Abstract
Purpose To analyze the reliability and validity of a picture-based questionnaire, the Modified Spinal Function Sort (M-SFS). Methods Sixty-two injured workers with chronic musculoskeletal disorders (MSD) were recruited from two work rehabilitation centers. Internal consistency was assessed by Cronbach’s alpha. Construct validity was tested based on four a priori hypotheses. Structural validity was measured with principal component analysis (PCA). Test–retest reliability and agreement was evaluated using intraclass correlation coefficient (ICC) and measurement error with the limits of agreement (LoA). Results Total score of the M-SFS was 54.4 (SD 16.4) and 56.1 (16.4) for test and retest, respectively. Item distribution showed no ceiling effects. Cronbach’s alpha was 0.94 and 0.95 for test and retest, respectively. PCA showed the presence of four components explaining a total of 74% of the variance. Item communalities were >0.6 in 17 out of 20 items. ICC was 0.90, LoA was ±12.6/16.2 points. The correlations between the M-SFS were 0.89 with the original SFS, 0.49 with the Pain Disability Index, −0.37 and −0.33 with the Numeric Rating Scale for actual pain, −0.52 for selfreported disability due to chronic low back pain, and 0.50, 0.56–0.59 with three distinct lifting tests. No a priori defined hypothesis for construct validity was rejected. Conclusions The M-SFS allows reliable and valid assessment of perceived self-efficacy for work-related tasks and can be recommended for use in patients with chronic MSD. Further research should investigate the proposed M-SFS score of <56 for its predictive validity for non-return to work.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the Global Burden of Disease Study, musculoskeletal disorders (MSD) are a leading cause of work disability, inflicting substantial burden on society and the individual [1]. Long-term work disability in patients with MSD is often associated with low perceived self-efficacy [2]. According to Bandura, perceived self-efficacy (PSE) refers to the individual’s beliefs about their own competence and ability to undertake behaviors to achieve desired goals [3]. PSE affects how people behave in difficult situations, and people who doubt their capabilities shy away from tasks that they view as a personal threat. PSE is embedded in the theory of planned behavior (TPB). In the TPB it is assumed that intention to demonstrate a behavior is an important predictor for the actual behavior [4]. Behavioral intentions reflect the effort that people plan to behave in the valued direction and they are a function of: (a) the person attitude toward the behavior; (b) person’s perception of social norms regarding the behavior; and (c) the perceived behavioral control i.e. the person’s perception of ease or difficulty of the behavior [5]. By applying this model to rehabilitation it is assumed that patients with low levels of PSE are less likely to perform well on the tasks presented, and patients with high levels of PSE are assumed to perform better. In addition, PSE appears to be closely related to health outcomes [6] and return to work (RTW) in persons with MSD and psychological disorders [7, 8]. Therefore, measuring levels of PSE may be critical when tailoring interventions aimed to increase PSE and improve RTW outcomes.
An efficient way of assessing PSE in patients with MSD is the use of questionnaires. However, questionnaires have important limitations for their use in patients with diverse cultural backgrounds. The first is that the use of questionnaires depends on the literacy and linguistic skills of an evaluee, which may be limited in these patients [9]. The second is that only a few questionnaires assessing PSE have a work-related point of reference, but consider an unlimited spectrum of activities. These limitations may be overcome by using a picture-based questionnaire such as the Spinal Function Sort (SFS) [10]. The Spinal Function Sort (SFS) includes 50 depicted items, and claims to measure PSE to perform work-related tasks [10].
The SFS was shown to have good predictive value for work resumption in a multilingual European rehabilitation setting [11]. However, the rating of 50 items is time-consuming, and a shorter version of the SFS is warranted. It has also been suggested that the number of SFS items could be reduced by half because of redundant items [12, 13]. Another critique was that the SFS does not include pictures of prolonged work postures, ambulation and the images are outdated [12, 13]. Therefore, the 20-item Modified Spinal Function Sort (M-SFS) was developed using a mixed methods approach, which involved expert opinions, interviews with patients and item analysis based on data from clinical studies [14]. Validity and reliability of the M-SFS has not been established yet. The aim of this study is therefore assessing the validity, test–retest reliability and measurement error of the M-SFS in a group of patients with chronic nonspecific MSD in a rehabilitation setting.
