Abstract
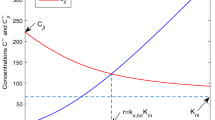
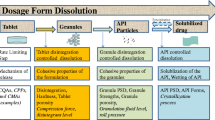
Intermittent drug dosing intervals are usually initially guided by the terminal pharmacokinetic half life and are dependent on drug formulation. For chronic multiple dosing and for extended release dosage forms, the terminal half life often does not predict the plasma drug accumulation or fluctuation observed. We define and advance applications for the operational multiple dosing half lives for drug accumulation and fluctuation after multiple oral dosing at steady-state. Using Monte Carlo simulation, our results predict a way to maximize the operational multiple dosing half lives relative to the terminal half life by using a first-order absorption rate constant close to the terminal elimination rate constant in the design of extended release dosage forms. In this way, drugs that may be eliminated early in the development pipeline due to a relatively short half life can be formulated to be dosed at intervals three times the terminal half life, maximizing compliance, while maintaining tight plasma concentration accumulation and fluctuation ranges. We also present situations in which the operational multiple dosing half lives will be especially relevant in the determination of dosing intervals, including for drugs that follow a direct PKPD model and have a narrow therapeutic index, as the rate of concentration decrease after chronic multiple dosing (that is not the terminal half life) can be determined via simulation. These principles are illustrated with case studies on valproic acid, diazepam, and anti-hypertensives.




Similar content being viewed by others
References
Sahin S, Benet LZ (2008) The operational multiple dosing half-life: a key to defining drug accumulation in patients and to designing extended release dosage forms. Pharm Res 25:2869–2877
Boxenbaum H, Battle M (1995) Effective half-life in clinical pharmacology. J Clin Pharmacol 35:763–766
Hamby DM (1994) A review of techniques for parameter sensitivity analysis of environmental models. Environ Monit Assess 32:135–154
Perucca E, Gatti G, Frigo GM, Crema A, Calzetti S, Visintini D (1978) Disposition of sodium valproate in epileptic patients. Br J Clin Pharmacol 5:495–499
Dutta S, Reed RC, O’Dea RF (2006) Comparative absorption profiles of divalproex sodium delayed-release versus extended-release tablets—clinical implications. Ann Pharmacother 40:619–625
Dutta S, Reed RC, Cavanaugh JH (2004) Absolute bioavailability and absorption characteristics of Divalproex sodium extended-release tablets in healthy volunteers. J Clin Pharmacol 44:737–742
Goldkind L, Bashaw D The essentials of “dosing interval” [PowerPoint slides]. U.S. Food and Drug Administration. www.fda.gov/ohrms/dockets/ac/02/slides/3873S2_02_Goldkind-Bashaw.ppt
Committee for Proprietary Medicinal Products (2002) Note for Guidance on clinical investigation of medicinal products for treatment of nociceptive pain. The European Agency for the Evaluation of Medicinal Products, London, UK
Mager DE, Wyska E, Jusko WJ (2003) Diversity of mechanism-based pharmacodynamic models. Drug Metab Dispos 31:510–518
Meibohm B, Derendorf H (1997) Basic concepts of pharmacokinetic/pharmacodynamic (PK/PD) modelling. Int J Clin Pharmacol Ther 35:401–413
Danhof M, de Lange EC, Della Pasqua OE, Ploeger BA, Voskuyl RA (2008) Mechanism-based pharmacokinetic-pharmacodynamic (PK-PD) modeling in translational drug research. Trends Pharmacol Sci 29:186–191
Depakote ER (2007) Physicians’ desk reference. Thomson PDR, Montvale, NJ
Charney DS, Mihic SJ, Harris RA (2006) Hypnotics and sedatives. In: Brunton LL, Lazo JS, Parker KL (eds) Goodman & Gilman’s the pharmacological basis of therapeutics, Chapter 16. McGraw-Hill, New York, pp 403–427
Locniskar A, Greenblatt DJ, Zinny MA, Harmatz JS, Shader RI (1984) Absolute bioavailability and effect of food and antacid on diazepam absorption from a slow-release preparation. J Clin Pharmacol 24:255–263
Schaefer HG, Heinig R, Ahr G, Adelmann H, Tetzloff W, Kuhlmann J (1997) Pharmacokinetic-pharmacodynamic modelling as a tool to evaluate the clinical relevance of a drug-food interaction for a nisoldipine controlled-release dosage form. Eur J Clin Pharmacol 51:473–480
Hocht C, Mayer MA, Opezzo JAW, Bertera FM, Taira CA (2008) Pharmacokinetic-pharmacodynamic modeling of antihypertensive drugs: from basic research to clinical practice. Curr Hypertens Rev 4:289–302
Csajka C, Buclin T, Fattinger K, Brunner HR, Biollaz J (2002) Population pharmacokinetic-pharmacodynamic modelling of angiotensin receptor blockade in healthy volunteers. Clin Pharmacokinet 41:137–152
drugs@FDA, FDA Approved Drug Products. U.S. Food and Drug Administration. www.accessdata.fda.gov/scripts/cder/drugsatfda
Lim HS, Cho JY, Oh DS, Chung JY, Hong KS, Bae KS, Yu KS, Lee KH, Jang IJ, Shin SG (2007) Angiotensin II type 1 receptor 1166A/C polymorphism in association with blood pressure response to exogenous angiotensin II. Eur J Clin Pharmacol 63:17–26
Blychert E, Hedner T, Dahlöf C, Elmfeldt D (1990) Plasma concentration-effect relationships of intravenous and extended-release oral felodipine in hypertensive patients. J Cardiovasc Pharmacol 15:428–435
Muller P, Flesch G, de Gasparo M, Gasparini M, Howald H (1997) Pharmacokinetics and pharmacodynamic effects of the angiotensin II antagonist valsartan at steady state in healthy, normotensive subjects. Eur J Clin Pharmacol 52:441–449
Oparil S, Williams D, Chrysant SG, Marbury TC, Neutel J (2001) Comparative efficacy of olmesartan, losartan, valsartan, and irbesartan in the control of essential hypertension. J Clin Hypertens 3:283–291 318
Brocks DR, Mehvar R (2010) Rate and extent of drug accumulation after multiple dosing revisited. Clin Pharmacokinet 49:421–438
Acknowledgments
We thank the Center for Drug Development Sciences at the University of California, San Francisco for the annotated list of drugs approved from 1980 to 2007 that served as the basis for the anti-hypertensive case study. AG is funded in part by an American Foundation for Pharmaceutical Education Pre-Doctoral fellowship and by an Achievement Rewards for College Scientists fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grover, A., Benet, L.Z. Intermittent drug dosing intervals guided by the operational multiple dosing half lives for predictable plasma accumulation and fluctuation. J Pharmacokinet Pharmacodyn 38, 369–383 (2011). https://doi.org/10.1007/s10928-011-9198-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-011-9198-0