Abstract
Purpose
Based on the theoretical framework of the Model of Preventive Behaviours at Work, the aim of this study was to describe the the occupational rehabilitation strategies the literature reports that support workers who have suffered an occupational injury in adopting preventive behaviours.
Methods
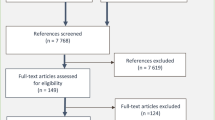
To conduct this scoping review, we used a systematic methodology in 7 steps : (1) definition of the research question and inclusion/exclusion criteria; (2) scientific and gray literature search; (3) determination of manuscripts’ eligibility; (4) extraction and charting of information; (5) quality assessment; (6) interpretation; and (7) knowledge synthesis.
Results
We selected 46 manuscripts of various types (e.g. randomized trials, qualitative studies, governmental documents). Manuscripts were mainly of good or high quality according to our quality assessment. The strategies for coaching, engaging, educating and collaborating were mostly reported in the literature to support the development of the six preventive behaviours during occupational rehabilitation. The results also suggest that heterogeneity exists regarding the specificity of the strategies reported in the literature, which may have hindered our ability to provide rich and detailed descriptions. Literature also mainly describes individually oriented behaviours and reports strategies requiring a low level of worker involvement, which represent issues to adress in future researh projects.
Conclusion
The strategies described in this article reprensent concrete levers that occupational rehabilitation professionals can use to support workers in the adoption of preventive behaviours at work on return from having suffered an occupational injury.

Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Notes
In the "Results" section, the number presented in the parentheses following the strategy refers to the number of manuscripts that address it, according to our scoping review.
References
Lange C, Burgmer M, Braunheim M, Heuft G. Prospective analysis of factors associated with work reentry in patients with accident-related injuries. J Occup Rehabil. 2007;17(1):1–10. https://doi.org/10.1007/s10926-006-9039-y.
Post RB, Van der Sluis CK, Ten Duis HJ. Return to work and quality of life in severely injured patients. Disabil Rehabil. 2006;28(22):1399–404. https://doi.org/10.1080/09638280600641392.
He Y, Hu J, Yu ITS, Gu W, Liang Y. Determinants of return to work after occupational injury. J Occup Rehabil. 2010;20(3):378–86. https://doi.org/10.1007/s10926-010-9232-x.
Jensen C, Jensen OK, Nielsen CV. Sustainability of return to work in sick-listed employees with low-back pain. Two-year follow-up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskelet Disord. 2012;13(1):156. https://doi.org/10.1186/1471-2474-13-156.
Kulmala J, Luoma A, Koskinen L. Able or unable to work? Life trajectory after severe occupational injury. Disabil Rehabil. 2019;41(18):2192–8. https://doi.org/10.1080/09638288.2018.1464603.
IRSST. Plan quinquennal de production scientifique et technique [Five-year scientific and technical production plan], 2018–2022. 2017.
Organization WH, Rehabilitation. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation?fbclid=IwAR32VJDb4WbtWWLlQXil06ITAEeg
Durand M-J, Baril R, Loisel P, Gervais J. Trajectoires des travailleurs recevant un programme de retour au travail: étude exploratoire des discussions d’une équipe interdisciplinaire [Trajectories of workers receiving a return-to-work program: exploratory study of an interdisciplinary team's discussions]. Perspectives interdisciplinaires sur le travail et la santé. 2008. https://doi.org/10.4000/pistes.2223.
Young A. Employment maintenance and the factors that impact it after vocational rehabilitation and return to work. Disabil Rehabil. 2010;32(20):1621–32. https://doi.org/10.3109/09638281003611029.
Berecki-Gisolf J, Clay FJ, Collie A, McClure RJ. Predictors of sustained return to work after work-related injury or disease: insights from workers’ compensation claims records. J Occup Rehabil. 2012;22(3):283–91. https://doi.org/10.1007/s10926-011-9344-y.
Marras WS, Ferguson SA, Burr D, Schabo P, Maronitis A. Low back pain recurrence in occupational environments. Spine. 2007;32(21):2387–97. https://doi.org/10.1097/BRS.0b013e3181557be9.
Wasiak R, Pransky G, Verma S, Webster B. Recurrence of low back pain: definition-sensitivity analysis using administrative data. Spine. 2003;28(19):2283–91. https://doi.org/10.1097/01.BRS.0000085032.00663.83.