Methods
Subjects, Context and Study Design
Subjects
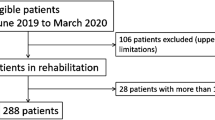
This study was embedded within the usual care for patients with MSD referred for an interdisciplinary inpatient work rehabilitation due to the following reasons: (1) having plateaued with previous medical and rehabilitative care; (2) not regaining full work capacity (WC); (3) exceeding expected healing times. Patient recruitment took place from December 2015 to June 2016 in two different Swiss Rehabilitation centers, in Bellikon (Canton Argovie) and Valens (Canton St. Gallen). Inclusion criteria were: Patients with chronic (>3 months), nonspecific MSD, age between 18 and 65, willing to participate in the retest after 2 days and to sign informed consent. Patients were excluded if they were pregnant, reported acute comorbidities (cardio-pulmonary, psychiatric, neurologic or internal medical), had a medically determined limit in lifting capacity <25 kg or were insufficiently proficient in the German language to understand instructions or read the questions.
Ethical approval for this study was granted by the Medical Ethics Committee of the Cantons Aargau and St. Gallen (EK AG 2012/073).
Study Design and Procedure
A test–retest design was chosen to evaluate the measurement properties of the M-SFS. After checking for eligibility, patients filled out demographic data and various questionnaires, including the M-SFS described in the next paragraph. Retest was performed no earlier than 2 days later than the first test to reduce risk for recall bias. The functional capacity evaluation (FCE) tests were performed after completion of the M-SFS retest.
Measurements
Modified Spinal Function Sort (M-SFS)
The M-SFS purports to measure PSE to perform work-related tasks. The M-SFS contains 20 drawings with simple written descriptions (see examples in Fig. 1). Patients rated their PSE for each task on a 5-point Likert scale ranging from “able” (4 points), to “restricted” (3, 2 or 1 points) or “unable” (0 points) adding up to a single rating score ranging from 0 to 80. Higher scores indicated higher PSE. The development of the M-SFS has been described in detail elsewhere [14].
Original Spinal Function Sort
The original Spinal Function Sort (SFS) measures PSE for work-related tasks that involve the spine [10]. The SFS contains 50 drawings with brief descriptions. The same 5-point Likert scale of the M-SFS is used in the SFS. The SFS yields a single rating ranging from 0 to 200, with higher scores indicating higher PSE. Validity and reliability of the SFS has been established for various musculoskeletal disorders, languages and settings [6, 7, 11, 12].
Pain Disability Index
The Pain Disability Index (PDI) is a self-report instrument assessing the degree to which chronic pain interferes with various daily activities [15]. The PDI contains seven categories of life activities: family, recreation, social activity, occupation, sexual behavior, self-care and life-support. A score of 0 means no disability at all, and a score of 10 signifies that all of the activities in which a person is normally involved are totally disrupted or prevented by pain. The total score ranges from 0 to 70, a higher score indicates more severe self-reported disability. Reliability and validity of the PDI as a brief measure of pain-related disability has been shown [16].
Oswestry Disability Index
Self-reported disability due to low back pain (LBP) was measured with the Oswestry Disability Index (ODI). The ODI contains 10 items: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life and travelling. Each item includes five statements reflecting different levels of perceived disability ranging from no disability (0) to total disability (5). The total score ranges from 0 to 50, a higher score indicates more severe self-reported disability. The ODI is reliable and has been validated in several languages and settings [17].
Pain
Pain intensity was measured with an 11-point numeric rating scale (NRS) ranging from no pain (0) to worst pain (10). The patient was asked to rate their actual pain (“pain now”). The NRS is a commonly used scale with proven reliability and validity in patients with MSD with different levels of literacy [18].
