest, as a significant number of participants expressed an unwillingness to pay for others' risky behaviors. For those respondents who assigned a positive value, an inquiry was made regarding their level of certainty in actualizing the stated payment. Notably, 13.49% of U.S. respondents and 15.52% of U.K. respondents indicated uncertainty, while 22.37% and 27.26%, respectively, expressed assurance, and 14.97% and 22.74%, respectively, conveyed a high level of confidence in their willingness to pay. Furthermore, within the category of respondents expressing a high level of certainty, U.S. participants demonstrated a willingness to pay $864.07, in contrast to the $131 indicated by their U.K. counterparts.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nduka, E. How do American and British Nonsmokers Value Secondhand Smoke Health Risks?. J of Prevention 45, 47–85 (2024). https://doi.org/10.1007/s10935-023-00752-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10935-023-00752-0