Wasiak R, Verma S, Pransky G, Webster B. Risk factors for recurrent episodes of care and work disability: case of low back pain. J Occup Environ Med. 2004. https://doi.org/10.1097/01.jom.0000105987.32375.3d.
Lecours A, Durand M-J, Coutu M-F, Groleau C, Bédard-Mercier R. Stay at Work after a period of disability due to an occupational injury: a complex process marked by social exchanges. J Occup Rehabil. 2022;Online:1–10. https://doi.org/10.1007/s10926-021-10008-5.
Lammerts L, Schaafsma FG, Eikelenboom M, Vermeulen SJ, van Mechelen W, Anema JR, et al. Longitudinal associations between biopsychosocial factors and sustainable return to work of sick-listed workers with a depressive or anxiety disorder. J Occup Rehabil. 2016;26(1):70–9. https://doi.org/10.1007/s10926-015-9588-z.
Hoefsmit N, Houkes I, Boumans N, Noben C, Winkens B, Nijhuis FJ. The effectiveness of an intervention to enhance cooperation between sick-listed employees and their supervisors (COSS). J Occup Rehabil. 2016;26(2):229–36. https://doi.org/10.1007/s10926-015-9606-1.
Steenstra IA, Anema JR, Bongers PM, De Vet HC, Van Mechelen W. Cost effectiveness of a multi-stage return to work program for workers on sick leave due to low back pain, design of a population based controlled trial. BMC Musculoskelet Disord. 2003;4(1):1–11. https://doi.org/10.1186/1471-2474-4-26.
Etuknwa A, Daniels K, Eib C. Sustainable return to work: a systematic review focusing on personal and social factors. J Occup Rehabil. 2019. https://doi.org/10.1007/s10926-019-09832-7.
Durand M-J, Coutu M-F, Tremblay D, Sylvain C, Gouin M-M, Bilodeau K, et al. Insights into the sustainable return to work of aging workers with a work disability: an interpretative description study. J Occup Rehabil. 2020. https://doi.org/10.1007/s10926-020-09894-y.
Brusletto B, Torp S, Ihlebæk C, Vinje H. A five-phase process model describing the return to sustainable work of persons who survived cancer: a qualitative study. Eur J Oncol Nurs. 2018;34:21–7. https://doi.org/10.1016/j.ejon.2018.03.003.
Palstam A, Törnbom M, Sunnerhagen K. Experiences of returning to work and maintaining work 7 to 8 years after a stroke: a qualitative interview study in Sweden. BMJ Open. 2018;8:e021182. https://doi.org/10.1136/bmjopen-2017-021182.
Celentano J, Palmaricciotti V, Nyssen AS, Malaise N, Salamun I, Faymonville M-E. Fibromyalgie et lombalgie chronique: étude des facteurs invalidants et facteurs facilitateurs à la réinsertion et au maintien professionnel [Fibromyalgia and chronic low back pain: study of disabling and facilitating factors for professional reintegration and retention]. Douleur et Analgésie. 2011;24:46–9. https://doi.org/10.1007/s11724-011-0235-y.
Bültmann U, Brouwer S. Individual-level psychosocial factors and work disability prevention. In: Loisel P, Anema JR, editors. Handbook of work disability. New York: Springer; 2013. p. 149–62.
Lecours A, Coutu M-F, Durand M-J. Description des stratégies favorisant l’adoption de comportements préventifs chez les travailleurs ayant subi une lésion professionnelle: une revue critique de la littérature [Description of strategies promoting the adoption of preventive behaviors among workers who have suffered an occupational injury: a critical review of the literature]. Montréal: Institut de recherhe Robert-Sauvé en santé et sécurité du travail; 2022.
Lecours A. Validation du modèle des comportements préventifs au travail: Une étude Delphi [Validation of the Model of Preventive Behaviour at work: A Delphi Study]. Recl Annuel Belge d’Ergothérapie. 2021;13:54–63.
Lecours A. Scientific, professional and experiential validation of the model of preventive behaviours at work: protocol of a modified Delphi study. BMJ Open. 2020;10(9):e035606. https://doi.org/10.1136/bmjopen-2019-035606.