Physical Performance
Functional capacity evaluation (FCE) is a standardized battery of functional tests that intend to measure a patient’s safe physical ability for work-related activity [19]. For the purpose of this study three lifting tests were analyzed: lifting floor to waist (“lifting low”), lifting waist to crown height (“lifting high”) and short two-handed carry (“horizontal lift”). Patients were asked to perform the test to their maximum ability. The tests are described in detail elsewhere [20]. In order to compare the results of this study with previous studies with the original version of the SFS we did include three FCE tests used in these studies only [11, 13]. That kept the burden of the study small for the participants. The three FCE tests have shown acceptable reliability and validity in patients with various musculoskeletal disorders and professional backgrounds [12, 17,18,19,20].
Data Analysis
Normal distribution was visually assessed using P-P plots and tested with the Kolmogorov–Smirnov and the Shapiro–Wilk tests. Floor and ceiling effects for the M-SFS were considered to be present if more than 15% of participants achieved the lowest or highest possible score of the items [21].
Internal Consistency
Internal consistency was assessed by item-to-total correlations and Cronbach’s alpha. Optimal consistency for measurements at group level was considered when alpha value was between 0.7 and 0.9. Values <0.7 may be indicative for items measuring different traits, values >0.9 may be indicative for item redundancy [22].
Item-Structure Analysis
The dimensionality of the 20 M-SFS items was measured using principal component analysis (PCA) with Kaiser normalization and Varimax rotation. An Eigenvalue criterion of 1.0 was used for the analysis. Multidimensionality was assumed since the M-SFS contained new items about activities with tasks including postural tolerance and ambulation.
Test–Retest Reliability and Measurement Error
Test–retest reliability was expressed as an intraclass correlation coefficient (model 1; one-way random) (ICC). ICC was interpreted as follows: ICC ≥0.90 is excellent; good when ICC was between 0.75 and 0.90; moderate when ICC was between 0.50 and 0.75; and poor when ICC ≤0.50. ICCs were acceptable when ICC ≥0.75, and the lower boundary of the 95% confidence interval of the ICC ≥0.50 [23]. Measurement error was expressed in limits of agreement (LoA) (mean difference ± 1.96 × standard deviation of mean difference) [24]. The narrower the limits of agreement, the smaller the disagreement between the repeated tests.
Construct Validation: Hypothesis Testing
Four predefined hypotheses on the strength of the association between M-SFS and the original SFS, pain self-reported disability (ODI), self-reported pain (NRS) and physical performance (FCE tests) are displayed in Table 1. The strength of the association is expressed in the absolute value of the correlation coefficient. Associations were calculated using Spearman’s rank or Pearson’s correlation coefficient as appropriate and interpreted as follows: 0.00–0.29 are “small”; 0.30–0.49 are “medium”; and 0.50–0.99 are “large” in terms of the magnitude of the correlation [25]. The rational for the four hypotheses was the following: although new items were added, the M-SFS was expected to be highly correlated due to the overlap in 12 items between the two the original SFS and the M-SFS. We expected moderate correlations between the M-SFS and the two pain measures because previous literature has suggested that self-reported pain may influence perceived self-efficacy but they are distinct constructs [26]. In contrast, larger correlation coefficients were anticipated because we assumed the results from a systematic review suggests that higher self-efficacy predicts higher performance as measured with FCE tests [27]. Our hypothesis about the expected correlation was also supported by two of our previous studies which compared the original SFS and FCE lifting tests [11, 13]. Furthermore, the authors expected that male patients would score higher on the M-SFS than age-matched females because males work more frequently in manual occupations, which usually entails higher average physical capacity [28].
The M-SFS was considered valid when the majority (≥80%) of the a priori hypotheses were not rejected [29]. A significance level of p < 0.05 was used. All analyses were performed using SPSS (Statistical Package for Social Sciences, Version 20, IBM Corp.).
Results
Participants
From December 2015 to June 2016, 62 subjects were included based on the inclusion criteria (Table 2).
Item Distribution and Internal Consistency
Item distribution showed no ceiling or floor effects. The M-SFS total score for all participants was 54.4 (SD 16.4) and 56.1 (SD 16.4) for test and retest, and ranged between 16 and 79, and 14 and 80 for test and retest, respectively. In the test, male participants scored 57.9 [median, Interquartile range (IQR) 49–69] and female 55.0 (median, IQR 30–64). In the retest, male participants scored 64.0 (median, IQR 52–72) and female 48.0 (median, IQR 28–64).Total score item distribution by gender of the first test is displayed in Fig. 2 (retest data available on request). Internal consistency was Cronbach’s alpha 0.94 and 0.95 for test and retest, respectively.
Item-Structure Based on Principal Component Analysis (PCA)
PCA with fixed factors showed the presence of four components with initial Eigenvalues exceeding 1, explaining 50.2, 11.5, 6.2, and 5.7%, respectively, with a total of 74% of the variance. The inspection of the scree plot revealed four components. For the interpretation of the components Varimax rotation was executed. The rotated solution revealed the presence of a mixed structure of components showing distinct loadings >0.6 for 17 of 20 items, indicating reasonable evidence for multidimensionality (Table 3). Item 16 (walking) loaded on components 1, 2, 3, and 4 with values of 0.380, 0.398, 0.439 and −0.353, respectively.
Test–Retest Reliability and Agreement
The test–retest reliability measured with the ICC was 0.90 (95% CI 0.84–0.94). For the 62 patients in the reliability study, mean M-SFS scores for test and retest were 54.4 (mean, SD 16.4), and 56.1 (mean, SD 16.4), respectively. Mean difference in M-SFS score between test and retest was 1.7 (SD 7.3, p = .0.068). Hence LOA were +12.6 (upper limit) and −16.2 (lower limit) points (Fig. 3). Variances were related to the magnitude of the score.
Construct Validation
Correlations for first test between the M-SFS and the original SFS were 0.89, and −0.49 with pain-related disability (PDI), and −0.37 and −0.33 with self-reported pain (NRS) for test and retest. Correlation coefficients between the M-SFS and FCE tests for the first test were 0.43, 0.46 and 0.52 for lifting low, lifting high and horizontal lifting, respectively. In patients with low back pain, correlation with self-reported disability (ODI) was −0.52. All correlations were significant (p-value <0.001). Correlations of M-SFS scores during retest were higher correlated with the FCE test-results compared to the first test, ranging from 0.50, 0.56 to 0.59 for lifting low, lifting high and lifting horizontally. Hence, the four hypotheses were not rejected and validity of M-SFS was confirmed.
Discussion
This study assessed test–retest reliability and validity of the M-SFS in 62 patients with chronic nonspecific MSD in a work-related rehabilitation setting. Men rated their physical capacity on average higher than woman. No floor or ceiling effect of the items was observed. Internal consistency as well as test–retest reliability was high. Limits of agreement of 14.8 suggest that true changes in individuals are above 18.1 of the total score. We found a high correlation with the original SFS [11], suggesting a high criterion validity of the newly developed M-SFS. Low correlations with pain ratings and moderate correlations with self-reported pain disability as well as performed physical capacity suggest acceptable construct validity. None of the a priori defined hypotheses (see Table 1) were rejected and validity of M-SFS for this setting was confirmed. Principal component analysis confirmed the existence of main components lifting & carrying, activities with bending of the spine, prolonged body postures. These components are in line with the themes that emerged from the previous mixed-method study based on expert opinions, interviews with patients and item analysis from clinical study-data [14].