Lecours A. Using an occupational perspective to understand behaviours fostering the prevention of work-related health problems: a proposed conceptual model. J Occup Sci. 2020;27(2):222–35. https://doi.org/10.1080/14427591.2019.1600575.
Lecours A, Therriault P-Y. Development of preventive behavior at work: description of occupational therapists’ practice. Work. 2018;61(3):477–88. https://doi.org/10.3233/wor-182811.
Lecours A, Therriault P-Y. Habiliter les travailleurs à la prévention: description des pratiques des ergothérapeutes visant la mise en place des antécédents du comportement préventif au travail [Enabling workers to prevention: a description of occupational therapists' practices aimed at establishing antecedents of preventive behaviours at work]. Revue Francophone de Recherche en Ergothérapie. 2019;5(1):59–79. https://doi.org/10.13096/rfre.v5n1.97.
van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60(6):429–37. https://doi.org/10.1136/oem.60.6.429.
Gouvernement de l’Alberta. Let’s talk: a guide to resolving workplace conflicts. Alberta: Alberta Human Services; 2016. p. 36.
Andersen LN, Juul-Kristensen B, Sørensen TL, Herborg LG, Roessler KK, Søgaard K. Efficacy of tailored physical activity or chronic pain self-management programme on return to work for sick-listed citizens: a 3-month randomised controlled trial. Scand J Public Health. 2015;43(7):694–703. https://doi.org/10.1177/1403494815591687.
Reicher S, Michie S, West R. The UK government’s “personal responsibility” policy for covid is hypocritical and unsustainable. BMJ. 2022;378:1903.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69.
Colquhoun HL, Levac D, Amp, Apos, Brien KK, Straus S, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. https://doi.org/10.1016/j.jclinepi.2014.03.013.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Merriam-Webster. Merriam-Webster dictionnary. 2023. Available from: http://www.merriam-webster.com.
Oxford dictionnary of public health: Oxford University Press. 2023. Available from: http://www.oxfordreference.com/.
Kielhofner G. Model of human occupation: Theory and application. 4th ed. Baltimore, Mar: Lippincott Williams & Wilkins. 2008. xvii, p. 565
Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4(1):1–10. https://doi.org/10.1186/s13643-015-0125-0.
Covidence. Covidence systematic review management. 2022. Available from: https://www.covidence.org/.
Egger M, Smith GD, O’Rourke K. Introduction: Rationale, potentials, and promise of systematic reviews. In: Egger M, Smith GD, Altman D, editors. Systematic reviews in health care: meta-analysis in context. 2nd ed. BMJ Books. 2001. pp. 1–19.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097–e. https://doi.org/10.1371/journal.pmed.1000097.
Higgins JPT, Deeks J. Selecting studies and collecting data. Cochrane Handbook for Systematic Reviews of Interventions. 2008. https://doi.org/10.1002/9780470712184.ch.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348(mar07 3):g1687–g. https://doi.org/10.1136/bmj.g1687.
Pluye P, Gagnon M-P, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud. 2009;46(4):529–46. https://doi.org/10.1016/j.ijnurstu.2009.01.009.
Souto RQ, Khanassov V, Hong QN, Bush PL, Vedel I, Pluye P. Systematic mixed studies reviews: updating results on the reliability and efficiency of the mixed methods appraisal tool. Int J Nurs Stud. 2015;52(1):500–1. https://doi.org/10.1016/j.ijnurstu.2014.08.010.
Scottish Intercollegiate Guidelines Network (SIGN). Methodology Cheklist 1: Systematic Reviews and Meta-analyses Edinburgh: SIGN. 2020. Available from: http://www.sign.ac.uk.
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the mixed methods appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459–67. https://doi.org/10.1111/jep.12884.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. J Clin Epidemiol. 2019;111:49–59. e1.
Souto RQ, de Araújo Lima KS, Pluye P, Hong QN, Barbosa K, de Araújo GKN. Translation and cross-cultural adaptation of the mixed methods appraisal tool to the Brazilian context. RPCFO. 2020;12:510–6. https://doi.org/10.5935/0103-507X.20180033.
Shukla VK, Bai A, Milne S, Wells G, editors. Systematic review of quality assessment instruments for randomized control trials: selection of SIGN50 methodological checklist. XV Cochrane Colloquium. 2007.