The lower correlations of the M-SFS with physical performance than previously found of the original SFS can, from our point of view, be explained by several factors. First the time of measurement, which in the current study was at the beginning of the rehabilitation stay while the original SFS was compared with physical performance at the end of rehabilitation. It has formerly been shown that self-reported physical capacity becomes more accurate with repeated testing, which happened in the retest [11]. Second, the items of the M-SFS focus less on lifting than the original SFS and include new items with postural activities and ambulation tasks. Third, several items depicting heavy-lifting tasks contained in the original SFS were removed, and finally, as reported in other studies, self-reported and performance-based measures of activity are related but distinct [28, 29].
This study revealed on average a 1.7 higher rated physical capacity at the retest measurement. The highest contribution to this systematic error in measurement results from patients with lower M-SFS scores. These patients showed higher total score variations from test to retest (see also Fig. 3). Obviously, such variation results in increased LoA. Large LoA scores in patient-reported outcome measure are common in pain patients [7, 30, 31]. We are unaware of accepted guidelines for cutoff points of LoA [30]. The observed 18% measurement error ratio (in our study is markedly below that score). In addition, sample characteristics need to be taken into account when interpreting the results. Previous studies reported that the LoA values of the original SFS administered by injured workers from a French-speaking rehabilitation setting were ±11 (6% of the maximal score of 200) while in the German-speaking area the values were ±27 (14% of the maximal score). Another study reported LoA values of ±33 (16% of the maximal score) of the original SFS in workers with subacute whiplash injuries [7]. The authors argued that beside individual differences, the cultural and legal context may also influence test–retest values [6, 7].
Bland–Altman plot of the M-SFS scores. The middle line represents the mean difference between the test and retest. The lines above and below the middle line represent the upper and lower limit of agreement, i.e. mean difference + 1.96 SD of the differences and mean difference −1.96 SD of the differences, respectively
Practical Implications of Measuring PSE
Guiding rehabilitation of workers with MSD by using the M-SFS may supported for the following reasons: First, the M-SFS attempts to measure PSE with specific, picture-based questions. It has been suggested that the closer a question to actual behavior, the more accurately behavior was predicted [32]. Therefore, the M-SFS may complement direct observations and information from peers to help guide treatment and RTW interventions. Second, the M-SFS assists the clinician to maintain the focus on function throughout the treatment by identifying and intervene on specific items with low scores. Third, substantial discrepancies between the self-reported ability measured with the M-SFS and observed ability may indicate psychological problems which may require more exploration [33]. Fourth, there is a need for measures which take into account culturally diverse patient groups [34, 35]. Hence, the M-SFS lends to translation into other languages because the short text is supplemented by pictorial illustrations [36].
Limitations
Besides its strengths, this study has limitations. First, additional studies are needed to compare the M-SFS to other work-related measures including tasks of postural tolerance, ambulation or repetitive bending of the spine. Second, the missing follow-up after rehabilitation prevents assessment of the predictive validity of the M-SFS for return to work. A cutoff score of <100 of the original SFS has shown to be predictive for non-return to work and was achieved by 42% of the responding patients with nonspecific chronic low back pain [11]. The equivalent M-SFS score at the 42nd percentile is <56. We therefore hypothesize that an M-SFS score <56 will be predictive for non-return to work in patients with MSD and recommend its cautious use until further research determines the predictive validity of the M-SFS. Third, the small sample size, which may alter results of the PCA. However, it has been suggested that if factor loadings are above 0.6, even relatively small samples (<100) may be perfectly adequate [37]. In this study 17 out of 20 items had factor loadings >0.6. Nevertheless, the factor structure of the M-SFS should be studied with larger samples. Further research on the M-SFS should also address the anticipated effect of repeated testing, investigate the ability to measure change (responsiveness) and predictive validity for return to work. Finally, transcultural adaptation and translation of the German M-SFS into other languages as well as validation in other settings and populations is needed.
Conclusion
Perceived self-efficacy for work-related tasks can reliably and validly be assessed with the M-SFS. Measurement properties of the M-SFS were similar to those of the original SFS while time for administration is substantially reduced. Hence, we recommend the use of the modified-version of the SFS. Further research should investigate the properties of the M-SFS with regards to other work-related measures and the proposed M-SFS score of <56 for its predictive validity for non-RTW.
References
GBD 2013 DALYs and HALE Collaborators, Murray CJ, Barber RM, Foreman KJ, Abbasoglu Ozgoren A, Abd-Allah F, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–2191.
Rahman A, Reed E, Underwood M, Shipley ME, Omar RZ. Factors affecting self-efficacy and pain intensity in patients with chronic musculoskeletal pain seen in a specialist rheumatology pain clinic. Rheumatology. 2008;47(12):1803–1808.
Bandura A. Self efficacy. In: Ramachaudran V, editor. Encyclopedia of human behavior. New York: Academic Press; 1994. pp. 71–88.
Madden TJ, Ellen PS, Ajzen I. A comparison of the theory of planned behavior and the theory of reasoned action. Personal Soc Psychol Bull. 1992;18(1):3–9.
Hogg M, Vaugham GM. Attitudes. Social psychology. 7th ed. Harlow: Pearson Education Limited; 2014. pp. 159–162.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Black O, Keegel T, Sim MR, Collie A, Smith P. The effect of self-efficacy on return-to-work outcomes for workers with psychological or upper-body musculoskeletal injuries: a review of the literature. J Occup Rehabil. 2017. doi:10.1007/s10926-017-9697-y.
Volker D, Zijlstra-Vlasveld MC, Brouwers EP, van Lomwel AG, van der Feltz-Cornelis CM. Return-to-work self-efficacy and actual return to work among long-term sick-listed employees. J Occup Rehabil. 2015;25(2):423–431.
Burrus C, Ballabeni P, Deriaz O, Gobelet C, Luthi F. Predictors of nonresponse in a questionnaire-based outcome study of vocational rehabilitation patients. Arch Phys Med Rehabil. 2009;90(9):1499–1505.
Matheson LN, Matheson ML, Grant J. Development of a measure of perceived functional ability. J Occup Rehabil. 1993;3(1):15–30.
Oesch PR, Hilfiker R, Kool JP, Bachmann S, Hagen KB. Perceived functional ability assessed with the spinal function sort: is it valid for European rehabilitation settings in patients with non-specific non-acute low back pain? Eur Spine J. 2010;19(9):1527–1533.
Borloz S, Trippolini MA, Ballabeni P, Luthi F, Deriaz O. Cross-cultural adaptation, reliability, internal consistency and validation of the spinal function sort (SFS) for French- and German-speaking patients with back complaints. J Occup Rehabil. 2012;22(3):387–393.
Trippolini MA, Dijkstra PU, Geertzen JH, Reneman MF. Measurement properties of the spinal function sort in patients with sub-acute whiplash-associated disorders. J Occup Rehabil. 2015;25(3):527–536.
Janssen S, Trippolini MA, Hilfiker R, Oesch P. Development of a modified version of the spinal function sort (M-SFS): a mixed method approach. J Occup Rehabil. 2015;26(3):253–263.
Pollard CA. Preliminary validity study of the pain disability index. Percept Mot Skills. 1984;59(3):974.
Tait RC, Chibnall JT, Krause S. The pain disability index: psychometric properties. Pain. 1990;40(2):171–182.
Fairbank JC, Pynsent PB. The oswestry disability index. Spine. 2000;25(22):2940–2952 (discussion 2952).
Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17(8):1022–1024.
Isernhagen SJ. Functional capacity evaluation: rational, procedure, utility of the kinesiophysical approach. J Occup Rehabil. 1992;2(3):157–168.
Trippolini MA, Reneman MF, Jansen B, Dijkstra PU, Geertzen JH. Reliability and safety of functional capacity evaluation in patients with whiplash associated disorders. J Occup Rehabil. 2013;23(3):381–390.
McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4(4):293–307.