Cancelliere C, Kristman VL, Cassidy JD, Hincapié CA, Côté P, Boyle E, et al. Systematic review of return to work after mild traumatic brain injury: results of the international collaboration on mild traumatic brain injury prognosis. Arch Phys Med Rehabil. 2014;95(3):201-S9. https://doi.org/10.1016/j.apmr.2013.10.010.
Sameem M, Wood T, Ignacy T, Thoma A, Strumas N. A systematic review of rehabilitation protocols after surgical repair of the extensor tendons in zones V–VIII of the hand. J Hand Ther. 2011;24(4):365–73. https://doi.org/10.1016/j.jht.2011.06.005.
Townsend EA, Beagan B, Kumas-Tan Z, Versnel M, Iwana J, Landry J, et al. Habiliter: La compétence primordiale en ergothérapie [Enabling: The most important skill in occupational therapy]. In: Townsend EA, Polatajko HJ, editors. Habiliter à l’occupation : Faire avancer la perspective ergothérapique de la santé, du bien-être et de la justice par l’occupation. Ottawa, ON: CAOT Publications ACE; 2013. pp. 103–58.
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35(1):29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440.
Fortin M-F, Gagnon J. Fondements et étapes du processus de recherche: méthodes quantitatives et qualitatives [Foundations and stages of the research process: quantitative and qualitative methods]. 3rd ed. Montréal, Québec: Chenelière éducation. 2016. p. 518
Lecours A, Lord M-M, Negrini A, Robitaille R. How does returning to work after retirement influence older workers’ health? A scoping review protocol. BMJ Open. 2019;9(3):e026446.
Arends I, Bültmann U, Nielsen K, van Rhenen W, de Boer MR, van der Klink JJ. Process evaluation of a problem solving intervention to prevent recurrent sickness absence in workers with common mental disorders. Soc Sci Med. 2014;100:123–32. https://doi.org/10.1016/j.socscimed.2013.10.041.
Blonk RW, Brenninkmeijer V, Lagerveld SE, Houtman IL. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress. 2006;20(2):129–44. https://doi.org/10.1080/02678370600856615.
Brendbekken R, Eriksen HR, Grasdal A, Harris A, Hagen EM, Tangen T. Return to work in patients with chronic musculoskeletal pain: multidisciplinary intervention versus brief intervention: a randomized clinical trial. J Occup Rehabil. 2017;27(1):82–91. https://doi.org/10.1007/s10926-016-9634-5.
Dalgaard VL, Aschbacher K, Andersen JH, Glasscock DJ, Willert MV, Carstensen O, et al. Return to work after work-related stress: a randomized controlled trial of a work-focused cognitive behavioral intervention. Scand J Work Environ Health. 2017;43(5):436–46. https://doi.org/10.5271/sjweh.3655.
Du Bois M, Donceel P. Guiding low back claimants to work: a randomized controlled trial. Spine. 2012;37(17):1425–31. https://doi.org/10.1097/BRS.0b013e31824e4ada.
Gross D, Park J, Rayani F, Norris C, Esmail S. Motivational interviewing improves sustainable return to work in injured workers after rehabilitation: a cluster randomized controlled trial. Arch Phys Med Rehabil. 2017;98(12):2355–63. https://doi.org/10.1016/j.apmr.2017.06.003.
Hampel P, Köpnick A, Roch S. Psychological and work-related outcomes after inpatient multidisciplinary rehabilitation of chronic low back pain: a prospective randomized controlled trial. BMC Psychol. 2019;7(1):1–10. https://doi.org/10.1186/s40359-019-0282-3.
Irvine AB, Russell H, Manocchia M, Mino DE, Cox Glassen T, Morgan R, et al. Mobile-web app to self-manage low back pain: randomized controlled trial. J Med Internet Res. 2015;17(1):e1. https://doi.org/10.2196/jmir.3130.
Leon L, Jover JA, Candelas G, Lajas C, Vadillo C, Blanco M, et al. Effectiveness of an early cognitive–behavioral treatment in patients with work disability due to musculoskeletal disorders. Arthritis Care Res. 2009;61(7):996–1003. https://doi.org/10.1002/art.24609.