Portney LG, Watkins MP. Reliability. Foundations of clinical research. Applications to practice. 2nd ed. Upper Saddle River: Prentice-Hall Health; 2000. pp. 61–77.
Bland JM, Altman DG. A note on the use of the intraclass correlation coefficient in the evaluation of agreement between two methods of measurement. Comput Biol Med. 1990;20(5):337–340.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–310.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Erlbaum; 1988.
Asante AK, Brintnell ES, Gross DP. Functional self-efficacy beliefs influence functional capacity evaluation. J Occup Rehabil. 2007;17(1):73–82.
van Abbema R, Lakke SE, Reneman MF, van der Schans CP, van Haastert CJ, Geertzen JH, Wittink H. Factors associated with functional capacity test results in patients with non-specific chronic low back pain: a systematic review. J Occup Rehabil. 2011;21(4):455–473.
Soer R, van der Schans CP, Geertzen JH, Groothoff JW, Brouwer S, Dijkstra PU, Reneman MF. Normative values for a functional capacity evaluation. Arch Phys Med Rehabil. 2009;90(10):1785–1794.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
Altman DG. Some common prolems in medical research. In: Altman DG, editor. Practical statistics for medical research. London: Chapman & Hall; 1991. pp. 396–403.
Keller A, Hellesnes J, Brox JI. Reliability of the isokinetic trunk extensor test, Biering-Sorensen test, and Astrand bicycle test: assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine. 2001;26(7):771–777.
Krauss SJ. Attitudes and the prediction of behavior. Personal Soc Psychol Bull. 1995;21(1):58–75.
Huijnen IP, Verbunt JA, Peters ML, Delespaul P, Kindermans HP, Roelofs J, Goossens M, Seelen HA. Do depression and pain intensity interfere with physical activity in daily life in patients with chronic low back pain? Pain. 2010;150(1):161–166.
Brady B, Veljanova I, Chipchase L. Are multidisciplinary interventions multicultural? A topical review of the pain literature as it relates to culturally diverse patient groups. Pain. 2016;157(2):321–328.
Scheermesser M, Bachmann S, Schamann A, Oesch P, Kool J. A qualitative study on the role of cultural background in patients’ perspectives on rehabilitation. BMC Musculoskelet Disord. 2012;13(5):1–13.
Matheson LN. History, design characteristics, and uses of the pictorial activity and task sorts. J Occup Rehabil. 2004;14(3):175–195.
MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychol Methods. 1999;4(1):84–99.
Acknowledgements
The authors thank the therapists from both participating clinics, the Rehaklinik Bellikon and the Kliniken Valens, for helping recruit participants, and all subjects for their participation. Additionally, we thank Michael Oliveri, for his important support, which led to the design of the new images of the M-SFS.
Author information
Authors and Affiliations
Contributions
MAT and SJ were responsible for funding and conducting the study at the Rehaklinik Bellikon and PO for conducting the study at the Rehabilitation Centre Valens. MAT and RH performed the statistical analysis. MAT conceived the first version of the manuscript. All authors were involved in the design, the method, and the interpretation of the results, and amended and approved the final version of the manuscript study report.
Corresponding author
Ethics declarations
Conflict of interest
This study was funded in part by a grant from the Swiss Accident Insurance Fund (Suva). The Verein Interessensgemeinschaft (IG) Ergonomie of the Swiss Association of Rehabilitation (SAR), a nonprofit organization, funded the drawing of new images of the M-SFS. Peter Oesch and Maurizio Trippolini are members of the Verein IG Ergonomie. All other authors declare that they have no conflict of interest. No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as modified in 2000.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Trippolini, M.A., Janssen, S., Hilfiker, R. et al. Measurement Properties of the Modified Spinal Function Sort (M-SFS): Is It Reliable and Valid in Workers with Chronic Musculoskeletal Pain?. J Occup Rehabil 28, 322–331 (2018). https://doi.org/10.1007/s10926-017-9717-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-017-9717-y