Marhold C, Linton SJ, Melin L. A cognitive-behavioral return-to-work program: effects on pain patients with a history of long-term versus short-term sick leave. Pain. 2001;91(1):155–63. https://doi.org/10.1016/s0304-3959(00)00431-0.
Netterstrøm B, Friebel L, Ladegaard Y. Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: results from a randomised, wait-list controlled trial. Psychother Psychosom. 2013;82(3):177–86. https://doi.org/10.1159/000346369.
Noordik E, van der Klink JJ, Geskus RB, de Boer MR, van Dijk FJ, Nieuwenhuijsen K. Effectiveness of an exposure-based return-to-work program for workers on sick leave due to common mental disorders: a cluster-randomized controlled trial. Scand J Work Environ Health. 2013;39(2):144–54. https://doi.org/10.5271/sjweh.3320.
Stenlund T, Nordin M, Järvholm LS. Effects of rehabilitation programmes for patients on long-term sick leave for burnout: a 3-year follow-up of the REST study. J Rehabil Med. 2012;44(8):684–90. https://doi.org/10.2340/16501977-1003.
van den Hout JH, Vlaeyen JW, Heuts PH, Zijlema JH, Wijnen JA. Secondary prevention of work-related disability in nonspecific low back pain: does problem-solving therapy help? A randomized clinical trial. Clin J Pain. 2003;19(2):87–96. https://doi.org/10.1097/00002508-200303000-00003.
Volker D, Zijlstra-Vlasveld MC, Anema JR, Beekman AT, Brouwers EP, Emons WH, et al. Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: results of a cluster randomized controlled trial. J Med Internet Res. 2015;17(5):e116. https://doi.org/10.2196/jmir.4097.
Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298(12):1401–11.
Bee PE, Bower P, Gilbody S, Lovell K. Improving health and productivity of depressed workers: a pilot randomized controlled trial of telephone cognitive behavioral therapy delivery in workplace settings. Gen Hosp Psychiatry. 2010;32(3):337–40. https://doi.org/10.1016/j.genhosppsych.2010.01.006.
Axén I, Brämberg EB, Vaez M, Lundin A, Bergström G. Interventions for common mental disorders in the occupational health service: a systematic review with a narrative synthesis. Int Arch Occup Environ Health. 2020;93(7):823–38. https://doi.org/10.1007/s00420-020-01535-4.
Doki S, Sasahara S, Matsuzaki I. Psychological approach of occupational health service to sick leave due to mental problems: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2015;88(6):659–67. https://doi.org/10.1007/s00420-014-0996-8.
Heathcote K, Wullschleger M, Sun J. The effectiveness of multi-dimensional resilience rehabilitation programs after traumatic physical injuries: a systematic review and meta-analysis. Disabil Rehabil. 2019;41(24):2865–80. https://doi.org/10.1080/09638288.2018.1479780.
Pomaki G, Franche R-L, Murray E, Khushrushahi N, Lampinen TM. Workplace-based work disability prevention interventions for workers with common mental health conditions: a review of the literature. J Occup Rehabil. 2012;22(2):182–95. https://doi.org/10.1007/s10926-011-9338-9.
Nieuwenhuijsen K, Verbeek JH, Neumeyer-Gromen A, Verhoeven AC, Bültmann U, Faber B. Interventions to improve return to work in depressed people. Cochrane Database of Systematic Reviews. 2014. https://doi.org/10.1002/14651858.CD006237.pub4.
Dewa C, Loong D, Bonato S, Joosen M. The effectiveness of return-to-work interventions that incorporate work-focused problem-solving skills for workers with sickness absences related to mental disorders: a systematic literature review. BMJ Open. 2015;5(6):e007122. https://doi.org/10.1136/bmjopen-2014-007122.
Ito D, Watanabe A, Takeichi S, Ishihara A, Yamamoto K. A preliminary study of work-focused cognitive behavioural group therapy for japanese workers. Behav Cogn Psychother. 2019;47(2):251–6. https://doi.org/10.1017/s1352465818000280.
Feuerstein M, Callan-Harris S, Hickey P, Dyer D, Armbruster W, Carosella AM. Multidisciplinary rehabilitation of chronic work-related upper extremity disorders. Long-term effects. J Occup Medicine. 1993;35(4):396–403.
Hållstam A, Löfgren M, Benson L, Svensén C, Stålnacke B-M. Assessment and treatment at a pain clinic: a one-year follow-up of patients with chronic pain. Scandinavian J Pain. 2017;17(1):233–42. https://doi.org/10.1016/j.sjpain.2016.08.004.
Woby SR, Roach NK, Urmston M, Watson PJ. Outcome following a physiotherapist-led intervention for chronic low back pain: the important role of cognitive processes. Physiotherapy. 2008;94(2):115–24. https://doi.org/10.1016/j.physio.2007.08.008.
Ekberg K. Workplace changes in successful rehabilitation. J Occup Rehabil. 1995;5(4):253–69. https://doi.org/10.1007/bf02109989.
Sjöström R, Alricsson M, Asplund R. Back to work–evaluation of a multidisciplinary rehabilitation programme with emphasis on musculoskeletal disorders. A two-year follow-up. Disabil Rehabil. 2008;30(9):649–55. https://doi.org/10.2147/JMDH.S32372.
Sullivan MJL, Ward LC, Tripp D, French DJ, Adams H, Stanish WD. Secondary prevention of work disability: community-based psychosocial intervention for musculoskeletal disorders. J Occup Rehabil. 2005;15(3):377–92. https://doi.org/10.1007/s10926-005-5944-7.
Braathen TN, Veiersted KB, Heggenes J. Improved work ability and return to work following vocational multidisciplinary rehabilitation of subjects on long-term sick leave. J Rehabil Med. 2007;39(6):493–9. https://doi.org/10.2340/16501977-0081.
Gismervik S, Fimland MS, Fors EA, Johnsen R, Rise MB. The acceptance and commitment therapy model in occupational rehabilitation of musculoskeletal and common mental disorders: a qualitative focus group study. Disabil Rehabil. 2019;41(26):3181–91. https://doi.org/10.1080/09638288.2018.1490824.
Sullivan MJL, Feuerstein M, Gatchel R, Linton SJ, Pransky G. Integrating psychosocial and behavioral interventions to achieve optimal rehabilitation outcomes. J Occup Rehabil. 2005;15(4):475–89. https://doi.org/10.1007/s10926-005-8029-9.
Johnston V, Shaw WS. Helping workers help themselves: empowering physiotherapy clients to manage musculoskeletal problems at work. Phys Therapy Reviews. 2013;18(5):373–8. https://doi.org/10.1179/1743288x13y.0000000087.
Lecours A, Groleau C. Habiliter les travailleurs à préserver leur santé mentale: que font les ergothérapeutes [Enabling workers to preserve their mental health: what are occupational therapists doing]? Can J Occup Ther. 2022;89(2):147–58. https://doi.org/10.1177/00084174221076228.
Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. J Orthop Sports Phys Therapy. 2019;49(4):212–5. https://doi.org/10.2519/jospt.2019.0605.
Longtin C, Coutu M-F, Tousignant-Laflamme Y. Deciphering programs for optimal self-management of persistent musculoskeletal-related pain and disability–clinical implications for PTs. Physiother Theory Pract. 2019;37(12):1264–72. https://doi.org/10.1080/09593985.2019.1698083.
Wallensten J, Åsberg M, Wiklander M, Nager A. Role of rehabilitation in chronic stress-induced exhaustion disorder: a narrative review. J Rehabilitation Med. 2019;51(5):331–42. https://doi.org/10.2340/16501977-2545.
Stergiopoulos E, Cimo A, Cheng C, Bonato S, Dewa CS. Interventions to improve work outcomes in work-related PTSD: a systematic review. BMC Public Health. 2011;11(1):1–10. https://doi.org/10.1186/1471-2458-11-838.
Kröger C, Bode K, Wunsch E-M, Kliem S, Grocholewski A, Finger F. Work-related treatment for major depressive disorder and incapacity to work: preliminary findings of a controlled, matched study. J Occup Health Psychol. 2015;20(2):248. https://doi.org/10.1037/a0038341.
Farholm A, Halvari H, Niemiec CP, Williams GC, Deci EL. Changes in return to work among patients in vocational rehabilitation: a self-determination theory perspective. Disabil Rehabil. 2017;39(20):2039–46. https://doi.org/10.1080/09638288.2016.1215559.
Hedges H. Blurring the boundaries: connecting research, practice and professional learning. Camb J Educ. 2010;40(3):299–314. https://doi.org/10.1080/0305764x.2010.502884.
Champagne F, Brousselle A, Hartz Z, Contandriopoulos A. Modéliser les interventions [Modeling interventions]. In: Brousselle A, Champagne F, Contandriopoulos A, Hartz H, editors. L’évaluation: Concepts et méthodes Montréal. Les Presses de l’Université de Montréal; 2011. pp. 71–84.
McLaughlin JA, Jordan GB. Using logic models. In: Newcomer K, Hatry H, Wholey J, editors. Handbook of practical program evaluation. 2 ed. États-Unis: John Wiley & Sons; 2015. pp. 7–32.
Longtin C, Tousignant-Laflamme Y, Coutu M-F. A logic model for a self-management program designed to help workers with persistent and disabling low back pain stay at work. Work. 2020;67(2):395–406. https://doi.org/10.3233/WOR-203289.
Bilodeau K, Gouin M-M, Lecours A, Lederer V, Durand M-J. Co-design of a return-to-work intervention after breast cancer treatments: feasibility study protocol. JMIR Preprints. 2022. https://doi.org/10.2196/preprints.37009.
Dulude E, Coutu M-F, Durand M-J. Promoting resilience in work rehabilitation: development of a transdiagnostic intervention. Disabil Rehabil. 2021;43(25):3652–62. https://doi.org/10.1080/09638288.2020.1744041.
Du S, Yuan C, Xiao X, Chu J, Qiu Y, Qian H. Self-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Patient Educ Couns. 2011;85(3):e299–e310. https://doi.org/10.1016/j.pec.2011.02.021.
Blau PM. Exchange and power in social life. New York: Wiley; 1964. p. 352.
Gouldner AW. The norm of reciprocity: a preliminary statement. Am Sociol Rev. 1960;25(2):161–78. https://doi.org/10.2307/2092623.
Tjulin Ã, MacEachen E, Ekberg K. Exploring workplace actors experiences of the social organization of return-to-work. J Occup Rehabil. 2010;20(3):311–21. https://doi.org/10.1007/s10926-009-9209-9.
Gates LB. Workplace accommodation as a social process. J Occup Rehabil. 2000;10(1):85–98. https://doi.org/10.1023/a:1009445929841.
Dawson DR, Gaya A, Hunt A, Levine B, Lemsky C, Polatajko HJ. Using the cognitive orientation to occupational performance (CO-OP) with adults with executive dysfunction following traumatic brain injury. Can J Occup Ther. 2009;76(2):115–27. https://doi.org/10.1177/000841740907600209.
Babulal GM, Foster ER, Wolf TJ. Facilitating transfer of skills and strategies in occupational therapy practice: practical application of transfer principles. Asian J Occup Therapy. 2016;11(1):19–25. https://doi.org/10.11596/asiajot.11.19.
Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87. https://doi.org/10.1016/S0738-3991(02)00032-0.
Tousignant-Laflamme Y, Longtin C, Coutu M-F, Gaudreault N, Kairy D, Nastasia I, et al. What are the essential components of a self-management program designed to help workers with chronic low back pain stay at work? A mapping review. Eur J Physiotherapy. 2020. https://doi.org/10.1080/21679169.2020.1822443.
Acknowledgements
This study would not have been possible without the colossal documentary research work of the following assistants and research professionals: Laurence Quenneville, Corinne St-Pierre, Annabelle Verville and Lysanne Scalabrini. Special thanks to Roxanne Bédard-Mercier for her support in the writing of this article. The invaluable assistance of the librarian Marie Denise Lavoie is also acknowledged.
Funding
This research was realized with the financial support of Institut de recherche Robert-Sauvé en santé et sécurité du Travail (IRSST), Grant No. 2019-0031.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AL, with the support of MFC and MJD. The first draft of the manuscript was written by AL. MFC and MJD commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical Approval
was not required for the review of previously published scientific literature.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lecours, A., Coutu, MF. & Durand, MJ. Fostering Stay at Work After a Period of Disability: A Scoping Review of Occupational Rehabilitation Strategies to Support Workers in the Adoption of Preventive Behaviours. J Occup Rehabil 34, 56–70 (2024). https://doi.org/10.1007/s10926-023-10122-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-023-10122-6